Abstract
Background:
Since the introduction of mobile phones, technology has been increasingly used to enable diabetes self-management education and support. This timely systematic review summarizes how currently available technology impacts outcomes for people living with diabetes.
Methods:
A systematic review of high quality review articles and meta analyses focused on utilizing technology in diabetes self-management education and support services was conducted. Articles were included if published between January 2013 and January 2017.
Results:
Twenty-five studies were included for analysis. The majority evaluated the use of mobile phones and secure messaging. Most studies described healthy eating, being active and metabolic monitoring as the predominant self-care behaviors evaluated. Eighteen of 25 reviews reported significant reduction in A1c as an outcome measure. Four key elements emerged as essential for improved A1c: (1) communication, (2) patient-generated health data, (3) education, and (4) feedback.
Conclusion:
Technology-enabled diabetes self-management solutions significantly improve A1c. The most effective interventions incorporated all the components of a technology-enabled self-management feedback loop that connected people with diabetes and their health care team using 2-way communication, analyzed patient-generated health data, tailored education, and individualized feedback. The evidence from this systematic review indicates that organizations, policy makers and payers should consider integrating these solutions in the design of diabetes self-management education and support services for population health and value-based care models. With the widespread adoption of mobile phones, digital health solutions that incorporate evidence-based, behaviorally designed interventions can improve the reach and access to diabetes self-management education and ongoing support.
Keywords: diabetes, diabetes self-care, digital health, education, self-management, technology
Diabetes is a chronic condition requiring ongoing self-management and support.1 Education and skill development for effective self-management is described in the United States National Standards (Standards) for Diabetes Self-Management Education and Support (DSMES).2 Self-management support is recognized as a key component in new, evolving models of care including patient-centered medical homes (PCMH), accountable care organizations (ACO), and population health programs.3,4,5 Health care payment methods are evolving from fee-for-service (per visit) to value-based systems where payment is based on clinical quality and costs.6
The use of technology in diabetes self-management education and support and management has expanded since the introduction of mobile technology with ubiquitous availability and adoption by all populations.7 These technologies provide a platform for the rapid development of person-centered interventions that support self-management beyond traditional computer, web-based programs, and underutilized traditional, institution-based, diabetes education programs. In this article, we refer to DSMES as the traditional, in-person, diabetes education programs following the Standards, including services that quality for Medicare reimbursement. We define diabetes self-management education and support as encompassing a wider definition of diabetes education, implemented by the health care team including diabetes educators, nurses, dietitians, health care providers, coaches, community health workers, and others that may or may not follow the Standards and may not be currently reimbursed.
Technology attributes that support the informed, activated patient and the prepared, proactive team to produce outcomes include a complete feedback loop.8 This feedback loop incorporates monitoring, interpretation of data, adjustment of treatment, and communication of tailored advice and repetition of the cycle as required elements.9 Diabetes self-management education and support incorporates analysis of patient-generated health data (PGHD) including structured glucose data, lifestyle data, and a structured feedback loop.10,11 The application of this feedback loop to chronic condition management is incorporated in the e-Health Enhanced Chronic Care Model.12
Many review articles have been published on the application of computer technology in health care. This growing body of knowledge includes the impact of technology-enabled self-management in diabetes. There is a need for a systematic review of recent articles to clarify the status of technology in diabetes self-management education and support. The Standards for DSMES2 and the American Association Diabetes Educators 7 Self-Care Behaviors© (AADE7)13 provide a context for evaluating the effectiveness of technology in people with type 1 and type 2 diabetes.
By systematically examining high quality published review articles this summary provides health care organizational decision makers with the current evidence to evaluate technology-enabled solutions for diabetes self-management education and support that address the Standards, evolving models of care and reimbursement, and appropriate behavioral frameworks.
Methods
The reviewers searched for English language documents published between 2011 and 2017. A medical librarian searched multiple databases using appropriate subject headings and text words related to technology, diabetes mellitus, self-management or self-care or patient education, and systematic reviews or meta-analysis following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)14 recommendations. See Figure 1 for the PRISMA flow diagram.
Figure 1.
PRISMA flow diagram. Study selection. Searched PubMed, Medline Complete, Academic Search Premier, Cumulative Index of Nursing and Allied Health Literature, Health Source: Nursing and Academics.
Sources and Searching
The electronic databases searched were Academic Search Premier, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Health Source: Nursing/Academic Edition, Medline Complete, and PubMed. The initial searches were completed in August 2016 and repeated in December 2016 to retrieve current literature. The team identified additional articles from references and hand searching.15 See Appendix A for the search strategy.
Duplicates Removed
After identifying duplicates, researchers screened abstracts from 265 articles specific to diabetes self-management or education interventions using technology. A total of 145 full-text articles met our criteria. Articles identified the impact of technology on diabetes self-management education and support; articles without measured outcomes were excluded. If technology was not a major focus of the article it was excluded. We included 25 articles for data extraction. Each full-text article was assigned to 2 reviewers for data extraction. When there was disagreement between the 2 reviewers, a third reviewer examined the article before inclusion.
Screening Criteria
Only high quality systematic reviews were eligible for inclusion; reviews lacking multiple elements of Assessing the Methodological Quality of Systematic Reviews (AMSTAR) methodological criteria16 were excluded. Our highest AMSTAR scores of 22 were given for the Pal17 study in the Cochrane Database and Kitsiou et al;18 the average AMSTAR score was 18 (range 22-11). The AMSTAR score rated each yes or exact match as a 2 for each AMSTAR question; a partial match scored as 1; for example, question 5 asks if a list of studies (included and excluded) was provided, we scored 1 when the included studies were listed in the bibliography and excluded studies were described by a simple count, a no or can’t answer evaluation received a zero score. Risk of bias in the selected reviews was assessed by using AMSTAR question 10. Most selected reviews (16/25, 64%) included graphical aids, such as a funnel plot or described the likelihood of publication bias in their reviews. See Appendix B for individual AMSTAR scores.
