Abstract
Background: This study evaluates the results of ulnar shortening using the ulna osteotomy locking plate system (UOL; I.T.S. GmbH, Graz, Austria) with special regard to the time-dependent recovery of subjective and objective outcome parameters and surgeons’ experiences. Methods: Ulnar shortening using the UOL was performed on 11 patients (3 men, 8 women) with an average age of 47 ± 19.6 years. Range of motion (ROM) and grip strength were compared with the contralateral hand. Patient-rated outcomes were measured using a visual analogue scale (VAS) for pain and the Disability of the Arm, Shoulder and Hand (DASH) and the Patient Rated Wrist Evaluation (PRWE) survey for subjective outcomes. Ulnar variance and bony union were assessed using conventional wrist radiographs. The surgeons evaluated intraoperative handling through a standardized feedback form. Results: ROM improved and grip strength increased significantly between preoperative values and final follow-up. Flexion and supination improved significantly between weeks 8 and 12 and grip strength from week 8 onward. Patient-rated outcomes changed significantly with a final DASH score of 14.2 ± 12.4 and a PRWE score of 24.3 ± 17.0. Pain levels improved significantly with no pain at rest and a mean VAS of 0.8 ± 1.2 during activity. The average amount of shortening was 4.0 ± 1.9 mm with a final ulnar variance of 0.2 ± 1.8 mm. All osteotomies healed with 2 cases of delayed union. Conclusions: In ulnar shortening with the UOL, wrist function recovered after an initial decrease from week 8 onward. Subjective outcome parameters showed early recovery and improved continuously over time.
Keywords: ulnar impaction syndrome, ulnar shortening osteotomy, ulna osteotomy locking plate, positive ulnar variance, ulna leveling, wrist pain, recovery, time dependent
Introduction
Ulnar shortening osteotomy (USO) is a common procedure for various ulnar-sided wrist disorders, especially ulna impaction syndrome as a major cause of ulnar-sided wrist pain, which is caused by compression between the ulnar head, the triangular fibrocartilage complex (TFCC), and the proximal lunate and triquetrum due to positive ulnar variance.5
The correction of the radioulnar length discrepancy leads to pain relief and restoration of function. To achieve this difference, surgical options have been proposed in the literature. They range from diaphyseal10,11,17,19 or metaphyseal ulnar shortening15,20 to ablative techniques4,25 with specific indications, advantages, and drawbacks.
According to the number of reported cases, ulnar shortening at the diaphyseal level seems to be the most commonly applied procedure. Midterm and long-term results are generally favorable,6,23 as long as associated complications of nonunion and symptomatic plate prominence requiring implant removal can be avoided. Recent technical advances in plate design and osteotomy devices are reported to reduce complication rates.10,13,17 In addition to implant-related aspects, careful soft tissue handling is important to support biological healing capacity. The periosteum is highly vascular and has osteogenic capabilities. Therefore, keeping the periosteum intact to cover the osteotomy site may further reduce the nonunion rate.8
The ulna osteotomy locking plate system (UOL; I.T.S. GmbH, Graz, Austria) used in this study is one of the new-generation ulnar shortening devices. It combines parallel osteotomy, rotationally stable compression, stabilization by lag screw, and a locking plate system in a multifunctional device facilitating and standardizing this technically demanding surgical procedure.19
This study evaluates the results of ulnar shortening using the UOL with special regard to the time-dependent recovery of subjective and objective outcome parameters as well as surgeons’ experiences with its application.
Materials and Methods
Eleven patients with positive ulnar variance who underwent USO with the UOL between September 2011 and August 2014 participated in this prospective case series. Three senior hand surgeons performed the surgeries. Institutional ethics approval and preoperative informed consent were obtained.
The study group included 3 men and 8 women with an average age of 47 ± 19.6 years at the time of surgery. Of these patients, 3 were smokers with a mean daily consumption of 10.7 ± 8.1 cigarettes. None of them stopped smoking despite being informed about the higher risk of nonunion. In the majority of cases, the dominant hand was affected (8 of 11; 72.7%). Preoperative ulnar variance measured 4.2 ± 2.7 mm.
All patients were evaluated preoperatively and postoperatively at follow-up appointments after 3, 8, and 12 weeks and 6 months.
