Abstract
Background:
Hip arthroscopic surgery is a rapidly growing procedure that requires distraction of the leg to access the joint. A frequently reported complication of this procedure is postoperative numbness, with rates between 1% and 20% reported in the literature.
Purpose/Hypothesis:
The purpose of this study was to determine the factors contributing to the development and effect of numbness on functional outcomes. We hypothesized that this complication is underreported and that its prevalence is higher than what has been described in the literature.
Study Design:
Case series; Level of evidence, 4.
Methods:
Patients who had undergone hip arthroscopic surgery between 2012 and 2016 were included, and a telephone survey was conducted to collect data. Data related to the procedure and outcome scores were collected via a systematic chart review for the included patients. Data analysis was conducted for means, SDs, frequencies, and percentages. For comparative statistics, t tests and multiple logistic regression models were used.
Results:
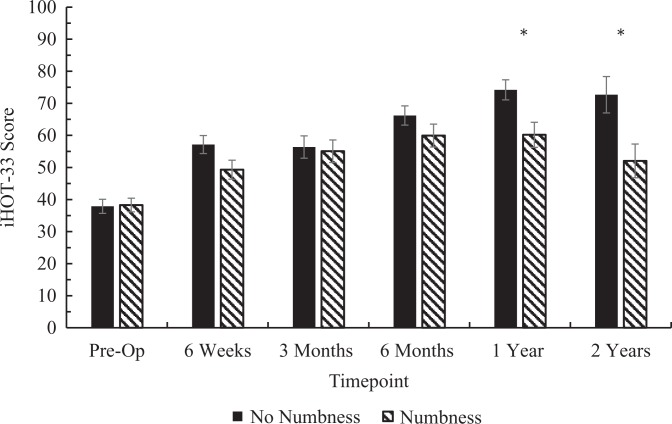
A total of 221 patients (113 male, 108 female; mean age, 39.8 ± 13.34 years) completed the survey out of 362 eligible patients. Overall, 37% (n = 82) of patients reported having experienced some form of numbness after surgery. Approximately 43% (35/82) of the patients reported resolution by 6 weeks postoperatively, and 68% (56/82) of numbness was reported to have completely resolved by 6 months. The duration of surgery was a significant factor for the development of postoperative numbness (P = .010; odds ratio, 2.18) when comparing procedures longer than 50 minutes with procedures shorter than 50 minutes (first incision until closure). Postoperative numbness was associated with a negative effect on the International Hip Outcome Tool–33 (iHOT-33) score that reached statistical significance at the 1-year (numbness, 60.19; no numbness, 74.21; P = .006) and 2-year time points (numbness, 52.04; no numbness, 72.69; P = .01).
Conclusion:
This study confirmed our hypothesis that postoperative numbness is more common in our patient population than the incidence reported in the literature. This adverse event was also shown to be associated with decreased postoperative functional outcomes, as measured by the iHOT-33 at 1 and 2 years postoperatively.
Keywords: numbness, iHOT-33, traction, constrained
Hip arthroscopic surgery is a rapidly growing procedure that is used for the diagnosis and treatment of hip abnormalities. A survey in 2012 showed that there was an 18-fold increase in the number of hip arthroscopic procedures as performed by candidates of the American Board of Orthopaedic Surgery examination between 1999 and 2009.7 However, as a rapidly growing new technique, hip arthroscopic surgery has a unique set of complications.2,4,5,8–14,17,18
The hip joint is an anatomically constrained deep-seated joint with a thick envelope of soft tissues and is surrounded by a group of very powerful muscles. To overcome these anatomic constraints, traction force is usually required to open the joint enough to introduce arthroscopic instruments safely without damaging the labrum or cartilage. One of the most commonly reported postoperative complications is numbness, which is believed to be related to the use of traction during the procedure. The current reported rate of postoperative numbness varies between 1% and 20%.5,14,22–25
The primary objective of this study was to investigate the rate of postoperative numbness in a high-volume tertiary center. We hypothesized that this complication is underreported and is higher than what is reported in the literature. The secondary objectives were to (1) assess the associations of variables that could contribute to the development of this complication and (2) evaluate the effect of postoperative numbness on functional outcomes in this patient population. This study will help address the inconsistencies in the literature and will make recommendations on ways to decrease the incidence of this postoperative complication.
