Abstract
Background
Teamwork in the operating theatre is becoming increasingly recognized as a major factor in clinical outcomes. Many tools have been developed to measure teamwork. Most fall into two categories: self‐assessment by theatre staff and assessment by observers. A critical and comparative analysis of the validity and reliability of these tools is lacking.
Methods
MEDLINE and Embase databases were searched following PRISMA guidelines. Content validity was assessed using measurements of inter‐rater agreement, predictive validity and multisite reliability, and interobserver reliability using statistical measures of inter‐rater agreement and reliability. Quantitative meta‐analysis was deemed unsuitable.
Results
Forty‐eight articles were selected for final inclusion; self‐assessment tools were used in 18 and observational tools in 28, and there were two qualitative studies. Self‐assessment of teamwork by profession varied with the profession of the assessor. The most robust self‐assessment tool was the Safety Attitudes Questionnaire (SAQ), although this failed to demonstrate multisite reliability. The most robust observational tool was the Non‐Technical Skills (NOTECHS) system, which demonstrated both test–retest reliability (P > 0·09) and interobserver reliability (Rwg = 0·96).
Conclusion
Self‐assessment of teamwork by the theatre team was influenced by professional differences. Observational tools, when used by trained observers, circumvented this.
Introduction
The past decade has seen a dramatic shift in understanding of surgical performance and outcomes. In addition to surgeons' technical proficiency, non‐technical skills have been implicated in clinical outcomes after surgery and operating theatre efficiency. These non‐technical skills include, in addition to teamwork, attitudes towards safety, situational awareness, decision‐making, communication and theatre environment1, 2, 3, 4, 5, 6, 7, 8, 9, 10. This review was designed to focus on teamwork. Therefore, tools that did not explicitly claim to involve teamwork metrics in their measurement were not considered.
A variety of tools with varying degrees of validity and reliability exist. They fall broadly into two categories: self‐assessment by operating theatre staff and direct observation of the theatre team by others. Without a widely accepted method of quantifying teamwork within the operating theatre, it is difficult to evaluate teamwork in a consistent and comparable manner.
A number of problems exist when attempting to quantify teamwork. A comprehensive definition has not been agreed, reflecting the variations in content and approach to measuring teamwork. Pragmatic factors such as cost and practicality may influence whether one tool is selected over another for clinical purposes. However, selected tools should be valid and reliable. Theoretically, comprehensive tools are not useful scientifically if invalid or unreliable when tested in unsimulated environments; nor can validity or reliability be sacrificed for ease of implementation and cost. Although previous authors11 12 have commented on the validity and reliability of teamwork tools, none has focused specifically on teamwork in the operating theatre. This is an important distinction to make, as many authors would agree that teamwork measures a set of processes that are specific to a situation. To align with this definition, this study presents a more targeted and focused approach by excluding studies that relate to, for example, simulated settings or military trauma.
Methods
Search strategy
The search strategy was completed according to the PRISMA recommendations for systematic reviews13 (Fig. 1). The Ovid search engine was used to interrogate the MEDLINE and Embase databases using the following individual search strategies. MEDLINE: (*patient care team/ or teamwork.mp. or cumulative experience.mp.) and (surg*.mp. or operation op * operating rooms/ma) and (quality indicators, health care/ or complications.mp. or outcomes.mp. or safety.mp. or performance.mp. or mortality.mp.). EMBASE: (teamwork/ or cumulative experience.mp.) and (surg*.mp. or operating room/ or surgery/ or operation.mp.) and (health care quality/ or complications.mp. or safety.mp. or outcomes.mp. or performance.mp. or mortality.mp.). The reference lists of included articles were searched for additional studies. Two independent reviewers assessed the titles and abstracts of all identified articles to determine eligibility. Eligible studies were assessed in full with a third reviewer if information retrieved from the titles and abstracts was insufficient to determine inclusion. A fourth independent reviewer was responsible for resolving any dispute in initial study inclusion/exclusion.
Figure 1.
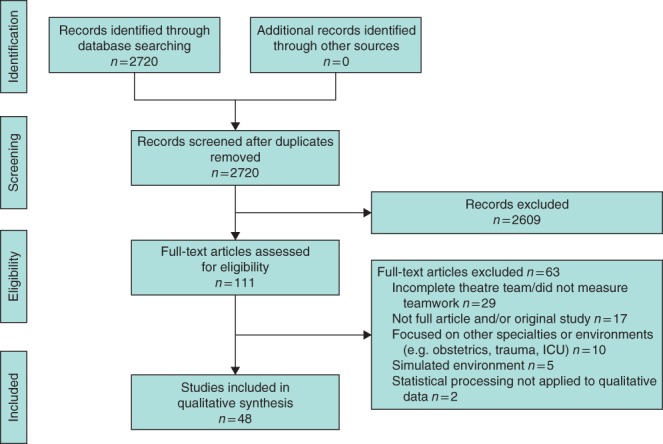
Flow diagram showing selection of articles for review
Study selection
The papers were selected for review based on the following inclusion criteria: original paper; English version obtainable; focuses on measurement of teamwork as defined by the authors themselves; includes statistical processing of data related to measurement of teamwork (for quantitative studies); and investigates operating theatre teams. The following exclusion criteria were applied: abstract only; no statistical processing of data related to measurement of teamwork (for quantitative studies); teamwork not assessed holistically (for example, choosing to investigate communication only); and involves teamwork outside the operating theatre. Authors independently reviewed articles and all queries were resolved.