Studies of school site or classroom interventions were excluded. Studies that focused only on diabetes devices (eg, insulin pump, continuous glucose monitors) were excluded. The full-text articles from publications older than 2013 were removed from eligibility because they did not reflect current mobile phone technology. Twenty-five systematic reviews met our inclusion criteria. See Table 1 for the list of articles, by first author, AMSTAR scores, and study characteristics.
Table 1.
Selected Reviews With AMSTAR Scores, Number of Articles, Number of Research Participants, and Their Mean Age or Age Range (n = 25).
| Author | Date | AMSTAR total | No. articles | No. subjects | Mean age or range (years) |
|---|---|---|---|---|---|
| Alharbi | 2016 | 17 | 32 | 40 454 | NR |
| Amante | 2014 | 17 | 16 | 73 579 | 30-75+ |
| Anglada-Martinez | 2015 | 19 | 20 | 7402 | 1-80 |
| Bonoto | 2017 | 21 | 13 | 1263 | 13-62 |
| Connelly | 2013 | 17 | 15 | 4540 | 51-62 |
| Cui | 2016 | 17 | 13 | 1022 | 45-67 |
| El-Gayar | 2013 | 12 | 16 | NR | NR |
| Garabedian | 2015 | 12 | 20 | NR | NR |
| Greenwood | 2014 | 19 | 15 | 3744 | 47-71 |
| Hall | 2015 | 21 | 15 | 50 809 | NR |
| Hamine | 2015 | 11 | 107 | 7765 | NR |
| Harrison | 2014 | 17 | 26 | NR | 4-79 |
| Hou | 2016 | 19 | 14 | 1360 | 34-62 |
| Kitsiou | 2017 | 22 | 16 | 11 833 | NR |
| Kuo | 2016 | 14 | 11 | 43 538 | 4-79 |
| Nelson | 2016 | 13 | 24 | 3076 | 39-62 |
| Or | 2014 | 19 | 62 | NR | NR |
| Pal | 2013 | 22 | 20 | 3578 | 46-67 |
| Pereira | 2014 | 14 | 14 | 2802 | 25-75 |
| Peterson | 2014 | 17 | 14 | 422 | NR |
| Saffari | 2014 | 19 | 10 | 960 | 53 |
| Tao | 2013 | 19 | 43 | 6486 | 9-71 |
| Toma | 2014 | 20 | 34 | 4977 | 15-71 |
| Wu | 2017 | 21 | 12 | 974 | NR |
| Zhai | 2014 | 20 | 47 | 7688 | 43-71 |
Abbreviations: NR, not reported, not all the selected systematic reviews identified the total number of people living with diabetes who participated in the research, some reported the average number or range of participants and ages.
Results
The authors developed tables for data analysis with the type of diabetes addressed in the review article, the types of technology used for the intervention along with outcomes measured. The most common health outcome measure was hemoglobin A1c (A1c). This shared data element allowed comparison between the varying interventions addressed in these reviews.
Outcomes are listed in Table 2. Table 3 describes the intervention features and A1c change. Table 4 identifies the AADE7 self-care behaviors addressed by the reviews that are essential for diabetes self-management.13 Including other core data elements19 from the AADE7 self-care behaviors facilitated the generalizability of interventions.
Table 2.
Summary Table of Technology Used and Outcome Measures Reported in Included Reviews (n = 25).
| Author | Type of technology | Outcome measure |
|---|---|---|
| Alharbi | SP, tHealth, Web | A1c |
| Amante | SMS, Web | A1c +, BP, usage |
| Anglada-Martinez | SMS | Med |
| Bonoto | Apps | A1c +, BP, weight, QOL |
| Connelly | CD, C, SP, Text, Web | A1c |
| Cui | C, SMS, SP | A1c +, BP, weight |
| El-Gayar | Apps, C, EMR | A1c +, PA, |
| Garabedian | Apps, SMS, SP, tHealth WD | A1c, BP, usage |
| Greenwood | EMR, SMS, tHealth VC, Web | A1c |
| Hall | SMS, SP, Text | Comp, weight |
| Hamine | C, SMS, SP | A1c +, usage |
| Harrison | C, SMS | PS |
| Hou | Apps | A1c |
| Kitsiou | Apps, C, SP, SMS, Text, WD Web | A1c, PS, QOL, SE, weight |
| Kuo | EMR, SMS, WD | A1c +, BP |
| Nelson | Apps, SP, Text, Web | Usage |
| Or | Apps, C, SP | A1c +, QOL, weight |
| Pal | Apps, C, SP | A1c, SE |
| Pereira | Apps, EM, SP, Text, Web | A1c +, BP, EB, SE, PA |
| Peterson | Apps, SP, Web, VC | A1c |
| Saffari | SMS, Text, Web | A1c |
| Tao | Apps, C, tHealth, Web | A1c |
| Toma | EM, SM, SMS, SP, Web | A1c +, BP, PS |
| Wu | Apps | A1c |
| Zhai | EM, SP, VC, WD, Web | A1c |
Abbreviations: A1c, hemoglobin A1c; A1c +, hemoglobin A1c and other laboratory results; apps, mobile applications; BP, blood pressure; C, personal computers, laptops, personal digital assistants, tablet computers, touchscreen computers; CD, compact disks; COMP, complications; EB, eating behavior; EM, electronic mail; EMR, electronic medical records; Med, medication monitoring; PA, physical activity; PS, patient satisfaction; QOL, quality of life; SE, self-efficacy; SM, online social media; SMS, secure messaging system; SP, iPhones, smartphones, mobile phones; tHealth, tele-monitoring, telemedicine; Text, text message; VC, video conferencing; WD, wireless devices; Web, Internet, websites, portals.
Table 3.
