Abstract
Human visceral leishmaniasis one of the seven most neglected tropical diseases in the world. In Morocco, HVL is widespread in all regions; but it is more common in the northern part with sporadic cases observed in the South.
During the period between 2004 and 2013, the most affected Moroccan provinces were Taounate province, with 220 cases (16.09% of all cases), followed by Chefchaouen with 13.17% and Taza with 10.46% of the total cases. Children < 5 years old are the most affected age group, most cases registered were male.
Geographic distribution of HVL showed predominance in rural areas but we noted that it's opening to be urban.
Keywords: Leishmania infantum, Visceral leishmaniasis, Epidemiology, Urbanization, Vectors, Morocco
1. Introduction
Human visceral leishmaniasis (HVL), also known as kala-azar, is the most several form of leishmaniasis, able to cause mortality in absence or inadequately of treatment. According to Alvar et al. (2012), the incidence of this form was about 150 cases/year between 2006 and 2008. More than 90% of global VL cases occur in just six countries: India, Bangladesh, Sudan, South Sudan, Brazil and Ethiopia (Alvar et al., 2012).
In Morocco, leishmaniases are endemic diseases posing a major threat to public health. HVL is caused by Leishmania infantum, protozoan parasite, and transmitted by the bite of certain species of sandfly (Diptera, Psychodidae, Phlebotominae), belonging to the subgenus Larroussius: Phlebotomus ariasi and potentially P. perniciosus and P. longicuspis (Guessouss-Idrissi et al., 1997, Kahime et al., 2015b). L. infantum in Morocco can cause also zoonotic cutaneous leishmaniasis and canine leishmaniasis in the north and center-south regions of the country (Kahime et al., 2015a, Boussaa et al., 2014) with the domestic dog is the main reservoir host for all forms (Rhajaoui, 2011, Kahime et al., 2014).
HVL evolution in Morocco shows 154 cases in 2004 against 76 cases reported in 1997 (Tamimy, 2011). Children less than 4 years are the most affected population (Amro et al., 2013). Almost all of these cases were from Northern traditional foci like Chefchaouen, Taounate, Taza, Fès, My Yacoub, Meknes, Sefrou, Sidi Kacemand Al Houceima. In Central and South of Morocco, L. infantum infections are sporadic. However, their appearance becomes more frequent recently (Moroccan Ministry of Health (MMH), 2015; Kahime et al., 2015b).
The aim of this study is to establish the spatio-temporal epidemiologic pattern of HVL in Morocco according to many variables (age, gender, locality, urbanization…).
2. Materials and methods
We used clinical and epidemiological data provided by the Moroccan Directorate of Epidemiology and Fight Against Diseases, during 2004–2014 (Moroccan Ministry of Health (MMH), 2015).
A cross-sectional study was done that included all cases of HVL registered in Morocco, from January 2004 to December 2014. A suspected case was defined, according to the surveillance guide of the Moroccan Ministry of Health, before any confirmation by all different diagnosis, as a subject with fever and splenomegaly from an endemic area. Generally, HVL's evolution is very slow, from months to sometimes several years with gradual increase and worsening of clinical and biological symptoms.
The analyzed variables were gender, age, locality, month; statistical analysis was done through the program Epi-Info 6.04 of the Moroccan Directorate of Epidemiology and Fight Against Diseases.
Maps were produced for incidence repartition calculated for the studied area by using ArcMap GIS version 10. All data were analyzed by using SPSS software and results were considered significant when the P-value was less than 0.05 by using a Tukey test.
