Abstract
The effect of sulforaphane on nuclear factor erythroid 2-related factor 2 (Nrf2) and its protective mechanism for lung injury in rabbits with acute respiratory distress syndrome (ARDS) were investigated. Thirty rabbits were randomly divided into control (n=10), model (n=10) and experimental groups (n=10). Rabbits in model group and experimental group were treated with femoral venous injection of oleic acid to establish the ARDS model, while those in control group were injected with the same volume of normal saline. The experimental group received intravenous injection of sulforaphane. Twelve hours after modeling, the clinical manifestations and deaths of rabbits in each group were recorded and compared, including blood gas indexes, lung index (LI), alveolar damage coefficient, serum Nrf2 expression, as well as messenger ribonucleic acid (mRNA) and protein expression of Nrf2 in lung tissues. Pink frothy sputum and death were observed in rabbits in model group and experimental group, but the number of such cases in experimental group was smaller than that in the model group (p<0.05). Compared with those in control group, LI and IQA in model group and experimental group were increased, but LI and IQA in the experimental group were significantly decreased compared with those in the model group. Compared with those in the model group, the blood gas indexes (PaO2, PaCO2 and SaO2) in the experimental group were significantly increased (p<0.05). Nrf2 in serum and lung tissues of rabbits in experimental group was significantly increased compared with that in model group (p<0.05). Sulforaphane significantly inhibits ARDS in rabbits and plays a protective role in ARDS through upregulating Nrf2.
Keywords: Nrf2, acute respiratory distress syndrome, sulforaphane, acute lung injury, mRNA
Introduction
Acute lung injury (ALI), also known as acute respiratory distress syndrome (ARDS), is a common critical disease caused by ALI (1,2). Its clinical features are the increased permeability of alveolar capillary barrier and air exchange dysfunction, and its typical clinicopathologic features include the injury of pulmonary capillary endothelial cells, extensive pulmonary edema and microatelectasis of alveolar epithelial cells, microthrombosis and microcirculation disorder (3). Severe infections, trauma, shock, poisoning and inhalation of toxic gases are the most common causes of ALI (4). At present, patients with ARDS mainly receive supportive therapy, especially the maintenance of ventilation and oxygenation, normal cardiac function and nutritional support, and application of nitric oxide and corticosteroids, so as to prevent further complications (5,6). Therefore, there is a lack of effective treatment means for ADRS.
Sulforaphane, also known as ‘raphanin’, is the extract of cruciferous vegetables (such as broccoli, Brussels sprouts and cabbage). As an agonist of nuclear factor erythroid 2-related factor 2 (Nrf2), sulforaphane has been proved to be able to activate the Nrf2 expression in the heart and the nervous system, and protect multiple organs, such as liver, lung and kidney (7,8). Moreover, it has also been shown that sulforaphane can protect Nrf2-positive peritoneal macrophages in mice (9); however, there are no studies on it in the ADRS model induced by inflammatory factors. In this study, the protective mechanism of sulforaphane against ADRS was mainly studied, so as to provide a certain theoretical basis for the clinical treatment of ADRS.
Materials and methods
Grouping and treatment of experimental animals
A total of 30 specific pathogen-free (SPF) rabbits (license no. BD20174321) were purchased from the Laboratory Animal Center (Jiangsu, China). They were randomly divided into: Control (n=10), model (n=10) and experimental groups (n=10). Rabbits in the model group and experimental group were treated with femoral venous injection of 0.1 ml/kg oleic acid to establish the oleic acid-induced ARDS model, while those in control group were injected with the same volume of normal saline. Whereas, rabbits in the experimental group received femoral venous injection of 5 mg/ml/kg sulforaphane (Aokai, Guangzhou, China) dissolved by normal saline, while those in the model group were injected with the same volume of normal saline. Within 12 h after treatment, the reactions and deaths of rabbits in each group were observed and recorded.
