Abstract
Background: Stenosing tenosynovitis, or trigger digit, is a common condition for which patients often seek relief. Corticosteroid injections have been shown to provide relief in many cases, and several different approaches for delivering the injection have been described in the literature. We compared patients’ perception of pain following each of 3 accepted injection methods, namely, palmar proximal, palmar distal, and webspace approaches. Methods: We prospectively followed 38 patients with 39 symptomatic digits in this trial, with varying severities of trigger finger as graded by the Patel and Moradia classification. The patients were divided into 3 groups representing the 3 approaches without randomization, based upon the treating surgeons’ preference. Disabilities of the Arm, Shoulder and Hand and visual analog scale (VAS) pain scores were calculated pre-injection and at 4-week and 8-week follow-up visits. Results: No statistically significant differences in age, sex, affected extremity, grade, or duration of symptoms were observed among the 3 approaches. No statistically significant differences in VAS score were found between the palmar proximal (mean = 6.6, SD = 2.6), palmar distal (mean = 6.0, SD = 2.8), and webspace (mean = 6.8, SD = 1.8) approaches. Conclusion: Our data suggest that injection approach does not affect patient pain perception scores or outcomes. We recommend that the technique that is most comfortable to the surgeon be utilized, with the understanding that one injection alone has a low likelihood of relieving symptoms.
Keywords: trigger finger, corticosteroid, injections, DASH, VAS
Introduction
Stenosing tenosynovitis, or trigger digit, is a common idiopathic condition caused by inflammation of the flexor tendon within its corresponding fibroosseous sheath.2 Patients present with pain, catching, triggering, and/or locking of the digit; an inability to smoothly flex or extend the digit; and display tenderness and/or a nodule at the A1 pulley.1,8,9
Two types of stenosing tenosynovitis are described: nodular and diffuse.4 When a well-defined nodule, which is caused by spindle-shaped thickening in a localized area of tendon, is palpated under the examiner’s fingers, it is considered nodular-type.6 However, if there is diffuse swelling, with no defined nodule, it is termed diffuse. Although all digits can be affected, the ring is most often involved, followed by the thumb, long, index, and small fingers.4 More than 1 trigger can be present on the same hand, or in both hands. This condition can be very disabling, especially if locking is present.
Many treatments have been described9 including splinting,10,11 injections,5,10 percutaneous release,11 and open surgical release,7 but all share the common goals of producing smooth and painless range of motion of the affected digits. Corticosteroid injections, pioneered by Howard et al5 in 1953, are commonly used as a first-line or early treatment of this condition and may bring about its complete resolution in 48% to 95% of cases if multiple injections are used.3,4,9,11,14
There is, however, debate within the literature as to which approach for injection is superior. While several approaches have been described to deliver the steroid, including proximal palmar, palmar distal, and webspace approaches, no studies have compared patients’ perception of pain following each injection method.
We compared the differences in subjective pain perception among patients receiving corticosteroid injections for symptomatic trigger digits using the 3 approaches described above. We also assessed the differences in outcomes before and after the injection using functional scoring questionnaires. We hypothesized that all 3 approaches would demonstrate similar efficacy, while the webspace approach would be least painful.
Materials and Methods
Following the approval of our institutional review board, we began to prospectively collect data on patients who presented to 3 board-certified hand surgeons with symptomatic trigger digits. Informed consent was obtained from all individual participants included in the study. Inclusion criteria were the following: age 18 years or older, single idiopathic trigger digit in Patel and Moradia grades 1 to 3, no prior injection into the affected digit, patient able to understand English, and symptoms for less than 12 months. Exclusion criteria were the following: patients with comorbid endocrine disorders, rheumatoid arthritis, on renal dialysis, age younger than 18 years, locked trigger digit, or symptoms greater than 12 months. Each surgeon performed injections using 1 of the 3 approaches according to his or her personal practice preference.
