Abstract
Background
Cardiovascular disease is the most common cause of morbidity and mortality worldwide. Numerous strategies have been effective in reducing cardiovascular disease risk, from pharmacological approaches to lifestyle modification interventions. One of these strategies includes the reduction in dietary sodium which in turn reduces cardiovascular risk by reducing high blood pressure, perhaps the most important cardiovascular risk factor.
Methods
We evaluated an educational dietary salt reduction intervention in a cardiac care unit population in Lebanon, assessing salt related knowledge and behaviours before and after administering an evidence-based educational leaflet to patients.
Results
Salt-related knowledge improved significantly immediately post-intervention and subsequently fell on 4-week follow-up, but remained above baseline. Three of the four salt-related behaviours measured improved on 4-week follow-up: trying to buy low-salt foods increased from 54% to 74% (P=0.007), adding salt at the table reduced from 44% to 34% (P=0.03) and trying to buy food with no added salt increased from 24% to 52% (P=0.02) of the cohort. Adding salt during cooking did not differ significantly. A trend towards improved behavioural risk category in the cohort overall was observed on follow-up (P=0.07), 32% of participants were categorised as high behavioural risk pre-intervention, reducing to 17% on follow-up. Multi-ordered regression modelling identified being in the high-risk behavioural category at baseline as a predictor of being in the high-risk or moderate-risk category on follow-up.
Conclusions
This hospital-based educational intervention had a modestly positive impact on salt-related knowledge and behaviour, with participants in the highest behavioural risk category at baseline being most resistant to behavioural improvement.
Keywords: Educational intervention, dietary salt, knowledge, cardiac care unit (CCU)
Introduction
Cardiovascular disease is the most common cause of morbidity and mortality globally, the majority of which is preventable (1,2). Numerous strategies are effective in reducing cardiovascular disease risk. Pharmacological approaches include the use of drugs to reduce blood pressure (3), serum cholesterol (4) and more recently inhibit pro-inflammatory pathways (5). Aspects of lifestyle modification have also been well demonstrated to reduce cardiovascular disease risk, including optimising physical activity, smoking cessation and dietary modification, including dietary sodium reduction (2,6). Reduction in dietary sodium reduces cardiovascular risk by reducing high blood pressure, perhaps the most important cardiovascular risk factor (7,8) In Lebanon 47% of deaths are attributed to cardiovascular disease and dietary salt consumption is high, estimated between 7–14 g per day (9,10). High dietary salt intake increases blood pressure and a reduction in dietary salt consumption reduces both blood pressure and the risk of hypertension-mediated disease. A meta-analysis has demonstrated that higher dietary sodium intake was consistently associated with a greater risk of fatal coronary artery disease and stroke. The same meta-analysis demonstrated that dietary salt reduction reduces systolic and diastolic blood pressure, with a greater mean reduction in systolic blood pressure in patients with hypertension (11). A subsequent meta-analysis comparing the effects of salt consumption on hypertensive and normotensive individuals confirmed that individuals with established hypertension benefit most from a reduction in dietary salt intake (12).
The substantial body of evidence demonstrating that reducing dietary salt consumption reduces cardiovascular death has led to recommendations for maximal daily salt/sodium intake for both high risk and general populations (13,14). Further, the World Health Assembly has set a global target to reduce global salt consumption by 30% by 2025 (1). In concordance with this dietary salt reduction has become a target for numerous national public health initiatives. These initiatives have taken several approaches including: food industry engagement to reduce sodium content of common foods, changing food labelling, taxing high-salt foods and consumer education. However, these national salt-reduction initiatives have predominantly been established in high-income countries (15). In parallel to national initiatives smaller scale salt-reduction interventions have been shown to be effective in reducing salt intake. For example, a recent school-based educational intervention was shown to reduce salt consumption of both the children exposed to the intervention and their families (16). The lack of national salt-reduction initiatives in low- to middle-income countries, such as Lebanon, could be attributed to limited funding and organizational infrastructure at governmental level. In Lebanon, an academically-led group called Lebanese Action on Sodium and Health (LASH) has been established aiming to take an evidence-based approach to reducing national sodium consumption (17).
In line with the principles of LASH, we previously gathered baseline information on knowledge, attitudes and behaviours related to salt consumption in both the general population and a high-risk cardiac care unit (CCU) population in Lebanon (18,19). In the high-risk population we identified several knowledge gaps and behavioural practices that predispose to higher salt intake, in addition to perceived motivators for reducing salt intake. Further, we identified several factors that were associated with more positive salt-related behaviours (19). The majority of the Lebanese population are aware that high-salt consumption can have a negative impact on health. However, most individuals lacked knowledge as to which commonly consumed foods in Lebanon were high in salt, for example, most individuals surveyed did not think ketchup, processed sauces and Manaeesh (a traditional bread with a thyme and cheese topping) were high in salt. Another interesting observation was that men were often unable to respond to the question “Do you add salt during cooking?”, as a female family member would often do all of the cooking in the household (18,19).
Utilising our population specific evidence we designed a hospital-based educational intervention aimed at reducing salt consumption in individuals at particularly high cardiovascular risk (CCU patients). Here, we evaluate the efficacy of this hospital-based educational intervention by assessing the change in knowledge and self-reported salt related behaviour following implementation.
Methods
The study was approved by the Institutional Review Board of the American University of Beirut.
