Abstract
Objectives
FTO rs9939609 variant has been shown to be associated with insulin resistance in Caucasian children. However, studies in Asia show inconsistent findings. We investigated the association between FTO rs9939609 polymorphisms and insulin resistance in obese female adolescents in Indonesia, a genetically distinct group within Asia.
Results
A total of 78 obese female adolescents participated in this study. The risk allele (A) frequency of FTO rs9939609 variant in Indonesian obese female adolescence was 44.2%. The frequency of insulin resistance was higher in the subjects with AA (54.6%) or AT (59.6%) than the subject with TT genotype (50%), but did not statistically different (p = 0.81 and p = 0.47, respectively). The insulin resistance rate was also higher in the risk allele (A) than the non-risk allele (T) subjects (0.58 vs. 0.55), but did not statistically different (p = 0.75). There was no association between FTO rs9939609 variant and body mass index, fasting glucose level, fasting insulin level, homeostatic model assessment of insulin resistance, and waist circumference (p > 0.05). In conclusion, FTO rs9939609 variant may not be associated with insulin resistance in Indonesian obese female adolescents. A multicenter study with a larger sample size is needed to clarify these findings.
Keywords: Common variant, FTO, rs9939609, Indonesia, Insulin resistance, Obese female adolescents
Introduction
Obesity is one of the major health problems all over the world. The obesity incidence in children and adolescents has increased over the last two decades. Obesity is related to other diseases such as insulin resistance. Recently, the prevalence of obesity in Indonesian children and adolescents increased to 10% [1]. It is suggested that there are genetic factors that affect the insulin resistance in obesity.
Fat mass and obesity related gene (FTO), located at 16q12.2, is associated with obesity and type 2 diabetes mellitus (T2DM). FTO rs9939609 common variant has been significantly related with increased insulin resistance in obese female adolescents (p < 0.001) [2], but not in male adolescents in Chile after adjustment for body mass index (BMI). However, other studies did not show any association between FTO rs9939609 polymorphism and insulin resistance [3, 4].
Indonesia is a country with approximately 400 ethnic and linguistic groups [5]. Indonesian native ancestries are genetically similar to Asians, with some genetic evidence of a division between East and Southeast Asians [6, 7]. There appears to be some differences in allele frequencies of common variants within Asian populations according to the Y chromosome polymorphism findings in North Asians, Han Chinese, Japanese and Southeast Asians [8]. Thus, Indonesian obese female adolescents can shed additional light on the FTO rs9939609 effect on insulin resistance by providing data from a genetically distinct group within Asia.
Main text
Methods
Subjects
We enlisted obese female adolescents aged 11–15 years old at six junior high schools in Yogyakarta, Indonesia. We determined their height and weight to calculate the BMI and categorize them into underweight, normal, overweight or obese. The prevalence of obesity among those female adolescents was 136/2101 (6.4%).
After getting informed consent, we collected the blood samples from 78 obese female adolescents. The inclusion criteria of this study were as follows: (1) female adolescent aged 11–15 years old; (2) obese (BMI ≥ 95%) according to the Center for Disease Control and Prevention criteria based on age and sex; (3) reached menarche; and (4) signed informed consent form, while the exclusion criteria consisted of: (1) incomplete data; and (2) poor quality of DNA. The study has been approved by Institutional Review Board of Faculty of Medicine Universitas Gadjah Mada/Dr. Sardjito Hospital (KE/FK/183/EC).
Insulin resistance measurement
Insulin resistance was determined according to homeostatic model assessment of insulin resistance (HOMA-IR), and calculated by the following formula: fasting glucose level (mg/dL) × fasting insulin level (mU/mL)/405. The subject with the HOMA-IR of ≥ 3.16 was classified as having insulin resistance. As for the measurement of fasting glucose and insulin level, blood sampling was taken in the morning after fasting 8–12 h (last meal at 10 pm). Blood insulin level was determined using the immunoassay method, whereas glucose level was measured by the hexokinase technique.
