In addition to direct patient contact, residents are responsible for communication, order entry, data review, and documentation. With more patient care being facilitated through computer today, there is increasing concern that little time remains for direct patient contact and education.1 Electronic health record (EHR) audit reports can provide granular information about workflows, and are being increasingly used to investigate trainee practices.2 Herein, we examine resident behavior on an inpatient general medicine service to describe how trainees use the EHR system as residents balance education and patient care.
Methods
Our institution uses the EPIC EHR system. In March 2015 we retrospectively analyzed all time-stamped electronic actions logged between June 25, 2013 and June 29, 2014, by internal medicine house staff at a large academic university hospital by institutional EHR audit. Actions corresponded to behaviors performed on the EHR, recording activities as clinicians move through various parts of the medical chart. These included, but were not limited to, reviewing medical charts, placing orders, accessing laboratory results, and generating notes. Data were extracted with our institutional informatics platform3 and linked with residency scheduling information. Bedside computers are reserved for nursing duties while physician workstations are located in separate workrooms. This study was reviewed and approved by the Stanford Administrative Panel on Human Subjects in Medical Research.
Consecutive actions were considered part of a single computer session if they were separated by less than 5 minutes of inactivity. Because patient information is updated through EHR sign-out during transitions of care, total working time was calculated as the difference between the first and last action recorded each day. Data processing was performed with Python software, version 2.7, and R, version 2.13. P values for numerical and count data were calculated by 2-tailed t tests and Fisher exact tests, respectively, with significance thresholds of .05.
Results
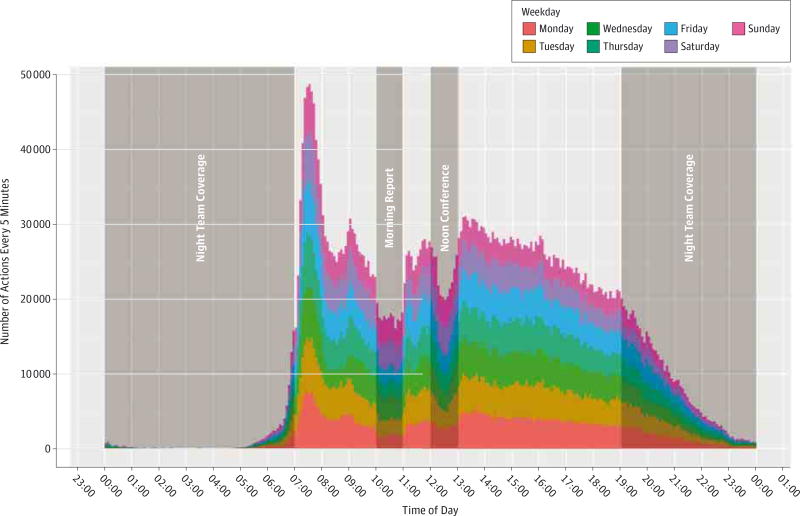
We analyzed 4 327 708 unique actions performed by 91 residents on the inpatient general medicine service. Peak activity occurred in the morning with decreases corresponding to teaching conferences (Figure). House staff worked a median (interquartile range [IQR]) of 69.2 (IQR, 56.9–79.3) hours each week; 4.2 hours (IQR, 2.9–5.5 hours) of total working time (36%) (IQR, 28.4%–43.2% of time) was spent using the EHR system per day. House staff reviewed a median of 14 patient medical charts (IQR, 10–21 charts) and had a median of 31 independent sessions (IQR, 23–38 sessions). Medical chart review accounted for most EHR activity (Table).
Figure. Electronic Health Record Activity for General Medicine Inpatient Residents.
On the general medicine service, residents receive sign-out at 7 AM, morning report is scheduled for 10 to 11 AM, and the remaining morning hours are dedicated to rounds and patient care.
Table.