Participant recruitment
Patients admitted to the CCU were approached after fulfilling the following inclusion criteria: a history of hypertension, coronary artery disease, heart failure, and/or a history of stroke/transient ischemic attack. Written informed consent was obtained prior to the administration of questionnaires. A total of 55 patients were recruited. The sample size calculation was based on the prevalence of expected knowledge found in our previous study (19), assuming a similar level of knowledge in the sampled CCU population. Using the sample size calculation method for the McNemar test, a sample of 46 patients was estimated to be appropriate. Assuming a 20% loss to follow up the required sample size was determined to be 55.
The intervention
CCU patients were given an educational leaflet presenting information aiming to encourage a reduction in salt consumption (Supplementary file 1, Tables S1,S2, Box S1). The leaflet was designed with a consideration of: knowledge gaps, common negative salt-related behaviours and associations with positive salt-related behaviours identified in a previous cross-sectional study of CCU patients in Lebanon (19).
The leaflet included information such as the recommended daily limit for salt intake, major dietary sources of salt and advice on reading food content labels.
Pre-intervention questionnaire
A pre-intervention questionnaire was administered to the patients, which included 38 questions on socio-demographics, knowledge, attitudes and behaviours related to salt consumption. This questionnaire was previously validated in both a CCU population and a population of supermarket shoppers in Lebanon (18,19). The internal consistency for the knowledge and attitude components of this questionnaire were previously evaluated by calculating Cronbach’s alpha coefficients, which were 0.748 and 0.724, respectively (18).
The socio-demographic section included variables on: age, gender, educational level, type of occupation and other information to calculate the crowding index (20). Patients’ medical histories were collected from their medical health records and confirmed by the patients.
Furthermore, the questionnaire included 27 questions on salt-related knowledge, four questions on salt-related attitude, nine questions on salt-related behaviour in addition to five questions exploring motivation for behavioural change (Supplementary file 2).
A knowledge score (0 to 27, based on number of correct knowledge responses) and an attitude score (0 to 4, based on number of positive attitude responses) was calculated for every patient.
Post-intervention questionnaire
The post-intervention questionnaire was given immediately after patients had read the educational leaflet. It comprised three knowledge questions from the baseline questionnaire: “What is the maximum daily amount of salt recommended for adults?”, “Which of the following statements best describes the relationship between salt and sodium?”, and “Which of the following do you think is the main source of salt in the Lebanese diet?”
Four-week follow-up questionnaire
The follow-up questionnaire was administered over the phone 4-week post-intervention. The follow-up questionnaire assessed knowledge and self-reported salt-related behaviours. The questionnaire included the same three knowledge questions used in the post-intervention questionnaire and four questions (from the baseline questionnaire) regarding salt-related behaviour: do you: “…add salt at the table?”; “…add salt during cooking?”; “…try to buy ‘low salt’ foods”; and “…try to buy ‘no added salt’ foods?”
All behaviour questions had the possible responses: often, sometimes, never or not applicable.
Statistical methods
Continuous and categorical data were expressed as mean ± standard deviation (SD) and counts and percentages, respectively. Comparisons between pre- and post-intervention (immediate and 4 weeks later) were conducted using the McNemar test.
Participants were stratified according to their risk of high-salt consumption, based on their behavioural responses to the four behaviour questions, risk scores were calculated for pre- and post-intervention. Participants were given 1 point for answering “often” to “add salt at the table” and 1 point for a response to any of the other behaviour questions that would predispose to higher salt consumption, e.g., responding “never” to “do you try to buy ‘low salt’ foods/try to buy no added salt foods”, or responding “often” to “add salt during cooking”. Patients who reported that they were not involved in grocery shopping and cooking were excluded from this analysis (a total of ten patients). Accordingly, patients with 0 point were considered to have low-risk behaviour for high-salt consumption, patients with 1 point were considered to have moderate-risk behaviour and patients with 2 points were considered to have high-risk behaviour.
Multinomial ordered logistic regression modelling was performed to study the predictors of remaining in the high- or moderate-risk category as compared to low-risk category on follow-up. The model adjusted for baseline risk category, age, gender, number of comorbidities, crowding index, knowledge score and attitude score. P values <0.05 were considered statistically significant. Analyses were done using SPSS version 22.0 software (IBM, Armonk, NY).
Results
Sample characteristics
Fifty-five participants were recruited, of which 5 were lost to follow-up and excluded from the analysis. Of the remaining 50, 32% were female and 40% were over 60.
The most common components of medical history recorded in this cohort were: hypertension (68%) and dyslipidaemia (54%). Key demographic variables are detailed in Table 1.
Table 1. Demographic variables of participating cardiac care unit patients (n=50).
| Characteristics | N | % |
|---|---|---|
| Age (years) | ||
| ≤50 | 20 | 40 |
| 51–60 | 10 | 20 |
| >60 | 20 | 40 |
| Gender | ||
| Male | 34 | 68 |
| Female | 16 | 32 |
| Health-related major* | ||
| Yes | 6 | 12 |
| No | 43 | 86 |
| Educational level | ||
| Intermediate or lower | 13 | 26 |
| High school or technical degree | 16 | 32 |
| University | 21 | 42 |
| Crowding index | ||
| <1 person/room | 29 | 58 |
| ≥1 person/room | 21 | 42 |
| Medical history | ||
| Hypertension | 34 | 68 |
| Dyslipidemia | 27 | 54 |
| Diabetes mellitus | 14 | 28 |
| Percutaneous coronary intervention | 11 | 22 |
| Myocardial infarction | 10 | 20 |
| Angina | 10 | 20 |
| Congestive heart failure | 19 | 38 |
| Coronary artery bypass graft | 14 | 28 |
| Smoker | 26 | 52 |
*, health-related major includes careers related to medicine, biochemistry, nutrition, food science, public health, and nursing.
