Abstract
A case of left distal forearm and wrist osteolipoma in a 56 year old female is reported. The patient presented with a 3 year history of nontender left wrist mass. Radiographs demonstrated a lobulated mass of mixed low density and calcifications, not adjacent to and with no connection to underlying bone. Ultrasound showed a spheroid hyperechoic lesion with internal heterogeneity and rim of calcifications. Magnetic resonance imaging revealed a lesion with predominantly fat characteristics on T1 weighted and T2 weighted sequences, with rim of peripheral calcification and specks of internal calcification. Histological examination after excision of the mass showed the lesion to be an osteolipoma. Osteolipoma is a rare variant of lipoma with osseous metaplasia and should be considered in the differential of a fat containing mass with ossification.
KEYWORDS: Adipocytic neoplasm, forearm, lipoma, ossifying lipoma, osteolipoma

INTRODUCTION
Lipomas are the most frequent soft-tissue tumors, predominantly occurring in subcutaneous regions of upper back, neck, shoulder, and abdomen. They typically consist of mature adipose tissue without cellular atypia. However, other mesenchymal elements such as smooth muscle, fibrous, chondral, or osseous tissue can sometimes be found.[1]
Lipoma that contains mature osseous elements is termed osteolipomas. They most frequently occur in the head and neck regions. It is rare for a lipoma with no connection to bone to contain mature osseous tissue.[2] Here, we describe a case of an osteolipoma in the forearm with no connection to underlying bony structures.
CASE REPORT
A 56-year-old Chinese female patient presented with a mass at volar side of the left wrist. She had first noticed the mass 3 years ago, progressively increasing in size. She did not experience any pain or numbness over the mass or at a level distal to it.
Clinical examination showed a 3 cm × 7 cm mass over a volar region of the left wrist and distal forearm. The mass was firm in nature and the borders were well defined. It was not fixed to overlying skin or underlying structures. The mass was not tender and Tinel's sign was negative. Ranges of movement of left wrist, fingers, and thumb were full.
Initial radiograph revealed a lobulated mass at the subcutaneous region of left volar forearm and wrist, of mixed low density and calcifications [Figure 1]; the lesion showed no connection to the underlying radius or ulna, nor was it located right adjacent to the bony structures. Ultrasound showed a spheroid hyperechoic lesion with internal heterogeneity, located at a perimuscular location close to the flexor digitorum muscles [Figure 2]. It measures 3.1 cm × 1.3 cm × 6.7 cm in size. A continuous rim of echogenicity with posterior shadowing was seen, corresponding to the calcifications. Differential diagnosis at this stage was myositis ossificans.
Figure 1.

Lateral x-ray of the left wrist shows a mass with internal calcifications at volar aspect of left distal forearm. The low density of the lesion on radiograph likely signifies a lesion that is fat-predominant.
Figure 2.

Ultrasound reveals a spheroid hyperechoic lesion with internal heterogeneity. A continuous hyperechoic rim with posterior shadowing is present, suggestive of calcifications, and is in keeping with x-ray findings.
Magnetic resonance imaging (MRI) revealed a T1- and T2-weighted hyperintense lesion at volar aspect of left distal forearm [Figures 3 and 4] situated deep to the fascia and compressing on the flexor digitorum superficialis and flexor carpi radialis muscles. Again, no connection with underlying forearm bones was depicted. The lesion demonstrated hypointense signal on fat suppression sequence. A rim of calcification was seen surrounding the lesion and with specks of internal calcification. The preoperative differential diagnosis included a lipoma with tumoral calcinosis and possibility of liposarcoma cannot be excluded.
Figure 3.