Data of interest
Data that were extracted and synthesized for analysis included: first author, aim of the study, study design, country of origin, setting and specialty, use of crew resource management, number of teams, size of teams, number of surgical procedures, teamwork intervention used, duration/frequency of intervention, number of surgeons, experience of surgical team, outcome measures (mortality, morbidity, team efficiency, duration of operation, ‘never’ events, team opinions, teamwork quality), and feedback provision. All included articles were read in full to evaluate the methods used by authors to show content validity, predictive validity, reliability between test sites, and reliability between observers for observational tools. Only sections of tools relating to teamwork, as defined by the creators of each tool, were analysed. Other fields that may comprise part of a broader tool, such as the job satisfaction domain of the Safety Attitudes Questionnaire (SAQ), were not taken into account.
Analysis
Study characteristics and outcomes were summarized and contrasted using descriptive methods. Critical assessments of content validity, predictive validity and concurrent validity were made. Although largely subjective14, content validity was deemed to be of greater value in tools that had shown high internal agreement or evidence of translation from other fields as opposed to simple transposition. Predictive validity was judged by the impact of training on teamwork scores, that is whether one can predict whether staff had undergone team training from scores registered before and after intervention. Concurrent validity is displayed with statistical correlation with other factors thought to be related to teamwork. Tools were also deemed to be more valid if multiple facets of validity were displayed. Statistical measures of inter‐rater agreement (Rwg and Cohen's κ) and inter‐rater reliability (intraclass coefficient, ICC) were also compared. Non‐significant scores across time intervals or institutions were taken as markers of test–retest reliability. Heterogeneity in study design and variation in outcome, population and setting precluded meta‐analysis. Therefore, a predominantly qualitative approach was adopted.
Results
Of 2720 citations, 48 articles were included for review. Studies were published between 2002 and 2015, encompassing 59 306 patients and 13 453 staff at 228 sites. These articles comprised 24 cross‐sectional studies, 21 prospective studies, one retrospective and two qualitative studies (Tables 1 and 2).
Table 1.
Teamwork measurement tools using self‐assessment
| Tool | Design | Content validity | Predictive validity | Concurrent validity | Test–retest reliability |
|---|---|---|---|---|---|
| Teamwork climate of SAQ2 3, 15, 16, 17, 18, 19, 20, 21 | Likert scale survey | Developed from FMAQ, used in aviation. Psychometric basis, minimal alterations Cronbach's α = 0·78 for a sample of items on the SAQ teamwork scale (same profession, same site)3 | Scores were better in the site that had received teamwork training compared with one that had not2 | Correlation with theatre efficiency17 | No, two sites had a significantly different baseline score2 |
| TeamSTEPPS questionnaire4 | Likert scale survey | As part of government‐ sponsored TeamSTEPPS programme | Scores improved after TeamSTEPPS training | No | n.r. |
| MTTQ22 | Likert scale survey | Statistical method of factor analysis | No | No | No, different sites had significantly different MTTQ responses (P < 0·001) |
| ORMAQ23 | Likert scale survey | Adapted from aviation and other languages by 3 surgeons | No | No | n.r. |
| Study‐specific survey1 | Likert scale survey | Claims validated, unable to find method of validation | Teamwork scores of surgeons and anaesthetists improved after team training; those of nurses did not | No | n.r. |
| Study‐specific survey5 | Yes/no responses | No | Increased perceptions of teamwork after training | No | n.r. |
| Study‐specific survey9 | Two parts: yes/no and Likert scale survey | Based on literature review | After safety checklist implementation, greater proportion of surgeons reported positive teamwork events | No | n.r. |
| Study‐specific survey24 | Likert scale survey | Input from orthopaedic surgeons, anaesthetists, ICU and physicians | Improved perceptions of teamwork after perioperative checklist implementation | No | n.r. |
| Study‐specific survey25 | Free‐text answers calculated into score out of 5 | No | No | No | n.r. |
| Study‐specific survey26 | Self reporting of statements taken from observational tools | Survey items translated from observational tools (NOTSS and ANTS) | No | No | n.r. |
SAQ, Safety Attitudes Questionnaire; FMAQ, Flight Management Attitudes Questionnaire; TeamSTEPPS, Team Strategies and Tools to Enhance Performance and Patient Safety; n.r., not reported; MTTQ, Medical Team Training Questionnaire; ORMAQ, Operating Room Management Attitudes Questionnaire; NOTSS, Non‐technical Skills for Surgeons; ANTS, Anaesthetists' Non‐Technical Skills.