Pre-intervention questionnaire responses: knowledge, attitude and behavior
Average knowledge score for the cohort was 18.86±3.21 (possible scores: 0 to 27, based on number of correct knowledge responses). Average attitude score for the cohort was 3.27±0.64 (0 to 4, based on number of positive attitude responses).
Ninety-two percent of respondents knew that a high-salt/sodium diet worsens health, with high proportions correctly identifying that high blood pressure (96%) and fluid retention (90%) was caused or aggravated by salty foods. Fewer respondents knew that osteoporosis (36%) and stomach cancer (18%) were caused or aggravated by salty foods.
Pre-intervention the relationship between salt and sodium was identified correctly by 40% of respondents; the maximum recommended daily salt intake was identified correctly by 24% of respondents; and the main source of salt in the Lebanese diet was identified correctly by 54% of respondents.
Regarding attitude, 64% of respondents reported being concerned about the amount of salt/sodium in their diet. A high proportion of participants agreed with the statements: “reducing the amount of salt you add to foods is definitely important to you” (88%) and “reducing the amount of processed foods you eat is definitely important to you” (88%).
Regarding behaviour, 44% of participants reported checking food labels often, with 42% reporting that their food purchase is often influenced by food labels. In contrast, only 18% checked labels specifically for salt/sodium and 18% reported that their purchasing decision was influenced by salt/sodium content often. Proportion of respondents reporting to add salt to food during cooking often was 38%. Forty-four percent of patients reported adding salt at the table often and 78% reported to cutting down on salt (Table 2).
Table 2. Pre-intervention knowledge, attitude and behaviour responses of participating cardiac care unit patients (n=50).
| Knowledge (correct responses) | N | % |
|---|---|---|
| Effect of high-salt/sodium diet on health (correct answer: “worsens health”) | 46 | 92 |
| Health problems caused or aggravated by salty foods | ||
| High blood pressure | 48 | 96 |
| Stroke | 34 | 68 |
| Osteoporosis | 18 | 36 |
| Fluid retention | 45 | 90 |
| Heart attacks | 40 | 80 |
| Stomach cancer | 9 | 18 |
| Kidney disease | 33 | 66 |
| Relationship between salt and sodium (correct answer: “salt contains sodium”)* | 20 | 40 |
| Maximum daily amount of salt recommended for adults (correct answer: “5 g, <1 teaspoon”)* | 12 | 24 |
| Main source of salt in the diet of Lebanese people (correct answer: “processed foods…”)* | 27 | 54 |
| Correctly identified foods as either high, medium or low sources of salt/sodium | ||
| Bread (medium) | 13 | 26 |
| Manaeesh-traditional thyme or cheese-filled pies (high) | 39 | 78 |
| Traditional pies (high) | 38 | 76 |
| Pizza (high) | 40 | 80 |
| Rice (low) | 13 | 26 |
| Cheese (high) | 39 | 78 |
| Milk (low) | 42 | 84 |
| Pear (low) | 44 | 88 |
| Soya sauce (high) | 36 | 72 |
| Fresh carrot (low) | 46 | 92 |
| Ketchup (high) | 44 | 88 |
| Bottled salad dressings (high) | 41 | 82 |
| Traditional roasted nuts (high) | 48 | 96 |
| Sausages and hot dogs (high) | 48 | 96 |
| Attitude (positive responses) | ||
| You are concerned about the amount of salt/sodium in your diet (yes) | 32 | 64 |
| Reducing the amount of salt you add to foods is definitely important to you (agree) | 44 | 88 |
| Reducing the amount of processed foods you eat is definitely important to you (agree) | 44 | 88 |
| Reducing your sodium intake is definitely important to you (agree) | 43 | 86 |
| Behavioural practices | ||
| Use of food labels | ||
| Check labels (often) | 22 | 44 |
| Information on food labels affects purchasing decisions (often) | 21 | 42 |
| Check labels specifically for salt/sodium content (often) | 9 | 18 |
| Salt/sodium content indicated on label affects purchasing decisions (often) | 9 | 18 |
| Try to buy “low salt” foods (often)* | 27 | 54 |
| Try to buy “no added salt” foods (often)* | 12 | 24 |
| Other salt-related behavioral practices | ||
| Add salt during cooking (often)* | 19 | 38 |
| Add salt at the table (often)* | 22 | 44 |
| Is cutting down on salt intake (yes) | 39 | 78 |
*, the behavioural practices followed up.
Knowledge follow-up
For all three knowledge questions the proportion of patients submitting correct answers improved significantly from baseline (pre-intervention) to immediately post-intervention (P<0.001, Figure 1). Proportion of correct responses subsequently dropped for all three questions on 4-week follow-up compared to immediately post-intervention, but remained above baseline levels. However, proportion of correct knowledge responses at 4-week follow-up only remained significantly higher than baseline for the questions querying the relationship between salt and sodium (P=0.003) and the main source of salt/sodium in the Lebanese diet (P=0.02). For the question: “what is the maximum recommended daily salt intake”, the proportion of correct responses was 24% at baseline and remained above this on 4-week follow-up at 42%, but this difference did not reach statistical significance (P=0.08).