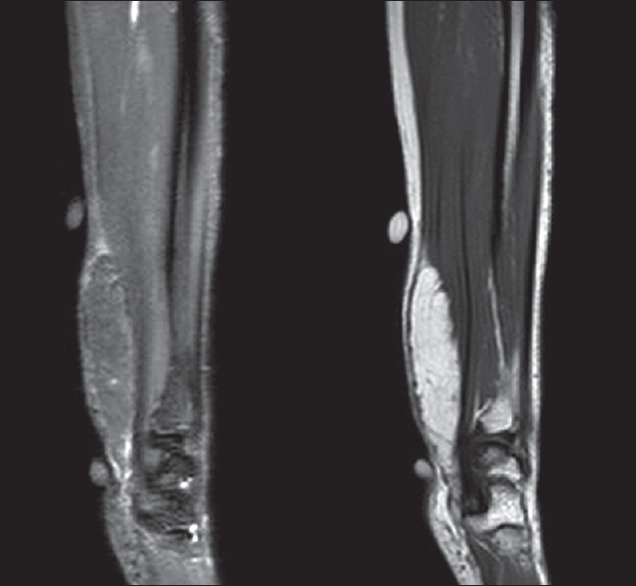
MRI T2-weighted fat suppressed sequence (left) and T1-weighted sequence (right). A well-demarcated T1 hyperintense lesion is noted compressing on the flexor digitorum superficialis and flexor carpi radialis muscles. The lesion shows fat suppression.
Figure 4.

MRI examination with T1-weighted post-gadolinium sequence in sagittal view. The fat-contaning lesion shows no significant contrast enhancement. No invasion into adjacent muscles detected.
Excision of the mass was performed. Intraoperatively, the mass was found below subcutaneous layer, sitting on the pronator quadratus muscle [Figure 5]. Its proximal end was 6 cm proximal to the wrist joint, and distally it extended into the carpal tunnel. The mass was well defined; there was no invasion to surrounding muscles. Blunt dissection was carried out. The procedure was uneventful.
Figure 5.
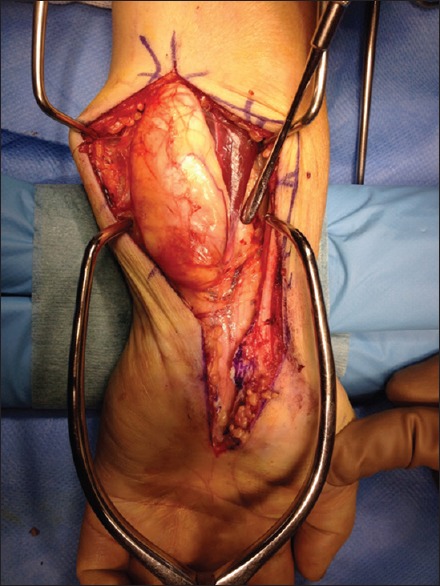
Intraoperative photograph showing a well-demarcated oval tumour.
Gross examination of the resected specimen demonstrated a 2 cm × 2.7 cm × 6 cm nodular piece of fatty tissue with smooth surface. Cut surfaces showed focal calcified areas, and the noncalcified areas showed fatty tissues without necrosis. Histological examination revealed adipose tissues with a few foci of ossification [Figure 6]. There was no definite lipoblast or features of malignancy. The pattern was consistent with an osteolipoma.
Figure 6.