Table 2.
Teamwork measurement using direct observation
| Tool | Design | Content validity | Predictive validity | Concurrent validity | Test–retest reliability | Inter‐rater reliability (ICC) and agreement (κ, Rwg) |
|---|---|---|---|---|---|---|
| NOTECHS27, 28, 29, 30, 31, 32, 33 | Scale: observed behaviours | Translated from aviation by theatre experts and human factors experts27 |
Improved scores after team training (P = 0·005)27
Improved scores after team and systems training (P = 0·025)33 |
Expected and observed correlation with glitch rate (P = 0·045)28 | 0·09 < P < 0·64 across 5 sites (non‐significant variation)28 Non‐significant variation across different time intervals27 | Rwg = 0·9627 ICC = 0·73–0·8828 |
| OTAS10 34, 35, 36, 37, 38, 39, 40 | Checklist: tasks and scale: observed behaviours | Theatre and human factors experts involved in development | No | Adverse correlation between impact of distractions and completion of patient‐related tasks (P < 0·050)6 10 | n.r. | Cohen's κ > 0·4034 Pearson's coefficient = 0·7138 ICC = 0·42–0·9040. In German operating theatres: κ > 0·40 in 70% of scale items, ICC = 0·78–0·8939 |
| SO‐DIC‐OR41 | Checklist: observed behaviours | Representative sample of theatre team involved in development | No | No | n.r. | Cohen's κ = 0·74–0·95 including for ‘tired’ observers |
| Coding of field notes42 | Scale: impact of coded field notes | No | No | No | n.r. | No, each observer had a different role |
| Mayo‐HPTS43 44 | Checklist: tasks and scale: behaviours | Validated for crew resource management44 | Improved scores after team training (P = 0·01) | No | n.r. | Cohen's κ = 0·46–0·9743 |
| METEOR45 | Checklist: tasks | Scale items verified by agreement between theatre experts | No | No | n.r. | Observers ‘calibrated’ until Cohen's κ > 0·70 Observer agreement for cases n.r. |
| NOTSS40 46 | Scale: behaviours | Theatre experts involved in development | No | Good correlation with Cannon‐Bowers scale32 | n.r. | ICC = 0·12–0·8347 |
| Cannon‐Bowers46 48 | Literature review | Based on psychological theory | No | Good correlation with NOTSS | n.r. | Cronbach's α = 0·80 |
| HFRS‐M47,49 | Scale: behaviours | Took elements of LOSA checklist for aviation | Briefing workshops and simulation had no significant effect on scores | No | n.r. | Cronbach's α = 0·8947 |
| Study‐specific survey7 | Scale: observed behaviours | Based on behavioural markers | No | No | n.r. | Observers ‘calibrated’ Rwg = 0·85 after training. Observer agreement for cases n.r. |
| Study‐specific survey50 | Checklist: coded events | Based on previously validated tool for assessing mental fitness and concerns | No | No | n.r. | Cohen's κ = 0·77 |
ICC, intraclass coefficient; NOTECHS, Non‐Technical Skills; OTAS, Observational Teamwork Assessment for Surgery; SO‐DIC‐OR, Simultaneous Observation of Distractions and Communication in the Operating Room; Mayo‐HPTS, Mayo High Performance Teamwork Score; METEOR, Metric for Evaluating Task Execution in the Operating Room; NOTSS, Non‐technical Skills for Surgeons; HFRS‐M, Modified Human Factors Rating Scale; LOSA, Line Oriented Safety Audit.
Self‐assessment methods
Self‐assessment tools were used in 18 studies across 194 sites (Table 1). The most popular tool was the teamwork subsection or ‘climate’ of the SAQ2 3, 15, 16, 17, 18, 19, 20.
Content validity
A number of tools contained evidence of content validity, although the SAQ was the only one that demonstrated high internal agreement by users (Cronbach's α = 0·78)3. The SAQ also had the benefit of translation from a well validated tool used in aviation, a feature shared with the Operating Room Management Attitudes Questionnaire (ORMAQ). However, adaptations to the operating theatre were largely semantic11 16, 51. Tools had also been borrowed from other medical specialties including the TeamSTEPPS training4, medical team training22, and ICU and trauma24, although none exhibited convincing adaptation to the operating room specifically. Some studies did not demonstrate content validity5 25.
Predictive validity
Although statistically significant improvements in SAQ scores were demonstrated after teamwork training2, this finding was not reproduced in all studies18 20, 21. Other tools showed improvement in teamwork scores after training and implementation of a surgical safety checklist4 5, 9 24, although the improvements were not always seen in representatives of the nursing profession1.
Concurrent validity
SAQ scores correlated with theatre efficiency, but not with an independent scoring system for communication3 17.