Methods
Patients
Approval was granted by the Nova Scotia Health Authority Research Ethics Board. All patients had previously undergone hip arthroscopic surgery for different diagnoses at the Queen Elizabeth II Health Sciences Centre, Halifax, Nova Scotia. Patients who underwent hip arthroscopic surgery performed by the senior author (I.W.) during the time period of 2012 to 2016 were included and contacted to participate in the study. The patients excluded from the study were those who declined participation as well as those who could not be contacted by telephone. Patients who did not answer after 3 separate telephone calls were also excluded from the study. A telephone survey with a blinded assessor was completed by all patients who consented to participate (Table 1). A chart review was then performed for each survey participant to collect demographic and clinical information related to the arthroscopic procedure. The International Hip Outcome Tool–33 (iHOT-33) scores, which are routinely collected and documented for patients at their postoperative clinic visits, were also acquired from the patients’ charts.
TABLE 1.
Questions Asked During Telephone Interview With Patients
| Did You Have Any Numbness After Surgery? |
|---|
| 1. If yes, where was it located (foot/groin/thigh/other)? |
| a. If it was in the groin, did you have a new sexual dysfunction after surgery? |
| b. Did you have erectile dysfunction that did not exist before surgery? |
| c. Did you have pain during sexual intercourse that did not exist before surgery? |
| 2. When did you first notice the numbness begin after surgery? |
| a. Immediately after surgery |
| b. Within 6 hours |
| c. Within 12 hours |
| d. After 12 hours |
| 3. How long did the numbness last? |
| a. Less than 24 hours |
| b. Up to 1 week |
| c. Up to 6 weeks |
| d. Up to 6 months |
| e. Persistent |
| 4. Has the numbness affected your lifestyle? |
| a. If yes, how? |
Procedure
All patients underwent hip arthroscopic surgery in either the supine or lateral position. There was a change in patient positioning in 2014. Before this time, the surgeon had primarily performed the surgical procedure in the supine position because of available infrastructure and equipment. After 2014, a change in technique to the lateral decubitus position was made, although the surgeon had already been familiar with this position.
In the supine position, the patient was placed on a traction table (Hip Positioning System with Active Heel Technology; Smith & Nephew). The feet were then well padded using foam pads and placed into boots attached to the traction table. The groin was protected with an extra-large perineal post pad (9 inches in diameter). Traction was applied to the operative hip, with countertraction being applied to the nonoperative leg. The operative hip was then distracted by approximately 1 cm to facilitate the atraumatic introduction of the instruments.
In the lateral position, the patient’s operative hip was exposed facing upward. The Hip Positioning System with Active Heel Technology was then attached to the table. The affected limb was placed in the Universal Hip Distractor (Smith & Nephew). The groin was well padded with a perineal post (6 inches in width), and the foot was placed flat and snug in the Active Heel Traction Boot (Smith & Nephew) in neutral alignment. The leg was then moved to approximately 45° of hip abduction for pretensioning. Once adequate pretensioning was achieved, the foot boot was unlocked in rotation, and the hip was adducted to neutral abduction to subluxate the joint and obtain approximately 1 cm of joint distraction. The operative leg was then maintained in slight flexion and placed in 15° of abduction during central compartment work for both patient positions, and traction was released with the operative leg taken to 45° of abduction for peripheral compartment work.
We utilized standard hip arthroscopic portals for the procedures, including anterolateral and midanterior portals. Either ultrasound or a C-arm was used to localize the portals at the beginning of the procedure.
Data Collection
Data collected during the telephone survey included (1) presence of numbness symptoms, (2) location, (3) duration, and (4) previous diagnosis of numbness. Data collected from the chart review included (1) age at the time of surgery, (2) sex, (3) operative position, (4) duration of the surgical procedure (first incision until closure), (5) body mass index (BMI), (6) radiological findings, (7) diagnosis (indication for surgery) and surgical findings, and (8) iHOT-33 scores.
For the purposes of this study, numbness was defined as any change in sensory perception in the lower extremity that was not present preoperatively.