Materials and detection of the indexes
At 12 h after treatment of rabbits in each group, they were anesthetized with chloral hydrate, and the body weight of rabbits was recorded. Then blood was drawn from the femoral artery until the death of rabbits. The blood was placed at 4°C for 1 h for stratification, followed by centrifugation at 2,380 × g for 10 min. The upper-layer serum was taken, and rabbit lung tissues were excised and weighed, and the lung index (LI) was calculated: LI = total lung mass (g)/body mass (kg). After weighing, lung tissues were immediately divided into two parts; one part was stored in liquid nitrogen for reverse transcription-polymerase chain reaction (RT-PCR), while the other part was fixed in 4% paraformaldehyde for hematoxylin and eosin (H&E) morphological examination and immunohistochemistry (IHC). The study was approved by the Ethics Committee of Cangzhou Central Hospital (Cangzhou, China).
The alveolar damage coefficient [index of quantitative assessment (IQA)] was calculated following the steps below: Six H&E staining sections of lung tissues were taken from rabbits in each group, and 10 images were taken in the same field of view, and the number of damaged alveoli (containing more than 2 erythrocytes or neutrophils in alveoli) was calculated. The ratio of the number of damaged alveoli to the total number of alveoli was used as the IQA to evaluate the degree of lung injury.
RT-PCR
Total ribonucleic acid (RNA) was extracted by using TRIzol reagent (Invitrogen, Carlsbad, CA, USA) from lung tissues, and purified by using the extraction kit (Qiagen, Valencia, CA, USA) according to instructions provided by the manufacturer. The content of Nrf2 gene was detected by using the qRT-PCR kit, followed by quantification using the fluorescence quantitative detection system (Applied Biosystems, Foster City, CA, USA), with β-actin as the internal reference. Primer sequences of gene amplification are as follows: Nrf2 forward, 5′-CCCACACAAGGTTCGGCATCAC-3′ and reverse, 5′-TGGCGATTCCTCTGGCGTCT-3′; β-actin forward, 5′-CGCGCCATCAAGGAGAAGCTG-3′ and reverse, 5′-ATTGCCAATGGGTGATACCTG-3′.
Enzyme-linked immunosorbent assay (ELISA) detection
Commercially-available ELISA kits were used to detect the serum Nrf2 in rabbits in each group. According to instructions provided by the manufacturer, Nrf2 was labeled by using the double-antibody sandwich method, and the optical density (OD) values were detected by using a microplate reader at dual wavelengths of 450 and 600 nm, and the sample concentration was calculated.
H&E staining and IHC
The nuclei and cytoplasm of lung tissues were stained with H&E (Google Biological Co., Ltd., Wuhan, China), and sections were dehydrated with gradient ethanol and then sealed with neutral gum. The Nrf2 protein (1:500; Cell Signaling Technology, Danvers, MA, USA) expressed in the nuclei was specifically labeled by using the two-step method and IHC assay kits (Zhongshan Golden Bridge Biotechnology Co., Ltd., Guangzhou, China). H&E and IHC sections were observed under an inverted microscope (DM-5000B; Leica Store Wetzlar, Wetzlar, Germany). At least 3 regions were photographed in each section, and brown yellow-stained cells in IHC staining were positive cells; the proportion of Nrf2-positive cells in each field of view in the total cells ≤5% indicated negative, while that >5% indicated positive.
Arterial blood gas analysis
Blood was drawn from the femoral artery under anesthesia, and the blood gas indexes (PaO2, PaCO2 and SaO2) were determined by using a blood-gas analyzer (Hunan Sanhe Apparatus, Changsha, China).
Statistical analysis
Experimental results were analyzed by using GraphPad Prism statistical software 5.01 (GraphPad Software, Inc., La Jolla, CA, USA). Measurement data are presented as mean ± SD, and one-way analysis of variance (ANOVA) was used for the comparison of differences among groups. P<0.05 was considered to indicate a statistically significant difference.
Results
Clinical manifestations and mortality rate of the rabbit models
Within 12 h after modeling, rabbits in both model and experimental groups spit pink frothy sputum, including 5 rabbits (50%) in the model group, and only 2 rabbits (20%) in the experimental group. There were 6 deaths (60%) in the model group and 3 deaths (30%) in the experimental group (Table I).
Table I.