Reliability
The SAQ did not appear reliable in retest conditions, with significant differences in scores across institutions and across time intervals without intervention2. Similarly, the Medical Team Training Questionnaire (MTTQ) also did not display test–retest reliability across different institutions22.
A number of studies1 5, 15 16, 19 22, 23 showed that perceptions of teamwork varied between the professions that constitute the operating team. For example, surgeons rated the teamwork of their theatre colleagues higher than that of anaesthetists or nurses15. This finding was present regardless of the assessment method. Furthermore, members of each profession tended to give the highest ratings of teamwork to their own profession11 15. All forms of self‐assessed scores for teamwork included some form of questionnaire or survey, many of which were based on a Likert scale. The response rate to these surveys varied from 45 to 87 per cent (Table 3). For studies using the SAQ, mean response rates varied from 52 to 87 per cent.
Table 3.
Reported response rates for self‐assessment of teamwork
Methods of direct observation
Twenty‐eight studies quantified teamwork using direct observation (Table 2). The two most commonly used tools were the Observational Teamwork Assessment for Surgery (OTAS)34, 35, 36, 37, 38, 39 52 and the Non‐Technical Skills (NOTECHS) system27, 28, 29, 30, 31, 32, 33.
Content validity
NOTECHS benefited from development from a previously well validated tool used in aviation27, whereas another method was developed from a tool for assessing mental fitness50. The majority of the observational tools had been developed using theatre experts, or adapted from existing tools by theatre experts. Exceptions include the Mayo High Performance Teamwork Score (HPTS) and the Modified Human Factors Rating Scale (HFRS‐M), which comprised elements taken directly from crew resource management without translation44 47, 49, and the Cannon‐Bowers scale based on psychological theory46 48. NOTECHS has also been validated in vascular, orthopaedic and general surgery27 28, 31. OTAS also shows evidence of validation in multiple specialties, having been tested in urology, vascular and general surgery, and in operating theatres in Germany34 36, 39.
Predictive validity
NOTECHS consistently demonstrated highly significant improvement in teamwork scores after teamwork training27 33. The only other observational tool to demonstrate predictive validity was the Mayo‐HPTS, which also showed statistically significant improvements after team training44. Team training and simulation did not have any significant effect on HFRS‐M scores49.
Concurrent validity
NOTECHS scores correlated inversely with ‘glitch rate’, whereas OTAS scores inversely correlated with the impact of distractions6 10. NOTSS and the Cannon‐Bowers scale correlated well with each other40 46, 48.
Test–retest reliability
NOTECHS was the only tool to demonstrate reliability when tested across different sites and different time intervals27 28.
Inter‐rater reliability and agreement
NOTECHS showed superior statistical measures of inter‐rater reliability (ICC = 0·73–0·88)28, with relatively small ranges in the statistical measures of inter‐rater reliability, compared with OTAS (ICC = 0·42–0·90)40 and NOTSS (ICC = 0·12–0·83)47. Inter‐rater agreement was strong for NOTECHS (Rwg = 0·96)27, Simultaneous Observation of Distractions and Communication in the Operating Room (SO‐DIC‐OR) (κ = 0·74–0·90) and a study‐specific survey (κ = 0·77)50, but less strong for OTAS (κ > 0·40) and Mayo‐HPTS (κ > 0·46).
Qualitative studies
Two studies used structured interviews with a combined total of seven surgeons, 25 nurses and eight anaesthetists. One study produced ethnographic field notes on 35 procedures. ‘Differences in professional culture’ between surgeons, anaesthetists and nurses was identified as a major influence in team communication53. Operating theatre staff also implicated the ‘role of the institution’ in teamwork and communication. Perceived barriers to effective teamwork included a lack of ‘open communication’ and ‘dominance and hierarchy’54. Field notes of observed communication exchanges in the operating theatre showed themes such as ‘mimicry’ (for example, junior surgeons mimicking the behaviours of fellows and consultant), ‘withdrawal’ (typically juniors withdrawing from tense communication between other team members), and ‘association’ (attitudes towards a certain individual being extended to members of their professional subteam)54.
Discussion
As far as validity and reliability were concerned, NOTECHS was the most valid and reliable observational tool for measuring teamwork. The NOTECHS score also demonstrated predictive validity, concurrent validity, superior test–retest reliability and superior inter‐rater reliability28. NOTECHS has been used across a range of specialties including general, vascular and orthopaedic surgery27 28, 31. It was adapted from a synonymous, well accepted score used in aviation, which has roots in psychological theory55. The changes between the aviation NOTECHS and the operating theatre NOTECHS involved the input of surgical, anaesthetic and nursing experts27.
OTAS has been validated in urology, vascular surgery and general surgery36. Its content, like that of NOTECHS, has contributions from psychological and clinical expertise. Despite this, a proportion of OTAS components (behaviours or tasks) were consistently not witnessed in practice12 36, 37. After translation to German operating theatres, inter‐rater agreement also remained poor (κ < 0·40 in 30 per cent of tool items)39. This may be explained by suboptimal team performance, but also casts doubt on its content validity and tool reliability. There was no evidence for the predictive validity of OTAS, and no evidence of test–retest reliability.