Clinical signs of ulna impaction syndrome consisted of ulnar-sided wrist pain that was aggravated by activity, forearm rotation and ulnar deviation of the wrist, swelling, positive ulnar fovea sign, and positive ulnocarpal stress test.18 The indication for surgery was an idiopathic ulna impaction syndrome in 5 patients and a symptomatic posttraumatic positive ulnar variance secondary to malunited distal radius fracture in another 5 patients. In addition, we included one geriatric patient with an acute comminuted distal radius fracture. In this case, it was not possible to restore radial length without bone grafting. We combined osteosynthesis of the distal radius with primary shortening of the ulna to address radioulnar length discrepancy. This is an alternative to a salvage procedure, like the distal ulna resection, that is in our hands limited to patients with rheumatoid arthritis, or the Sauvée-Kapandji technique.1
Surgical Technique
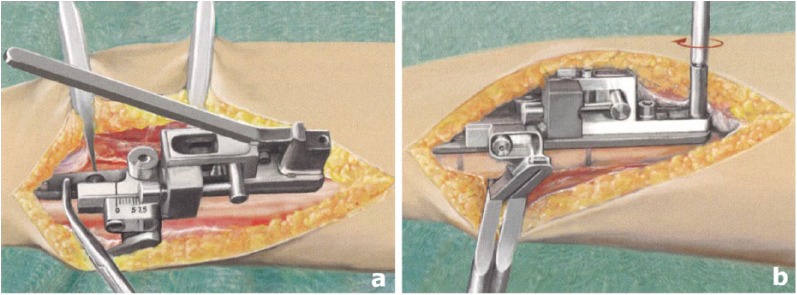
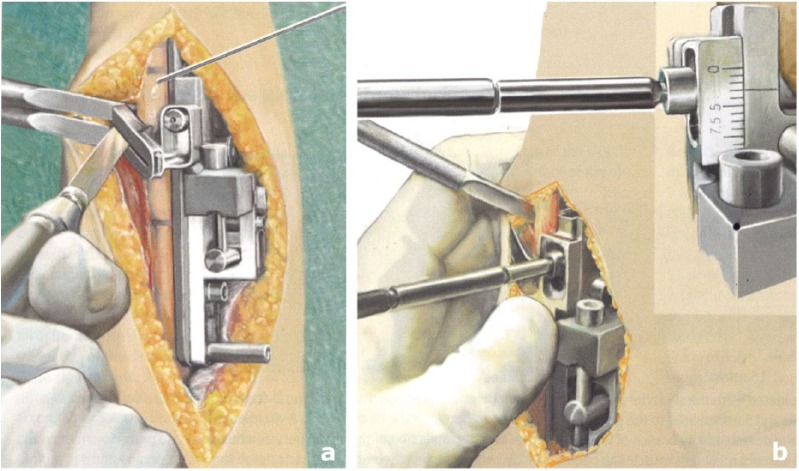
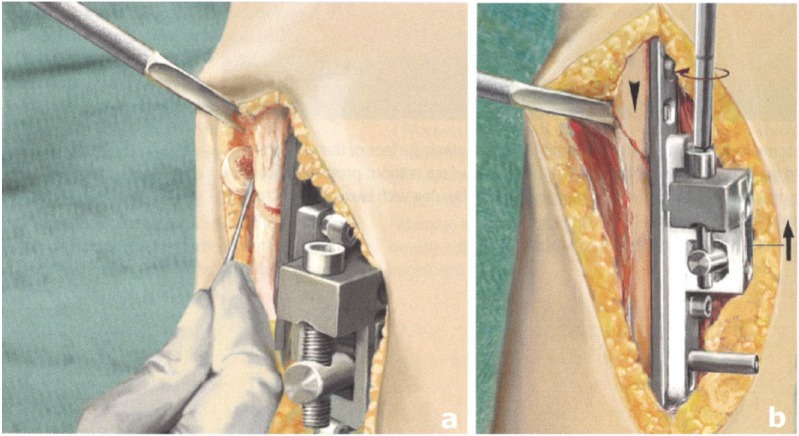
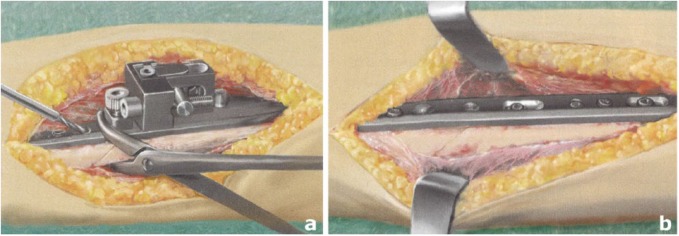
The shortening osteotomy was performed according to the manufacturer’s recommended technique.19 The UOL is mounted on the palmar surface of the ulna using standard ulnopalmar exposure (Figures 1a and 1b). Two parallel 45° osteotomies are performed according to the desired amount of shortening (Figures 2a and 2b) followed by rotationally stable shortening and compression (Figures 3a and 3b). After insertion of an interfragmentary lag screw perpendicular to the osteotomy site, compression screws replace the tension bolts sequentially in the sliding holes. For the remaining screw holes, locking screws are used to enhance stability (Figures 4a and 4b).