The percentage of pink frothy sputum and death occuring in three groups at 12 h from modeling.
| Pink frothy sputum | Death | ||||
|---|---|---|---|---|---|
| Groups | No. | No. | % | No. | % |
| Control | 10 | 0 | 0 | 0 | 0 |
| Model | 10 | 5 | 50 | 6 | 60 |
| Experimental | 10 | 2 | 20 | 3 | 30 |
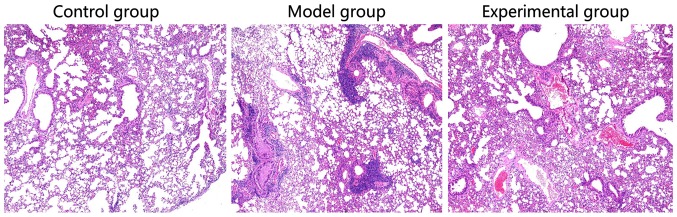
Pathological examination of lung tissues of rabbits
Compared with the rabbit lung tissues in control group, obvious alveolar edema, alveolar interstitial serous exudate, aggregation of a large number of inflammatory cells, and partial pulmonary septal thickening could be seen in rabbits in model group. In experimental group, there was no aggregation of a number of inflammatory cells, but only a small amount of serous exudate (Fig. 1).
Figure 1.
Detection of pathological features of rabbit lung tissues in two groups via H&E staining. ##P<0.05.
Detection of Nrf2 mRNA level in rabbit lung tissues via RT-PCR
There was no statistically significant difference in the comparison of Nrf2 mRNA level in rabbit lung tissues between model group and control group (p>0.05), and Nrf2 mRNA level in rabbit lung tissues in experimental group was significantly increased compared with that in model group (p<0.05; Fig. 2).
Figure 2.
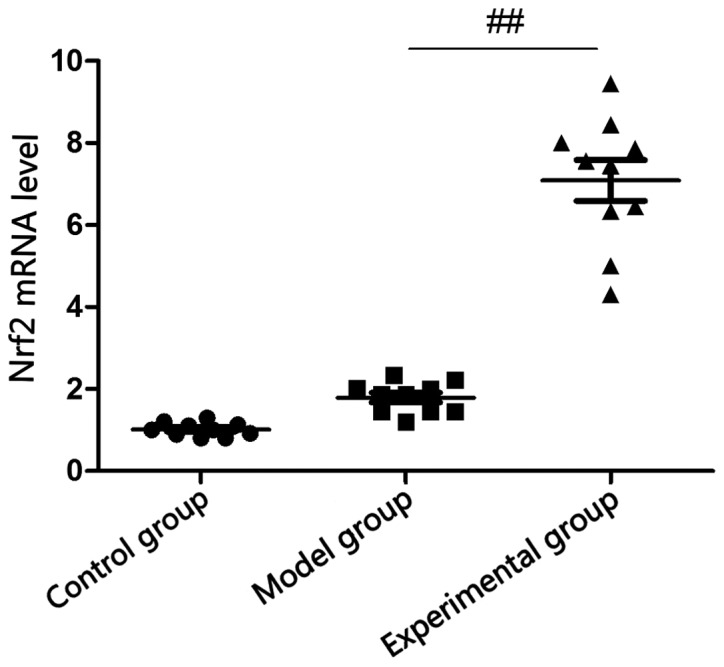
Detection of Nrf2 mRNA level in rabbit lung tissues via RT-PCR. Compared with model group, ##P<0.01. Nrf2, nuclear factor erythroid 2-related factor 2.
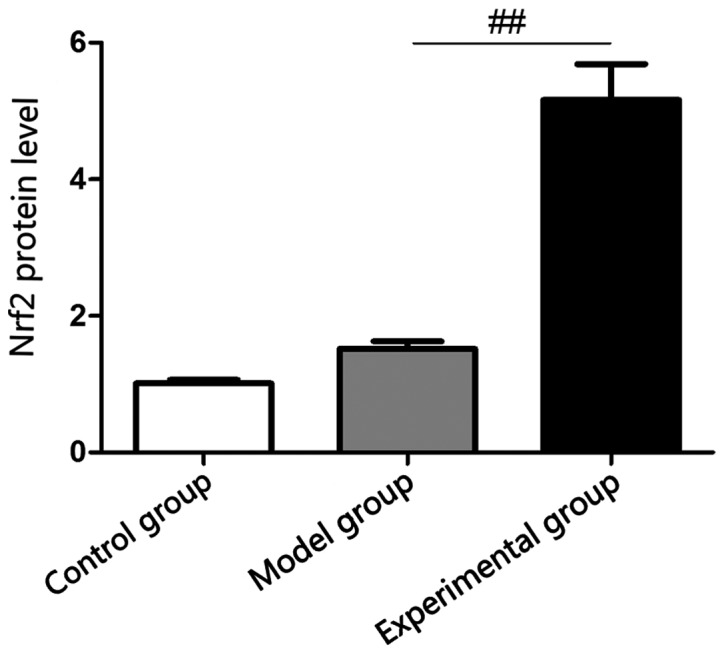
Detection of serum Nrf2 content in rabbits via ELISA
ELISA showed that there was no statistically significant difference in the comparison of Nrf2 protein level in rabbit lung tissues between model and control groups (p>0.05), and Nrf2 protein level in rabbit lung tissues in experimental group was significantly increased compared with that in model group (p<0.05), which were consistent with results of RT-PCR (Fig. 3).