3. Results
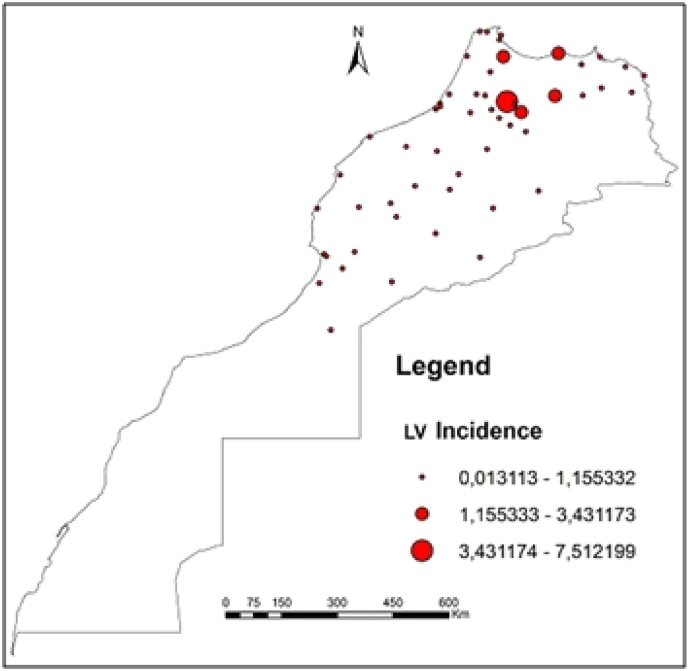
The spatiotemporal analysis shows that in 2011 two areas were exposed to HVL by L. infantum in Morocco under a hypo-endemic way in rural foci. The first is mainly along a northeast axis where L. infantum is endemic, while the second spread from the center to south, including the Marrakech-Tensift-Al Haouz, Tadla-Azilal and Agadir-Tiznite regions like Marrakech, Chichaoua, Al Haouz, El Kelaâ, Azilal, Taroudannt, Agadir and Tiznite provinces (Table 1) and the South-East area including Zagora, Tinghhir and the entire area below the High Atlas Mountains where cases have been recorded (Fig. 1).
Table 1.
HVL cases in Morocco recorded between 2004 and 2013 (Moroccan Ministry of Health (MMH), 2015).
| Provinces | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | Total | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Taounate | 16 | 25 | 25 | 31 | 36 | 21 | 27 | 17 | 9 | 13 | 220 | 16.09 |
| Chefchaouen | 18 | 12 | 24 | 28 | 26 | 17 | 18 | 16 | 12 | 9 | 180 | 13.17 |
| Taza | 23 | 21 | 19 | 13 | 16 | 21 | 7 | 11 | 9 | 3 | 143 | 10.46 |
| Moulay Yacoub | 19 | 17 | 22 | 9 | 9 | 11 | 8 | 6 | 4 | 8 | 113 | 8.27 |
| Al Hoceima | 14 | 5 | 3 | 5 | 14 | 10 | 16 | 6 | 7 | 11 | 91 | 6.66 |
| Fez | 13 | 12 | 17 | 1 | 8 | 5 | 7 | 4 | 8 | 2 | 77 | 5.63 |
| Séfrou | 6 | 6 | 13 | 6 | 9 | 9 | 13 | 5 | 4 | 4 | 75 | 5.49 |
| Sidi Kacem | 8 | 3 | 5 | 6 | 5 | 4 | 6 | 5 | 2 | 2 | 46 | 3.37 |
| Meknès | 4 | 2 | 5 | 9 | 4 | 5 | 2 | 3 | 6 | 1 | 41 | 3.00 |
| Tétouan | 3 | 5 | 3 | 4 | 4 | 1 | 1 | 2 | 5 | 28 | 2.05 | |
| El Hajeb | 1 | 2 | 6 | 6 | 3 | 2 | 1 | 2 | 2 | 25 | 1.83 | |
| Nador | 2 | 2 | 2 | 3 | 1 | 2 | 3 | 3 | 3 | 4 | 25 | 1.83 |
| Khénifra | 2 | 2 | 5 | 10 | 2 | 2 | 1 | 24 | 1.76 | |||
| Kénitra | 1 | 4 | 2 | 2 | 3 | 7 | 3 | 22 | 1.61 | |||
| Beni Mellal | 4 | 2 | 2 | 4 | 1 | 3 | 2 | 1 | 1 | 20 | 1.46 | |
| Al Haouz | 3 | 2 | 3 | 1 | 1 | 1 | 1 | 4 | 16 | 1.17 | ||
| Larache | 3 | 4 | 2 | 2 | 2 | 2 | 1 | 16 | 1.17 | |||