Several important limitations of self‐reported tools have been identified. It is difficult to obtain a meaningful score for the whole team. Studies consistently showed that assessment of the teamwork of colleagues, and of the whole team, was different for each profession1 5, 11 15, 16 22. Participants tended to rate their own specialty the highest on scales of communication and teamwork. Assuming honest ratings not coloured by factionism, this suggests that each profession has different ideas of what comprises good teamwork. Qualitative studies have identified ‘differences in professional culture’ as a major influence on teamwork53. The frequent occurrence of behaviours such as ‘mimicry’ and ‘association’ substantiate this. Junior staff belonging to a specialty often mimic the negative teamwork behaviours of their seniors, and members of other specialties associate juniors with negative traits of seniors54. It appears challenging for individuals in theatre subteams adequately to assess themselves and their colleagues from other professions.
Self‐assessed methods of teamwork appear to be greatly influenced by the site at which the work was done. Two studies2 22 showed significantly different scores at different sites, and no other studies reported on this subject. This may be an example of failure to show test–retest reliability. Otherwise, if the difference in perceived teamwork between sites was true, it can be better described by the difference in the pattern of responses, not the absolute score. In this case, self‐assessment is suitable for qualitative investigation of interactions between team members, but not useful as an overall quantifier of teamwork. Either self‐assessment tools are unreliable, or they are more useful in qualitative assessment.
The relative abundance of operating room nurses and scarcity of anaesthetists presents a further problem for self‐assessment of teamwork. Of the studies included, the combined ratio of nurses to surgeons to anaesthetists was roughly 3 : 2 : 1 (Table S1, supporting information). Consequently, a simple arithmetic combination of scores from each profession would over‐represent nursing perspectives and under‐represent anaesthetic perspectives. Problems with sampling were also evident, as shown by the wide range of response rates between studies, and between sites within a study. The lack of sampling methods could allow studies to have an inherent bias, self‐selecting for individuals with an interest in teamwork.
A valid tool measures accurately and precisely what it is designed to measure in the real world. Broadly, there are three types of validity relevant to this review: content validity, predictive validity and concurrent validity. A tool is deemed to have content validity if it actually measures what it was intended to measure in a given content. This remains largely a qualitative judgement despite attempts to quantify it14. Many authors have attempted to show content validity by involving psychological experts and operating theatre experts.
In the traditional sense, a tool has predictive validity if it can be used to make reasonable predictions based on what it measures. However, teamwork in the operating theatre is not proven to have causal relationships with other measurable variables. One must first establish causation between teamwork and another variable before going back to ascertain whether a tool that measures teamwork also has predictive validity for that variable. At this stage, true predictive validity for teamwork relating to other variables cannot be demonstrated. However, by considering scores before and after training, the presence or absence of training may be inferred if a tool shows predictive validity. Concurrent validity is similar to predictive validity, but the variable that is correlated to teamwork is happening at the same time.
Any tool deemed to be reliable must show test–retest reliability. As such, scores should not be affected by testing at different sites or in different time intervals without intervention. In addition, observational tools must show reliability between raters/observers. This is different from inter‐rater agreement. Raters can agree exactly on a test, but unreliably so; likewise, raters may reliably disagree over their observations. The studies employed a variety of statistical tools to examine these issues (Table 2). Rwg and Cohen's κ are measures of inter‐rater agreement; ICC values provide an estimate of reliability between raters.
Some studies focused on a single‐specialty approach to validity, perhaps on the premise that teamwork was not only situation‐dependent (operating theatre as opposed to emergency teams), but also task‐dependent. There was no evidence that requirements for teamwork varied by surgical specialty. As OTAS and NOTECHS have been validated in multiple specialties, there is evidence to the contrary27 29, 30 35.
A common shortcoming was that some tools that have been validated in other settings were directly transferred to the operating theatre environment without adaptation or validity testing. Common settings included: crew resource management43 47, 49, medical as opposed to surgical teams4 22, ICU and trauma24. Some authors1 5, 9 25, 42 used study‐specific tools without reporting processes of development and validation.
Furthermore, statistical tests must be applied appropriately. For example, Pearson's coefficient, although used by authors38 for quantifying correlation between raters for teamwork, is a tool for estimating correlations between variables that do not share a metric and variance, and, therefore, inappropriate for use to correlate observations of two raters on the same score56 57.
Meta‐analysis was not attempted and heterogeneity of the different tools limits the conclusions of this review. Within these limitations, it seems that the ideal tool should employ trained observers, must be valid for the operating theatre and reliable between observers, specialties and sites. So far, the tool closest to fulfilling these criteria is the NOTECHS. Future research might aim to demonstrate its reliability for longer procedures, similar to the SO‐DIC‐OR.