Figure 1.
(a) The completely assembled ulna osteotomy locking plate system is applied on the palmar surface of the ulna with the shaped end facing distally. (b) It is fixed distally with 2 locking screws and proximally with 2 tension bolts at the sliding holes that consist of a threaded front part and a massive head that is later used for fragment transport.
Source. Adapted from Schmidle et al19(p287) with permission of Springer.
Figure 2.
(a) The attached osteotomy guide is used to perform 2 parallel, oblique osteotomies under continuous irrigation with a sterile saline solution to prevent heat necrosis. (b) The screw of the osteostomy guide is loosened, the desired amount of shortening is set according to the preoperative measurements using the integrated millimeter scale, and the screw is tightened again. At this point, the second parallel osteotomy is performed as previously described.
Source. Adapted from Schmidle et al19(p288) with permission of Springer.
Figure 3.
(a) The bone fragment is removed and (b) after loosening of the tension bolts, shortening is performed using the setscrew for bone compression until bone contact is completed. The bolts are tightened again afterward.
Source. Adapted from Schmidle et al19(p288) with permission of Springer.
Figure 4.
(a) The oblique screw hole is drilled perpendicular to the osteotomy for an interfragmentary cortical lag screw. (b) As the bone fragments are stabilized by the lag screw, the bolts are replaced with cortical screws with the distal one first. After removal of the multifunctional device, angular stable screws are inserted at the remaining screw holes.
Source. Adapted from Schmidle et al19(p289) with permission of Springer.
To minimize devascularization, the periosteum is incised and reflected only as much as is needed to expose the osteotomy site. After the shortening procedure, it is brought back to cover the osteotomy site preserving the blood supply of the bone (Figures 5a and 5b).
Figure 5.
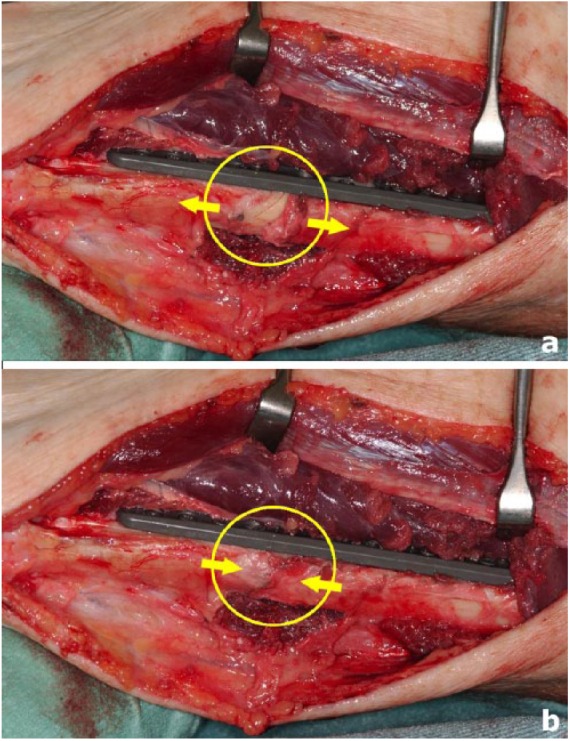
(a) The periosteum is incised and reflected only sufficiently to expose the osteotomy site (arrows). (b) At the end of the procedure, it is repositioned to cover the bone (arrows).