Intervention Features of Studies With Significant A1c Outcomes (n = 18).
| Review | Intervention features | A1cc | |||
|---|---|---|---|---|---|
| Authora,b | Communication (1- or 2-way) | Patient-generated health data (tracking or analysis) | Education content (general or customized) | Feedback (automated or live) | |
| Garabedian | 2 | Analysis | Both | Automated | −0.8% decreased |
| Cui | 2 | Analysis | Both | Both | −0.4% diff |
| Alharbi | 2 | Both | Both | Both | −0.5% diff |
| Bonotob | 2 | Both | Both | Both | −0.4% diff P < .001 |
| Greenwood | 2 | Both | Both | Both | −0.2 to −1.2 rangee |
| Hou | 2 | Both | None | Both | −0.5% diff |
| Kuo | Both | Both | Both | Both | −0.5% diff |
| Palb | Both | Both | Both | Both | −0.2% diff P = .009 Mobile: −0.5% diff P < .00001 |
| Pereira | Both | Both | Both | Both | Significantf |
| Saffarib | Both | Both | Both | Both | −0.5% diff P < .001 SMS and Internet: −0.9% diff P < .001 |
| Taob | Both | Both | Both | Both | −0.3% diff P < .00001 Mobile: −0.4% diff. P < .00001 |
| Wu | Both | Both | Both | Both | −0.5% diff T2D: −0. 7% diff |
| Tomab | Both | Both | General | Both | −0.5% diff P < .00001 |
| Kitsiou | Both | Tracking | General | Both | T2D: 0.8% decreased
T1D: −0.3% decreased |
| Orb | Both | Tracking | General | Both | −0.3% decreased P < .001 |
| Zhaib | Both | Tracking | General | Both | −0.4% diff |
| Hamine | Both | Tracking | None | Live | 11/26 studiesg |
| Peterson | Both | Tracking | None | None | 7/15 studiesg
−0.6% to −0.8% rangee |
Abbreviations: Diff, difference-between intervention and control; SMS, text messaging; T1D, type 1 diabetes; T2D, type 2 diabetes.
Authors ordered from most features to least features.
Items signify a meta-analysis.
A1c was not reported consistently in reviews; P values are included if they were reported.
Decrease means there was a decrease in A1c reported.
Range refers to the range of A1c difference reported.
Significant means authors did not specify an A1c level.
Studies indicates the number of studies reporting significant A1C.
Table 4.
AADE7 Self-Care Behaviors Addressed by Technology (n = 25).
| Author | Healthy Eating | Being Active | Monitoring | Taking Medications | Reducing Risk | Problem Solving | Healthy Coping |
|---|---|---|---|---|---|---|---|
| Alharbi | X | ||||||
| Amante | X | X | |||||
| Anglada-Martinez | X | ||||||
| Bonoto | X | X | X | X | |||
| Connelly | X | X | |||||
| Cui | X | X | |||||
| El-Gayar | X | X | X | X | X | ||
| Garabedian | X | X | X | X | X | ||
| Greenwood | X | ||||||
| Hall | X | X | |||||
| Hamine | X | X | X | X | |||
| Harrison | X | X | X | X | |||
| Hou | |||||||
| Kitsiou | X | X | X | X | |||
| Kuo | X | X | |||||
| Nelson | X | X | X | X | |||
| Or | X | X | X | X | X | X | |
| Pal | X | X | X | X | X | X | |
| Pereira | X | X | X | X | X | ||
| Peterson | X | ||||||
| Saffari | X | X | X | X | |||
| Tao | X | X | X | X | X | ||
| Toma | X | X | X | X | X | X | |
| Wu | X | X | X | X | X | X | |
| Zhai | X | X | X | X |
Study Characteristics
Most of the selected reviews used research from locations around the globe. Three reviews included only US studies.20-22 The mean age range reported was from 1 to 80 years old. Nine studies did not report age ranges (see Table 1). Six studies reported on education, income, socioeconomic status, or ethnicity.23-28
Type of Diabetes
Most of the included studies included outcomes in type 1 and type 2 diabetes (15/25); 8 focused on type 2 diabetes. Type 1 diabetes outcomes were addressed in a review of a secure message service21 and one study22 did not specify the type of diabetes.
Outcomes Measured, Primary Focus
Twenty-two studies included A1c as an outcome. Two reviews studied medication adherence and other self-management behaviors without reporting A1c levels.29,30 Improvements in A1c were reported with reductions ranging from 0.1%31 to 0.8%.18 Table 3 shows the significant A1c outcomes reported as a decrease, a difference between intervention and control, or a range of values.
Other reported outcomes included patient satisfaction (4/25), self-efficacy (3/25) and engagement with technology (5/25). Many studies included blood pressure (7/25) and weight (6/25) along with other laboratory findings (9/25); 3 included healthy eating as an outcome 20,24,30 and 3 included quality of life measures.18,23,32 Complications, including foot health, screening exams and immunizations, were identified by Wu et al33 in their review. Smoking status was included in 2 reviews.28,29
In general, participants with type 2 diabetes improved A1c more than participants with type 1 diabetes.18,33-35 Incorporating multiple modalities, such as text messaging or other mobile interventions and web–based tools in combination, was more effective at improving outcomes compared to singular interventions.18,34,36
Type of Technology
Studies reviewed multiple types of technology (Table 2). Mobile phones (19/25) were the most frequently evaluated technology followed by secure messaging (12/25) and web-based information (12/25). Mobile phone applications were the primary technology of interest by Bonoto et al,23 Kitsiou et al,18 and Wu et al.33 Six other reviews included app technologies (9/25). Nine reviews included text messaging, 8 included wireless devices, 5 included electronic mail or video conferencing, and 4 reviews identified decision support or telehealth as one of the technologies for diabetes education. Three reviews included electronic medical records11,20,30 and one described social media technologies.34
Intervention Features
Four key concepts emerged during the analysis of the intervention features in the reviews: 2-way communication, PGHD analysis, education, and feedback (Table 3). These concepts support the complete feedback loop described by Jimison9 as essential for technology-enabled interventions. Nineteen of the 25 reviews described communication strategies that are 2-way between participant and health care team. Patient-generated health data were analyzed in Cui et al37 and Garabedian et al.22 Tracking of PGHD was described in 5 of the reviews.18,21,32,38,39 Tracking and analysis of the PGHD together were described in most these reviews (11/19, 58%) however, Saffari et al36 did not clarify how PGHD were used but concluded that interactive data sharing was more effective. Education was described in these reviews as either general or customized. Most of the reviews (11/19, 58%) described a combination of general and customized educational content. General diabetes self-management education only was described in 5 of the reviews.18,32,34,36 Generally speaking education was not well defined or reported. Two reviews reported on tailored education.11,35 Feedback to the participant was described in these reviews as either live38 (1/19), automated22 (1/19) or a combination of both (16/19, 84%). The type of feedback provided was not described by Peterson.21
Self-Management Behaviors
The AADE7 self-care behaviors13 provide a framework to identify essential behaviors for managing diabetes including healthy eating, being active, monitoring, taking medications, risk reduction, problem solving, and healthy coping. Technology-enabled self-management in the 25 studies reviewed addressed many of these behaviors, a few reviews did not identify specific behaviors but described the impact of the technologies on “lifestyle changes.”18 See Table 4.