| El Jadida | 3 | 2 | 3 | 4 | 2 | 14 | 1.02 | |||||
| Zagora | 2 | 3 | 3 | 1 | 1 | 2 | 2 | 14 | 1.02 | |||
| Ouazzane | 4 | 3 | 5 | 12 | 0.88 | |||||||
| Azilal | 2 | 4 | 1 | 4 | 11 | 0.80 | ||||||
| Boulemane | 2 | 2 | 1 | 4 | 1 | 10 | 0.73 | |||||
| Errachidia | 1 | 3 | 3 | 2 | 9 | 0.66 | ||||||
| Khémisset | 2 | 3 | 2 | 2 | 9 | 0.66 | ||||||
| Tata | 1 | 1 | 6 | 1 | 9 | 0.66 | ||||||
| Berkane | 1 | 1 | 1 | 2 | 2 | 1 | 8 | 0.59 | ||||
| Driouach | 2 | 2 | 3 | 7 | 0.51 | |||||||
| Taourirte | 1 | 1 | 3 | 1 | 1 | 7 | 0.51 | |||||
| Chichaoua | 1 | 1 | 1 | 1 | 2 | 6 | 0.44 | |||||
| Ouarzazate | 1 | 3 | 1 | 1 | 6 | 0.44 | ||||||
| Settat | 1 | 2 | 1 | 2 | 6 | 0.44 | ||||||
| Taroudannt | 2 | 2 | 1 | 1 | 6 | 0.44 | ||||||
| El Kelaâ | 1 | 1 | 3 | 5 | 0.37 | |||||||
| Guercif (Taza) | 1 | 2 | 2 | 5 | 0.37 | |||||||
| Marrakech | 1 | 1 | 1 | 1 | 1 | 5 | 0.37 | |||||
| Tinghir (Ouarz) | 1 | 1 | 3 | 5 | 0.37 | |||||||
| Essaouira | 1 | 1 | 2 | 4 | 0.29 | |||||||
| Safi | 3 | 1 | 4 | 0.29 | ||||||||
| Agadir | 2 | 1 | 3 | 0.22 | ||||||||
| Chtouka | 1 | 1 | 1 | 3 | 0.22 | |||||||
| Jrada | 1 | 1 | 1 | 3 | 0.22 | |||||||
| Khouribga | 1 | 1 | 1 | 3 | 0.22 | |||||||
| Mdiq Fnideq | 1 | 1 | 1 | 3 | 0.22 | |||||||
| Salé | 1 | 1 | 1 | 3 | 0.22 | |||||||
| Sidi Youssef | 2 | 2 | 0.15 | |||||||||
| Tiznit | 1 | 1 | 2 | 0.15 | ||||||||
| Assa Zag | 1 | 1 | 0.07 | |||||||||
| Fahs Anjra | 1 | 1 | 0.07 | |||||||||
| Ifrane | 1 | 1 | 0.07 | |||||||||
| Inezgane | 1 | 1 | 0.07 | |||||||||
| Oujda | 1 | 1 | 0.07 | |||||||||
| Rabat | 1 | 1 | 0.07 | |||||||||
| Sidi Slimane | 1 | 1 | 0.07 | |||||||||
| Tanger Assilah | 1 | 1 | 0.07 | |||||||||
| Temara | 1 | 1 | 0.07 | |||||||||
| Other provinces | 12 | 12 | 0.88 | |||||||||
| Total | 154 | 114 | 171 | 160 | 163 | 134 | 139 | 107 | 113 | 112 | 1367 | 100% |
Fig. 1.
Geographical distribution of HVL incidence (cases due to L. infantum/100,000 population/(2003–2014 period) in Moroccan provinces.