The patients were immobilized after surgery in a short arm cast for 3 weeks after the operation. Early active motion of all nonfixed joints of the upper extremity and prophylaxis of edema was commenced immediately. Active and passive motion of the wrist in sagittal and frontal plane started after cast removal. Patients were instructed to restrict forearm rotation up to 30° in supination and pronation, respectively, until they showed radiological signs of bone healing, to reduce shear forces at the osteotomy site. Weight bearing and forced active and passive motion therapy was commenced after bony union (blurring of the cortical margins and trabecular bridging of the osteotomy gap without tenderness at the osteotomy site).
Range of motion (ROM) measurements were performed using a standard goniometer. The assessment consisted of forearm supination/pronation, wrist extension/flexion, and wrist radial abduction/ulnar abduction for the affected and contralateral side. Grip strength was measured in kilograms on both the affected and contralateral hand using a hand dynamometer (Baseline® Hydraulic Hand Dynamometer; Irvington, New York). Grip strength was determined as a mean of 3 measurements in 1 handle position (position 2).26 ROM and grip strength were measured preoperatively, at the 8- and 12-week follow-ups and after 6 months. The data for ROM and grip strength were compared with the contralateral side.
Patients self-reported pain using a visual analogue scale (VAS). The VAS was scored from 0 (no pain) to 10 (maximal pain). Subjective outcomes were assessed using the Disability of Arm, Shoulder and Hand (DASH) and Patient Rated Wrist Evaluation (PRWE) questionnaires. In the DASH and PRWE surveys, outcomes are measured from 0 to 100 with lower scores corresponding to less disability. These subjective outcome parameters were assessed preoperatively and postoperatively at the 8-week, 12-week, and 6-month follow-up appointments.
The preoperative ulnar variance measurements of both sides and the postoperative measurement of the affected side were done using standard radiograph examination of the wrist in posteroanterior projection (shoulder 90° abducted, elbow flexed 90°, and forearm in neutral rotation). Ulnar variance was determined using the perpendicular line technique (Figures 6a and 6b).21 It is positive if the ulna projects distal to the lunate fossa and negative if it projects proximally. The status of bony union was recorded at 3, 8, and 12 weeks and at the final follow-up after 6 months. Union was defined as blurring of the cortical margins of osteotomy and trabecular bone bridging of the osteotomy gap without tenderness at the osteotomy site. Delayed union was defined as bone healing between 3 and 6 months. Absent bone healing after 6 months was defined as nonunion.
Figure 6.

(a) Preoperative radiograph demonstrating the method for determination of ulnar variance in a patient with idiopathic ulnar impaction syndrome with a positive ulnar variance of 2.9 mm (+UV) and (b) the postoperative result with a negative ulnar variance of −1.3 mm (−UV).
A standardized feedback form was used to gather information about the intraoperative performance of the locking plate system from the surgeons. The overall rating of system performance, as well as difficulties in plate positioning, application of the cutting guide, fragment transport, compression at the osteotomy site, screw placement, system assembly, and handling, was evaluated separately.
All values are expressed as means ± standard deviations. Significance was established at P < .05. The data were tested for normal distribution using the Kolmogorov-Smirnov test. Outcome parameters were analyzed for significant time-dependent changes by using the paired t test for parametric data. Nonparametric data were analyzed by the Wilcoxon signed rank test for paired differences. The analysis was conducted with the SPSS software package (SPSS 20.0, Chicago, Illinois).
Results
Table 1 shows the results for the objective outcome parameters of ROM and grip strength at the respective time intervals.
Table 1.