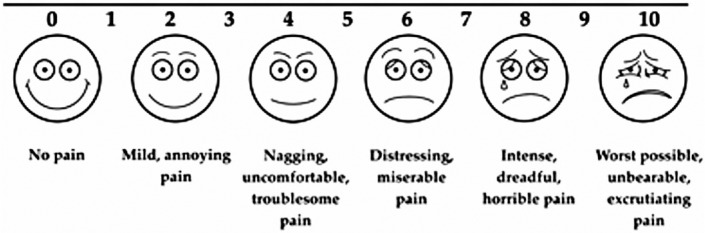
Patients were classified according to the Patel and Moradia classification for trigger digits (Table 1).11 Each patient filled out a visual analog scale (VAS) (Figure 1) immediately following their injection. Disabilities of the Arm, Shoulder and Hand (DASH) questionnaires were collected both prior to and after the injections, at 4-week and 8-week follow-up visits. Participating patients were asked to classify their result into 1 of 4 categories: (1) complete resolution of symptoms, (2) improved result, but incomplete resolution of symptoms, not warranting further treatment, (3) partial response, but unsatisfactory, warranting further treatment, and (4) no response. The patients and clinicians discussed this categorization, and responses were recorded.
Table 1.
Patel and Moradia Classification.
| Grade 1: Uneven movements, no locking |
| Grade 2: Clicking, no locking |
| Grade 3: Locking, actively or passively |
| Grade 4: Locked, cannot be unlocked |
Figure 1.
The visual analog scale used by patients to quantify their pain felt after injection.
Method of Injection
Each surgeon performed the injection according to his or her personal preference in practice. All surgeons used 4 mg (1 cc) of dexamethasone without the addition of a local anesthetic. The palmar proximal approach (Figure 2) is described: A 27-gauge needle is used to inject directly into the tendon sheath from the palmar aspect. The starting point is at the central proximal aspect of the A1 pulley, aiming distally. The needle is introduced through the skin, into the synovial sheath, through tendon, and into bone. It is then retracted slightly, at which point the steroid is injected.
Figure 2.
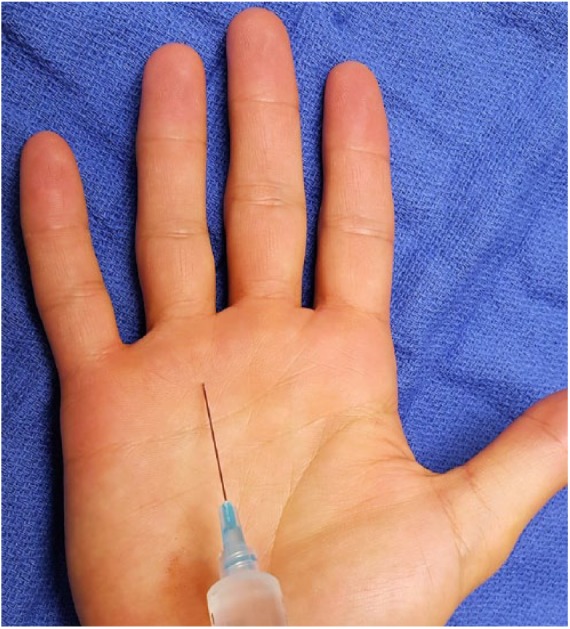
The palmar proximal approach. The starting point is at the central proximal aspect of the A1 pulley, aiming distally.
The palmar distal approach (Figure 3) was performed in the following manner: A 27-gauge needle is used to inject directly into the tendon sheath from the palmar aspect, with the insertion site in the midline at the proximal phalanx, aiming proximally toward the A1 pulley. The needle is inserted through skin, subcutaneous tissue, tendon sheath, and tendon until bone is reached. Gentle pressure is applied on the syringe, enabling free flow of steroid.
Figure 3.

The palmar distal approach. The needle is inserted directly into the tendon sheath from the palmar aspect, with the insertion site in the midline at the proximal phalanx, aiming proximally toward the A1 pulley.
The webspace approach (Figure 4) was performed as follows: A 27-gauge needle is inserted into the webspace of the proximal phalanx on the dorsal radial aspect of the finger (the index is approached from the dorsal ulnar webspace). The needle is inserted until slight resistance is felt, and the steroid is injected into the sheath.
Figure 4.

The webspace approach. The needle is inserted into the webspace of the proximal phalanx on the dorsal radial aspect of the finger (the index is approached from the dorsal ulnar webspace).