Figure 1.
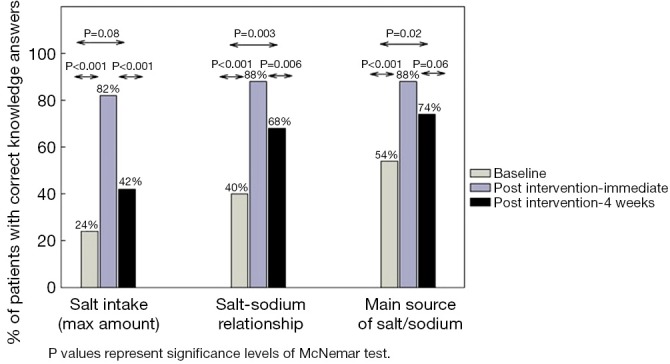
Proportion of respondents answering three knowledge questions correctly at: baseline (pre-intervention), immediately post-intervention and 4 weeks post-intervention.
Behavioural practices follow-up
There was a significant improvement in the proportion of patients reporting more positive salt-related behaviours at 4-week post-intervention, for the behaviours: adding salt at the table, trying to buy no added salt food and trying to buy low-salt food. No significant improvement in the behaviour of adding salt during cooking was found between baseline and follow-up (Figure 2).
Figure 2.
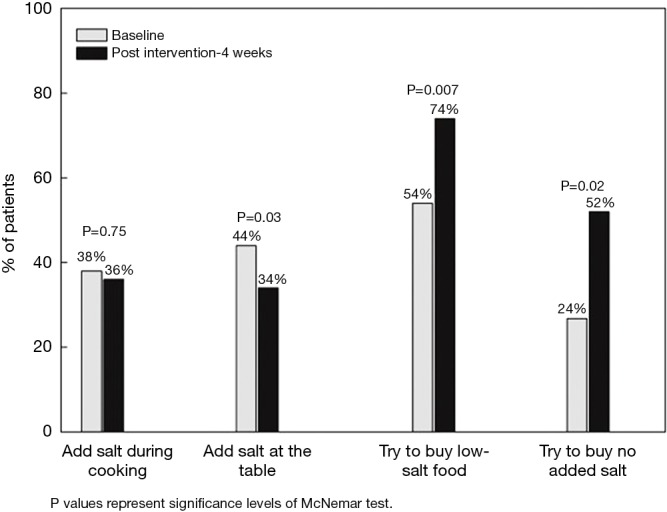
Proportion of respondents answering four behaviour questions correctly at: baseline (pre-intervention) versus 4 weeks post-intervention.
Risk stratification and multinomial ordered logistic regression modelling
At baseline, 31.7% of the cohort were categorised as having high-risk behaviour, this reduced to 17.1% on follow-up. Within the high-risk category, 30.8% shifted to the moderate-risk group and 15% shifted to the low-risk category on follow-up. At baseline 41.5% of the cohort were categorised as moderate risk, with 43.9% categorised as moderate risk on follow-up. Of the participants categorised as moderate risk at baseline, 35.3% shifted to the low-risk category on follow-up. The low-risk category increased from 26.8% to 39.0% of the cohort from baseline to follow-up. The McNemar test showed a trend towards behaviour category improving from baseline to follow-up (P=0.07).
Multinomial ordered logistic regression modelling identified being in the high-risk category at baseline as a significant predictor of remaining in the high-risk or moderate-risk category on follow-up (P=0.004) (This model factored in baseline risk category, age, gender, number of co-morbidities, crowding index, knowledge score and attitude score) (see Figure 3).
Figure 3.
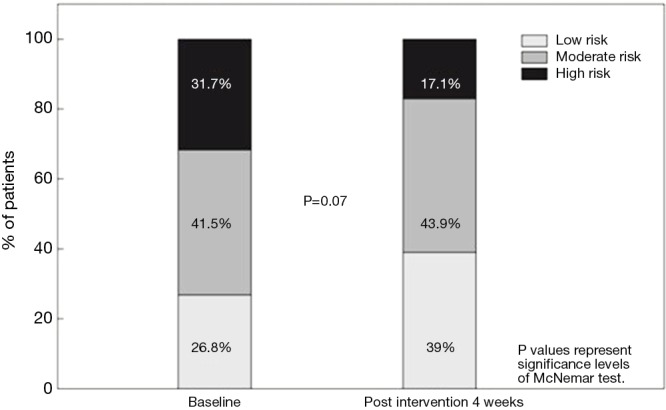
The cohort divided into low-risk, moderate-risk and high-risk categories, based on their behavioural responses at baseline and at 4-week follow-up. The low-risk category comprises participants not reporting any of the four risky behavioural practices. The moderate-risk category comprises participants reporting either “adding salt at the table” or an unfavourable response to any of the other three behaviour questions. The high-risk category comprises participants who “add salt at the table” and report at least one other unfavourable behavioural response.