Supporting information
Table S1 Self‐assessment responses by staff profession
Acknowledgements
P.M. has worked extensively on NOTECHS, but without influence on the methodology used in this analysis or interpretation of the results.
Disclosure: The authors declare no other conflict of interest.
Funding information
No funding information has been provided
References
- 1. Awad SS, Fagan SP, Bellows C, Albo D, Green‐Rashad B, De La Garza M et al Bridging the communication gap in the operating room with medical team training. Am J Surg 2005; 190: 770–774. [DOI] [PubMed] [Google Scholar]
- 2. Bleakley A, Boyden J, Hobbs A, Walsh L, Allard J. Improving teamwork climate in operating theatres: the shift from multiprofessionalism to interprofessionalism. J Interprof Care 2006; 20: 461–470. [DOI] [PubMed] [Google Scholar]
- 3. Davenport DL, Henderson WG, Mosca CL, Khuri SF, Mentzer RM. Risk‐adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions. J Am Coll Surg 2007; 205: 778–784. [DOI] [PubMed] [Google Scholar]
- 4. Forse RA, Bramble JD, McQuillan R. Team training can improve operating room performance. Surgery 2011; 150: 771–778. [DOI] [PubMed] [Google Scholar]
- 5. Halverson AL, Anderrson JL, Anderson K, Lombardo J, Park CS, Rademaker AW et al Surgical team training. Arch Surg 2014; 144: 107–112. [DOI] [PubMed] [Google Scholar]
- 6. Healey AN, Primus CP, Koutantji M. Quantifying distraction and interruption in urological surgery. Qual Saf Health Care 2007; 16: 135–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mazzocco K, Petitti DB, Fong K, Bonacum D, Brookey J, Graham S et al Surgical team behaviors and patient outcomes. Am J Surg 2009; 197: 678–685. [DOI] [PubMed] [Google Scholar]
- 8. Neily J, Mills PD, Young‐Xu Y, Carney B, West P, Berger DH et al Implementation of a medical team training program and the effect on surgical mortality. JAMA 2010; 304: 1693–1700. [DOI] [PubMed] [Google Scholar]
- 9. Papaconstantinou HT, Jo C, Reznik SI, Smythe WR, Wehbe‐Janet H. Implementation of a surgical safety checklist: impact on surgical team perspectives. Ochsner J 2013; 13: 299–309. [PMC free article] [PubMed] [Google Scholar]
- 10. Sevdalis N, Undre S, McDermott J, Giddie J, Diner L, Smith G. Impact of intraoperative distractions on patient safety: a prospective descriptive study using validated instruments. World J Surg 2014; 38: 751–758. [DOI] [PubMed] [Google Scholar]
- 11. Whittaker G, Abboudi H, Khan MS, Dasgupta P, Ahmed K. Teamwork assessment tools in modern surgical practice: a systematic review. Surg Res Pract 2015; 2015: 494827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dietz A, Provonost P, Benson K, Mendez‐Tellez PA, Dwyer C, Wyskiel R et al A systematic review of behavioural marker systems in healthcare: what do we know about their attributes, validity and application? BMJ Qual Saf 2014; 23: 1031–1039. [DOI] [PubMed] [Google Scholar]
- 13. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group . Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med 2009; 151: 264–269. [DOI] [PubMed] [Google Scholar]
- 14. Smith GT. On construct validity: issues of method and measurement. Psychol Assess 2005; 17: 396–408. [DOI] [PubMed] [Google Scholar]
- 15. Makary MA, Sexton JB, Freischlag J, Holzmueller CG, Millman EA, Rowen L et al Operating room teamwork among physicians and nurses: teamwork in the eye of the beholder. J Am Coll Surg 2006; 202: 746–752. [DOI] [PubMed] [Google Scholar]
- 16. Sexton JB, Makary MA, Tersigni A, Pryor D, Hendrich A, Thomas EJ et al Teamwork in the operating room: frontline perspectives among hospitals and operating room personnel. Anesthesiology 2006; 105: 877–884. [DOI] [PubMed] [Google Scholar]
- 17. Stepaniak PS, Heij C, Buise MP, Mannaerts GHH, Smulders JF, Nienjuijs SW. Bariatric surgery with operating room teams that stayed fixed during the day: a multicenter study analyzing the effects on patient outcomes, teamwork and safety climate, and procedure duration. Anesth Analg 2012; 115: 1384–1392. [DOI] [PubMed] [Google Scholar]
- 18. Wolf FA, Way LW, Stewart L. The efficacy of medical team training: improved team performance and decreased operating room delays. Ann Surg 2010; 128: 71–80. [DOI] [PubMed] [Google Scholar]
- 19. Carney BT, West P, Neily J, Mills PD, Bagian JP. Differences in nurse and surgeon perceptions of teamwork: implications for use of a briefing checklist in the OR. AORN J 2010; 91: 722–729. [DOI] [PubMed] [Google Scholar]
