Abstract
Mushroom poisoning is a rare cause of acute kidney injury. Here, we present a case with presumed Amanita nephrotoxic syndrome, a first of its kind from the Indian subcontinent.
Keywords: Acute kidney injury, amatoxin, hemodialysis, mushroom
Introduction
Mushroom poisoning or mycetism is a perennial problem in Northeast India where mushroom hunting and foraging in the wild is popular, especially in rural areas. Most mushroom gatherers in this region have no formal training in identifying poisonous and nonpoisonous mushrooms. They largely depend on experience and traditional wisdom passed on over generations to differentiate between edible and nonedible-mushrooms. Usually, the collection is based on a number of species that are identified with confidence. Perhaps, a hundred mushroom species or more cause symptoms when ingested; of which only about fifty or so species worldwide are potentially fatal. The majority of mushroom poisonings occur due to misidentification as edible variety. Poisoning may also occur after deliberate ingestion of hallucinogenic mushrooms such as Amanita muscaria.
Worldwide, amatoxin-containing mushrooms account for >95% of mushroom poisoning-related deaths. These include mushrooms of the genera - Amanita, Galerina, and Lepiota. Many of these deaths are attributed to Amanita phalloides, commonly referred to as death caps.[1] Amatoxin mushrooms cause severe liver damage with an exponential rise in hepatic transaminase values and coagulopathy. Such poisonings remain commonplace in Northeast India with hundreds of recorded deaths in Assam over the past century, including dozens in just the last decade alone.
Irreversible nephrotoxic mushroom poisonings from the consumption of orellanine-containing mushrooms of the Cortinarius species result in the so-called “Orellanus syndrome”, which is characterized by progressive rise in serum urea nitrogen and creatinine levels along with decreasing urine output leading to a dialysis-dependent end-stage renal disease.
Over the past two decades, there have been several reports of nephrotoxic Amanita species poisonings in North America (Amanita smithiana) and Europe (Amanita proxima in France, Amanita solitaria in Germany, etc.) characterized by a mild transaminitis with subsequent development of acute kidney injury (AKI). The subjects required temporary dialysis which later recovered completely.[1,2,3] The toxin in these nephrotoxic Amanita cases has been definitively identified as allenic norleucine.[4] Heretofore, there have been no reports of nephrotoxic Amanita poisonings from the Indian subcontinent. Here, we report a case of foraged mushroom ingestion in Northeast India causing a temporary dialysis-dependent renal failure that meets the clinical criteria for nephrotoxic allenic norleucine Amanita poisoning.
Case Report
A 52-year-old male without significant medical history was admitted to a rural hospital in Meghalaya with recurrent vomiting and oliguria that begun 10–12 h following consumption of wild mushrooms collected from a nearby forest. The mushrooms were cooked in soup and eaten consumed for lunch and dinner the same day. Beginning 10–12 h after the first meal, he had multiple episodes of vomiting which eventually responded to injected antiemetics at the local hospital. He was provided intravenous hydration, but urine output remained poor and he became progressively weaker. He was transferred to North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences in Shillong, Meghalaya the following day. He had no history of long-term medications, herbal supplements, or fish gall bladder consumption. No other family members had consumed the same mushroom; the patient consumed the mushroom in his workplace. On arrival to the emergency department, he was conscious and oriented, but weak and lethargic. Blood pressure was 110/70 mmHg, and respiratory rate was 20/min. He maintained normal oxygen saturation on room air and was afebrile. Urine output over the first 24 h was only 50 ml.
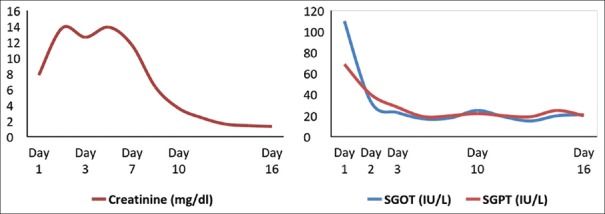
Investigations confirmed AKI with liver dysfunction [Figure 1]. Blood counts, arterial blood gas, and international normalized ratio were normal. Ultrasound revealed normal-sized kidneys with increased cortical echogenicity without evidence of obstruction. He was fluid resuscitated with Ringer's lactate and dextrose in normal saline at 200–300 ml/h. He was also given oral pyridoxine (50 mg/day), silymarin (840 mg/day), ursodeoxycholic acid (600 mg/day), and folinic acid (5 mg/day).
Figure 1.
Graphs showing serial measurements of serum creatinine, serum glutamic oxaloacetic transaminase and serum glutamic pyruvic transaminase during hospital stay. SGOT: Serum glutamic oxaloacetic transaminase, SGPT: Serum glutamic pyruvic transaminase
Twenty-four hours after admission, urine output remained poor (100 ml/24 h) and serum urea nitrogen and creatinine levels increased to 166 mg/dl and 13.8 mg/dl, respectively, despite aggressive intravenous hydration [Figure 1]. Liver enzymes returned to normal. Hemodialysis was performed on the 2nd, 5th, and 8th day post-admission. Urine output began to improve on day 4 followed by progressive improvement in renal biochemistry. On day 15, he was discharged with fully recovered renal functions.
