Abstract
Pill-induced esophagitis is a rare cause of acute chest pain. Patients likely to be affected are those with underlying esophageal disorders, those who ingest medications without a sufficient amount of water, or adopt a supine position during or shortly after swallowing medication. Esophagitis secondary to ingestion of ascorbic acid pills is extremely rare. Here, we report a case of ascorbic acid-induced esophagitis in a middle-aged adult, with no known underlying pathological abnormalities of the esophagus. Diagnosis was made based on the history and endoscopic findings. The patient fully recovered and an esophageal ulcer healed after discontinuation of ascorbic acid.
Keywords: Chest pain, pill-induced esophagitis, ascorbic acid
Introduction
Pill-induced esophagitis is a rare cause of acute chest pain. It is one of the potential side effects of commonly used drugs such as tetracycline, doxycycline, clindamycin, and nonsteroidal anti-inflammatories (NSAIDs).1–4 However, few published reports exist that describe ascorbic acid causing esophagitis.5 Risk factors for the development of drug-induced esophagitis include use of a small quantity of water when swallowing medication, lying down during or immediately after drug ingestion, and the presence of underlying esophageal disorders.6,7 The most common esophagitis symptoms are chest pain, odynophagia, and dysphagia.8 Esophagogastroscopy typically demonstrates a nonspecific ulcer located in the middle or lower third of the esophagus with normal adjoining mucosa.8
Here, we report a case of ascorbic acid-induced esophagitis which presented as acute chest pain, diagnosed on endoscopy and resolved after discontinuation of ascorbic acid.
Case report
A 38-year-old gentleman, a cardiologist by profession, presented with acute onset of severe chest pain. He had no history of coronary heart disease, hypertension, diabetes, pulmonary disease, or gastroesophageal reflux. The only clinically relevant history was ingestion of two pills of ascorbic acid (100 mg per pill, an acidic substance with diameter of 7 mm and thickness of 2 mm) the night before the onset of chest pain. The patient was taking ascorbic acid due to its perceived antioxidant and health-promoting benefits. He ingested these pills with a small quantity of water and lay down immediately after drug ingestion. On clinical examination, there were no obvious findings. Since his previous annual medical checkup was normal, detailed cardiorespiratory investigations were not performed. Endoscopy was performed, which revealed an isolated ulcer measuring 0.3 cm, round and regular, no bleeding, and at the lower end of the esophagus, approximately 35 cm from the incisors with no evidence of Barrett’s esophagus, dysplastic mucosa, or a hiatal hernia (Figure 1). As there was no suspicion of malignancy on endoscopy, biopsy was deferred. Based on a positive history of drug ingestion and endoscopy findings, a clinical diagnosis of drug-induced esophagitis was made and the patient was advised to discontinue ascorbic acid. Pantoprazole (40 mg twice daily) was prescribed for 2 weeks. At follow-up, patient reported complete resolution of symptoms 2 days after the initiation of treatment and repeat esophagoscopy 2 weeks after admission confirmed complete healing of the ulcer (Figure 2). Half a year later, the symptoms were negative. When the endoscopy was done again, normal esophagus mucosa found.
Figure 1.
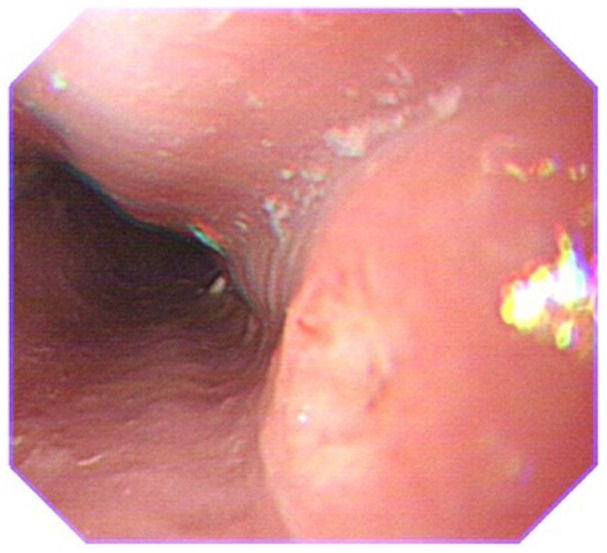
Upper endoscopy revealed an isolated ulcer in the esophagus at 35 cm from the incisors.
Figure 2.
Upper endoscopy revealed a normal esophagus.
Discussion
Ascorbic acid is a commonly used drug due to its antioxidant properties. It is often used in dental ulcer, angina pectoris or whitening, and so on. Development of esophageal injury due to ascorbic acid is extremely rare with only one previously reported case in the published literature.5 In the reported case by Walta et al.,5 the patient had diffused esophageal spasm, which predisposed to the development of esophagitis. In the patient described here, ingestion of the drug with minimal water and then adopting a supine position resulted in esophageal injury, a common mechanism as reported by several other studies on drug-induced esophagitis.4,6,7 Walta et al.5 also performed a study in an animal model and hypothesized that prolonged mucosal contact with ascorbic acid leads to esophagitis. The rarity of this side effect of ascorbic acid can be explained due to the minimal time ascorbic tablets come into contact with esophageal mucosa in individuals taking the tables correctly. Nowadays, more people pay attention to antiaging. In this case, the patient without potential diseases had the ascorbic acid pills for healthcare. What is more, this patient had the pills and went to bed immediately without enough water. It is not clear as to whether this side effect is dose dependent. In the case reported by Walta et al.,5 the dose of ascorbic acid was 500 mg, while the patient in our report had a dose of 200 mg. A capsule form has been reported to be more frequently associated with esophagitis than tablets or syrups,9 however, in our case, the patient had consumed ascorbic acid pills.