- 20. Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AHS, Delinger EP et al; Safe Surgery Saves Lives Study Group. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist‐based surgical safety intervention. BMJ Qual Saf 2011; 20: 102–107. [DOI] [PubMed] [Google Scholar]
- 21. Kawano T, Taniwaki M, Ogata K, Sakamoto M, Yokoyama M. Improvement of teamwork and safety climate following implementation of the WHO surgical safety checklist at a university hospital in Japan. J Anesth 2014; 28: 467–470. [DOI] [PubMed] [Google Scholar]
- 22. Mills P, Neily J, Dunn E. Teamwork and communication in surgical teams: implications for patient safety. J Am Coll Surg 2008; 206: 107–112. [DOI] [PubMed] [Google Scholar]
- 23. Flin R, Yule S, McKenzie L, Paterson‐Brown S, Maran N. Attitudes to teamwork and safety in the operating theatre. Surgeon 2006; 4: 145–151. [DOI] [PubMed] [Google Scholar]
- 24. Böhmer AB, Wappler F, Tinschmann T, Kindermann P, Rixen D, Bellendir M et al The implementation of a perioperative checklist increases patients perioperative safety and staff satisfaction. Acta Anaesthesiol Scand 2012; 56: 332–338. [DOI] [PubMed] [Google Scholar]
- 25. Berenholtz S, Schumacher K, Hayanga AJ, Simon M, Goeschel C, Provonost P et al Briefings and debriefings at a large regional medical center. Jt Comm J Qual Patient Saf 2009; 35: 391–397. [DOI] [PubMed] [Google Scholar]
- 26. Wauben LSGL, Doorn CMDV, Wijngaarden JDHV, Goossens RHM, Huijsman R, Klein J et al Discrepant perceptions of communication, teamwork and situation awareness among surgical team members. Int J Qual Health Care 2011; 23: 159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mishra A, Catchpole K, McCulloch P. The Oxford NOTECHS System: reliability and validity of a tool for measuring teamwork behaviour in the operating theatre. Qual Saf Health Care 2009; 18: 104–108. [DOI] [PubMed] [Google Scholar]
- 28. Robertson ER, Hadi M, Morgan LJ, Pickering SP, Collins G, New S et al Oxford NOTECHS II: a modified theatre team non‐technical skills scoring system. PLoS One 2014; 9: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Catchpole K, Mishra A, Handa A, McCulloch P. Teamwork and error in the operating room: analysis of skills and roles. Ann Surg 2008; 247: 699–706. [DOI] [PubMed] [Google Scholar]
- 30. Catchpole KR, Dale TJ, Hirst DG, Smith JP, Giddings TA. A multicenter trial of aviation‐style training for surgical teams. J Patient Saf 2010; 6: 180. [DOI] [PubMed] [Google Scholar]
- 31. Morgan L, Hadi M, Pickering S, Robertson E, Griffin D, Collins G et al The effect of teamwork training on team performance and clinical outcome in elective orthopaedic surgery: a controlled interrupted time series study. BMJ Open 2015; 5: e006216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Morgan L, Pickering S, Hadi M, Robertson E, New S, Griffin D et al A combined teamwork training and work standardisation intervention in operating theatres: controlled interrupted time series study. BMJ Qual Saf 2015; 24: 111–119. [DOI] [PubMed] [Google Scholar]
- 33. McCulloch P, Morgan L, New S, Catchpole K, Robertson E, Hadj AM et al Combining systems and teamwork approaches to enhance the effectiveness of safety improvement interventions in surgery. Ann Surg 2015; 265: 90–96. [DOI] [PubMed] [Google Scholar]
- 34. Hull L, Arora S, Kassab E, Kneebone R, Sevdalis N. Observational teamwork assessment for surgery: content validation and tool refinement. J Am Coll Surg 2011; 212: 234–243.e5. [DOI] [PubMed] [Google Scholar]
- 35. Healey AN, Undre S, Vincent CA. Developing observational measures of performance in surgical teams. Qual Saf Health Care 2004; 13(Suppl 1): i33–i40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Undre S, Sevdalis N, Healey AN, Darzi A, Vincent C. Observational Teamwork Assessment for Surgery (OTAS): refinement and application in urological surgery. World J Surg 2007; 31: 1373–1381. [DOI] [PubMed] [Google Scholar]
- 37. Undre S, Healey AN, Darzi A, Vincent C. Observational assessment of surgical teamwork: a feasibility study. World J Surg 2006; 30: 1774–1783. [DOI] [PubMed] [Google Scholar]
- 38. Hull L, Arora S, Kassab E, Kneebone R, Sevdalis N. Assessment of stress and teamwork in the operating room: an exploratory study. Am J Surg 2011; 201: 24–30. [DOI] [PubMed] [Google Scholar]