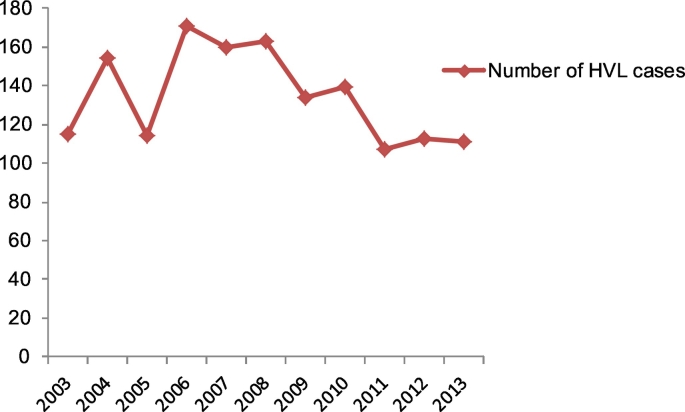
According to Moroccan Ministry of Health (Moroccan Ministry of Health, 2014), the epidemiological situation of HVL in Morocco, between 2004 and 2013, is marked by the continued reporting of cases with an average of 137 cases/year. However, some increase since 2006 was noted (Table 1). During the period between January 2003 to December 2013, 1481 cases of VL were registered in Morocco. 171 cases have been observed in 2006 against 111recorded in 2013 (Fig. 2).
Fig. 2.
Confirmed cases of visceral leishmaniasis in Morocco, from January 2003 to December 2013.
According to locality, Taounate (Lat: 35.249; Long: − 3.940, Alt: 567 m) province is the most affected, with 220 cases (16.09% of all cases), followed by Chefchaouen (Lat: 35.171; Long: − 5.272; Alt: 600 m) with 13.17% and Taza (Lat: 34.228; Long: − 4.021; Alt: 1100 m) with 10.46% of the total cases (Table 1). For this latter province, the number of cases rose, with 1 case in 1990 to reach 26 cases in 2000. The provinces of Alhoceima (Lat: 35,249; Long: − 3,938; Alt: 14 m), Chefchaouen, Taounante and Moulay Yacoub (Lat: 34.088; Long: − 5.181; Alt: 260 m) were unharmed during the years 1990–1991 and 1992, they have become foci of HVL from 2000.
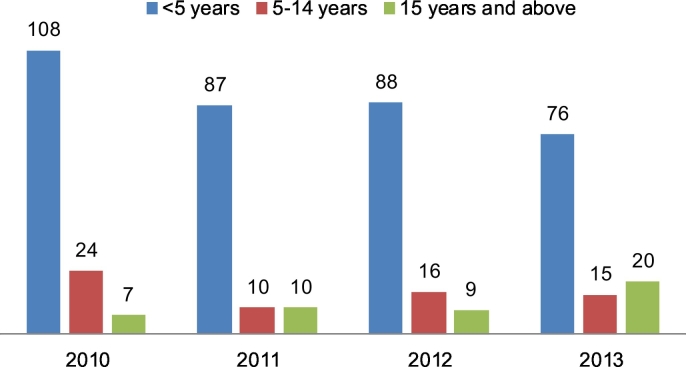
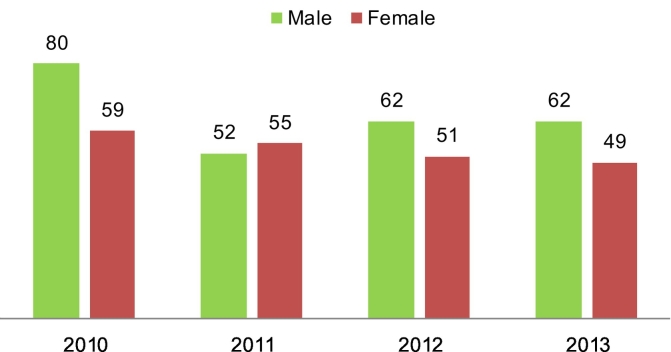
As shown in Fig. 3, Moroccan HVL occurred mainly in children under 5 years old, this category was significantly (P < 0.05) affected. It can affect also young and old people, reflecting the beginning of a bimodal pattern of incidence (Fig. 3). Most cases registered were male, except for 2011 as shown in Fig. 4. In fact, this may be due to social behavior of male gender, who are more active out of the houses at night and then more accessible to the vector bits. In general, the difference of gender infection is not statistically significant.