Statistical Analysis
Descriptive analyses were conducted using means and SDs for continuous variables, while frequencies and percentages were used for categorical variables. We then used t tests to compare the means of the continuous variables. Multiple logistic regression models were used to determine the odds ratio of having postoperative numbness for each independent variable while controlling for all of the other variables, with a predetermined significance threshold of 5%.
Results
Out of 362 patients who were eligible for the study, 221 (61.1%) competed the survey. Of the patients who did not complete the questionnaire, 20 (14.2%) were reached and did not wish to participate. The remaining 121 (85.8%) patients either did not have a valid telephone number on file or could not be reached after 3 separate calls. Of the 221 patients who consented to the questionnaire, 113 were male and 108 were female, with a mean age of 39.8 ± 13.34 years. Overall, 37% (n = 82) of patients reported having experienced some form of numbness after surgery (Table 2).
TABLE 2.
Demographics and Clinical Characteristics of Patientsa
| Total (N = 221) | Numbness (n = 82) | No Numbness (n = 139) | |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 113 (51.1) | 38 (33.6) | 75 (66.4) |
| Female | 108 (48.9) | 44 (40.7) | 64 (59.3) |
| Age, y | 39.8 ± 13.34 | 38.9 ± 11.85 | 40.3 ± 14.16 |
| Body mass index, kg/m2 | 26.2 ± 4.68 | 26.2 ± 4.46 | 26.2 ± 4.81 |
| Position in surgery, n (%) | |||
| Supine | 167 (75.6) | 58 (34.7) | 109 (65.3) |
| Lateral | 54 (24.4) | 24 (44.4) | 30 (55.6) |
| Duration of surgery, min | 50.25 ± 14.53 | 53.80 ± 13.86 | 48.25 ± 14.56 |
aData are presented as mean ± SD unless otherwise specified.
Of the 113 male patients included in the study, 38 (33.6%) developed postoperative numbness. Of the 108 female patients included, 44 (40.7%) developed postoperative numbness (Table 2). Table 2 summarizes the demographic information and clinical characteristics for the 2 groups of patients: those with and those without the development of postoperative numbness.
The 2 most common areas of numbness reported were the groin (n = 34) and the anterolateral area of the upper leg (n = 33) (Table 3). This was followed by numbness in the foot (n = 24) and other areas including the knee, calf, gluteal area, and genitalia (n = 9) (Table 3). Approximately 43% (35/82) of the patients reported resolution by 6 weeks postoperatively, and 68% (56/82) of numbness was reported to have completely resolved by 6 months (Table 4). The most common diagnosis in the population was the presence of femoroacetabular impingement (FAI) with a labral tear, which occurred in 183 patients (83%). Two patients underwent surgery for an infection, and 9 patients were reported to have “other indications,” such as avascular necrosis or dysplasia associated with a labral tear.
TABLE 3.
Location of Reported Postoperative Numbnessa
| Location | n (%) |
|---|---|
| Groin | 34 (41.46) |
| Thigh | 33 (40.24) |
| Foot | 24 (29.27) |
| Other (knee, gluteal area, calf) | 9 (10.98) |
aSome patients reported numbness in multiple locations.
TABLE 4.
Duration of Symptoms Postoperatively
| Duration | n (%) |
|---|---|
| 1 wk | 5 (6.1) |
| 6 wk | 30 (36.6) |
| 6 mo | 21 (25.6) |
| >6 mo | 19 (23.2) |
| Intermittent | 7 (8.5) |
Regarding positioning during surgery, 167 patients were operated on in the supine position and 54 in the lateral position. Fifty-eight patients (34.7%) from the supine group developed postoperative numbness as well as 24 patients (44.4%) from the lateral group. However, there was no significant association between the position during surgery and postoperative numbness (P = .25). Of note, 2 patients had preoperative symptoms of numbness.
The mean age at the time of surgery for the numbness group and no numbness group were 38.9 years and 40.3 years, respectively. However, age was not significantly associated with the development of postoperative numbness (P = .290). Overall, 126 patients had a BMI ≥25 kg/m2 (high BMI), and 95 had a BMI <25 kg/m2 (low BMI). In the high BMI group, 50 patients (40%) developed postoperative numbness, and in the low BMI group, 32 patients (34%) developed numbness. This again was not statistically significant (P = .56) (Table 5).