Figure 3.
Detection of Nrf2 protein level in rabbit serum via ELISA. Nrf2, nuclear factor erythroid 2-related factor 2.
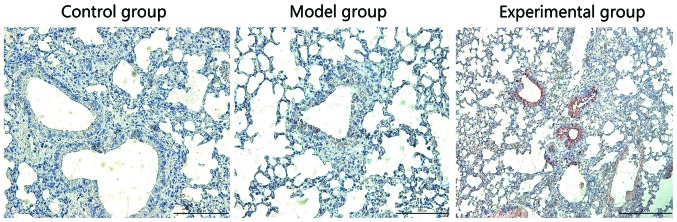
Detection of Nrf2 protein expression in rabbit lung tissues via IHC
Nrf2 protein was mainly located in the cytoplasm. As shown in Fig. 4, the Nrf2 expression was negative in rabbit lung tissues in control group, which was negative in model group, but strongly positive in the experimental group.
Figure 4.
Detection of Nrf2 protein level in rabbit lung tissues via IHC. Nrf2, nuclear factor erythroid 2-related factor 2; IHC, immunohistochemistry.
Comparison of lung injury indexes between two groups of rabbits
LI was selected to show the degree of pulmonary edema (Table II).
Table II.
Comparisons of lung injury indexes (LI and IQA) between two groups of rabbits (mean ± SD).
| Groups | LI | IQA |
|---|---|---|
| Control | 4.32±0.12 | 12.36±2.07 |
| Model | 7.18±0.73a | 42.71±4.12b |
| Experimental | 5.76±0.42c | 22.73±6.65d |
Compared with control group
p<0.05
p<0.001; compared with model group
p<0.05
p<0.01. LI, lung index; IQA, index of quantitative assessment.
Comparison of arterial blood gas indexes between two groups of rabbits
Compared with those in control group, the blood gas indexes (PaO2, PaCO2 and SaO2) in the model and experimental groups were obviously decreased (p<0.05); but the blood gas indexes in the experimental group were significantly increased compared with those in the model group (p<0.05; Table III).
Table III.
Comparisons of PaO2, PaCO2 and SaO2 between three groups 12 h after modeling.
| Index | Control | Model | Experimental |
|---|---|---|---|
| PaO2 (KPa) | 9.13±0.21 | 4.84±0.52a | 6.02±0.86b |
| PaC02 (KPa) | 5.42±0.27 | 2.16±0.43a | 3.94±1.05b |
| SaO2 (%) | 96.34±1.32 | 61.85±6.07a | 84.91±1.87c |
Compared with control group
p<0.05; compared with model group
p<0.05
p<0.01.
Discussion
ARDS is a non-cardiogenic pulmonary edema secondary to alveolar damage after inflammatory process. However, the pathogenesis of this disease remains to be elucidated (10). It was believed initially that the primary cause of ALI is the cell activation caused by pathogenic factors and body fluid, leading to inflammatory response syndrome and pathological processes, such as alveolar collapse, imbalance of ventilation/perfusion ratio and decreased lung compliance (11). The imbalance of inflammatory response and anti-inflammatory response is of great significance in the development of ARDS. According to its pathological features, ARDS can be divided into early and late stages: Acute lung tissue inflammation and injury (12).