In pill-induced esophagitis, ulcers are typically located at the level of the mid-esophagus when identified during esophagogastroscopy.10 This site is commonly implicated as pills often ’ lodged in narrow areas of the esophagus, leading to prolonged mucosal contact. This may result in mucosal inflammation, erosion, and ulceration, even in the absence of underlying esophageal disorders.11 Endoscopic biopsy of the ulcer is rarely diagnostic as it often shows acute inflammatory changes in the majority of cases.9 Biopsy is more useful in order to rule out underlying malignancy, viral infections, or other causes of esophagitis in such cases.
There are some shortcomings. First, our case lacks the biopsy in the ulcer and in the margin of the ulcer. As described in our case, we can differentiate pill-induced esophagitis from eosinophilic esophagitis (EoE), Bechet’s disease, and tuberculosis (TB) with medical history, the follow-up symptoms, and the result of esophagogastroscopy. Second, the figure of the ulcer under endoscopy was not clear enough. As this was a non-sedative esophagogastroscopy and the patient felt violent nausea, unfortunately, we did not catch a clearer picture.
Treatment of pill-induced esophagitis consists of discontinuation of the offending drug, use of proton pump inhibitors, or sucralfate to hasten esophageal mucosal healing and to rule out any underlying esophageal motility disorder.5,9
In conclusion, this case highlights the importance of a detailed drug and disease history when treating patients with esophagitis. It showed that seemingly safe drugs such as ascorbic acid can lead to esophagitis if ingested inappropriately. It also underlines the importance of providing appropriate instructions such as not lying down immediately after administration and getting appropriate water to help the capsule/pill to slide down the esophagus.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Health and Family Planning Commission of Zhejiang Province (Grant nos 201483560 and 2016KYB257). The funding authorities had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Patient consent: Written informed consent was obtained from the patients for their anonymized information to be published in this article.
ORCID iD: Lei Xu  https://orcid.org/0000-0001-6017-3745
https://orcid.org/0000-0001-6017-3745
References
- 1. Singh NP, Rizk JG. Oesophageal perforation following ingestion of over-the-counter ibuprofen capsules.J Laryngol Otol 2008; 122(8):864–866. [DOI] [PubMed] [Google Scholar]
- 2. Guttman OR, Zachos M. Drug-induced esophageal injury with an occult vascular ring. Paediatr Child Healt 2011; 16(9): 554–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Almashat SJ, Duan L, Goldsmith JD. Non-reflux esophagitis: a review of inflammatory diseases of the esophagus exclusive of reflux esophagitis. Semin Diagn Pathol 2014; 31(2): 89–99. [DOI] [PubMed] [Google Scholar]
- 4. Carlborg B, Densert O, Lindqvist C. Tetracycline induced esophageal ulcers: a clinical and experimental study. Laryngoscope 1983; 93(2): 184–187. [DOI] [PubMed] [Google Scholar]
- 5. Walta DC, Giddens JD, Johnson LF, et al. Localized proximal esophagitis secondary to ascorbic acid ingestion and esophageal motor disorder. Gastroenterology 1976; 70(5 PT. 1): 766–769. [PubMed] [Google Scholar]
- 6. de Groen PC, Lubbe DF, Hirsch LJ, et al. Esophagitis associated with the use of alendronate. New Engl J Med 1996; 335(14): 1016–1021. [DOI] [PubMed] [Google Scholar]
- 7. Jaspersen D. Drug-induced oesophageal disorders: pathogenesis, incidence, prevention and management. Drug Safety 2000; 22(3): 237–249. [DOI] [PubMed] [Google Scholar]
- 8. Kim SH, Jeong JB, Kim JW, et al. Clinical and endoscopic characteristics of drug-induced esophagitis. World J Gastroentero 2014; 20(31): 10994–10999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dag MS, Ozturk ZA, Akin I, et al. Drug-induced esophageal ulcers: case series and the review of the literature. Turk J Gastroenterol 2014; 25(2): 180–184. [DOI] [PubMed] [Google Scholar]
- 10. Abid S, Mumtaz K, Jafri W, et al. Pill-induced esophageal injury: endoscopic features and clinical outcomes. Endoscopy 2005; 37(8): 740–744. [DOI] [PubMed] [Google Scholar]
- 11. Kikendall JW. Pill esophagitis. J Clin Gastroenterol 1999; 28(4): 298–305. [DOI] [PubMed] [Google Scholar]