TABLE 5.
Simple and Multiple Logistic Regression Showing the Association Between Postoperative Numbness and Variablesa
| Variable | Unadjusted | Adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Age at surgery | ||||
| <45 y | 0.68 (0.5-1.3) | .195 | 0.72 (0.6-1.5) | .290 |
| ≥45 y | Reference | |||
| Sex | ||||
| Male | 1.35 (1.1-1.9) | .274 | 1.69 (1.2-2.1) | .105 |
| Female | Reference | |||
| Body mass index | ||||
| <25 kg/m2 | 1.17 (1.0-1.5) | .577 | 1.55 (1.2-2.5) | .176 |
| ≥25 kg/m2 | Reference | |||
| Position in surgery | ||||
| Supine | 1.50 (1.3-2.1) | .200 | 1.49 (1.3-2.0) | .252 |
| Lateral | Reference | |||
| Duration of surgery | ||||
| ≥50 min | 1.97 (1.3-2.3) | .016 | 2.18 (1.9-3.2) | .010 |
| <50 min | Reference | |||
| Cam FAI (alpha angle >50°) | ||||
| Present | 2.28 (1.9-2.9) | .040 | 3.77 (2.5-4.5) | .090 |
| Absent | Reference | |||
| Pincer FAI | ||||
| Present | 1.11 (1.1-2.0) | .070 | 1.74 (1.2-2.3) | .120 |
| Absent | Reference | |||
| Both cam and pincer FAI | ||||
| Present | 1.87 (1.3-2.5) | .090 | 1.98 (1.1-2.2) | .210 |
| Absent | Reference | |||
aFAI, femoroacetabular impingement; OR, odds ratio.
The mean duration of hip arthroscopic surgery was 50.25 minutes, with the longest procedure being 105 minutes and the shortest procedure being 13 minutes. The duration of surgery was significantly associated with the development of postoperative numbness after accounting for the other confounding factors in the multiple logistic regression model (P = .01), with an odds ratio of 2.18 (Table 5). This was after comparing surgical procedures that took longer than or equal to 50 minutes with surgical procedures that took less than 50 minutes.
When exploring the association between postoperative numbness and type of FAI, the presence of cam-type FAI was a risk factor, with an odds ratio of 2.28 (P = .04) (Table 5). However, when adjusted for the other variables in the multiple logistic regression model, the presence of cam-type FAI proved to be no longer significant (P = .09).
The mean preoperative iHOT-33 score for all patients was 38.03 (Table 6). At the 2-year postoperative time point, the mean iHOT-33 score had increased to 64.09 (Table 6). The mean iHOT-33 scores were significantly lower for the numbness group compared with the group with no numbness at 1 year (Δ = 14.02; P = .006) and 2 years postoperatively (Δ = 20.65; P = .01) (Figure 1).
TABLE 6.
Mean International Hip Outcome Tool–33 (iHOT-33) Scores at Baseline and Postoperative Time Pointsa
| Total | Numbness | No Numbness | P | |
|---|---|---|---|---|
| Preoperatively | 38.03 | 38.27 | 37.88 | .90 |
| 6 wk | 54.26 | 49.31 | 57.15 | .07 |
| 3 mo | 55.94 | 55.06 | 56.37 | .81 |
| 6 mo | 63.77 | 59.96 | 66.21 | .19 |
| 1 y | 68.20 | 60.19 | 74.21 | .006 |
| 2 y | 64.09 | 52.04 | 72.69 | .01 |
aThe iHOT-33 is graded on a scale ranging from 0 to 100, with 100 representing the best possible score.
Figure 1.
Progression of mean postoperative International Hip Outcome Tool–33 (iHOT-33) scores at 6 weeks, 3 months, 6 months, 1 year, and 2 years after surgery. Error bars denote standard error, and asterisks (*) represent significant difference.