Genotyping
DNA was extracted from a 5-mL blood using salting out method. Genotyping of FTO rs9939609 was determined using polymerase chain reaction (PCR) twice. The PCR was conducted using GoTaq®PCR reaction mixture. The first PCR used an allele A specific primer, while the second PCR used an allele T specific primer. The PCR conditions were 94 °C for 3 min, followed by 35 cycles of 94 °C for 30 s, 65 °C for 30 s, then 72 °C for 30 s, and finally 72 °C for 5 min. To ensure the validity, the genotyping was determined by two independent experts. If any difference existed, the PCR was repeated.
Statistical analysis
The association between the FTO rs9939609 variants (TT, TA, AA) and insulin resistance was determined by Chi square test. Data distribution was tested by the Kolmogorov Smirnov test. If the data distribution was abnormal, the Mann–Whitney U and Kruskal–Wallis tests were used for continue and category data analysis. Logistic regression was applied to adjust for differences in BMI between insulin resistance and non-insulin resistance groups. The analysis was performed using SPSS ver. 20.0 for Windows (SPSS, Inc. Chicago, IL).
Results
There were three genotypes of FTO rs9939609 found in the subjects: AA, AT and TT (Fig. 1). The risk allele (A) frequency of FTO rs9939609 variant in Indonesian obese female adolescence was 44.2%. Among 78 obese female adolescents, 25.6% were TT, 60.2% were AT, and 14.1% were AA. The frequency of insulin resistance was higher in the subjects with AA (54.6%) or AT (59.6%) than the subject with TT genotype (50%), however, these differences did not reach a significant level (p = 0.81 and p = 0.47, respectively) (Table 1). The insulin resistance rate was also higher in the risk allele (A) than the non-risk allele (T) subjects (0.58 vs. 0.55, respectively), but did not statistically different (0.75) (Table 1).
Fig. 1.
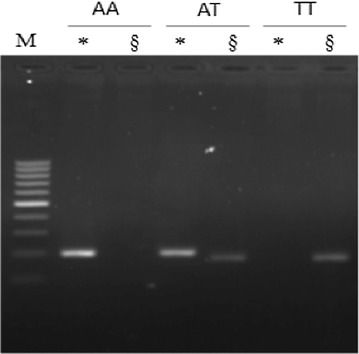
PCR products of FTO rs9939609. *Showed A allele specific PCR product (201 bp), while §showed T allele specific PCR product (178 bp). We conducted two times PCR for each sample. Positive result o n A allele specific PCR product but negative on T allele specific PCR product means AA genotype (lanes 1 and 2). Both positive A and T allele specific PCR product means AT genotype (lanes 3 and 4). Negative result on A allele specific PCR product but positive on T allele specific PCR product means TT genotype (lanes 5 and 6)
Table 1.
The frequency of genotype and allele of FTO rs9939609 polymorphism in insulin resistance (IR) and non-insulin resistance (NIR) groups
| N | % | NIR (%) | IR (%) | OR (95% IK) | p | |
|---|---|---|---|---|---|---|
| Genotypes | ||||||
| AA | 20 | 25.6 | 5 (45.5) | 6 (54.5) | 1.2 (0.2–6.5) | 0.81 |
| AT | 47 | 60.3 | 19 (40.4) | 28 (59.6) | 1.5 (0.5–9.8) | 0.47 |
| TT | 11 | 14.1 | 10 (50) | 10 (50) | Reference | |
| Alleles | ||||||
| A | 87 | 44.2 | 29 (42) | 40 (58) | 1.1 (0.6–2.1) | 0.75 |
| T | 69 | 55.8 | 39 (44.8) | 48 (55.2) | Reference | |
IR insulin resistance, NIR non-insulin resistance
This study further aimed to evaluate the effect of FTO rs9939609 variants on the following parameters: BMI, fasting glucose level, fasting insulin level, HOMA-IR and waist circumference. All measurements were higher in the AA genotype group compared to other genotype groups, however the results did not reach significant levels (Table 2). Accordingly, the results showed that there was no significant association statistically between risk allele A rs9939609 variant and BMI, fasting glucose level, fasting insulin level, HOMA-IR and waist circumference (Table 2).