Functional Outcomes.
| Preoperative | 8 weeks | 12 weeks | 6 months | |
|---|---|---|---|---|
| ROM mean° ± SD (% contralateral) | ||||
| Extension | 53.1 ± 9.2 (84.1 ± 22.7) |
50.3 ± 17.5 (76.6 ± 26.3) |
55.3 ± 13.8 (86.3 ± 20.9) |
59.6 ± 11.3 (90.7 ± 12.5) |
| Flexion | 47.5 ± 11.3 (79.2 ± 24.3) |
44.0 ± 15.6 (78.5 ± 33.3) |
51.3 ± 10.0*
(94.3 ± 13.6) |
53.4 ± 9.2 (88.3 ± 15.1) |
| Ulnar abduction | 26.9 ± 11.6 (72.9 ± 29.9) |
29.3 ± 11.8 (83.9 ± 31.5) |
29.8 ± 11.6 (87.7 ± 18.3) |
33.8 ± 5.9 (96.7 ± 7.1) |
| Radial abduction | 18.8 ± 5.2 (83.1 ± 17.0) |
20.9 ± 6.2 (79.1 ± 26.5) |
20.2 ± 4.3 (92.0 ± 13.3) |
19.0 ± 5.7 (80.2 ±22.3) |
| Supination | 78.1 ±15.1 (89.9 ± 18.3) |
67.4 ± 19.4 (78.7 ± 21.1) |
81.3 ± 13.3*
(98.3 ± 13.3) |
85.0 ± 5.3 (100.3 ± 3.4) |
| Pronation | 76.3 ± 15.8 (86.6 ± 20.8) |
72.5 ± 14.4 (86.2 ± 12.8) |
77.6 ± 16.1 (95.5 ± 16.7) |
81.9 ± 7.9 (96.9 ± 7.5) |
| Grip strength mean kg ± SD (% contralateral) |
21.4 kg ± 11.9 (73.4 ± 9.8) |
16.0 kg ± 8.6 (54.2 ± 23.3) |
28.5 kg ± 16.6*
(85.5 ± 3.7) |
29.4 kg ± 14.3*
(96.4 ± 10.5) |
Note. ROM = range of motion; SD = standard deviation.
Indicating a statistically significant difference (P < .05) in comparison with the preceding values.
ROM improved over time not reaching statistical significance between preoperative values and the final follow-up. Significant improvement of flexion and supination occurred between weeks 8 and 12. For sagittal wrist motion (extension/flexion) and forearm rotation (supination/pronation), an initial decrease in ROM was found at week 8.
Grip strength increased significantly between preoperative values and final follow-up. The most considerable change was found between 8 and 12 weeks showing a significant difference.
The subset comparison of patients with idiopathic and posttraumatic ulnocarpal impingement showed significantly better function in idiopathic cases for pronation at 8 weeks and wrist flexion at the final follow-up (Table 2). There were no additional significant differences between these two groups.
Table 2.
Significant Differences in Outcomes According to Etiology.
| Preoperative | 8 weeks | 12 weeks | 6 months | |
|---|---|---|---|---|
| ROM mean° ± SD (% contralateral) | ||||
| Flexion | ||||
| Idiopathic | 53 ± 8.4 (89.6 ± 15.8) |
48 ± 19.2 (85.4 ± 42.9) |
56 ± 5.5 (98.5 ± 3.4) |
61.3 ± 2.5*
(102.1 ± 4.2) |
| Posttraumatic | 38.3 ± 10.4 (65.4 ± 30) |
42.5 ± 11.9 (80 ± 15.2) |
46.8 ± 13 (87.4 ± 20.9) |
46.8 ± 8.3*
(79.1 ± 13.5) |
| Pronation | ||||
| Idiopathic | 81 ± 10.3 (90.3 ± 13.1) |
82 ± 8.4*
(93.3 ± 9.9) |
87 ± 6.7 (100 ± 0) |
87.5 ± 5 (100 ± 0) |
| Posttraumatic | 68.3 ± 22.6 (81.6 ± 31.3) |
58.8 ± 10.3*
(76.8 ± 12.4) |
67.8 ± 19.2 (88.6 ± 27.1) |
77.8 ± 8.3 (96.1 ± 10) |
Note. ROM = range of motion; SD = standard deviation.
Indicating a statistically significant difference (P < .05) comparing idiopathic and posttraumatic cases of ulnocarpal impaction.
The results for the subjective parameters are shown in Table 3. All parameters improved significantly between preoperative values and final follow-up.
Table 3.