Data Analysis
Descriptive statistics were used to describe the patient characteristics. Differences in patient characteristics were compared among the 3 approaches using chi-square tests. Differences in pre- and post-injection DASH scores, as well as patient-reported pain VAS score immediately following their injection, were compared using analysis of variance. In addition, subgroup analysis was also performed to describe the average scores of pre- and postinjection DASH, and VAS for thumbs and the lesser digits. Statistical significance was defined as P < .05. The data analyses were performed using SAS 9.3.
Results
We enrolled 39 patients into the study with an average duration of symptom presentation for 2.5 months. One patient withdrew from the study, giving a sample size of 38 patients, including 39 symptomatic digits. Twelve digits were included in the palmar distal injection group, 22 in the palmar proximal injection group, and 5 in the webspace injection group. The 39 digits included 16 thumbs (41%) (Table 2). There were 12.8% of patients (n = 5) with grade 1 triggering symptoms, 15.4% (n = 6) with grade 2, and 71.8% (n = 28) with grade 3. No statistically significant differences in age, sex, race, affected side, grade, and duration of symptoms were observed among the 3 approaches. No statistically significant differences in VAS score were found among the palmar proximal (mean = 6.6, SD = 2.6), palmar distal (mean = 6.0, SD = 2.8), and webspace (mean = 6.8, SD = 1.8) approaches (Table 3). While no statistically significant differences were observed in post-injection DASH average scores among the 3 approaches (P = .664), statistically significant differences in pre-injection DASH scores were found among the 3 methods. Specifically, for webspace injection, the DASH average score was 9.3 (SD = 8.6), which was significantly lower than DASH average scores for the palmar proximal (mean = 31.2, SD = 16.4) and palmar distal (mean = 18.7, SD = 12.8) approaches. A large proportion of patients, regardless of injection method, either opted for a repeat injection (18 patients, 46.2%) or surgical release (22 patients, 56.4%).
Table 2.
Patient Demographics by the Three Approaches.
| All patients (N = 39) |
Palm (n = 22) |
Phalanx (n = 12) |
Webspace (n = 5) |
P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Sex | 0.543 | ||||||||
| Male | 17 | 43.6 | 8 | 47.1 | 6 | 35.3 | 3 | 17.7 | |
| Female | 22 | 56.4 | 14 | 63.6 | 6 | 27.3 | 2 | 9.1 | |
| Race | 0.894 | ||||||||
| White | 34 | 87.2 | 18 | 52.9 | 11 | 32.4 | 5 | 14.7 | |
| Black | 3 | 7.7 | 2 | 66.7 | 1 | 33.3 | 0 | 0.0 | |
| Other | 2 | 5.1 | 2 | 100.0 | 0 | 0.0 | 0 | 0.0 | |
| Grade | 0.406 | ||||||||
| 1.0 | 5 | 12.8 | 4 | 80.0 | 0 | 0.0 | 1 | 20.0 | |
| 2.0 | 6 | 15.4 | 4 | 66.7 | 1 | 16.7 | 1 | 16.7 | |
| 3.0 | 28 | 71.8 | 14 | 50.0 | 11 | 39.3 | 3 | 10.7 | |
| Affected side | 0.904 | ||||||||
| Right | 21 | 53.8 | 11 | 52.4 | 7 | 33.3 | 3 | 14.3 | |
| Left | 18 | 46.2 | 11 | 61.1 | 5 | 27.8 | 2 | 11.1 | |
| Affected finger | 0.104 | ||||||||
| Index | 2 | 5.1 | 2 | 100.0 | 0 | 0.0 | 0 | 0.0 | |
| Long | 11 | 28.2 | 8 | 72.7 | 2 | 18.2 | 1 | 9.1 | |
| Ring | 9 | 23.1 | 3 | 33.3 | 6 | 66.7 | 0 | 0.0 | |
| Small | 1 | 2.6 | 0 | 0.0 | 0 | 0.0 | 1 | 100.0 | |
| Thumb | 16 | 41.0 | 9 | 56.3 | 4 | 25.0 | 3 | 18.8 | |
| Age (mean, SD) | 57.7, 9.3 | 54.7, 10.2 | 62.5, 6.5 | 58.8, 5.4 | 0.060 | ||||
| Symptom duration (mean, SD) | 2.5, 1.3 | 2.4, 1.2 | 3.0, 1.6 | 1.5, 0.4 | 0.062 | ||||
Note. Data were expressed as weighted number (n) and percent prevalence (%). Totals do not add up to 100% due to rounding or missing. P values were calculated by chi-squred tests or Fisher’s exact method, ANOVA or Kruskal-Wallis test.
