Abstract
Hepatic splenosis represents the heterotopic implantation of splenic tissue caused by the spillage of cells from the spleen usually after splenectomy or splenic trauma. This condition is usually an incidental finding during surgery and its real incidence is unknown. Splenic implants, which can be placed anywhere in the abdominal cavity, are usually multiple and may be confused with different benign and malignant conditions such as renal tumors, abdominal lymphomas, and endometriosis. We hereby report an unusual case of multiple abdominal splenosis, with a particular intra-hepatic location, that could be misinterpreted as an hepato-cellular carcinoma.
Keywords: Abdomen, computed tomography (CT), magnetic resonance imaging (MRI), liver, spleen
Introduction
Splenosis is the auto-transplantation of splenic tissue in a heterotopic location that mostly develops after abdominal injuries (1). It is presumed that the spillage of the damaged splenic pulp into the adjacent cavities causes the beginning of the seeding process (2). There are other hypotheses such as the hematogenous spread of splenic pulp, which claims that the splenic erythrocyte progenitor cells enter the liver through the portal vein and then grow as a consequence of tissue hypoxia (3). The term “splenosis” was first used by Buchbinder and Lipkoff in 1939, to describe the heterotopic transplantation of splenic tissue as a consequence of splenic trauma or surgery (4). Nowadays the incidence rate for patients with a history of splenic trauma or splenic surgery is reported to be 67% (5,6). The appropriate use of commonly available diagnostic tools can facilitate accurate diagnosis, avoiding unnecessary surgical procedures.
This case report shows an unusual case of multiple abdominal splenosis, with a particular intra-hepatic location, that could be misinterpreted as an hepato-cellular carcinoma.
Case report
A 69-year-old man, was admitted to our institution because of dyspnea, severe lower extremity edema, and right upper quadrant abdominal pain. Physical examination and past medical history were unremarkable except for the history of ventricular tachycardia. The sister had died because of breast cancer. He had a post-traumatic splenectomy as a result of a car accident that had happened when he was a child. An abdominal ultrasound was performed, showing no significant abdominal abnormalities except for the presence of a 4-cm solid echogenic mass located in the sixth liver segment. The patient had no history of alcohol abuse. Initial routine laboratory tests, including complete blood count and serum chemistry, did not reveal any abnormalities except for a mild anemia and a slight alteration of C-reactive protein. Moreover, the patient’s serology for hepatitis B and C was negative. Additionally, specific laboratory tests, including tumor markers such as carcino-embryonic antigen and alpha-fetoprotein, were unremarkable. Contrast-enhanced helical computed tomography (CT) examination of the abdomen was subsequently performed and it showed multiple intra-abdominal nodular lesions. The largest of these lesions was found adjacent to the sixth liver segment with a maximum diameter of 6.5 × 4.6 cm and 4.0 × 1.8 cm and near the falciform ligament (Figs. 1 and 2). Additional lesions were found next to the mesenteric bowels, in the left para-vesical space (Figs. 3 and 4), scattered throughout the peritoneal cavity, in the splenic loggia and near the posterior cecal wall. A contrast-enhanced magnetic resonance (MR) scan, which confirmed the presence of the multiple abdominal and intra-hepatic nodular lesions, was obtained. These masses displayed low signal intensity on unenhanced T1-weighted (T1W) images, and were slightly hyperintense on T2-weighted (T2W) sequences, showing lower enhancement on contrast-enhanced T1W images compared to the normal surrounding liver parenchyma. Considering the CT and MR imaging (MRI) findings, and according to the history of splenectomy, the absence of hepatic liver diseases, and normal lab examination, the possibility of multiple abdominal splenosis with particular intra-hepatic locations was claimed. The patient subsequently underwent fine needle aspiration biopsy of the largest liver mass at the sixth segment. Histopathologic examination confirmed the benign nature of the lesion, which consisted of splenic tissue. Thus, a final diagnosis of multiple splenosis was made and the patient was discharged without any other complications.
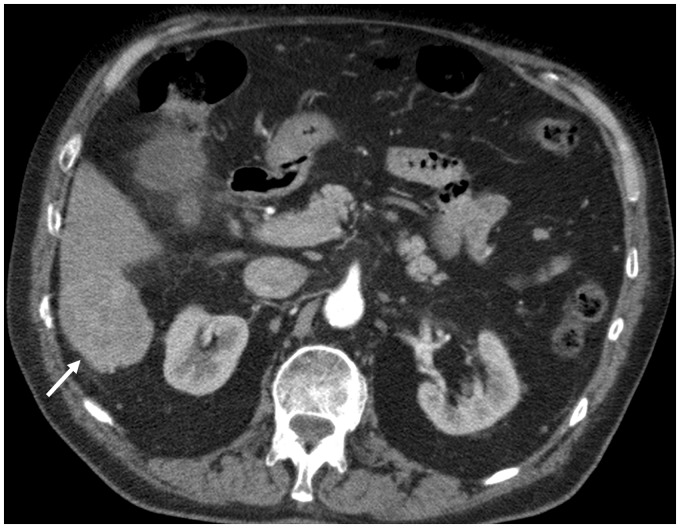
Fig. 1.