Subjective Outcomes.
| Preoperative | 3 weeks | 8 weeks | 12 weeks | 6 months | |
|---|---|---|---|---|---|
| DASH mean ± SD |
34.3 ± 16.9 | — | 38.6 ± 16.6 | 26.7 ± 11.9* | 14.2 ± 12.4* |
| PRWE mean ± SD |
55.8 ± 16.0 | — | 38.3 ± 20.7* | 32.0 ± 13.6 | 24.3 ± 17.0* |
| Pain at rest VAS mean ± SD |
2.3 ± 2.1 | 2.1 ± 1.8 | 1.0 ± 1.6* | 0.5 ± 1.0 | 0.0 ± 0.0 |
| Pain during activity VAS mean ± SD |
5.4 ± 3.3 | — | 3.1 ± 2.1* | 1.5 ± 1.5* | 0.8 ± 1.2 |
Note. DASH = Disability of the Arm, Shoulder and Hand; SD = standard deviation; PRWE = Patient Rated Wrist Evaluation; VAS = visual analogue scale (0 min, 10 max).
Indicating a statistically significant difference (P < .05) in comparison with the preceding values.
Subjective outcome scores improved over time with a significant effect on the DASH score from week 8 onward. The PRWE score showed significant changes between operation and 8 weeks as well as between 12 weeks and final follow-up.
Pain as measured by the VAS improved significantly between 3 and 8 weeks. Pain during activity was significantly reduced between preoperative values and the 8-week follow-up with a further significant reduction until week 12.
Postoperative ulnar variance measured 0.2 ± 1.8 mm. The mean amount of shortening was 4.0 ± 1.9 mm. Preoperatively, the ulnar variance on the affected side was 2.3 ± 1.8 mm higher. The shortening procedure resulted in an ulnar variance of −1.1 ± 1.4 mm compared with the opposite side. All osteotomies healed with 2 cases of delayed union. Eight patients healed within 8 weeks, 1 within 12 weeks, and 2 until the 6-month follow-up leading to a mean time to union of 11.3 ± 6.4 weeks.
Positioning of the plate on the palmar side, use of the cutting guide, and screw placement were rated by the surgeons as very easy or easy in 90.9% of cases. System assembly, fragment transport, and compression were seen as very easy or easy in 81.8%. Overall handling of the ulna osteotomy locking plate system was rated as very good and good in 10 of 11 cases.
Discussion
USO at the diaphyseal level is a standard procedure for various ulnar-sided disorders. Its effectiveness in pain relief and restoration of function for idiopathic and posttraumatic ulnocarpal impingement syndrome has been shown multiple times.11,13,19,23 Severe malunion of the distal radius, reverse inclination of the distal radioulnar joint (DRUJ) and active DRUJ arthritis are known contraindications for this technique. If they are respected, reliable results can be expected.16,24 Smoking is a known risk factor for nonunions but was not seen as a contraindication for the procedure.
Metaphyseal USO may lead to faster healing and needs only screws to stabilize, but these techniques are limited in their amount of shortening up to 4 mm and are technically more challenging.15,20 The osteotomy has to be performed by freehand technique and there is a higher risk of injury to the dorsal branch of the ulnar nerve due to the more distal approach. The anatomical relationship between TFCC and extensor retinaculum requires caution in the design of the flap to avoid scarring over the underlying tendons causing a reactive synovitis.
The complications of nonunion and symptomatic plate prominence necessitating hardware removal are known risks for USO at the diaphyseal level and have led to an evolution of technique and hardware systems. Changes in plate design, palmar plate position, guided parallel osteotomy, rotationally stable shortening, compression at the osteotomy site, adding of angular stability as well as the preservation of the periosteum helps minimize these complications. With these advances in surgical technique and hardware systems, the USO has become a technically simple procedure with high success rates.2,3,8,13,19
This prospective study evaluates the results of USO using a new-generation UOL with special regard to time-dependent recovery of subjective and objective outcome parameters. The knowledge of time-dependent changes may be of importance for aftercare and preoperative patient counseling.
The immediate postoperative period with cast immobilization and limitation of forearm rotation to promote bone healing led to an initial decrease in ROM without long-term consequences. The main increase was found between 8 and 12 weeks with a significant improvement for flexion and supination. Only minor changes were found thereafter. Grip strength increased significantly from week 8 onward.