Fig. 3.
Age distribution of confirmed cases (y-axis) of human visceral leishmaniasis in Morocco, from January 2010 to December 2014.
Fig. 4.
Gender distribution of confirmed cases (y-axis) of human visceral leishmaniasis, in Morocco, from January 2010 to December 2014.
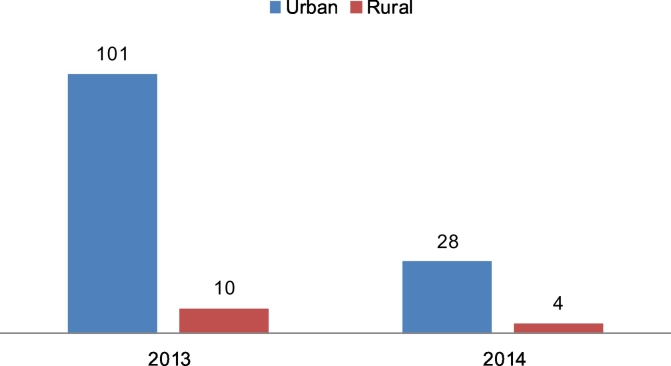
According to register of Ministry of Health, the geographic distribution of HVL showed predominance in rural areas but we noted that it's opening to be urban (Fig. 5). The difference was not statistically significant. Analysis according to urbanization was not possible because of a lack of information pre-2013 concerning type of urbanization.
Fig. 5.
Confirmed cases (y-axis) of visceral leishmaniasis by living area, of Morocco, from January 2010 to December 2014.
4. Discussion
In Morocco the eco-epidemiological complex which characterizes HVL is not yet well understood. According to Moroccan Ministry of Health, all human cases are due to L. infantum MON 1.
In Morocco, L. tropica species may cause the visceral canine leishmaniasis. Several cases of canine leishmaniasis caused by L. tropica have been reported in regions where canine leishmaniasis is caused by L. infantum MOM 1 (Kahime et al., 2015b). In the provinces of Taounate and Al Hoceima, L. tropica was isolated from dogs with VL (Guessouss-Idrissi et al., 1997, Lemrani et al., 2002).
HVL-L. infantum is transmitted by sandflies belonging to the subgenus Larroussius with domestic dog being the host reservoir (Kahime et al., 2014), as Canis familiaris play for this culprit parasite in southwest Europe and northwest Africa, including Morocco. Nevertheless, P. ariasi, P. perniciosus and P. longicuspis are the proven vectors in Mediterranean countries (Amro et al., 2013, Berdjane-Brouk et al., 2012, Kahime et al., 2015b), while in Morocco, only P. ariasi vectorial role was confirmed.
Zarrouk et al. (2015) hypothesized the potential involvement of typical (PN) and atypical (PNA) morphs of P. perniciosus, P. longicuspis sensu stricto (LCss), and P. longicuspis (LCx), at least, with P. ariasi, in the epidemiological cycle of L. infantum in Morocco.
HVL is encountered habitually in children related to their immaturity and immune systems (World Health Organization, 2010); the average age is between 3.5 and 4 years (Hassani et al., 2011). A slight male predominance is noted (Lakhdar Idrissi et al., 2007).
Human visceral leishmaniasis disease is frequent in rural communities of Africa (Hailu et al., 2005). In Morocco, HVL is now spread throughout many provinces. It exist more in rural area, where, the majority of the population live at the poverty level in unsanitary housing, poorly nourished, and possibly with decrease of the immunity. Moreover, HVL is recorded in urban area. One of the major risk factors is the leishmaniasis spread may be urbanization (World Health Organization (WHO), 2002), closely related to the sharp increase in migration rural–rural and/or rural–urban related to socio-economic, demographic, and environmental-climatic factors.