Summary Statistics for General Medicine Inpatient EHR Usea
| Variable | PGY-1 Interns (n = 46) |
PGY-2/3 Residents (n = 45) |
|---|---|---|
| Hours per week, median (IQR) | 67.2 (55.3–76.4) | 73.5 (62.2–84.2) |
| EHR of total working time, median (IQR) | 36.5 (29.2–43.7) | 34.7 (26.7–42.0) |
| Patient medical charts per day, median (IQR) | 11.9 (7.0–14.0) | 25.8 (15.0–32.0) |
| Independent sessions per day, median (IQR) | 30.5 (23.0–38.0) | 29.4 (23.0–37.0) |
| EHR action/access type, No. (%) | ||
| Medical chart review | 1 142 893 (40.8) | 699 444 (42.5) |
| Notes | 263 289 (9.4) | 116 208 (7.1) |
| Patient list review | 150 377 (5.4) | 152 791 (9.3) |
| Results review | 151 556 (5.4) | 97 069 (5.9) |
| Order entry | 99 087 (3.5) | 40 896 (2.5) |
Abbreviations: EHR, electronic health record; IQR, interquartile range; PGY, postgraduate year.
P < .001 for all comparisons except for independent sessions per day (P = .005).
Discussion
Studies performed before EHRs suggest a longstanding imbalance between indirect and face-to-face patient care.4 However, today’s EHR systems commonly feature time-saving tools that have eliminated daily transcription of vital signs, laboratory values, and medications. Using electronic audits to analyze EHR use, we show that residents continue to spend more than a third of their time on indirect patient care. Our results are consistent with those of prior efforts to quantify indirect patient care5 and show that medical chart review accounted for most activity.
The distribution of activity is noteworthy, with morning peaks occurring when house staff have traditionally examined patients and communicated face-to-face. This supports anecdotal observations that the traditional model of gathering overnight updates at the bedside has evolved into electronic “prerounding.”1 While computer use decreased during teaching conferences, the persistent level of activity high-lights the balance between education and patient care. Of note, this study was limited to a single specialty at 1 institution without direct observation.
Responsibility for larger volumes of information, new documentation requirements, and poor user-interfaces could be contributing to increased EHR activity, highlighting opportunities to streamline workflow and directions for future study. As the role of EHRs increase, training programs should be aware of how EHRs might affect resident responsibilities and learning opportunities.
Acknowledgments
Funding/Support: Dr Chen is supported in part by VA Office of Academic Affiliations and Health Services Research and Development Service Research funds. The Stanford Translational Research Integrated Database Environment (STRIDE) project described was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant UL1 RR025744.
Footnotes
Author Contributions: Dr Ouyang had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: All authors.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Ouyang, Chi.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Ouyang, Chen,
Administrative, technical, or material support: Chen, Hom.
Study supervision: Hom, Chi.
Conflict of Interest Disclosures: None reported.
Disclaimer: Content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, VA, or Stanford Healthcare.
Additional Contribution: Patient data were extracted and deidentified by Gomathi Krishnan, PhD, of the STRIDE project, a research and development project at Stanford University to create a standards-based informatics platform supporting clinical and translational research. She was not compensated for her contributions.
Contributor Information
David Ouyang, Department of Internal Medicine, Stanford University School of Medicine, Stanford, California.
Jonathan H. Chen, Center for Innovation to Implementation (Ci2i), Veterans Affairs Palo Alto Health Care System, Palo Alto, California.
Jason Hom, Department of Internal Medicine, Stanford University School of Medicine, Stanford, California.
Jeffrey Chi, Department of Internal Medicine, Stanford University School of Medicine, Stanford, California.
References
- 1.Chi J, Verghese A. Clinical education and the electronic health record: the flipped patient. JAMA. 2014;312(22):2331–2332. doi: 10.1001/jama.2014.12820. [DOI] [PubMed] [Google Scholar]
- 2.Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB. Use of electronic clinical documentation: time spent and team interactions. J Am Med Inform Assoc. 2011;18(2):112–117. doi: 10.1136/jamia.2010.008441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lowe HJ, Ferris TA, Hernandez PM, Weber SC. STRIDE: an integrated standards-based translational research informatics platform. AMIA Annu Symp Proc. 2009;2009:391–395. [PMC free article] [PubMed] [Google Scholar]
- 4.Oxentenko AS, West CP, Popkave C, Weinberger SE, Kolars JC. Time spent on clinical documentation: a survey of internal medicine residents and program directors. Arch Intern Med. 2010;170(4):377–380. doi: 10.1001/archinternmed.2009.534. [DOI] [PubMed] [Google Scholar]
- 5.Block L, Habicht R, Wu AW, et al. In the wake of the 2003 and 2011 duty hours regulations, how do internal medicine interns spend their time? J Gen Intern Med. 2013;28(8):1042–1047. doi: 10.1007/s11606-013-2376-6. [DOI] [PMC free article] [PubMed] [Google Scholar]