Table 3.
Study Outcomes by the Three Approaches.
| All patients (N = 39) |
Palm (n = 22) |
Phalanx (n = 12) |
Webspace (n = 5) |
P value | |||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Repeated injection | 0.256 | ||||||||
| Yes | 18 | 46.2 | 8 | 44.4 | 8 | 44.4 | 2 | 11.1 | |
| No | 21 | 53.8 | 14 | 66.7 | 4 | 19.1 | 3 | 14.3 | |
| Surgery | 0.430 | ||||||||
| Yes | 22 | 56.4 | 14 | 63.6 | 5 | 22.7 | 3 | 13.6 | |
| No | 17 | 43.6 | 8 | 47.1 | 7 | 41.2 | 2 | 11.8 | |
| Result | 0.450 | ||||||||
| 1 | 1 | 2.6 | 0 | 0.0 | 1 | 100.0 | 0 | 0.0 | |
| 2 | 8 | 20.5 | 3 | 37.5 | 3 | 37.5 | 2 | 25.0 | |
| 3 | 15 | 38.5 | 8 | 53.3 | 5 | 33.3 | 2 | 13.3 | |
| 4 | 15 | 38.5 | 11 | 73.3 | 3 | 20.0 | 1 | 6.7 | |
| Pre-DASH score (mean, SD) | 24.5, 16.4 | 31.2, 16.4 | 18.7, 12.8 | 9.3, 8.6 | 0.006 | ||||
| Post-DASH score (mean, SD) | 23.8, 12.8 | 25.6, 11.6 | 21.5, 15.8 | 21.8, 11.1 | 0.664 | ||||
| VAS score (mean, SD) | 6.5, 2.5 | 6.6, 2.6 | 6.0, 2.8 | 6.8, 1.8 | 0.754 | ||||
Note. Data were expressed as weighted number (n) and percent prevalence (%). Totals do not add up to 100% due to rounding or missing. P values were calculated by chi-squred tests or Fisher’s exact method, ANOVA or Kruskal-Wallis test. DASH = Disabilities of the Arm, Shoulder, and Hand; VAS = visual analog scale.
Subgroup analysis was also performed, comparing thumbs with the lesser digits. In the thumbs, mean pre-injection DASH score was 21.6 (SD = 15.9), while mean post-injection DASH was 22.0 (SD = 14.8), and VAS scores following injection averaged 6.6 (SD = 2.4). In the lesser digits, mean pre-injection DASH score was 26.6 (SD = 16.9), while mean post-injection DASH was 24.0 (SD = 12.3), and VAS scores following injection averaged 6.3 (SD = 2.7).
Discussion
Stenosing tenosynovitis is a painful condition for which patients often seek medical treatment. Prior studies have demonstrated good outcomes with good cure rates with corticosteroid injections.3,4,5,9,10,11,14 Our results indicate that there is no significant difference between the VAS scores reported by patients following each of the 3 different injection approaches.
While it was not a primary goal of our study, we also demonstrated no difference in the efficacy of each of the 3 injection approaches. Because previous studies have demonstrated the lack of difference between injections given in the sheath and around the tendon sheath,13 it was not surprising that the efficacy of injection was not affected by approach utilized.
Prior studies have demonstrated highly variable success rates for a single corticosteroid injection. Our overall success rate, however, was lower than even the lowest published success rates of single-injection therapy, with only 33.3% (13 of 39 patients) of patients reporting an improvement or resolution of their symptoms. We surmise that this may be due to the type of steroid used, the small sample size, and the timing of follow-up.
Dexamethasone was the steroid utilized in this study. Ring et al12 concluded that while triamcinolone demonstrated improved early success rates over dexamethasone, the long-term results were in fact significantly better with dexamethasone. Because our follow-up period was relatively short, we may not have captured the true incidence of long-term resolution of symptoms, and either offered another injection or surgical intervention prematurely.