Discussion
We introduced an educational leaflet aiming to reduce dietary salt intake in a cohort of patients at high cardiovascular risk. To evaluate the efficacy of this intervention we measured salt-related knowledge and self-reported salt intake-related behaviours before and after its delivery. The leaflet design was based on a previous survey gathering information on salt-related knowledge, attitudes, behaviours and motivators for behaviour change in a CCU population in Lebanon, and for the first time incorporated culturally specific dietary data (19). We found that knowledge improved significantly immediately post-intervention for all of the knowledge questions followed up (P<0.001), knowledge retention subsequently declined on 4-week follow-up, but remained above baseline levels. Further, there was a non-significant trend towards behavioural risk category improving in the cohort overall following intervention (P=0.07). Additionally, multinomial ordered logistic regression modelling found that being in the high-risk category at baseline was a predictor of remaining in a higher-risk category (high or moderate risk) on follow-up.
The baseline knowledge, attitude and behaviour findings were consistent with those identified in our previous cross-sectional study of a Lebanese CCU population. For example, 24% of participants could identify the recommended maximal salt intake in this study compared to 19% in the previous study. Also, consistent with the previous CCU study we found that average knowledge and attitude scores in CCU patients were higher compared to the general Lebanese population (19). Higher knowledge score in the CCU population compared to the general population could be related to receiving previous advice from healthcare professionals. Several similar knowledge gaps related to salt consumption were identified in baseline surveys in other regions including Europe, America and Australasia (21-23).
Specific aspects of knowledge and behaviour improved following our intervention. Knowledge improved significantly from pre-intervention for all three knowledge questions when assessed immediately post-intervention (P<0.001). Knowledge levels subsequently dropped on 4-week follow-up compared to immediately post-intervention, but remained significantly above pre-intervention baseline levels for knowing: the relationship between salt and sodium (P=0.003) and the main source of salt in the Lebanese diet (processed foods) (P=0.02). Proportion knowing the recommended daily salt intake was 24% pre-intervention and 42% on follow-up, but this was not significantly higher (P=0.08). This decay in knowledge-retention over time following an educational programme is well described in various healthcare settings (24-26). As knowledge is likely to be an important driver of behaviour, strategies should be employed to ensure long-term retention of knowledge (27). Spacing information over time and periodically testing individuals on aspects of knowledge has been shown to enhance long-term knowledge retention (28,29). In this CCU context most patients will be followed up regularly by a physician, therefore one strategy to enhance salt-related knowledge retention could be for the patient to be quizzed on key aspects of salt-related knowledge on physician follow-up and re-educated on aspects of knowledge not retained. Alternatively, reinforcement of knowledge could be led predominantly by patients. Gomez-Pardo et al. (30) recently evaluated a peer-group based approach comprising monthly meetings aimed at reducing cardiovascular risk in individuals with cardiovascular risk factors. This peer-group approach could be used to reinforce dietary salt reduction messages among high-risk individuals in Lebanon. However, a weakness of this approach is that the intervention was limited to self-selecting volunteers. Other approaches utilized text messaging to reinforce health related knowledge (31,32). In our case text messaging could be used to reinforce the key salt-related messages following the initial hospital-based educational intervention.
We found behaviour improved following intervention in 3 of the 4 salt-related behaviours. After 4 weeks 74% of the cohort was trying to buy low-salt food and 52% were trying to buy no added salt foods, which represented a significant change. Adding salt at the table reduced significantly following our intervention (P=0.03), however, adding salt during cooking was resistant to change. This could be attributed to a number of factors including not sufficiently emphasising the significance of reducing salt use in cooking in the intervention. Additionally, our survey specifically asked about the direct adding of salt to cooking, however, individuals may add salt via high-salt ingredients such as bouillons and processed cooking sauces. The educational leaflet contains a table of common cooking ingredients that are high in salt, so perhaps indirect adding of salt to cooking via high-salt ingredients was reduced, but was not captured by our questionnaire.
There was a non-significant trend towards an overall improvement in behavioural risk category following the intervention (P=0.07). Pre-intervention, 31.7% of the cohort were in the high-risk group compared to 17.1% post-intervention. Further, the low-risk group grew from 26.8% to 39.0% of the cohort. Other consumer education based salt-reduction interventions have similarly demonstrated a modest impact on salt-related behaviours and/or salt consumption (30,33,34). For example, in a cohort of heart failure patients receiving salt-related education by phone or face-to-face (every 6 weeks), there was no significant reduction in salt consumption on initial 6-week follow-up, but there was on 6-month follow-up (34).
A unique finding of this study is that being in the high-risk behaviour category pre-intervention is a strong predictor of being classified as high or moderate risk on follow-up. This effect persists when adjusting for age, gender, number of co-morbidities, crowding index, knowledge score and attitude score. A patient in the high-risk group at baseline is 29.5 times more likely to be in the high or moderate category than the low-risk category on follow-up (P=0.004). This suggests that the patients with the largest number of unfavourable salt-related behaviours are the most resistant to significantly improving behaviour.
Some key limitations of this study should be noted. A small sample sized may have limited statistical conclusions in this study. For example, the trend shown of improving behavioural risk category on follow-up may have been statistically significant with a larger cohort. Additionally, as behaviour was self-reported, social approval bias may have impacted upon these findings (35). Taking physiological measurements, such as urinary sodium would have allayed this limitation, however, at baseline patients were in hospital, so this approach would not have been feasible as dietary intake would have been controlled by the hospital, concurrent illness may have affected appetite and medications (diuretics) will alter urinary sodium. Furthermore, the study was limited to a single centre and impact of this intervention beyond one month is unknown.