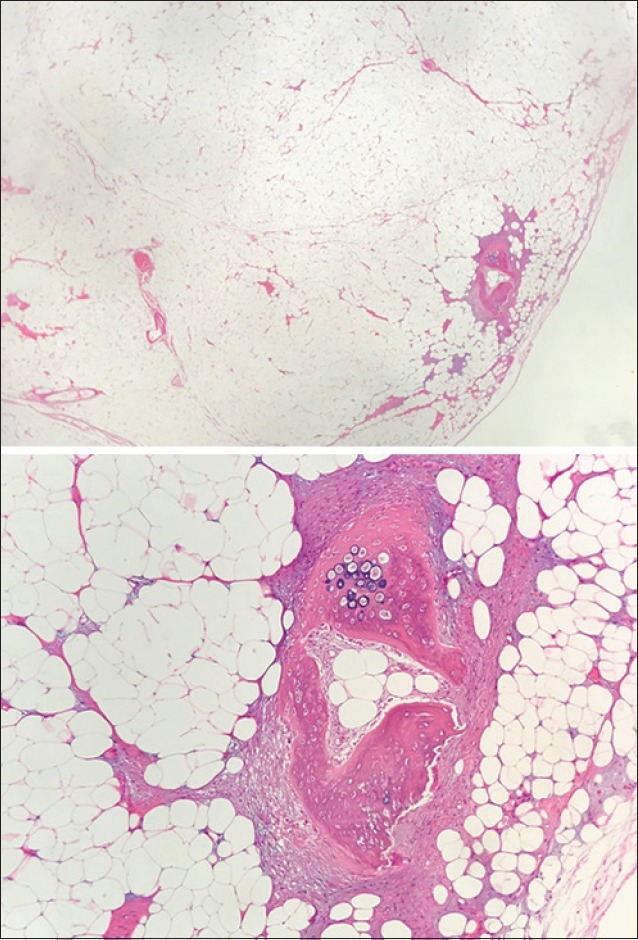
Histological views of the osteolipoma. The tumour consists of adipose tissues with a few foci of ossification. Lipoblasts are not present and there is no feature of malignancy.
DISCUSSIONS
In the World Health Organization (WHO) classification of soft tissue and bone tumors, there are 13 types of adipocytic tumors, and lipoma is the most common soft-tissue mesenchymal neoplasm in adults. Conventional lipoma is composed of mature adipocytes; the cells are identical to the surrounding adipose tissue except for slight variation in the size and shape. However, lipomas can occasionally have areas consisting of other mesenchymal elements, for example, cartilage (chondrolipoma), fibrous tissue (fibrolipoma), or extensive myxoid change (myxolipoma).[3]
According to the WHO description, lipomas with osseous metaplasia are referred to as osteolipomas,[3] and they are a rare variant of lipomas. Other authors have subclassified the lesion into “osteolipoma” or “ossifying lipoma:” if the fat component is predominant, the tumor is named ossifying lipomas; the term osteolipomas are used in a lesion without a predominant fat component.[4]
In a series of 635 lipomas seen over a 5-year period, only six cases contained ossifications.[5] Most prior reports of adipocytic tumor with osseous elements have had some connection to bones, which are termed parosteal lipomas. Parosteal lipomas are benign neoplasms of mature adipose tissues that are contiguous with underlying periosteal bones, commonly associated with reactive changes in the underlying cortex.[6] In contrast, about 10 cases of osteolipoma cases without bone connection are reported in the literature, as in our case.
The pathogenesis of osteolipoma remains unknown, although two main theories have been proposed. The first theory suggests that these tumors may originate directly from multipotent mesenchymal cells. However, the favored hypothesis now is secondary ossification arising from repetitive trauma, metabolic changes, or ischemia, leading to metaplasia of preexisting fibrous elements within the lipoma to develop into osteoblasts.[1,7,8]
The trabeculated bone in osteolipomas can be shown well on plain radiographs. The list of differentials for a low-density lesion with internal ossification detected on plain films can be long, which include parosteal lipoma, myositis ossificans, and tumoral calcinosis. Further, imaging with computed tomography (CT) and MRI will be helpful. Myositis ossificans is a benign process characterized by heterotopic ossification within large muscles. Tumoral calcinosis is a familial condition characterized by solitary or multiple painless, periarticular soft-tissue masses which are calcified.[9] Fat-attenuating density surrounding the ossifications/calcifications would not be present in both differentials.