Contrast-enhanced arterial phase CT of the abdomen showing one mildly enhancing lesion contiguous to the sixth liver segment (arrow) measuring 6.5 × 4.6 cm.
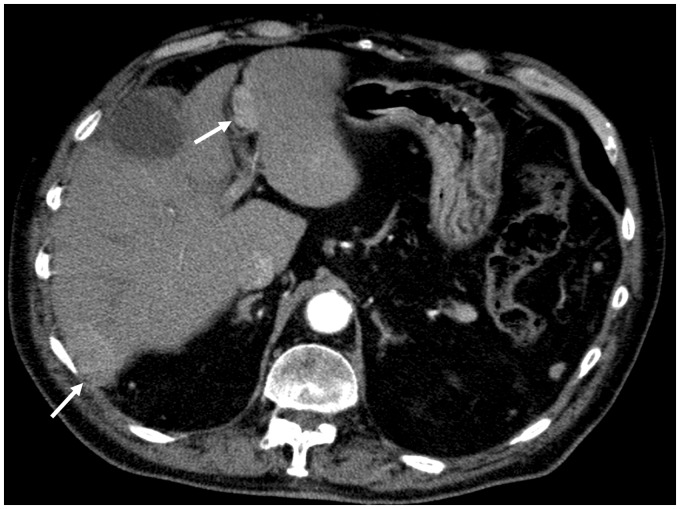
Fig. 2.
Contrast-enhanced arterial phase CT of the abdomen showing two additional lesions located within the sixth liver segment of 4.0 × 1.8 cm and along the falciform ligament of 2.6 × 1.2 cm (arrows).
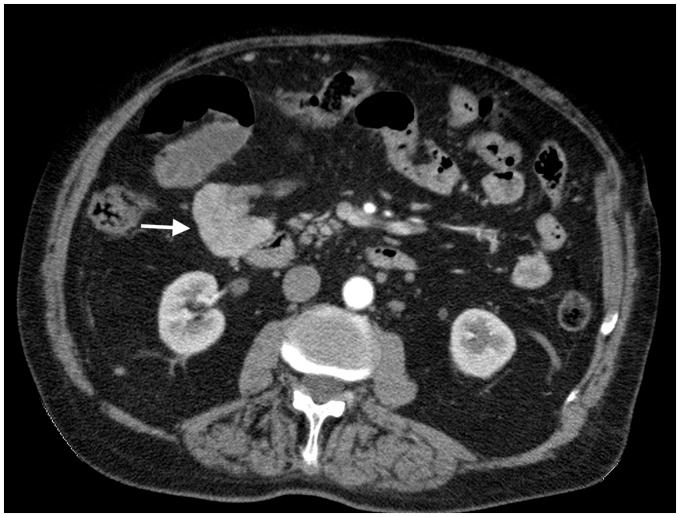
Fig. 3.
Contrast-enhanced arterial phase CT of the abdomen showing a 4.6 × 3.6 cm lesion adjacent to the mesenteric bowels, in the right anterior para-renal space (arrow).
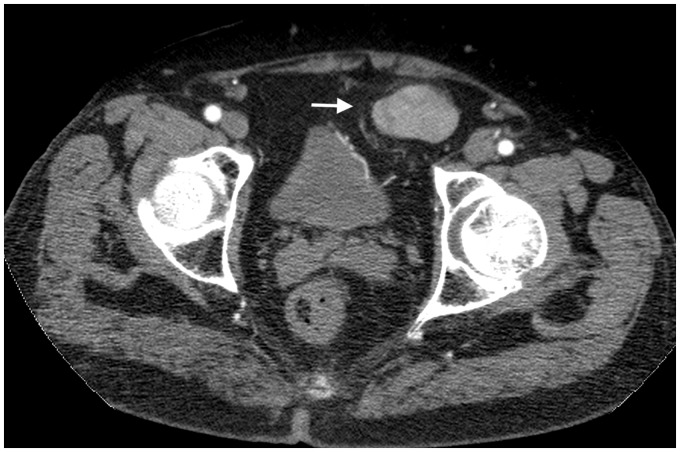
Fig. 4.
Contrast-enhanced arterial phase CT of the abdomen showing a lesion of 4.4 × 3.2 cm in the left anterior para-vesical space (arrow).