Discussion
There has been significant variability in the literature with regard to the reported rates of postoperative numbness.5,13,19,20,22–25 This could be because of a low overall appreciation of this complication by both surgeons and patients. As a result, patients may not be asked specifically about numbness symptoms or may assume that it is not related to their recent surgery. In our study, the patients were contacted by a blinded assessor and asked specific questions related to numbness symptoms as an extension of the senior author’s practice of routinely assessing numbness preoperatively and postoperatively. We found that in our study population, 37% of patients reported postoperative numbness.
Our results are in agreement with those of Dippmann et al,13 who reported postoperative numbness in 23 of 50 (43%) patients in their study. Their study was prospective in nature, and they evaluated postoperative numbness via a questionnaire offered at 1 year postoperatively about nerve dysfunction symptoms. This rigid study design would have allowed them to capture more patients with numbness symptoms. In a study by Telleria et al,27 the authors used electromyography and nerve conduction monitoring during hip arthroscopic surgery to measure changes in the sciatic nerve, and they reported significant changes in 58% of the patients during hip arthroscopic surgery. Although the majority were subclinical changes, they only monitored the sciatic nerve. Had they monitored the other nerves around the hip joint, their rate could have been increased even further.27 In our study, the majority (68%) of the patients’ symptoms had resolved by 6 months. This is in agreement with most reports that describe postoperative numbness as typically a transient phenomenon that resolves over time.3,5,13,15,16
The literature reports that obesity generally increases the risk of complications after hip arthroscopic surgery.6 However, our study found that obesity was not a risk factor for the development of postoperative numbness. This result is in agreement with that of Pailhé et al.24 We also did not find that positioning during the procedure was a risk factor for the development of postoperative numbness. This is contrary to the finding in the review by de Sa et al,11 which reported a higher rate of postoperative numbness in the supine position compared with the lateral position. This discrepancy in the literature could be related to the fact that the majority of the reported hip arthroscopic procedures were performed in the supine position versus the lateral decubitus position, as was shown in our study (75.6% vs 24.4%, respectively) and that of de Sa et al11 (63.2% vs 36.8%, respectively). In the future, a more rigid comparative study design with more homogenous groups could better control the issue of surgical position with respect to differences in outcomes.
Our results showed that the duration of the procedure (first incision until closure) was a significant factor in the development of postoperative numbness, with an odds ratio of 2.18. As a result, the patients with longer surgery times were more likely to develop postoperative numbness. This finding is in agreement with those of other reports in the trauma literature such as Kao et al,19 who reviewed pudendal nerve palsy after intramedullary nailing of femoral fractures and found that patients who developed palsy had a longer overall surgical time. However, other reports in the trauma and sports medicine literature have suggested that the amount of traction rather than the duration in traction is the important factor.1,24,26,27 Others, such as Mallet et al,21 have suggested that the amount of anesthetic relaxation is the most important factor.
Based on our review of the literature, we believe that all these factors contribute to the development of postoperative numbness and that they should be considered together when trying to lower the rate of this adverse outcome. Even though we did not study the amount of traction or the level of anesthetic in our study, it is clinically logical that prolonged traction and compression on the nerve tissue will lead to nerve dysfunction postoperatively. Some authors have developed techniques to perform the procedure without a perineal post, such as utilizing the effect of friction between the body and the table in the Trendelenburg position or placing a bean bag around the trunk to hold the body instead of the post.22,23 These techniques may lower the rate of postoperative numbness; however, they have yet to be proven reproducible in large-scale studies without increasing the risk of iatrogenic injuries to the labrum or cartilage.
Our study also showed that the patients with postoperative numbness had overall lower functional outcomes as measured by the iHOT-33 during the routine follow-ups, and this reached statistical significance at the 1- and 2-year time points. Although the iHOT-33 is not validated to specifically evaluate for postoperative numbness complications, common secondary effects of numbness include pain along the nerve distribution of the affected site, and some male patients may develop erectile dysfunction related to pudendal nerve palsy. Both of these related complications are covered within the validated iHOT-33 questionnaire.
The strengths of this study are that it is one of the few that explicitly address postoperative numbness. Further, our patients were specifically asked about symptoms of numbness postoperatively through a prospective survey design by a blinded assessor, with the results being blinded to the surgeon. Our study has a large number of patients compared with other reports. The senior author utilized 2 different surgical positions during the study period, which was useful for comparison in relation to the primary outcome.