The subset comparison of patients with idiopathic and posttraumatic ulnocarpal impingement showed significant differences for pronation at 8 weeks and wrist flexion at the final follow-up. Distal radius malunion itself as well as trauma-related scarring of ligaments and capsule can explain the limited ROM in the sagittal plane compared with uninjured wrists.
For subjective outcome measurement, we evaluated both the function-focused DASH score and the PRWE score that reflects wrist pain (the main problem in ulnocarpal impingement syndrome) to a greater extent. The mean improvements of the DASH (20.1 ± 13.2) and PRWE (30.6 ± 18.7) scores between preoperative values and 6 months were well beyond the amount that has been proposed to be necessary (13.5 DASH points, 17 PRWE points) to achieve a benefit that patients may perceive as clinically important.9
In our prospective case series, all osteotomies healed, with 2 cases of delayed union. One patient was male and young in the idiopathic group, and the other one was female and aged in the posttraumatic group. No specific characteristics stood out as different from the other patients. In contrast to other reports, we did not find any correlations between smoking and outcome with both patients with delayed unions being nonsmokers.7
Surgeons reported overall high satisfaction with the UOL. In 1 case, the surgeon was not satisfied with the system. Problems occurred with fragment transport and compression at the osteotomy site not influencing bony union and final outcome. To avoid such problems—especially in patients with reduced bone quality—it is advised to stabilize the plate against the bone during the shortening process (Figure 3b), for example, by pinch grip. This reduces the lever arm and prevents loosening of the tension bolts. After shortening, it is advised to secure the reduction with a bone clamp until final screw stabilization is achieved to avoid potential problems.
The postoperative follow-up was limited to 6 months, as patients usually reach stable functional recovery within this time period. In the literature, short-term results for ulnar shortening with a minimum follow-up of 1 year,13 as well as midterm6 and long-term results23 after 5 or 10 years have shown objective and subjective results comparable with our study. In up to 50% of long-term observations, degenerative changes in the DRUJ are present but they seem not to have significant clinical relevance.22
According to the literature, TFCC tears can be well addressed with USO in ulnar positive patients,12,14 which is why we did not perform wrist arthroscopy to confirm or address TFCC tears in our study.
The small sample size is a limitation to this study. In patients with ulnar impaction syndrome but only minor positive ulnar variance up to 2 to 3 mm, competitive surgical procedures, like the arthroscopic wafer procedure, have been performed. This, due to the surgeons’ preferences, limited patient recruitment. This is reflected in the high mean shortening of 4.0 mm. For this patient group, however, the USO at the diaphyseal level proved to be effective in improving subjective and objective outcome parameters with high user satisfaction and low complication rates.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Arora R, Gabl M, Pechlaner S, et al. Initial shortening and internal fixation in combination with a Sauve-Kapandji procedure for severely comminuted fractures of the distal radius in elderly patients. J Bone Joint Surg Br. 2010;92:1558-1562. [DOI] [PubMed] [Google Scholar]
- 2. Boardman MJ, Imbriglia JE. Surgical management of ulnocarpal impaction syndrome. J Hand Surg Am. 2010;35:649-651; quiz 651. [DOI] [PubMed] [Google Scholar]
- 3. Clark SM, Geissler WB. Results of ulnar shortening osteotomy with a new plate compression system. Hand (N Y). 2012;7:281-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Feldon P, Terrono AL, Belsky MR. Wafer distal ulna resection for triangular fibrocartilage tears and/or ulna impaction syndrome. J Hand Surg Am. 1992;17:731-737. [DOI] [PubMed] [Google Scholar]
- 5. Friedman SL, Palmer AK. The ulnar impaction syndrome. Hand Clin. 1991;7:295-310. [PubMed] [Google Scholar]