Discussion
We describe an unusual case of multiple abdominal splenosis with particular intra-hepatic locations, diagnosed with combined CT and MRI, that could be misinterpreted as a primitive hepatocellular carcinoma and histologically confirmed as benign splenic tissue. This case report highlights the rarity of this condition and the difficult differential diagnosis. A careful clinical history evaluation and an appropriate CT and MRI interpretations should be made by clinicians to distinguish splenosis from other similar benign and malignant lesions, in order to select the most appropriate diagnostic and therapeutic approach.
Splenosis is a condition with several cases described in the literature (5–9). Ectopic splenic tissue can be found in the body as two distinct forms: accessory spleens and splenosis. Accessory spleens are congenital, arising from the dorsal mesogastrium during the embryonic period (10), usually solitary, located near the spleen, in the region of gastrosplenic ligaments and receiving blood supply from the splenic artery. Histologically these resemble the normal spleen with a hilus, normal pulp, and splenic capsule. On the other hand, splenic implants are usually multiple and small (11), with a distorted architecture with no hilum, poorly formed capsules, and variable in shape and size (10). They receive blood supply from nearby arteries at the site of implantation that can occur in any part of the body: they may be localized in the peritoneum (10–12), in the thorax (13), in the pelvis (14,15), in the skin (16,17), or even cerebrum (18). In particular, hepatic splenosis refers to a heterotopic implantation of splenic tissues in the liver. Mechanism of splenic tissue spread is not completely understood. One of the hypotheses is that after rupture or capsule compromise, splenic pulp displaces and “seeds” on the liver surface and then penetrates into the depth. Alternatively, spleen cells may hematogenously spread through the splenic vein and subsequently implant in the liver (9,10,19–21). Splenic implants can be partially or fully functioning and usually are asymptomatic; nevertheless, some clinical features have been reported. They mainly depend on size and localization of the ectopic spleen tissues and can include abdominal pain, gastro-intestinal bleeding, bowel obstruction, or appendicitis secondary to adhesive bands of splenic implants associated with compression or sudden torsion of the solid lesion. When it happens, they represent an indication for surgical resection of the ectopic splenic tissue. Around 18 cases of intra-hepatic splenosis have been reported in the literature during the last ten years (22). According to published reports, intra-hepatic splenosis usually manifests as nodular and solitary lesions, in the size range of 2–6 cm (19). In our case, we detected three intra-hepatic nodules with a maximum diameter of 6.5 × 4.6 cm. In addition, several other intra-abdominal locations were identified near the mesenteric bowels, posteriorly to the cecum and in the left para-vesical space. Intra-hepatic splenosis, in absence of any clinical symptoms, do not require treatments. Thus, the correct identification of this rare condition is particularly important to avoid unnecessary procedures. The differential diagnosis of splenosis is difficult to realize, due to lack of typical radiological features using conventional ultrasound, CT, and MRI and include hepatic or renal malignancies, metastatic disease, pheochromocytoma, lymphoma, carcinomatosis, endometriosis, or adenopathy. Fine needle aspiration is actually considered the gold standard to make a definitive diagnosis of splenosis (9), but it is an invasive procedure which is not immune to complications especially bleeding. Nowadays, the use of 99mTc labelled heat-denatured erythrocyte scintigraphy (99mTc-Pyperythrocyte SPECT) allows the diagnosis to be confirmed. It should be considered as the technique of choice due to its great sensitivity and specificity, as previously described (23). Biopsy or operation could be avoided with the application of 99mTc-Pyperythrocyte SPECT scintigraphy (24). A missed diagnosis of intra-hepatic splenosis usually has a negative influence on patient’s management. Besides, the most difficult differential diagnosis is of accessory spleen. Splenosis may also have some immunologic values and splenic filtering functions, which could be beneficial for organism. Therefore, hepatic splenosis requires no treatment in most cases. When the diagnosis remains unclear, further biopsy or laparoscopy is recommended. If hepatic splenosis is confirmed, careful clinical and diagnostic follow-up with CT or MRI is beneficial.