The limitations of our study include the 61.1% response rate to our survey, which could have been biased toward those who experienced postoperative numbness, as they could have been more invested in completing a survey about the complications that they were experiencing. Also, because we used a telephone survey, it was difficult to determine if the numbness could have been related to factors other than the traction force, such as lateral thigh numbness related to the portal incision, without physically examining the patients.
Second, we used surgical time as a whole (first incision until closure), whereas in reality, part of that time was used to perform cam resection work, which is usually done with minimal to no traction applied to the leg; however, because of the retrospective nature of the study, the duration of the procedure was taken as is from the medical record. Yet, by accounting for the full surgical time, our data and results represent a real-world situation and suggest how quickly the procedure should be performed to minimize the risk of postoperative numbness.
We did not measure the amount of traction applied to the leg, which can differ significantly between patients. Also, we did not collect any information related to the amount of relaxation given by anesthesia, which could have an effect on the amount of traction required to distract the joint. Last, because of the change in positions, there was a decrease in the size of the perineal post from 9 to 6 inches in the supine to lateral positions, respectively. This could act as an independent factor affecting the rate of numbness postoperatively, although we believe that there was a reduced learning curve between the techniques, as the surgeon had already been familiar with both positioning styles. Future studies with prospective designs will allow for the control of these variables.
Conclusion
Our study showed that within our patient population, postoperative numbness was more common than has been reported in the literature. Although not generalizable to all patients, it suggests that postoperative numbness could be similarly underreported within larger populations. This adverse event was also shown to significantly affect postoperative functional outcomes as measured by the iHOT-33 at the 1- and 2-year time points. Of all the factors studied, duration of the surgical procedure was found to be a risk factor for the development of postoperative numbness. As a result, we suggest that decreasing the operative time in hip arthroscopic surgery is critical in reducing the incidence of postoperative numbness. Future comparative prospective studies with rigid designs are required to further examine this outcome and other potential risk factors that could lead to the development of postoperative numbness.
Acknowledgment
The authors thank Nicole Paquet, Jalisa Den Hartog, and Ryland Murphy for article preparation and editing and Swagata Ghosh for assistance with the statistical analysis.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the Nova Scotia Health Authority Research Ethics Board.
References
- 1. Brumback RJ, Ellison TS, Molligan H, Molligan DJ, Mahaffey S, Schmidhauser C. Pudendal nerve palsy complicating intramedullary nailing of the femur. J Bone Joint Surg Am. 1992;74(10):1450–1455. [PubMed] [Google Scholar]
- 2. Burrus MT, Cowan JB, Bedi A. Avoiding failure in hip arthroscopy: complications, pearls, and pitfalls. Clin Sports Med. 2016;35(3):487–501. [DOI] [PubMed] [Google Scholar]
- 3. Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res. 2010;468(3):741–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ciemniewska-Gorzela K, Piontek T, Szulc A. Abdominal compartment syndrome: the prevention and treatment of possible lethal complications following hip arthroscopy. A case report. J Med Case Rep. 2014;8(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Clarke MT, Arora A, Villar RN. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res. 2003;(406):84–88. [DOI] [PubMed] [Google Scholar]