In conclusion, there was a modest improvement in salt-related behaviour 4 weeks following the implementation of this educational intervention in patients at high cardiovascular risk. Therefore, circulation of this educational leaflet to CCU patients in Lebanon is justified. However, the impact of this modest behavioural improvement on health is unknown and needs to be tested. It is probable that educational interventions such as this one need to be complimented by other salt-reduction interventions in order to result in a significant impact on patient health. Therefore, future work in Lebanon should include examining the impact of a combination of dietary sodium reduction interventions on long-term behaviour, measured sodium consumption and health outcomes.
Acknowledgements
None.
Supplementary
Supplementary file 1 Tips and information on salt consumption
Salt (sodium chloride) is one of the major contributors to sodium intake. Excess sodium intake is associated with increased blood pressure, which in turn, increases the risk of chronic diseases such as stroke, heart disease and kidney disease.
Therefore, the World Health Organization (WHO) recommends that adults reduce sodium intake to less than 2,000 mg of sodium/day (5 g of salt/day) (refer to Box S1).
Research conducted in Lebanon has shown that salt intake among adults is higher than the recommended maximum intake level. Data from these studies have also indicated that the major sources of salt in the Lebanese diet are processed foods that include the following: bread and “ka’ak”, cold cuts and luncheon meats, dairy products, snacks and fast foods (potato chips, “falafel”, pizza, “manaeesh”, ...). These food items constitute %65 of daily salt intake (refer to Table S1).
To decrease salt consumption, read food labels carefully in order to be able to choose the food item with the lowest salt content (less than 140 mg/100 g). Therefore, it is important that you familiarize yourself with these labels and what they mean (refer to Table S2).
Key recommendations for decreasing salt consumption
ϖ Choose bread types that are low in salt or that are salt-free;
ϖ Use vinegar, lemon juice, garlic, onions and herbs for food seasoning, while limiting the use of salt in cooking;
ϖ Remove the salt shaker from the table;
ϖ Replace spread cheese and high-salt cheeses with low-fat, low-salt versions which are available in the Lebanese market, or soak them in water to decrease their salt content;
ϖ Limit the consumption of pickled vegetables, fast food items/meals (“manaeesh”, “fatayer”, “sambousek” and pizza), processed food items (dried soups, ketchup, mustard, stock/broth cubes (beef or chicken), soy sauce, and other ready-made sauces and dressings), cold cuts, luncheon meats and packaged meats (“sujuk”, “makanek”, mortadella and hot dogs);
ϖ Use fresh foods whenever possible. If you need to use canned vegetables and legumes, rinse them with water several times to reduce their salt content;
ϖ Choose unsalted nuts and seeds.
For more information, visit the Vascular Medicine Program page at www.vmp.aub.edu.lb.
Supplementary file 2 Items contained within the study questionnaire by category
Knowledge items
The Knowledge questions asked participants:
What they think the general effect of dietary salt/sodium is on health (“improves health”, “has no effect on health”, “worsens health” or “don’t know”);
Whether they thought high dietary salt caused or aggravated each of a list of seven health conditions (high blood pressure, stroke, osteoporosis, heart attacks, stomach cancer and kidney disease) by indicating either: “yes”, “no” or “don’t know”;
To identify which statement best describes the relationship between sodium and salt: “they are exactly the same”, “salt contains sodium”, “sodium contains salt” or “don’t know”;
To identify which statement identifies the maximal recommended daily salt intake: “3 g (½ teaspoonful)”, “5 g (<1 teaspoonful)”, “9 g (1 ½ teaspoons)”, “12 g (2 teaspoons)”, “15 g (2 ½ teaspoons)” or “don’t know”;
To identify the statement they thought represented the main source of salt in the Lebanese diet: “salt added during cooking”, “salt added at table”, “salt in processed foods such as breads, cured meats, canned foods and takeaway”, “salt from natural sources such as vegetables and fruits” or “don’t know”;
To classify a list of 16 common foods into “high”, “medium”, “low” or “don’t know” salt/sodium content.
Attitude
The attitude questions comprised:
Three questions that utilize a 5-point Likert scale ranging from “strongly disagree” to “strongly agree”, which are: “reducing the amount of salt you add to foods is definitely important to you”; “reducing the amount of processed foods (e.g., breads, cured meats, canned foods and takeaway) you eat is definitely important to you” and “reducing your sodium intake is definitely important to you”. For analysis “strongly agree” and “agree” were collapsed into one category to represent agreement with the statement, and “strongly disagree” and “disagree” to represent disagreement;
The final question was a “yes or no” question enquiring if the participant is concerned about the amount of salt/sodium in their diet.
Behaviour
The self-reported behaviour questions comprised:
Two questions on the use of food labels in general: “How often do you check food content labels when you are shopping?” and “Does what is on the food content label affect whether or not you purchase a food item?”;
Two questions on the use of salt-related food labels: “How often do you look at the salt/sodium content on food labels when you are shopping?” and “How often does the salt/sodium content shown on the food label affect whether you purchase a product?”;
Two questions on the frequency of behaviours that increase salt consumption: “Do you add salt during cooking?” and “Do you add salt at the table?”;
Two questions on the frequency of behaviours that reduce salt intake: “Do you try to buy ‘low salt’ foods?” and “Do you try to buy ‘no added salt’ foods?”;
-
A single “yes or no” question asking: “Are you cutting down on the amount of salt you eat?”.