Alternatively, Wojahn et al14 studied the long-term outcomes of single injections for trigger digits and concluded that females with only one affected digit had the highest success rate, at 56%. Overall, the long-term cure rate of a single injection was 45%. With this analysis in mind, our results do not seem aberrant.
The strengths of our study include its prospective nature, use of a standardized and validated functional outcome scoring system (DASH), and standardizing the amount and type of steroid injected throughout each of the 3 different approaches.
The limitations of this study include its small size, relatively short period of follow-up, and lack of randomization or blinding. Furthermore, the injections were performed by 3 different surgeons, possibly introducing unobserved confounding factors. A larger randomized controlled trial may determine whether 1-injection approach results in less pain to patients than the others.
However, our data suggest that injection approach does not affect patient pain perception scores or outcomes. Based on our findings, we recommend that the technique which is most comfortable to the surgeon be utilized, with the understanding that 1 injection alone has a low likelihood of relieving symptoms.
Footnotes
Ethical Approval: This study was approved by the Biomedical Sciences institutional review board of The Ohio State University, Columbus, OH (2011H0274).
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Anderson B, Kaye S. Treatment of flexor tenosynovitis of the hand (“trigger finger”) with corticosteroids. A prospective study of the response to local injection. Arch Intern Med. 1991;151:153-156. [PubMed] [Google Scholar]
- 2. Fahey JJ, Bollinger JA. Trigger-finger in adults and children. J Bone Joint Surg Am. 1954;36-A:1200-1218. [PubMed] [Google Scholar]
- 3. Fleisch SB, Spindler KP, Lee DH. Corticosteroid injections in the treatment of trigger finger: a level I and II systematic review. J Am Acad Orthop Surg. 2007;15:166-171. [DOI] [PubMed] [Google Scholar]
- 4. Freiberg A, Mulholland RS, Levine R. Nonoperative treatment of trigger fingers and thumbs. J Hand Surg Am. 1989;14:553-558. [DOI] [PubMed] [Google Scholar]
- 5. Howard LD, Jr, Pratt DR, Bunnell S. The use of compound F (hydrocortone) in operative and non-operative conditions of the hand. J Bone Joint Surg Am. 1953;35-A:994-1002. [PubMed] [Google Scholar]
- 6. Hueston JT, Wilson WF. The aetiology of trigger finger explained on the basis of intratendinous architecture. Hand. 1972;4:257-260. [DOI] [PubMed] [Google Scholar]
- 7. Lorthioir J., Jr. Surgical treatment of trigger-finger by a subcutaneous method. J Bone Joint Surg Am. 1958;40-A:793-795. [PubMed] [Google Scholar]
- 8. Marks MR, Gunther SF. Efficacy of cortisone injection in treatment of trigger fingers and thumbs. J Hand Surg Am. 1989;14:722-727. [DOI] [PubMed] [Google Scholar]
- 9. Murphy D, Failla JM, Koniuch MP. Steroid versus placebo injection for trigger finger. J Hand Surg Am. 1995;20:628-631. [DOI] [PubMed] [Google Scholar]
- 10. Patel MR, Bassini L. Trigger fingers and thumb: when to splint, inject, or operate. J Hand Surg Am. 1992;17:110-113. [DOI] [PubMed] [Google Scholar]
- 11. Patel MR, Moradia VJ. Percutaneous release of trigger digit with and without cortisone injection. J Hand Surg Am. 1997;22:150-155. [DOI] [PubMed] [Google Scholar]
- 12. Ring D, Lozano-Calderon S, Shin R, et al. A prospective randomized controlled trial of injection of dexamethasone versus triamcinolone for idiopathic trigger finger. J Hand Surg Am. 2008;33:516-522; discussion 523-514. [DOI] [PubMed] [Google Scholar]
- 13. Taras JS, Raphael JS, Pan WT, et al. Corticosteroid injections for trigger digits: is intrasheath injection necessary? J Hand Surg Am. 1998;23:717-722. [DOI] [PubMed] [Google Scholar]
- 14. Wojahn RD, Foeger NC, Gelberman RH, et al. Long-term outcomes following a single corticosteroid injection for trigger finger. J Bone Joint Surg Am. 2014;96:1849-1854. [DOI] [PMC free article] [PubMed] [Google Scholar]