In conclusion, considering the patient’s clinical history of splenectomy or splenic trauma, splenosis should be added to the list of possible differential diagnosis of multiple incidental intra-abdominal or intra-hepatic masses, in order to avoid unnecessary surgical intervention. When imaging features of a lesion are compatible with normal splenic tissue in a patient with splenic trauma or splenectomy, the diagnosis of splenosis should be taken into account.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Feferman I, Cramer J. Splenosis: an unusual cause of intra-abdominal haemorrhage. J Emerg Med 1991; 9: 239–240. [DOI] [PubMed] [Google Scholar]
- 2.Fremont RD, Rice TW. Splenosis: a review. South Med J 2007; 100: 589–593. [DOI] [PubMed] [Google Scholar]
- 3.Kwok CM, Chen YT, Lin HT, et al. Portal vein entrance of splenic erythrocyte progenitor cells and local hypoxia of liver, two events cause intrahepatic splenosis. Med Hypotheses 2006; 67: 1330–1332. [DOI] [PubMed] [Google Scholar]
- 4.Buchbinder JH, Lipkoff CJ. Splenosis: Multiple peritoneal splenic implants following abdominal injury. A report of a case and review of the literature. Surgery 1939; 6: 927–934. [Google Scholar]
- 5.Younan G, Wills E, Hafner G. Splenosis: a rare etiology for bowel obstruction. A case report and review of the literature. Case Rep Surg 2015; 2015: 890602–890602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imbriaco M, Camera L, Manciuria A, et al. A case of multiple intra-abdominal splenosis with computed tomography and magnetic resonance imaging correlative findings. World J Gastroenterol 2008; 14: 1453–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Vuysere S, Van Steenbergen W, Aerts R, et al. Intrahepatic splenosis: imaging features. Abdom Imaging 2000; 25: 187–189. [DOI] [PubMed] [Google Scholar]
- 8.Lin WC, Lee RC, Chiang JH, et al. MR features of abdominal splenosis. Am J Roentgenol 2003; 180: 493–496. [DOI] [PubMed] [Google Scholar]
- 9.Liu Y, Ji B, Wang G, et al. Abdominal multiple splenosis mimicking liver and colon tumours: a case report and review of the literature. Int J Med Sci 2012; 9: 174–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tsitouridis I, Michaelides M, Sotiriadis C, et al. CT and MRI of intraperitoneal splenosis. Diagn Interv Radiol 2010; 16: 145–149. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira H, Maciel C, Morgado A, et al. Rectovaginal splenosis: an unexpected cause of dyspareunia approached by laparoscopy. J Minim Invasive Gynecol 2017; 24: 715–716. [DOI] [PubMed] [Google Scholar]
- 12.Holstein A, Egberts EH, Stumpf O, et al. Intraperitoneal splenosis: a simple diagnosis if you remember to think of it. Clin J Gastroenterol 2009; 2: 417–419. [DOI] [PubMed] [Google Scholar]
- 13.Remtulla M, Drury NE, Kaushal NA, et al. Thoracic splenosis masquerading as advanced lung cancer. Thorax 2017; 72: 189–190. [DOI] [PubMed] [Google Scholar]
- 14.Anrique D, Anton A, Krüger K, et al. Splenosis: an uncommon differential diagnosis in gynecology. J Minim Invasive Gynecol 2013; 20: 708–709. [DOI] [PubMed] [Google Scholar]
- 15.Ekong E, Goojha C, Kamencic H. Expect the unexpected: a case of pelvic splenosis. J Obstet Gynaecol Can 2011; 33: 787–787. [DOI] [PubMed] [Google Scholar]
- 16.Lorenzi L, Bertoletti E, Facchetti F. A case of subcutaneous “red pulp” splenosis. Int J Dermatol 2015; 54: e559–561. [DOI] [PubMed] [Google Scholar]
- 17.Yeh CJ, Chuang WY, Kuo TT. Unusual subcutaneous splenosis occurring in a gunshot wound scar: pathology and immunohistochemical identification. Pathol Int 2006; 56: 336–339. [DOI] [PubMed] [Google Scholar]
- 18.Rickert CH, Maasjosthusmann U, Probst-Cousin S, et al. A unique case of cerebral spleen. Am J Surg Pathol 1999; 22: 894–896. [DOI] [PubMed] [Google Scholar]
- 19.Jereb S, Trotovsek B, Skrbinc B. Hepatic splenosis mimicking liver metastases in a patient with history of childhood immature teratoma. Radiology and Oncology 2016; 50: 212–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leong CW, Menon T, Rao S. Post-traumatic intrahepatic splenosis mimicking a neuroendocrine tumour. BMJ Case Rep 2013, pp. bcr2012007885–bcr2012007885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi GH, Ju MK, Kim JY, et al. Hepatic splenosis preoperatively diagnosed as hepatocellular carcinoma in a patient with chronic hepatitis B: a case report. J Korean Med Sci 2008; 23: 336–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang MY, Li B, Chen D, et al. Spleen implanting in the fatty liver mimicking hepatocarcinoma in a patient with hepatitis B&C: A case report and literature review. Medicine (Baltimore) 2017; 96: e7217–e7217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yuste JR, Buades J, Guillen EF, et al. Post-traumatic intra-thoracic splenosis. From clinical suspicion to non-invasive diagnosis. Am J Med 2014; 127: e3–4. [DOI] [PubMed] [Google Scholar]
- 24.Wu C, Zhang B, Chen L, et al. Solitary perihepatic splenosis mimicking liver lesion: a case report and literature review. Medicine (Baltimore) 2015; 94: e586–e586. [DOI] [PMC free article] [PubMed] [Google Scholar]