Healthy eating was described as “eating,” diet, or nutrition in 19 of the reviews. Being active was described as exercise or physical activity (17/25). Monitoring was referred to as remote patient monitoring or self-monitoring of blood glucose (17/25). Medications were addressed by medication management in 15 of the reviews. Risk reduction included the concept of complications and was described in 5 reviews.24,32,33,36,40 Problem solving (7/25) was described in shared decision-making and communication between health care providers and participants for the purpose of changing medications. Healthy coping strategies (5/15), including peer support by others living with diabetes and stress management, were less frequently described.
Discussion
The intent of this systematic review was to identify and evaluate the results from high quality reviews and meta-analyses that measured the impact of technology-enabled diabetes self-management education and support. Our team employed rigorous methodologies to identify articles that demonstrate a significant reduction in A1c utilizing readily available technologies. There was extreme heterogeneity of the interventions and methodologies given this rapidly evolving field. However, this review demonstrates clear evidence that technology-enabled diabetes self-management education and support is effective in reducing A1c in the context of a complete feedback loop. In this review, few studies researched the critical self-management concepts of problem solving, reducing risk and healthy coping behaviors. Systematic reviews published prior to 2013 featured technologies and interventions that were less mature with minimal benefit on outcomes. More recent reviews demonstrating consistent and significant A1c reductions included the technology intervention components of the complete feedback loop between participants and the health care team.9
Technology-Enabled Self-Management (TES) Feedback Loop
Effective technology-enabled self-management is facilitated by the TES feedback loop between a person with diabetes and their health care team. The authors identified 4 key elements and defined the TES feedback loop that contributed to an improved A1c: (1) 2-way communication, (2) PGHD analysis, (3) education, and (4) feedback (see Figure 2).
Figure 2.
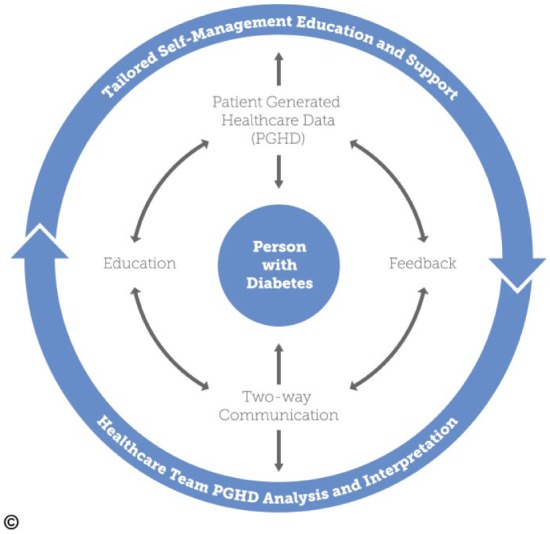
Technology-enabled self-management (TES) feedback loop.
Communication
Communication, in this article, is defined as a 2-way communication where both sender and receiver are engaged, facilitated by way of technology. Jimison9 noted that 1-way communication had no impact on participant outcomes. One-way communication typically consisted of personalized educational materials.21,33,35,37 Most of the reviews described 2-way communication strategies. In the review by Peterson21 focusing on type 1 diabetes, 2-way communication improved A1c in 12/14 studies. Greenwood11 documented that 10/15 studies described an interactive communication process between participants and providers using problem solving and shared decision-making strategies. Nelson27 and Toma34 concluded that direct communication with health care providers improved outcomes and facilitated engagement. Several reviews identified the value of communication and feedback together.23,24,34,36,38 Bonoto23 determined that mobile apps have better outcomes when communication is possible with the health care team. Several studies determined that mobile communication resulted in greater improvement in A1c compared to web-based interventions.17,18,21,26,38,40 One finding in a recent descriptive study concluded that participants may need training in how to best construct appropriate messages to their health care team to engage in 2-way communication.41
Patient-Generated Health Data
Patient-generated health data may include glucose and other biometric health data, lifestyle choices, symptoms and other information created, recorded and shared by the participant. However, simply tracking PGHD is not sufficient; data need to be analyzed for patterns and trends in relation to the individual participant and these data need to be interpreted and shared with the participant in a meaningful way to change the plan of care.9,42 Studies show improved A1c when participants document their own health data, review data online and in real-time.17,22,34,36,38 The generation of structured glucose data (e.g., 3-day profile, checking in pairs, etc) is required to analyze glucose data in a meaningful way and provide actionable feedback.11,42 The review by Greenwood11 identified 7 studies that described complex systems to analyze data and were associated with significant improvement in A1c whether through automated algorithms or by skilled health care providers.
Health care teams are exposed to an overload of data and may not be equipped to analyze and verify the submitted PGHD or provide feedback when large volumes of content are received.43 Systems that analyze PGHD will relieve some of the health care team burden as technology evolves. In addition, people with diabetes may need education or training on how to effectively transmit PGHD to the health care team.12
Education
Education is defined as diabetes self-management education and support addressing one or more of the AADE7 self-care behaviors.44 According to Ceriello et al42 education is the initial process in personalized care management for the person with diabetes. Education from the health care team often triggers the TES feedback loop. The person with diabetes assimilates the provided education into their own self-management plan then sends PGHD back to the health care team for analysis and interpretation. Finally, customized and tailored education, applying the AADE7 self-care behaviors, can be transmitted back to the person with diabetes thus completing a cycle of the feedback loop. Importantly, this customized education should be based on the interpretation of PGHD to provide tailored and targeted content to the individual and their unique circumstances.20,33,37 Using technology to deliver general education content, for example, 1-way text messaging, may be less effective because it may appear irrelevant to the participant and may not follow the self-management goals or plan of care.9 In general, the concept of education is the least well defined and reported concept in the reviews.