All of these questions enquiring about frequency had the possible responses: “often”, “sometimes”, “never” or “not applicable”.
Motivation
The questions exploring motivators for behaviour change were:
“What would motivate you to reduce your salt intake?” with the options: “A dramatic change in health status”, “if my doctor advised it”, “if family members or friends advised it” or “other, please specify”;
“What are the barriers against decreasing your salt intake?” with the options: “It tastes good”, “I am not concerned with decreasing my salt intake”, “I don’t know which foods to avoid” and “Other, please specify”;
“Where do you get your health information from” with the options: “My doctor, “my family and friends”, “the internet”, “the media” and “other, please specify”;
“Who is most responsible for helping you reduce your sodium/salt intake?”, with the options: “the government (public health campaign)” “Companies that make or sell foods with salt in them (food industry)”, “your doctor”, “yourself” and “other, please specify”;
“Have you been previously advised by a physician, nurse or dietitian about the risks of a salt-rich diet and the need to moderate salt intake?” with the options: “yes” or “no”.
Box S1 Maximum limit for daily salt intake.
| 5 g of salt/day ≈ ¾ teaspoon of salt (equivalent to a maximum of 2,000 mg of sodium/day) |
| To all individuals, with or without hypertension (including pregnant or lactating women) |
Table S1. Sodium content of selected food items.
| Food item | Serving size (equivalent to 100 g) | Sodium (mg) |
|---|---|---|
| Breads, all types | ¾ loaf | 316–700 |
| “Markouk” | 1 loaf | 811 |
| “Ka’ak” | 7 sticks | 452 |
| Pretzels, saltine or dry | 16 items | 1,357 |
| “Manaeesh” | 100 g | 735 |
| Pizza, plain, cheese | 1 large slice | 450–1,200 |
| Croissant | 1 large piece | 744 |
| “Mafroukeh b’kashta” | 1 medium slice | 183 |
| “Znood el sitt” | 2 items | 223 |
| “Baklawah” | 3 items | 227 |
| “Kol-wa-shkor” | 3 items | 244 |
| “Ish-el-bulbul” | 20 items | 248 |
| Potato chips | 1 large bag | 800–1,200 |
| Ketchup | 7 tablespoons | 1,113 |
| Lupine (“turmus”) | ½ cup | 1,121 |
| White cheese | 100 g | 320 |
| “Ashawan” cheese | 100 g | 249 |
| “Labneh” | 3.5 tablespoons | 356 |
| Frozen vegetables, all types | ½ cup | 2–160 |
Table S2. Understanding food-label claims.
| Food-label claims | What they mean |
|---|---|
| Sodium-free/no sodium | Less than 5 mg of sodium /serving and no sodium chloride in ingredients |
| Very low sodium | 35 mg or less sodium/serving |
| Low sodium | 140 mg or less sodium/serving |
| Reduced sodium/less sodium | At least 25% less sodium/serving than the regular food product |
| Unsalted, no salt added | No artificial salt added, but product may contain natural sodium as part of the product |
Ethical Statement: This study was approved by the Institutional Review Board (IRB), a core component of the Human Research Protection Program (HRPP) of the American University of Beirut Medical Center (No. 0002657).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.WHO. Sixty-sixth World Health Assembly. Follow-up to the Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. 2013. Available online: http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_R10-en.pdf
- 2.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315-81. 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.SPRINT Research Group , Wright JT Jr, Williamson JD, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med 2015;373:2103-16. 10.1056/NEJMoa1511939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344:1383-9. [PubMed] [Google Scholar]
- 5.Ridker PM, Everett BM, Thuren T, et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med 2017;377:1119-31. 10.1056/NEJMoa1707914 [DOI] [PubMed] [Google Scholar]
- 6.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2960-84. 10.1016/j.jacc.2013.11.003 [DOI] [PubMed] [Google Scholar]
- 7.Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep 2013;15:134-6. 10.1007/s11906-013-0340-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fahed AC, El-Hage-Sleiman AK, Farhat TI, et al. Diet, genetics, and disease: a focus on the middle East and north Africa region. J Nutr Metab 2012;2012:109037. 10.1155/2012/109037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Powles J, Fahimi S, Micha R, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013;3:e003733. 10.1136/bmjopen-2013-003733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. World Health Organisation: Non-communicable diseases country profiles 2014. 2014. Available online: http://www.who.int/nmh/countries/en/
- 11.Aburto NJ, Ziolkovska A, Hooper L, et al. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ 2013;346:f1326. 10.1136/bmj.f1326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Graudal N, Hubeck-Graudal T, Jürgens G, et al. The significance of duration and amount of sodium reduction intervention in normotensive and hypertensive individuals: a meta-analysis. Adv Nutr 2015;6:169-77. Erratum in: Adv Nutr 2015;6:285. 10.3945/an.114.007708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.WHO. Guideline: Sodium intake for adults and children. Geneva, World Health Organization (WHO), 2012. [PubMed] [Google Scholar]