Table 2.
The association between body mass index (BMI), fasting glucose level, fasting insulin level, HOMA-IR and waist circumference and FTO rs9939609 variant genotypes and alleles
| Parameters | Genotypes | p | Alleles | p | |||
|---|---|---|---|---|---|---|---|
| AA | AT | TT | A | T | |||
| BMIa | 30.79 ± 3.39 | 29.44 ± 2.37 | 29.61 ± 2.59 | 0.30 | 29.87 ± 2.76 | 29.52 ± 2.45 | 0.32 |
| Fasting glucoseb | 89.73 ± 13.13 | 89.96 ± 21.51 | 83.5 ± 8.47 | 0.39 | 89.80 ± 19.07 | 86.99 ± 17.02 | 0.72 |
| Fasting insulinc | 19.82 ± 15.03 | 17.73 ± 11.11 | 16.55 ± 8.37 | 0.74 | 18.39 ± 12.28 | 17.19 ± 9.86 | 0.34 |
| HOMA-IR | 4.29 ± 3.43 | 4.11 ± 3.69 | 3.41 ± 1.75 | 0.68 | 4.17 ± 3.56 | 3.79 ± 2.96 | 0.37 |
| Waist circumferenced | 91.59 ± 8.76 | 88.97 ± 5.94 | 88.25 ± 6.53 | 0.38 | 89.8 ± 6.92 | 86.99 ± 17.02 | 0.35 |
Data was presented with mean ± SD. p value was determined using Kruskal–Wallis test since the data distribution was abnormal according to Kolmogorov–Smirnov test (p < 0.05)
akg/m2; b mg/dL; c µM/mL; d cm
To assess the effect of population stratification, we analyzed the total Indonesian sample genotypes (44 IR subjects and 34 NIR subjects) for the Hardy–Weinberg equilibrium: rs9939609 (p > 0.05) showed no departures from expectations.
Discussion
In this study, we were unable to show any significant association between FTO rs9939609 common variant and insulin resistance. It should be noted that although not statistically significant, BMI, fasting glucose level, fasting insulin level, HOMA-IR and waist circumference are higher in individuals with risk allele (A) compared to those with non-risk allele (T).
Zavattari et al. [4] also showed that there was no association between FTO rs9939609 polymorphism and biochemistry parameters such as HOMA-IR, serum insulin levels and oral glucose tolerance test in obese adolescents in Italy. Shimaoka et al. [3] described the association between FTO rs1121980 variant (not rs9939609) and insulin resistance in a Japan population. However, this finding differed from other studies in Chile, Scotland and Finland [2, 9, 10].
In this study, the risk allele A frequency in obese female adolescents in Yogyakarta was 44.2%. This frequency was lower than the frequency in Western countries (55–65.4%) [2, 4], but higher than in a control population in Asia (16%), or world population (36%) that consisted of: Americans (28%), Europeans (42%), and Asians (16%), except Africans (54%) [11, 12].
There are several established findings regarding the association between insulin resistance and FTO rs9939609. Individuals with rs9939609 risk allele A have more FTO transcripts than individuals with allele T [13]. The mRNA FTO was associated with gene expression demonstrated to be important for glucose homeostasis [14], gene expression, which involved gluconeogenesis in liver [15], TNF and NFKB1 level in subcutaneous lipid [16] and insulin and mRNA KCNJ11 in beta cells, in which these genes were concluded to be responsible for glucose homeostasis. One study showed that overexpression of FTO in INS-1 pancreatic beta cells increased the first phase of insulin secretion response to glucose [17].
Those mechanisms provide possible explanations about how the FTO polymorphisms influence the insulin resistance. Additionally, previous studies showed that rs9939609 variants increased the FTO mRNA transcript important for gene expression involved in glucose homeostasis and insulin resistance. Furthermore, FTO is also associated with nucleic acid demethylation and co-activator transcription that regulate the expression of other genes.
The discrepancy in findings concerning the association between FTO rs9939609 variants and insulin resistance among other studies including our results indicates that the effect of FTO rs9939609 variants on insulin resistance may be influenced by other variables including: gender, age and ethnic [18–21]. The differences in our results may also be due to the limitations created by the small sample population [2, 20, 21].