Feedback
Feedback is the essential component to complete the feedback loop. Feedback must be individualized and specifically target the PGHD and communications. Feedback may be live or automated based on algorithms evaluating PGHD. Some research indicates that asynchronous feedback—data transfer that takes place in separate time frames, not simultaneously—may be more productive as it allows the participant to consider the exchange of data, information and knowledge without the influence of their current circumstances or environmental factors in a “controllable and less stressful” environment compared to traditional face-to-face patient-provider communications.45 Pereira24 noted that asynchronous communication was positive for participants as it provided time to process, learn and respond. Significant A1c improvement is associated with individualized, personalized and tailored feedback, whether through automated algorithms or health care teams.11,36,40,46 Several studies noted an improvement in A1c specifically when PGHD were incorporated11,18,22,23 and when feedback was in real time.11,22,34,38 Feedback is critical to the success of the TES feedback loop. Notably, Cui37 in a meta-analysis showed studies without feedback were not statistically significant. The TES feedback loop is a continuous process, evolving over time, and potentially improving as more data are available to analyze.
Limitations
This review has limitations. In the meta-analysis by Pal,17 11 studies had nonsignificant differences in A1c, and overall only demonstrated a small significant A1c difference of −0.2%; however, studies focused on mobile phones showed a −0.5% difference. We did not conduct a meta-analysis, however, in a large meta-analysis of 111 randomized clinical trials published after this systematic review was completed, Faruque47 confirmed the significant A1c reductions ranging from −0.57% at 3 months to −0.26% at 12 months. Several reviews did not include A1c as an outcome. Multiple studies indicated that although there were significant differences in A1c reduction between groups, individuals on average did not attain an A1c less than 7%.23 This review did not include studies of diabetes devices including insulin pumps and continuous glucose monitors due to the lack of mobile integration into practice.
Implications for Practice
This review demonstrated that utilizing technology-enabled diabetes self-management education and support solutions significantly impacts health outcomes. Solutions with a TES feedback loop offer the greatest impact on A1c outcomes. In the evolving health care environment (eg, ACOs, PCMH, etc) organizations, payers, and health care teams, making decisions regarding incorporating technology-enabled diabetes self-management education and support solutions, should assess for inclusion of the 4 key features of the TES feedback loop. Entities that provide in-person DSMES services should consider finding cost-effective ways to incorporate technology-enabled solutions as part of their existing services to afford individualized ongoing support, monitoring of participant progress, and to provide data for improving quality of care and population health management. Diabetes self-management education and support services are required during 4 key times—at diagnosis, during an annual assessment by a health care provider, when complicating factors arise, and during transitions in care.44 Technology-enabled self-management solutions will facilitate engagement at these key times by reducing barriers of travel time and cost, time away from work or family, and timely engagement following hospitalizations. Interestingly, several studies18,33-35 found interventions utilizing technology improved A1c levels more in people with type 2 diabetes compared to type 1 diabetes. This may be due to a variety of factors ranging from higher initial A1c levels, less familiarity with glucose monitoring and the associated therapeutics and perhaps less experience with self-management resulting in greater opportunities for improvement. Smartphones are rapidly being adopted worldwide by people of all socioeconomic and ethnic backgrounds.48 Hispanics and Latinos are adopting use of mobile phones more rapidly than other ethnic groups in the United States.49 The technologies identified in this review were primarily mobile phones that use apps and text or SMS messaging. We can conclude that those typically affected by the “digital divide” with limited access to technologies due to economic, social, or geographic inequalities, may have greater access to these proven health interventions. The expanding smartphone market will enable the incorporation of other data sets not typically included in health records including GPS location, websites visited, purchasing history, the Internet of things and others for the development and implementation of individualized and precision health care. Privacy and security of data will be a consideration as new technologies are incorporated. Health care providers can expand their reach and access to diabetes self-management education and support services with the inclusion of technology-enabled models of care into practice. Technology solutions have the potential to enhance the previously demonstrated significant 0.6% A1c improvement with traditional DSMES programs.50
Chronic conditions involve complex treatment regimens requiring long term health care tasks by the person with diabetes including medication taking, lifestyle changes, self-monitoring, significant paperwork to be completed, learning about reimbursement rules and more.51 The minimally disruptive medicine (MDM) care model is a person-centric approach focusing on helping the person with chronic illness achieve their goals and improve health while decreasing the burden of treatment.52 Health care teams caring for people with diabetes should incorporate technologies that focus on decreasing the burden of treatment and the “new proactive work of re-engineered patient-hood” by integrating the tenants of MDM.52 Technology solutions should not add more work and burden for the person with diabetes, but through data analysis and feedback, lighten the cognitive load.51 Caregivers and people with diabetes have greater access to PGHD via apps to support the individual and partner with the health care team. Organizational and professional associations developing protocols, guidelines and standards of care can substantiate and recommend that technology solutions incorporating the TES feedback loop be incorporated in the health care plan to increase access to diabetes self-management education and support and to improve A1c. A formal evaluation process for apps and technology solutions may be needed to help consumers, health care providers, and health systems make decisions on optimal solutions based on published outcomes and system needs. The evidence supports the need for regulatory policy makers to incorporate reimbursement for technology-enabled diabetes self-management education and support services. Effective technology solutions must be designed with the TES feedback loop to integrate into the clinician workflow and improve efficiencies to provide the health care team with information for decision-making in the most cost-effective manner for both the person with diabetes and the team.