- 39. Passauer‐Baierl S, Hull L, Miskovic D, Russ S, Sevdalis N, Weigl M. Re‐validating the Observation Teamwork Assessment for Surgery tool (OTAS‐D): cultural adaptation, refinement and psychometric evaluation. World J Surg 2014; 38: 305–313. [DOI] [PubMed] [Google Scholar]
- 40. Phitayakorn R, Minehart R, Pian‐Smith MCM, Hemingway MW, Milosh‐Zinkus T, Oriol‐Morway D et al Practicality of intraoperative teamwork assessments. J Surg Res 2014; 190: 22–28. [DOI] [PubMed] [Google Scholar]
- 41. Seelandt JC, Tschan F, Keller S, Beldi G, Jenni N, Kurmann A et al Assessing distractors and teamwork during surgery: developing an event‐based method for direct observation. BMJ Qual Saf 2014; 23: 918–929. [DOI] [PubMed] [Google Scholar]
- 42. Christian CK, Gustafson ML, Roth EM, Sheridan TB, Gandhi TK, Dwyer K et al A prospective study of patient safety in the operating room. Surgery 2006; 139: 159–173. [DOI] [PubMed] [Google Scholar]
- 43. Gettman MT, Pereira CW, Lipsky K, Wilson T, Arnold JJ, Leibovich BC et al Use of high fidelity operating room simulation to assess and teach communication, teamwork and laparoscopic skills: initial experience. J Urol 2009; 181: 1289–1296. [DOI] [PubMed] [Google Scholar]
- 44. Malec JF, Torsher LC, Dunn WF, Wiegmann DA, Arnold JJ, Brown DA et al The mayo high performance teamwork scale: reliability and validity for evaluating key crew resource management skills. Simul Healthc 2007; 2: 4–10. [DOI] [PubMed] [Google Scholar]
- 45. Russ S, Arora S, Wharton R, Wheelock A, Hull L, Sharma E et al Measuring safety and efficiency in the operating room: development and validation of a metric for evaluating task execution in the operating room. J Am Coll Surg 2013; 216: 472–481. [DOI] [PubMed] [Google Scholar]
- 46. Pugh CM, Cohen ER, Kwan C, Cannon‐Bowers J. A comparative assessment and gap analysis of commonly used team rating scales. J Surg Res 2014; 190: 445–450. [DOI] [PubMed] [Google Scholar]
- 47. Moorthy K, Munz Y, Adams S, Pandey V, Darzi A. A human factors analysis of technical and team skills among surgical trainees during procedural simulations in a simulated operating theatre. Ann Surg 2005; 242: 631–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cannon‐Bowers JA, Bowers C. Team development and functioning In APA Handbook of Industrial and Organizational Psychology. Building and Developing the Organization, Vol 1, Zedeck S. (ed.). American Psychological; Association: Washington, DC, 2010. [Google Scholar]
- 49. Koutantji M, McCulloch P, Undre S, Gautama S, Cunniffe S, Sevdalis N et al Is team training in briefings for surgical teams feasible in simulation? Cogn Technol Work 2008; 10: 275–285. [Google Scholar]
- 50. Schraagen JM, Schouten T, Smit M, Haas F, van der Beek D, van de Ven J et al Assessing and improving teamwork in cardiac surgery. Qual Saf Health Care 2010; 19: e29. [DOI] [PubMed] [Google Scholar]
- 51. Thomas EJ, Sexton JB, Laksy RE, Helmreich RL, Crandell DS, Tyson J. Teamwork and quality during neonatal care in the delivery room. J Perinatol 2006; 26: 163–169. [DOI] [PubMed] [Google Scholar]
- 52. Healey AN, Undre S, Sevdalis N, Koutantji M, Vincent C. The complexity of measuring interprofessional teamwork in the operating theatre. J Interprof Care 2006; 20: 485–495. [DOI] [PubMed] [Google Scholar]
- 53. Gillespie BM, Chaboyer W, Longbottom P, Wallis M. The impact of organisational and individual factors on team communication in surgery: a qualitative study. Int J Nurs Stud 2010; 47: 732–741. [DOI] [PubMed] [Google Scholar]
- 54. Gillespie BM, Gwinner K, Chaboyer W, Fairweather N. Team communications in surgery – creating a culture of safety. J Interprof Care 2013; 27: 387–393. [DOI] [PubMed] [Google Scholar]
- 55. Flin R, Martin L, Goeters K, Hormann H, Amalberti R, Nijhuis H. Development of the NOTECHS (non‐technical skills) system for assessing pilots' CRM skills. Hum Factors Aerosp Saf 2003; 3: 95–117. [Google Scholar]
- 56. Hallgren KA. Computing inter‐rater reliability for observational data: an overview and tutorial. Tutor Quant Methods Psychol 2012; 8: 23–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. LeBreton JM, Senter JL. Answers to 20 questions about interrater reliability and interrater agreement. Organ Res Methods 2008; 11: 815–852. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Self‐assessment responses by staff profession