Conclusions
FTO rs9939609 variant may not be associated with insulin resistance in Indonesian obese female adolescents. This emphasizes the necessity to perform a multicenter study with a larger sample size to clarify the impact of FTO rs9939609 variant on insulin resistance in obese female adolescent in Indonesia.
Limitations
First, it is difficult to conclude the causality based on a case–control design; a follow-up longitudinal study is recommended to provide confirmation of our findings. In addition, this study only examined one polymorphism, FTO rs9939609, among 40 common variants that are connected to each other in current comparisons of linkage disequilibrium such as the genomic HapMap description of r2 > 0.80 in Caucasian populations that demonstrates intervariability among ethnic groups in the present Human Genome Project efforts to map the DNA of Homo sapiens [12].
Authors’ contributions
KI, MJ, and RS conceived the study. KI, and RS drafted the manuscript, SYP, MJ critically revised the manuscript for important intellectual content. EH, HFL, SYP, MJ, and RS, facilitated all project-related tasks. All authors read and approved the final manuscript.
Acknowledgements
We thank the subjects who have contributed in these studies. We also thank all those who provided excellent technical support and assistance during the study.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed during this study are included in the submission. The raw data are available from the corresponding author on reasonable request.
Consent to publish
Not applicable.
Ethics approval and consent to participate
The Ethical Committee of Faculty of Medicine, Universitas Gadjah Mada/Dr. Sardjito Hospital permitted this study (KE/FK/183/EC). All parents signed informed consent form.
Funding
This work was supported by a Grant from Bakrie Scholarship (2014) (KI).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviation
- FTO
fat mass and obesity related
Contributor Information
Kristy Iskandar, Phone: +628992760786, Email: kristy.iskandar@mail.ugm.ac.id, Email: kristy.iskandar@gmail.com.
Suryono Yudha Patria, Email: yudhap64@yahoo.com.
Emy Huriyati, Email: emyhuriyati@ugm.ac.id.
Harry Freitag Luglio, Email: harryfreitag@ugm.ac.id.
Madarina Julia, Email: madarinajulia@yahoo.com.
Rina Susilowati, Email: rina_susilowati@yahoo.co.id.
References
- 1.Ministry of Health and National Institute of Health Research and Development. National report on basic health research. RISKESDAS 2013. Jakarta: Lembaga Penerbitan Badan Penelitian dan Pengembangan Kesehatan Kementrian Kesehatan Republik Indonesia; 2014.
- 2.Riffo B, Asenjo S, Sáez K, et al. FTO gene is related to obesity in Chilean Amerindian children and impairs HOMA-IR in prepubertal girls. Pediatr Diabetes. 2012;13:384–391. doi: 10.1111/j.1399-5448.2011.00834.x. [DOI] [PubMed] [Google Scholar]
- 3.Shimaoka I, Kamide K, Ohishi M, et al. Association of gene polymorphism of the fat-mass and obesity-associated gene with insulin resistance in Japanese. Hypertens Res. 2010;33:214–218. doi: 10.1038/hr.2009.215. [DOI] [PubMed] [Google Scholar]
- 4.Zavattari P, Loche A, Pilia S, et al. rs9939609 in the FTO gene is associated with obesity but not with several biochemical parameters in Sardinian obese children. Ann Hum Genet. 2011;75:648–654. doi: 10.1111/j.1469-1809.2011.00674.x. [DOI] [PubMed] [Google Scholar]
- 5.Ananta A. Changing ethnic composition and potential violent conflict in Riau archipelago, Indonesia: an early warning signal. Popul Rev. 2006;45:48–68. [Google Scholar]
- 6.Cavalli-Sforza LL. The Chinese human genome diversity project. Proc Natl Acad Sci USA. 1998;95:11501–11503. doi: 10.1073/pnas.95.20.11501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jixu Z. The rise of the agricultural civilization in China. Sino-Platonic Pap. 2006;175:1–38. [Google Scholar]