Need for Additional Research
Although there has been tremendous progress in the use of technology in diabetes self-management education and support, there remains a lack of empirical knowledge on how to integrate technology into the daily life of the person with diabetes, and into the workflow of health care team and in new models of care. It is imperative that new technologies are designed with a TES feedback loop to optimize participant-health care team communication, facilitate the analysis of PGHD and support decision making. Kulzer and colleagues53 are currently conducting clinical trials in primary care clinics with a personalized diabetes management (PDM) cycle focusing on self-management education and structured blood glucose monitoring. Although not focusing on remote management, the use of software to upload and analyze PGHD may provide valuable support for elements of the TES feedback loop, specifically PGHD analysis and feedback. The outcomes of the PDM research will help inform future analysis of the elements of the TES feedback loop.
Studies in populations of nonwhite, older adult, male gender, and non-English-speaking cohorts, as well as caregivers of people with diabetes are needed. Understanding how technology can enhance care and self-management education and support for people with disabilities (cognition, vision, hearing, etc) presents another platform for exploration. Focusing on the cost effectiveness of these new models, relative access, and ongoing engagement will provide decision makers with evidence for adopting these technologies. Researchers need to adopt iterative and adaptive designs and evaluation processes since technology advances faster than traditional randomized controlled trials can be conducted and published.54
In addition, these new technologies need to integrate a behavior change, theory-based foundation in their core design. Evaluating the concepts of problem solving, reducing risk and healthy coping will highlight the features of mobile technology that enhance daily decision making. High-quality research of new apps or technologies with TES attributes will be imperative to see real improvements in health outcomes. Research on the use of technology-enabled diabetes self-management education and support, incorporating all features of the TES feedback loop, is required to determine the nuances of the key elements and to identify the minimal level of engagement by the person with diabetes that creates the biggest improvements in A1c. Of importance is to design and test technology-enabled solutions that reduce the work of chronic disease management while increasing the ability of the person with diabetes to engage in self-management or the “work of being a patient,” and not add an additional burden of treatment to an already challenging condition.52 The goal is to make life easier for people with diabetes, make work easier for the health care team, improve outcomes, and reduce costs for all.
Conclusion
Technology-enabled diabetes self-management solutions improve A1c. The most effective interventions incorporated all TES feedback loop components that connected people with diabetes and their health care team using 2-way communication, analyzed PGHD, tailored education, and individualized feedback. The evidence suggests that organizations, diabetes educators, policy makers, and payers should consider these solutions in the design of diabetes self-management education and support services for population health and value-based care models. With the widespread adoption of mobile phones, digital health solutions that incorporate evidence-based, behaviorally designed interventions can improve the reach of and access to diabetes self-management education and ongoing support.
Acknowledgments
This review was informed by the 2016 AADE Technology Workgroup, of which PMG and MP were co-chairs and DAG was a member. KJF searched the literature and provided methodological and writing support for the review.
Appendix A
PubMed Search
(((“Diabetes Mellitus/self-management education and support”[Majr] OR “Diabetes Mellitus/prevention and control”[Majr]) OR diabetes[ti]) AND (“self care”[mesh] OR self care[tiab] OR “self concept”[mesh] OR self concept[tiab] OR “disease management”[mesh] OR ((“disease”[MeSH Terms] OR “disease”[All Fields]) AND management[tiab]) OR “behavior and behavior mechanisms” [mesh] OR behavior and behavior mechanisms[tiab])) AND ((“Biomedical technology”[majr] OR biomedical technology[tiab] OR “mobile applications”[majr] OR mobile applications[tiab] OR “technology”[majr] OR technology[tiab] OR “telemedicine”[majr] OR telemedicine[tiab] OR “technology assessment, biomedical”[majr] OR biomedical technology assessment[tiab]) OR (apps[tiab] OR digital health[tiab] OR eHealth[tiab] OR e-health[tiab] OR health policy[tiab] OR health technology[tiab] OR mHealth[tiab] OR m-health[tiab] OR mobile health[tiab] OR patient portals[tiab] OR personal health records[tiab] OR public health informatics[tiab] OR remote consultation[tiab] OR remote sensing technology[tiab] OR sensor technology[tiab] OR short message service[tiab] OR software[tiab] OR teleconsulting[tiab] OR telehealth[tiab] OR telerehabilitation[tiab] OR text messaging[tiab] OR wearable[tiab] OR wireless technology[tiab])) AND (Review[ptyp] AND (“2011/01/01”[PDAT] : “2017/12/31”[PDAT]) AND English[lang])
EBSCOHost Search Details
Searched on Academic Search Premier, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Health Source: Nursing/Academic Edition, and Medline Complete (diabetes mellitus OR diabetes) AND (self management or self care or patient self-management education and support) AND (technology OR biotechnology OR telemedicine) AND (systematic review or meta-analysis) Limiters—Published Date: 20110101-20161231 Language: English
Appendix B
Amstar Scores
| Author | Date | Amstar1 | Amstar2 | Amstar3 | Amstar4 | Amstar5 | Amstar6 | Amstar7 | Amstar8 | Amstar9 | Amstar10 | Amstar11 | AmstarTOTAL |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Alharbi | 2016 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 0 | 0 | 0 | 13 |
| Amante | 2014 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 0 | 2 | 17 |
| Anglada-Martinez | 2015 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 19 |
| Bonoto | 2017 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 21 |
| Connelly | 2013 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 17 |
| Cui | 2016 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 17 |
| El-Gayar | 2013 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 12 |
| Garabedian wood | 2015 | 2 | 0 | 1 | 0 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 12 |
| Greenwood | 2014 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 2 | 19 |
| Hall | 2015 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 21 |
| Hamine | 2015 | 2 | 2 | 2 | 0 | 1 | 2 | 0 | 0 | 0 | 0 | 2 | 11 |
| Harrison | 2014 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 1 | 0 | 2 | 16 |
| Hou | 2016 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 19 |
| Kitsiou | 2017 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 22 |
| Kuo | 2016 | 2 | 0 | 1 | 2 | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 14 |
| Nelson | 2016 | 2 | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 1 | 2 | 13 |
| Or | 2014 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 19 |
| Pal | 2013 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 22 |
| Pereira | 2014 | 2 | 1 | 2 | 0 | 1 | 2 | 1 | 1 | 1 | 1 | 2 | 14 |
| Peterson | 2014 | 2 | 0 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 17 |
| Saffari | 2014 | 2 | 2 | 2 | 0 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 19 |
| Tao | 2013 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 19 |
| Toma | 2014 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 20 |
| Wu | 2017 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 21 |
| Zhai | 2014 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 20 |
Footnotes
Abbreviations: A1c +, hemoglobin A1c and other laboratory results; AMSTAR, Assessing the Methodological Quality of Systematic Reviews; apps, mobile applications; BP, blood pressure; C, personal computers, laptops, personal digital assistants, tablet computers, touchscreen computers; CD, compact disks; CFL, complete feedback loop; COMP, complications; diff, difference; DSMES, diabetes self-management and education support; PDM, personalized diabetes management; PGHD, patient-generated health data; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; QOL, quality of life; SE, self-efficacy; SM, online social media; SMS, secure messaging system; SP, iPhones, smartphones, mobile phones; Standards, National Standards for Diabetes Self-Management Education and Support; TES, technology-enabled self-management; t-Health, telemonitoring, telemedicine; T2D, type 2 diabetes; VC, video conferencing; WD, wireless devices.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: DAG and MP are past presidents of AADE. MP is employed and DAG consults in digital health. PMG and KJF have no disclosures.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This article was partially funded by the American Association of Diabetes Educators.