On CT, osteolipomas are well defined and homogenous. The hypodense areas of fat have similar attenuation to adjacent adipose tissues, which are surrounded by hyperdense layers of calcification. On MRI, osteolipomas are discrete, encapsulated, homogenous fatty masses with similar signal intensity to adjacent subcutaneous fat on all sequences.[1] A fat suppression sequence would be beneficial. The other differential diagnosis for a lipomatous tumor with ossification would be a well-differentiated liposarcoma. Imaging features that may favor malignancy include large size, deep location in soft tissues, internal thickened septa, presence of nodular nonadipose regions, contrast enhancement, and decreased proportion of fat composition.[10]
Definitive diagnosis of osteolipoma is made by histopathological examination, which would reveal a tumor with diffuse, mature ossification within fatty tissues. The mature bone tissue is usually irregular in distribution. The bone spicules are surrounded by fibrous tissue bands.[1]
Osteolipomas have the same favorable prognosis as plain lipomas. The recommended treatment is surgical excision, and no recurrence has been reported.[7]
CONCLUSION
Osteolipomas are rare but have characteristic radiological and pathological appearances. It is important to keep this differential in mind when a lesion containing fatty tissue with ossification is encountered.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. Arthur King Hay Ma (Department of Orthopaedics and Traumatology, Tuen Mun Hospital, Hong Kong) and Dr. Amanda Nim Chi Kan (Department of Clinical Pathology, Tuen Mun Hospital, Hong Kong) for their assistance and contribution.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2018/8/1/20/231905.
REFERENCES
- 1.Demiralp B, Alderete JF, Kose O, Ozcan A, Cicek I, Basbozkurt M, et al. Osteolipoma independent of bone tissue: A case report. Cases J. 2009;2:8711. doi: 10.4076/1757-1626-2-8711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pandit HG, Bhosale PB, Khubchandani S. Ossifying lipoma of the thigh (a case report) J Postgrad Med. 1989;35:54–6. [PubMed] [Google Scholar]
- 3.Fletcher CD, Bridge JA, Hogendoorn PC, Mertens F, editors. In: WHO Classification of Tumours of Soft Tissue and Bone. 4th ed. Lyon: IARC Press; 2013. Adipocytic tumours; pp. 19–43. [Google Scholar]
- 4.Vanhoenacker FM, Parizel PM, Gielen JL, editors. In: Imaging of Soft Tissue Tumors. 4th ed. Berlin, Heidelberg, New York: Springer; 2017. Ossifying lipoma and osteolipoma; p. 221. [Google Scholar]
- 5.Allen PW. New York: Masson Publication USA; 1981. Tumors and Proliferations of Adipose Tissue. [Google Scholar]
- 6.Murphey MD, Johnson DL, Bhatia PS, Neff JR, Rosenthal HG, Walker CW, et al. Parosteal lipoma: MR imaging characteristics. AJR Am J Roentgenol. 1994;162:105–10. doi: 10.2214/ajr.162.1.8273646. [DOI] [PubMed] [Google Scholar]
- 7.Cheng S, Lu SC, Zhang B, Xue Z, Wang HW. Rare massive osteolipoma in the upper part of the knee in a young adult. Orthopedics. 2012;35:e1434–7. doi: 10.3928/01477447-20120822-35. [DOI] [PubMed] [Google Scholar]
- 8.Fritchie KJ, Renner JB, Rao KW, Esther RJ. Osteolipoma: Radiological, pathological, and cytogenetic analysis of three cases. Skeletal Radiol. 2012;41:237–44. doi: 10.1007/s00256-011-1241-0. [DOI] [PubMed] [Google Scholar]
- 9.Olsen KM, Chew FS. Tumoral calcinosis: Pearls, polemics, and alternative possibilities. Radiographics. 2006;26:871–85. doi: 10.1148/rg.263055099. [DOI] [PubMed] [Google Scholar]
- 10.Huynh TV, Cipriano CA, Hagemann IS, Friedman MV. Osteolipoma of the knee. Radiol Case Rep. 2017;12:124–9. doi: 10.1016/j.radcr.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]