Discussion
Delayed renal failure following ingestion of wild mushrooms is typically attributed to mushrooms containing the toxin orellanine as in Cortinarius species such as Cortinarius orellanus (Fool's Webcap) and Cortinarius rubellus (Deadly Webcap). Recently, Amanita species that do not contain amatoxin have been implicated in poisonings resulting in acute kidney injury.[2] These nephrotoxic Amanitas include A. proxima in France and A. smithiana in North America. There are essential differences in both the clinical picture and especially the prognosis of poisonings due to these Amanitas as compared to the Cortinarius species.
Cortinarius species poisonings result in a delayed onset renal failure, which is often preceded by gastrointestinal symptoms. Patients present after an extremely long latency of 3–21 days following ingestion. This asymptomatic period is followed by gastrointestinal symptoms that include vomiting and diarrhea, followed by oliguric renal failure. In 2001, in a review of literature of mushroom poisonings due to Cortinarius species, Danel et al. described a mean delay of 3 days to the onset of gastrointestinal symptoms after ingestion of Cortinarius mushrooms.[5] The gastrointestinal symptoms were followed by acute kidney injury (mean of 8.5 days). Patients experienced excessive thirst and polyuria, ultimately followed by oliguria or anuria. AKI progressed to end-stage renal disease requiring permanent dialysis or kidney transplant. Recovery of milder cases required several months.
Nephrotoxic Amanita ingestion produces gastrointestinal symptoms 20 min–24 h following ingestion, with oliguric renal failure developing within 1–6 days. Mild transaminase elevation is typical.[1,2] AKI is characterized by interstitial nephritis on renal biopsy and resolves over weeks. Allenic norleucine has been isolated from these fungi and accounts for their nephrotoxicity.[4]
The clinical course of our patient bears striking resemblance to poisonings caused by A. proxima and A. smithiana. Unfortunately, the mushroom itself was not identified as description of the physical characteristics of the mushroom by the patient was vague, and no samples were provided. Ischemic acute tubular necrosis was a potential differential diagnosis; however, a biopsy was not performed. Syndrome similar to this Amanita nephrotoxicity has been reported with ingestion of fish gallbladder of grass carp variety in Assam and elsewhere.[6]
Mushroom poisoning is an unrecognized public health crisis in India, especially in the northeast region. It remains vastly underreported in medical literature even though many such cases get reported in local newspapers. Common poisonous mushroom species identified from India are mostly Amanita species followed by Galerina, Lepiota and Conocybe genera, however, it is often impossible to precisely identify the offending mushrooms, especially when no specimen is provided.[7,8,9] There are few expert mycologists and laboratories capable of positively identifying toxins. In such resource-limited circumstances, it is essential for clinicians to maintain a high index of suspicion of mycetism.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Graeme KA. Mycetism: A review of the recent literature. J Med Toxicol. 2014;10:173–89. doi: 10.1007/s13181-013-0355-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirchmair M, Carrilho P, Pfab R, Haberl B, Felgueiras J, Carvalho F, et al. Amanita poisonings resulting in acute, reversible renal failure: New cases, new toxic Amanita mushrooms. Nephrol Dial Transplant. 2012;27:1380–6. doi: 10.1093/ndt/gfr511. [DOI] [PubMed] [Google Scholar]
- 3.West PL, Lindgren J, Horowitz BZ. Amanita smithiana mushroom ingestion: A case of delayed renal failure and literature review. J Med Toxicol. 2009;5:32–8. doi: 10.1007/BF03160979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garber I. Detection of Allenic Norleucine from Amanita smithiana Mushrooms. [Last accessed on 2017 Apr 21]. Available from: https://www.msacl.org/2014_EU_slides/201408221709_21104_slides.pdf .
- 5.Danel VC, Saviuc PF, Garon D. Main features of Cortinarius spp. poisoning: A literature review. Toxicon. 2001;39:1053–60. doi: 10.1016/s0041-0101(00)00248-8. [DOI] [PubMed] [Google Scholar]
- 6.Bhattacharyya PC, Nayak M, Barkataky A. Acute renal failure following consumption of fish gall bladder. Indian J Nephrol. 2009;19:161–2. doi: 10.4103/0971-4065.59339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verma N, Bhalla A, Kumar S, Dhiman RK, Chawla YK. Wild mushroom poisoning in North India: Case series with review of literature. J Clin Exp Hepatol. 2014;4:361–5. doi: 10.1016/j.jceh.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma SK, Aggarwal A, Pal LS, Bansal SK, Devichand P, Puri DS. Mushroom (Amanita phalloides) poisoning with special reference to serum enzyme levels. J Indian Med Assoc. 1980;75:213–7. [PubMed] [Google Scholar]
- 9.Sharma J, Malakar M, Sandiguria E, Das J. An expressive study of mushroom poisoning cases in Lakhimpur district of Assam. Int J Adv Res Technol. 2013;2:82–8. [Google Scholar]