References
*Article included in the review of reviews.
- 1. American Diabetes Association. Promoting health and reducing disparities in populations. Diabetes Care. 2017;40(suppl 1):S6-S10. [DOI] [PubMed] [Google Scholar]
- 2. Haas L, Maryniuk M, Beck J, et al. National standards for diabetes self-management education and support. Diabetes Educ. 2012;38(5):619-629. [DOI] [PubMed] [Google Scholar]
- 3. Knox L, Brach C, Schaefer J. Primary care practice facilitation curriculum (Module 32). AHRQ Publication No. 15-0060-EF, September 2015. Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- 4. Beebe CA, Schmitt S. Engaging patients in education for self-management in an accountable care environment. Clinical Diabetes. 2011;29(3):123-126. [Google Scholar]
- 5. Grady PA, Gough LL. Self-management: a comprehensive approach to management of chronic conditions. Am J Public Health. 2014;104(8):e25-e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. National Institute of Diabetes and Digestive and Kidney Diseases. Changing landscape: From fee-for-service to value-based reimbursement. Available at: https://www.niddk.nih.gov/health-information/health-communication-programs/ndep/health-care-professionals/practice-transformation/why-transform/changing-landscape/Pages/default.aspx. Accessed May 2, 2017.
- 7. Pew Research Center. Mobile fact sheet. Available at: http://www.pewinternet.org/fact-sheet/mobile/. Accessed May 2, 2017.
- 8. Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74(4):511-544. [PubMed] [Google Scholar]
- 9. Jimison H, Gorman P, Woods S, et al. Barriers and drivers of health information technology use for the elderly, chronically ill, and underserved. Evid Rep Technol Assess (Full Rep). 2008;175:1-1422. [PMC free article] [PubMed] [Google Scholar]
- 10. Ceriello A, Barkai L, Christiansen JS, et al. Diabetes as a case study of chronic disease management with a personalized approach: the role of a structured feedback loop. Diabetes Res Clin Pract. 2012;98(1):5-10. [DOI] [PubMed] [Google Scholar]
- 11. *Greenwood DA, Young HM, Quinn CC. Telehealth remote monitoring systematic review: structured self-monitoring of blood glucose and impact on A1C. J Diabetes Sci Technol. 2014;8(2):378-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gee PM, Greenwood DA, Paterniti DA, Ward D, Miller LMS. The eHealth enhanced chronic care model: a theory derivation approach. J Med Internet Res. 2015;17(4):e86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tomky D, Cypress M. AADE7 Self-care behaviors, AADE position statement. Diabetes Educ. 2008;34(3):445-449. [DOI] [PubMed] [Google Scholar]
- 14. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS MED. 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. *Pal K, Eastwood SV, Michie S, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2013;3:CD008776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. *Kitsiou S, Paré G, Jaana M, Gerber B. Effectiveness of mHealth interventions for patients with diabetes: an overview of systematic reviews. PLOS ONE. 2017;12(3):e0173160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Moore SM, Schiffman R, Waldrop-Valverde D, et al. Recommendations of common data elements to advance the science of self-management of chronic conditions. J Nurs Scholarsh. 2016;48(5):437-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. *El-Gayar O, Timsina P, Nawar N, Eid W. Mobile applications for diabetes self-management: status and potential. J Diabetes Sci Technol. 2013;7(1):247-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. *Peterson A. Improving type 1 diabetes management with mobile tools: a systematic review. J Diabetes Sci Technol. 2014;8(4):859-864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. *Garabedian LF, Ross-Degnan D, Wharam JF. Mobile phone and smartphone technologies for diabetes care and self-management. Curr Diab Rep. 2015;15(12):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. *Bonoto BC, de Araújo VE, Godói IP, et al. Efficacy of mobile apps to support the care of patients with diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2017;5(3):e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. *Pereira K, Phillips B, Johnson C, Vorderstrasse A. Internet delivered diabetes self-management education: a review. Diabetes Technol Ther. 2015;17(1):55-63. [DOI] [PubMed] [Google Scholar]
- 25. *Anglada-Martinez H, Riu-Viladoms G, Martin-Conde M, Rovira-Illamola M, Sotoca-Momblona JM, Codina-Jane C. Does mHealth increase adherence to medication? Results of a systematic review. Int J Clin Pract. 2015;69(1):9-32. [DOI] [PubMed] [Google Scholar]
- 26. *Kuo A, Dang S. Secure messaging in electronic health records and its impact on diabetes clinical outcomes: a systematic review. Telemed J E Health. 2016;22(9):769-777. [DOI] [PubMed] [Google Scholar]
- 27. *Nelson LA, Coston TD, Cherrington AL, Osborn CY. Patterns of user engagement with mobile- and web-delivered self-care interventions for adults with T2DM: a review of the literature. Curr Diab Rep. 2016;16(7):66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. *Amante DJ, Hogan TP, Pagoto SL, English TM. A systematic review of electronic portal usage among patients with diabetes. Diabetes Technol Ther. 2014;16(11):784-793. [DOI] [PubMed] [Google Scholar]
- 29. *Hall AK, Cole-Lewis H, Bernhardt JM. Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health. 2015;36:393-415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. *Harrison S, Stadler M, Ismail K, Amiel S, Herrmann-Werner A. Are patients with diabetes mellitus satisfied with technologies used to assist with diabetes management and coping? A structured review. Diabetes Technol Ther. 2014;16(11):771-783. [DOI] [PubMed] [Google Scholar]