The occurrence of inflammation begins from the inflammatory cell exudate and immune cell-mediated breakdown of alveolar epithelial interstitial barrier, making plasma and proteins, flood the pulmonary interstitium and air space in turn (13). Currently, ARDS is recognized as a neutrophil-driven disease; moreover, it has been increasingly recognized that innate cells (including macrophages and platelets) and adaptive immune system are involved in the incidence of ARDS (14,15). Experiments have found that neutrophils and macrophages are recruited into inflammatory lesions. The resulting inflammatory exudate interacts with the surfactant, finally causing dysfunction (16). H&E assays in this study clearly showed the aggregation of a number of inflammatory cells in rabbit lung tissues, which was consistent with the above conclusion.
Nrf2 is a key regulator of antioxidant gene activation. Reactive oxygen species (ROS) produced under pathological conditions interact with the protein to damage the body through a variety of pathways. Nrf2 can regulate the expression of thioredoxin peroxidases, enhance the ability of cells to scavenge ROS, maintain the redox equilibrium state of cells, and reduce the oxidative damage (17). Currently, the study on Nrf2 has shown that it is a promising therapeutic target for ADRS, and many studies have demonstrated the importance of Nrf2 activation in protecting ALI/ARDS (18). The study of Yu et al found that sulforaphane increases the Nrf2 gene expression in lung tissues of mice with lipopolysaccharide (LPS)-induced ALI (19). Nrf2 is also involved in the infection-induced ALI. Studies have shown that pneumonia is caused by Staphylococcus aureus, and develops into ALI in extreme cases due to increased alveolar permeability, neutrophil infiltration and production of cytokines. Compared with those in Nrf2−/− mice, ROS produced by mitochondria and mitochondrial autophagy-degradation-induced pulmonary epithelial cell apoptosis are significantly inhibited in Nrf2+/+ transgenic mice vaccinated with Staphylococcus aureus (20). In this study, sulforaphane significantly increased the Nrf2 expression in rabbit lung tissues and serum, and protect from lung injury in rabbits.
In conclusion, results of this study indicate that sulfadoxine exerts a significant anti-inflammatory effect on ARDS in rabbits through upregulating the Nrf2 expression. In addition, results of this study provide a certain theoretical basis for the application of sulforaphane and clinical prophylactic treatment of ALI.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
ZS wrote the manuscript and helped with ELISA. ZN and SW analyzed H&E staining and IHC. SS contributed to arterial blood gas analysis. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Cangzhou Central Hospital (Cangzhou, China).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353:1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- 2.Thille AW, Esteban A, Fernández-Segoviano P, Rodriguez JM, Aramburu JA, Vargas-Errázuriz P, Martín-Pellicer A, Lorente JA, Frutos-Vivar F. Chronology of histological lesions in acute respiratory distress syndrome with diffuse alveolar damage: A prospective cohort study of clinical autopsies. Lancet Respir Med. 2013;1:395–401. doi: 10.1016/S2213-2600(13)70053-5. [DOI] [PubMed] [Google Scholar]
- 3.Martin TR, Pistorese BP, Chi EY, Goodman RB, Matthay MA. Effects of leukotriene B4 in the human lung. Recruitment of neutrophils into the alveolar spaces without a change in protein permeability. J Clin Invest. 1989;84:1609–1619. doi: 10.1172/JCI114338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frank JA, Wray CM, McAuley DF, Schwendener R, Matthay MA. Alveolar macrophages contribute to alveolar barrier dysfunction in ventilator-induced lung injury. Am J Physiol Lung Cell Mol Physiol. 2006;291:L1191–L1198. doi: 10.1152/ajplung.00055.2006. [DOI] [PubMed] [Google Scholar]