- 6. Fufa DT, Carlson MG, Calfee RP, et al. Mid-term results following ulna shortening osteotomy. HSS J. 2014;10:13-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fulton C, Grewal R, Faber KJ, et al. Outcome analysis of ulnar shortening osteotomy for ulnar impaction syndrome. Can J Plast Surg. 2012;20:e1-e5. [PMC free article] [PubMed] [Google Scholar]
- 8. Hamada Y, Sairyo K, Hibino N, et al. Effect of preservation of corticoperiosteal attachment on bone healing at osteotomy sites after ulna-shortening osteotomy. Hand (N Y). 2015;10:105-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim JK, Park ES. Comparative responsiveness and minimal clinically important differences for idiopathic ulnar impaction syndrome. Clin Orthop Relat Res. 2013;471:1406-1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kitzinger HB, Karle B, Low S, et al. Ulnar shortening osteotomy with a premounted sliding-hole plate. Ann Plast Surg. 2007;58:636-639. [DOI] [PubMed] [Google Scholar]
- 11. Luria S, Lauder AJ, Trumble TE. Comparison of ulnar-shortening osteotomy with a new Trimed dynamic compression system versus the Synthes dynamic compression system: clinical study. J Hand Surg Am. 2008;33:1493-1497. [DOI] [PubMed] [Google Scholar]
- 12. Minami A, Kato H. Ulnar shortening for triangular fibrocartilage complex tears associated with ulnar positive variance. J Hand Surg Am. 1998;23:904-908. [DOI] [PubMed] [Google Scholar]
- 13. Nagy L, Jungwirth-Weinberger A, Campbell D, del Pino JG. The AO ulnar shortening osteotomy system indications and surgical technique. J Wrist Surg. 2014;3:91-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Papapetropoulos PA, Wartinbee DA, Richard MJ, et al. Management of peripheral triangular fibrocartilage complex tears in the ulnar positive patient: arthroscopic repair versus ulnar shortening osteotomy. J Hand Surg Am. 2010;35:1607-1613. [DOI] [PubMed] [Google Scholar]
- 15. Pechlaner S. [Decompression of the ulnar wrist joint compartment by decompression osteotomy of the head of the ulna]. Handchir Mikrochir Plast Chir. 1998;30:375-378. [PubMed] [Google Scholar]
- 16. Prommersberger KJ, Kalb K, van Schoonhoven J. [Mal-united fractures of the distal radius—biomechanics and operative treatment options]. Handchir Mikrochir Plast Chir. 2007;39:9-18. [DOI] [PubMed] [Google Scholar]
- 17. Rayhack JM, Gasser SI, Latta LL, et al. Precision oblique osteotomy for shortening of the ulna. J Hand Surg Am. 1993;18:908-918. [DOI] [PubMed] [Google Scholar]
- 18. Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome, and lunotriquetral ligament tears. J Hand Surg Am. 2008;33:1669-1679. [DOI] [PubMed] [Google Scholar]
- 19. Schmidle G, Arora R, Gabl M. Ulnar shortening with the ulna osteotomy locking plate. Oper Orthop Traumatol. 2012;24:284-292. [DOI] [PubMed] [Google Scholar]
- 20. Sennwald G, Della Santa D, Beaulieu JY. A comparison of diaphyseal and metaphyseal techniques of ulna shortening. J Hand Surg Eur Vol. 2013;38:542-549. [DOI] [PubMed] [Google Scholar]
- 21. Steyers CM, Blair WF. Measuring ulnar variance: a comparison of techniques. J Hand Surg Am. 1989;14:607-612. [DOI] [PubMed] [Google Scholar]
- 22. Tatebe M, Nishizuka T, Hirata H, et al. Ulnar shortening osteotomy for ulnar-sided wrist pain. J Wrist Surg. 2014;3:77-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tatebe M, Shinohara T, Okui N, et al. Clinical, radiographic, and arthroscopic outcomes after ulnar shortening osteotomy: a long-term follow-up study. J Hand Surg Am. 2012;37:2468-2474. [DOI] [PubMed] [Google Scholar]
- 24. Tolat AR, Stanley JK, Trail IA. A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg Br. 1996;21:587-594. [DOI] [PubMed] [Google Scholar]
- 25. Tomaino MM, Weiser RW. Combined arthroscopic TFCC debridement and wafer resection of the distal ulna in wrists with triangular fibrocartilage complex tears and positive ulnar variance. J Hand Surg Am. 2001;26:1047-1052. [DOI] [PubMed] [Google Scholar]
- 26. Trampisch US, Franke J, Jedamzik N, et al. Optimal jamar dynamometer handle position to assess maximal isometric hand grip strength in epidemiological studies. J Hand Surg Am. 2012;37:2368-2373. [DOI] [PubMed] [Google Scholar]