- 31. *Connelly J, Kirk A, Masthoff J, MacRury S. The use of technology to promote physical activity in type 2 diabetes management: a systematic review. Diabet Med. 2013;30(12):1420-1432. [DOI] [PubMed] [Google Scholar]
- 32. *Or CKL, Tao D. Does the use of consumer health information technology improve outcomes in the patient self-management of diabetes? A meta-analysis and narrative review of randomized controlled trials. Int J Med Inform. 2014;83(5):320-329. [DOI] [PubMed] [Google Scholar]
- 33. *Wu Y, Yao X, Vespasiani G, et al. Mobile app-based interventions to support diabetes self-management: a systematic review of randomized controlled trials to identify functions associated with glycemic efficacy. JMIR Mhealth Uhealth. 2017;5(3):e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. *Toma T, Athanasiou T, Harling L, Darzi A, Ashrafian H. Online social networking services in the management of patients with diabetes mellitus: systematic review and meta-analysis of randomised controlled trials. Diabetes Res Clin Pract. 2014;106(2):200-211. [DOI] [PubMed] [Google Scholar]
- 35. *Alharbi NS, Alsubki N, Jones S, Khunti K, Munro N, de Lusignan S. Impact of information technology–based interventions for type 2 diabetes mellitus on glycemic control: a systematic review and meta-analysis. J Med Internet Res. 2016;18(11):e310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. *Saffari M, Ghanizadeh G, Koenig HG. Health education via mobile text messaging for glycemic control in adults with type 2 diabetes: a systematic review and meta-analysis. Prim Care Diabetes. 2014;8(4):275-285. [DOI] [PubMed] [Google Scholar]
- 37. *Cui M, Wu X, Mao J, Wang X, Nie M. Type 2 diabetes self-management via smartphone applications: a systematic review and meta-analysis. PLOS ONE. 2016;11(11):e0166718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. *Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. *Zhai Y, Zhu W, Cai Y, Sun D, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine (Baltimore). 2014;93(28):e312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. *Tao D, Or CK. Effects of self-management health information technology on glycaemic control for patients with diabetes: a meta-analysis of randomized controlled trials. J Telemed Telecare. 2013;19(3):133-143. [DOI] [PubMed] [Google Scholar]
- 41. Gee PM, Paterniti DA, Ward D, Soederberg Miller LM. e-Patients perceptions of using personal health records for self-management support of chronic illness. Comput Inform Nurs. 2015;33(6):229-237. [DOI] [PubMed] [Google Scholar]
- 42. Ceriello A, Barkai L, Christiansen JS, et al. Diabetes as a case study of chronic disease management with a personalized approach: the role of a structured feedback loop. Diabetes Res Clin Pract. 2012;98(1):5-10. [DOI] [PubMed] [Google Scholar]
- 43. Deering MJ, Siminerio E, Seinstein S. Issue Brief: Patient-generated health data and health IT. Office of the National Coordinator for Health Information Technology; 2013. Available at: https://www.healthit.gov/policy-researchers-implementers/patient-generated-health-data. Assessed May 2, 2017.
- 44. Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Educ. 2015;41(4):417-430. [DOI] [PubMed] [Google Scholar]
- 45. Wright KB. Increasing computer-mediated social support. In: Parker JC, Thorson E, eds. Health Communication in the New Media Landscape. New York, NY: Springer; 2009:243-266. [Google Scholar]
- 46. *Hou C, Carter B, Hewitt J, Francisa T, Mayor S. Do mobile phone applications improve glycemic control (HbA1c) in the self-management of diabetes? A systematic review, meta-analysis, and GRADE of 14 randomized trials. Diabetes Care. 2016;39(11):2089-2095. [DOI] [PubMed] [Google Scholar]
- 47. Faruque LI, Wiebe N, Ehteshami-Afshar A, et al. Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. Can Med Assoc J. 2017;189(9):E341-E364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Anderson M. Technology device ownership: 2015. Pew Research Center; 2015. Available at: http://www.pewinternet.org/2015/10/29/technology-device-ownership-2015/. Accessed May 2, 2017.
- 49. Lopez MH, Gonzalez-Barera A, Patten E. Closing the digital divide: Latinos and technology adoption. Washington, DC: Pew Hispanic Center; 2013. Available at: http://www.pewhispanic.org/2013/03/07/closing-the-digital-divide-latinos-and-technology-adoption/. Accessed May 2, 2017.
- 50. Chrvala CA, Sherr D, Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient Educ Couns. 2016;99(6):926-943. [DOI] [PubMed] [Google Scholar]
- 51. Tran V-T, Barnes C, Montori VM, Falissard B, Ravaud P. Taxonomy of the burden of treatment: A multi-country web-based qualitative study of patients with chronic conditions. BMC Medicine. 2015;13(1). Available at: http://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-015-0356-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. May CR, Eton DT, Boehmer K, et al. Rethinking the patient: using burden of treatment theory to understand the changing dynamics of illness. BMC Health Serv Res. 2014;14:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kulzer K, Daenschel W, Daenschel I, et al. Integrated personalized diabetes management (PDM): design of the provalue studies: prospective, cluster-randomized, controlled, intervention trials for evaluation of the effectiveness and benefit of PDM in patients with insulin-treated type 2 diabetes. J Diabetes Sci Technol. 2016;10(3):772-781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Methodology Center. Overview of MOST. University Park: Pennsylvania State University; Available at: https://methodology.psu.edu/ra/most/research. Accessed May 2, 2017. [Google Scholar]