- 5.Comstock TL, Decory HH. Advances in corticosteroid therapy for ocular inflammation: Loteprednol etabonate. Int J Inflamm. 2012;2012:789623. doi: 10.1155/2012/789623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Emr BM, Roy S, Kollisch-Singule M, Gatto LA, Barravecchia M, Lin X, Young JL, Wang G, Liu J, Satalin J, et al. Electroporation-mediated gene delivery of Na+, K+-ATPase, and ENaC subunits to the lung attenuates acute respiratory distress syndrome in a two-hit porcine model. Shock. 2015;43:16–23. doi: 10.1097/SHK.0000000000000228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ather JL, Alcorn JF, Brown AL, Guala AS, Suratt BT, Janssen-Heininger YM, Poynter ME. Distinct functions of airway epithelial nuclear factor-kappaB activity regulate nitrogen dioxide-induced acute lung injury. Am J Respir Cell Mol Biol. 2010;43:443–451. doi: 10.1165/rcmb.2008-0416OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang L, Taneja R, Wang W, Yao LJ, Veldhuizen R, Gill SE, Fortin D, Inculet R, Malthaner R, Mehta S. Human alveolar epithelial cells attenuate pulmonary microvascular endothelial cell permeability under septic conditions. PLoS One. 2013;2:e55311. doi: 10.1371/journal.pone.0055311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fard N, Saffari A, Emami G, Hofer S, Kauczor HU, Mehrabi A. Acute respiratory distress syndrome induction by pulmonary ischemia-reperfusion injury in large animal models. J Surg Res. 2014;189:274–284. doi: 10.1016/j.jss.2014.02.034. [DOI] [PubMed] [Google Scholar]
- 10.Yan YM, Li YD, Song XL, Liu M, Diao F, Wang Y, Sun Y, Wang ZH, Lu J. Therapeutic effects of inhaling aerosolized surfactant alone or with dexamethasone generated by a novel noninvasive apparatus on acute lung injury in rats. J Trauma Acute Care Surg. 2012;73:1114–1120. doi: 10.1097/TA.0b013e318265cbe9. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt AE, Adamski J. Education Committee of the Academy of Clinical Laboratory Physicians and Scientists: Pathology consultation on transfusion-related acute lung injury (TRALI) Am J Clin Pathol. 2012;138:498–503. doi: 10.1309/AJCPFF6JKXM7BYOI. [DOI] [PubMed] [Google Scholar]
- 12.Chi X, Zhang R, Shen N, Jin Y, Alina A, Yang S, Lin S. Sulforaphane reduces apoptosis and oncosis along with protecting liver injury-induced ischemic reperfusion by activating the Nrf2/ARE pathway. Hepatol Int. 2015;9:321–329. doi: 10.1007/s12072-014-9604-y. [DOI] [PubMed] [Google Scholar]
- 13.Lin W, Wu RT, Wu T, Khor TO, Wang H, Kong AN. Sulforaphane suppressed LPS-induced inflammation in mouse peritoneal macrophages through Nrf2 dependent pathway. Biochem Pharmacol. 2008;76:967–973. doi: 10.1016/j.bcp.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149:818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 15.Abdulnour RE, Howrylak JA, Carlo T, Sham HP, Henkels KM, Miller TE, Dolinay T, Baron RM, Choi MK, Cambronero JG, et al. Phospholipase D regulates inflammatory responses during acute lung injury. Am J Respir Crit Care Med. 2016;193:A7773. [Google Scholar]
- 16.Fernandez-Bustamante A, Repine JE. Chronic inflammatory diseases and the acute respiratory distress syndrome (ARDS) Curr Pharm Des. 2014;20:1400–1408. doi: 10.2174/13816128113199990561. [DOI] [PubMed] [Google Scholar]
- 17.Myzak MC, Karplus PA, Chung FL, Dashwood RH. A novel mechanism of chemoprotection by sulforaphane: Inhibition of histone deacetylase. Cancer Res. 2004;64:5767–5774. doi: 10.1158/0008-5472.CAN-04-1326. [DOI] [PubMed] [Google Scholar]
- 18.Han CW, Kwun MJ, Kim KH, Choi JY, Oh SR, Ahn KS, Lee JH, Joo M. Ethanol extract of Alismatis Rhizoma reduces acute lung inflammation by suppressing NF-κB and activating Nrf2. J Ethnopharmacol. 2013;146:402–410. doi: 10.1016/j.jep.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 19.Yu J, Wang Y, Li Z, Dong S, Wang D, Gong L, Shi J, Zhang Y, Liu D, Mu R. Effect of heme oxygenase-1 on mitofusin-1 protein in LPS-induced ALI/ARDS in rats. Sci Rep. 2016;6:36530. doi: 10.1038/srep36530. doi: 10.1038/srep36530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shan Y, Akram A, Amatullah H, Zhou DY, Gali PL, Maron-Gutierrez T, González-López A, Zhou L, Rocco PR, Hwang D. ATF3 protects pulmonary resident cells from acute and ventilator-induced lung injury by preventing Nrf2 degradation. Antioxid Redox Signal. 2015;22:651–668. doi: 10.1089/ars.2014.5987. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.