- 8.Tajima A, Pan IH, Fucharoen G, et al. Three major lineages of Asian Y chromosomes: implications for the peopling of east and southeast Asia. Hum Genet. 2002;110:80–88. doi: 10.1007/s00439-001-0651-9. [DOI] [PubMed] [Google Scholar]
- 9.Doney AS, Dannfald J, Kimber CH, et al. The FTO gene is associated with an atherogenic lipid profile and myocardial infarction in patients with type 2 diabetes: a Genetics of Diabetes Audit and Research Study in Tayside Scotland (Go-DARTS) study. Circ Cardiovasc Genet. 2009;2:255–259. doi: 10.1161/CIRCGENETICS.108.822320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lappalainen TJ, Tolppanen AM, Kolehmainen M, et al. The common variant in the FTO gene did not modify the effect of lifestyle changes on body weight: the Finnish Diabetes Prevention Study. Obesity (Silver Spring). 2009;17:832–836. doi: 10.1038/oby.2008.618. [DOI] [PubMed] [Google Scholar]
- 11.1000 Genomes Project Consortium. Abecasis GR, Altshuler D, et al. A map of human genome variation from population-scale sequencing. Nature. 2010;467:1061–1073. doi: 10.1038/nature09534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International HapMap 3 Consortium Integrating common and rare genetic variation in diverse human populations. Nature. 2010;467:52–58. doi: 10.1038/nature09298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berulava T, Horsthemke B. The obesity-associated SNPs in intron 1 of the FTO gene affect primary transcript levels. Eur J Hum Genet. 2010;18:1054–1056. doi: 10.1038/ejhg.2010.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyre D. Is FTO a type 2 diabetes susceptibility gene? Diabetologia. 2012;55:873–876. doi: 10.1007/s00125-012-2478-4. [DOI] [PubMed] [Google Scholar]
- 15.Poritsanos NJ, Lew PS, Mizuno TM. Relationship between blood glucose levels and hepatic Fto mRNA expression in mice. Biochem Biophys Res Commun. 2010;400:713–717. doi: 10.1016/j.bbrc.2010.08.133. [DOI] [PubMed] [Google Scholar]
- 16.Samaras K, Botelho NK, Chisholm DJ, Lord RV. Subcutaneous and visceral adipose tissue FTO gene expression and adiposity, Insulin action, glucose metabolism, and inflammatory adipokines in type 2 diabetes mellitus and in health. Obesity (Silver Spring). 2010;18:884–889. doi: 10.1038/oby.2009.443. [DOI] [PubMed] [Google Scholar]
- 17.Russell MA, Morgan NG. Conditional expression of the FTO gene product in rat INS-1 cells reveals its rapid turnover and a role in the profile of glucose-induced insulin secretion. Clin Sci (Lond). 2011;120:403–413. doi: 10.1042/CS20100416. [DOI] [PubMed] [Google Scholar]
- 18.Ohashi J, Naka I, Kimura R, et al. FTO polymorphisms in oceanic populations. J Hum Genet. 2007;52:1031–1035. doi: 10.1007/s10038-007-0198-2. [DOI] [PubMed] [Google Scholar]
- 19.Li H, Wu Y, Loos RJ, et al. Variants in the fat mass- and obesity-associated (FTO) gene are not associated with obesity in a Chinese Han population. Diabetes. 2008;57:264–268. doi: 10.2337/db07-1130. [DOI] [PubMed] [Google Scholar]
- 20.Wing MR, Ziegler JM, Langefeld CD, et al. Analysis of FTO gene variants with obesity and glucose homeostasis measures in the multiethnic Insulin Resistance Atherosclerosis Study cohort. Int J Obes (Lond). 2011;35:1173–1182. doi: 10.1038/ijo.2010.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luczynski W, Zalewski G, Bossowski A. The association of the FTO rs9939609 polymorphism with obesity and metabolic risk factors for cardiovascular diseases in Polish children. J Physiol Pharmacol. 2012;63:241–248. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in the submission. The raw data are available from the corresponding author on reasonable request.