- 6. Collins JA, Beutel BG, Garofolo G, Youm T. Correlation of obesity with patient-reported outcomes and complications after hip arthroscopy. Arthroscopy. 2015;31(1):57–62. [DOI] [PubMed] [Google Scholar]
- 7. Colvin AC, Harrast J, Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94(4):e23. [DOI] [PubMed] [Google Scholar]
- 8. Contreras MEK, Hoffmann RB, de Araújo LCT, Dani WS, José Berral F. Complications in hip arthroscopy. Rev Bras Ortop. 2010;45(1):61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Curtin B, Friebe I. Dermal burn during hip arthroscopy. Orthopedics. 2014;37:e746–e749. [DOI] [PubMed] [Google Scholar]
- 10. Degen RM, O’Sullivan E, Sink EL, Kelly BT. Psoas tunnel perforation: an unreported complication of hip arthroscopy. J Hip Preserv Surg. 2015;2(3):272–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. de Sa D, Stephens K, Parmar D, et al. A comparison of supine and lateral decubitus positions for hip arthroscopy: a systematic review of outcomes and complications. Arthroscopy. 2016;32(4):716–725. [DOI] [PubMed] [Google Scholar]
- 12. Dietrich F, Ries C, Eiermann C, Miehlke W, Sobau C. Complications in hip arthroscopy: necessity of supervision during the learning curve. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):953–958. [DOI] [PubMed] [Google Scholar]
- 13. Dippmann C, Thorborg K, Kraemer O, Winge S, Hölmich P. Symptoms of nerve dysfunction after hip arthroscopy: an under-reported complication? Arthroscopy. 2014;30(2):202–207. [DOI] [PubMed] [Google Scholar]
- 14. Elsaidi GA, Ruch DS, Schaefer WD, Kuzma K, Smith BP. Complications associated with traction on the hip during arthroscopy. J Bone Joint Surg Br. 2004;86(6):793–796. [DOI] [PubMed] [Google Scholar]
- 15. Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15(2):132–137. [DOI] [PubMed] [Google Scholar]
- 16. Funke EL, Munzinger U. Complications in hip arthroscopy. Arthroscopy. 1996;12(2):156–159. [DOI] [PubMed] [Google Scholar]
- 17. Harris JD, McCormick FM, Abrams GD, et al. Complications and reoperations during and after hip arthroscopy: a systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29(3):589–595. [DOI] [PubMed] [Google Scholar]
- 18. Ilizaliturri VM. Complications of arthroscopic femoroacetabular impingement treatment: a review. Clin Orthop Relat Res. 2009;467(3):760–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kao JT, Burton D, Comstock C, McClellan RT, Carragee E. Pudendal nerve palsy after femoral intramedullary nailing. J Orthop Trauma. 1993;7(1):58–63. [DOI] [PubMed] [Google Scholar]
- 20. Kim SJ, Choi NH, Kim HJ. Operative hip arthroscopy. Clin Orthop Relat Res. 1998;(353):156–165. [DOI] [PubMed] [Google Scholar]
- 21. Mallet R, Tricoire JL, Rischmann P, Sarramon JP, Puget J, Malavaud B. High prevalence of erectile dysfunction in young male patients after intramedullary femoral nailing. Urology. 2005;65(3):559–563. [DOI] [PubMed] [Google Scholar]
- 22. Mei-Dan O, McConkey MO, Young DA. Hip arthroscopy distraction without the use of a perineal post: prospective study. Orthopedics. 2013;36(1):e1–e5. [DOI] [PubMed] [Google Scholar]
- 23. Merrell G, Medvecky M, Daigneault J, Jokl P. Hip arthroscopy without a perineal post: a safer technique for hip distraction. Arthroscopy. 2007;23(1):1–3. [DOI] [PubMed] [Google Scholar]
- 24. Pailhé R, Chiron P, Reina N, Cavaignac E, Lafontan V, Laffosse J-M. Pudendal nerve neuralgia after hip arthroscopy: retrospective study and literature review. Orthop Traumatol Surg Res. 2013;99(7):785–790. [DOI] [PubMed] [Google Scholar]
- 25. Schindler A, Lechevallier J, Rao N, Bowen R. Diagnostic and therapeutic arthroscopy of the hip in children and adolescents: evaluation of results. J Pediatr Orthop. 1995;15:317–321. [DOI] [PubMed] [Google Scholar]
- 26. Sharfman ZT, Amar E, Tsvieli O, Alkrinawi N, Levy O, Rath E. Complications of hip arthroscopy: patient perspectives. Orthop Nurs. 2016;35(4):208–213. [DOI] [PubMed] [Google Scholar]
- 27. Telleria JJ, Safran MR, Harris AH, Gardi JN, Glick JM. Risk of sciatic nerve traction injury during hip arthroscopy: is it the amount or duration? An intraoperative nerve monitoring study. J Bone Joint Surg Am. 2012;94(22):2025–2032. [DOI] [PubMed] [Google Scholar]