- 14.Appel LJ, Frohlich ED, Hall JE, et al. The importance of population-wide sodium reduction as a means to prevent cardiovascular disease and stroke: a call to action from the American Heart Association. Circulation 2011;123:1138-43. 10.1161/CIR.0b013e31820d0793 [DOI] [PubMed] [Google Scholar]
- 15.Trieu K, Neal B, Hawkes C, et al. Salt Reduction Initiatives around the World - A Systematic Review of Progress towards the Global Target. PLoS One 2015;10:e0130247. 10.1371/journal.pone.0130247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.He FJ, Wu Y, Feng XX, et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. BMJ 2015;350:h770. 10.1136/bmj.h770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Almedawar MM, Nasreddine L, Olabi A, et al. Sodium intake reduction efforts in Lebanon. Cardiovasc Diagn Ther 2015;5:178-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nasreddine L, Akl C, Al-Shaar L, et al. Consumer knowledge, attitudes and salt-related behavior in the Middle-East: the case of Lebanon. Nutrients 2014;6:5079-102. 10.3390/nu6115079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walsh JL, Fathallah J, Al-Shaar L, et al. Knowledge, attitudes, motivators and salt-related behaviour in a cardiac care unit population: A cross-sectional study in Lebanon. Med J Nutrition Metab 2017;10:79-91. 10.3233/MNM-16129 [DOI] [Google Scholar]
- 20.Melki IS, Beydoun HA, Khogali M, et al. Household crowding index: a correlate of socioeconomic status and inter-pregnancy spacing in an urban setting. J Epidemiol Community Health 2004;58:476-80. 10.1136/jech.2003.012690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Claro RM, Linders H, Ricardo CZ, et al. Consumer attitudes, knowledge, and behavior related to salt consumption in sentinel countries of the Americas. Rev Panam Salud Publica 2012;32:265-73. 10.1590/S1020-49892012001000004 [DOI] [PubMed] [Google Scholar]
- 22.Marakis G, Tsigarida E, Mila S, et al. Knowledge, attitudes and behaviour of Greek adults towards salt consumption: a Hellenic Food Authority project. Public Health Nutr 2014;17:1877-93. 10.1017/S1368980013002255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grimes CA, Riddell LJ, Nowson CA. Consumer knowledge and attitudes to salt intake and labelled salt information. Appetite 2009;53:189-94. 10.1016/j.appet.2009.06.007 [DOI] [PubMed] [Google Scholar]
- 24.Nelissen E, Ersdal H, Mduma E, et al. Helping Mothers Survive Bleeding After Birth: retention of knowledge, skills, and confidence nine months after obstetric simulation-based training. BMC Pregnancy Childbirth 2015;15:190. 10.1186/s12884-015-0612-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blumenfeld A, Ben Abraham R, Stein M, et al. Cognitive knowledge decline after Advanced Trauma Life Support courses. J Trauma 1998;44:513-6. 10.1097/00005373-199803000-00017 [DOI] [PubMed] [Google Scholar]
- 26.Sarti E, Flisser A, Schantz PM, et al. Development and evaluation of a health education intervention against Taenia solium in a rural community in Mexico. Am J Trop Med Hyg 1997;56:127-32. 10.4269/ajtmh.1997.56.127 [DOI] [PubMed] [Google Scholar]
- 27.Godin G, Kok G. The theory of planned behavior: a review of its applications to health-related behaviors. Am J Health Promot 1996;11:87-98. 10.4278/0890-1171-11.2.87 [DOI] [PubMed] [Google Scholar]
- 28.Raman M, McLaughlin K, Violato C, et al. Teaching in small portions dispersed over time enhances long-term knowledge retention. Med Teach 2010;32:250-5. 10.3109/01421590903197019 [DOI] [PubMed] [Google Scholar]
- 29.Larsen DP, Butler AC, Aung WY, et al. The effects of test-enhanced learning on long-term retention in AAN annual meeting courses. Neurology 2015;84:748-54. 10.1212/WNL.0000000000001264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gómez-Pardo E, Fernández-Alvira JM, Vilanova M, et al. A Comprehensive Lifestyle Peer Group-Based Intervention on Cardiovascular Risk Factors: The Randomized Controlled Fifty-Fifty Program. J Am Coll Cardiol 2016;67:476-85. 10.1016/j.jacc.2015.10.033 [DOI] [PubMed] [Google Scholar]
- 31.Kannisto KA, Koivunen MH, Välimäki MA. Use of mobile phone text message reminders in health care services: a narrative literature review. J Med Internet Res 2014;16:e222. 10.2196/jmir.3442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehran L, Nazeri P, Delshad H, et al. Does a text messaging intervention improve knowledge, attitudes and practice regarding iodine deficiency and iodized salt consumption? Public Health Nutr 2012;15:2320-5. 10.1017/S1368980012000869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sutherland J, Edwards P, Shankar B, et al. Fewer adults add salt at the table after initiation of a national salt campaign in the UK: a repeated cross-sectional analysis. Br J Nutr 2013;110:552-8. 10.1017/S0007114512005430 [DOI] [PubMed] [Google Scholar]
- 34.Welsh D, Lennie TA, Marcinek R, et al. Low-sodium diet self-management intervention in heart failure: pilot study results. Eur J Cardiovasc Nurs 2013;12:87-95. 10.1177/1474515111435604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hebert JR, Ma Y, Clemow L, et al. Gender differences in social desirability and social approval bias in dietary self-report. Am J Epidemiol 1997;146:1046-55. 10.1093/oxfordjournals.aje.a009233 [DOI] [PubMed] [Google Scholar]