In recent five years “urbanization” of HVL has been observed (Moroccan Ministry of Health (MMH), 2015), like for the ACL incidence increasing (World Health Organization (WHO), 2002; Kahime et al., 2015a).
Dogs (domestic and feral) are the main reservoir of infection. Due to a sizeable feral population and lack of a proven effective vaccine for control of canine leishmaniasis it is practically impossible to control HVL.
5. Conclusion
This study is an update of the state of HVL to L. infantum in Morocco whose geographical position, the coexistence of many potential vectors, the high dog population — as main reservoir of L. infantum (Dereure et al., 1986, Boussaa et al., 2014), climate (Ready, 2014), socio-economic condition (Kahime et al., 2012) all contribute to the spread of LVH infection. Continuous epidemiological surveillance is thus required. Furthermore, more investigations of risk factors associated especially with vector-reservoir population densities, urbanization and socio-economic conditions may provide an explanation for the change in geographical distribution of visceral forms of leishmaniasis at the local level.
Acknowledgments
Conflict of interest
The authors report no conflict of interest.
Contributor Information
Kholoud Kahime, Email: kahimkholoud@gmail.com.
Ali Boumezzough, Email: aboumezzough@gmail.com.
References
- Alvar J., Vélez I.D., Bern C., Herrero M., Desjeux P., Cano J., Jannin J. Leishmaniasis worldwide and global estimates of its incidence. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amro A., Hamdi S., Lemrani M., Idrissi M., Hida M., Rhajaoui M., Hamarshe O., Sconian G. Moroccan Leishmania infantum: genetic diversity and population structure as revealed by multi-locus microsatellite typing. PLoS One. 2013;8 doi: 10.1371/journal.pone.0077778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berdjane-Brouk Z., Charrel N.R., Hamrioui B., KiIzri A. First detection of Leishmania infantum DNA in Phlebotomus longicuspis Nitzulescu, 1930 from visceral leishmaniasis endemic focus in Algeria. Parasitol. Res. 2012;111:419–422. doi: 10.1007/s00436-012-2858-1. [DOI] [PubMed] [Google Scholar]
- Boussaa S., Kasbari M., El Mzabi A., Boumezzough A. Epidemiological investigation of canine leishmaniasis in Southern Morocco. Adv. Epidemiol. 2014;8 (ID 104697) [Google Scholar]
- Dereure J., Velez I.D., Pratlong F., Denial M., Lardi M., Moreno G., Serres E. Leishmania. Taxonomie et Phylogenèse. Applications Eco-épidémiologiques, Int Coll CNRS/INSERM/OMS (2–6 July 1984) Institut Méditerranéen d’Etudes Epidémiologiques et Ecologiques; Montpellier: 1986. La leishmaniose viscérale autochtone au Maroc méridional. Présence de Leishmania infantum MON-1 chez le Chien en zone présaharienne; pp. 421–425. [Google Scholar]
- Guessouss-Idrissi N., Berrag B., Riyad M., Sahibi H., Bichichi M., Rhalem A. Leishmania tropica: etiologic agent of a case of visceralizing canine leishmaniasis in north Morocco. Am. J. Trop. Med. Hyg. 1997;57:172–173. doi: 10.4269/ajtmh.1997.57.172. [DOI] [PubMed] [Google Scholar]
- Hailu A., Musa A.M., Royce C., Wasunna M. Visceral leishmaniasis: new health tools are needed. PLoS Med. 2005;2 doi: 10.1371/journal.pmed.0020211. (e211 05-PLME-ND-0101) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassani M.A., Lahlou H., Alami M., Filali Baba A., El Youssfi G., Ismaili L., Chaouki S. Parasitologie. Elsevier Masson SAS; 2011. Aspects biologiques de la leishmaniose viscérale infantile: À propos de 31 cas diagnostiqués sur 10 mois au laboratoire d’hématologie du CHU Hassan II de Fès (Maroc) [Google Scholar]
- Kahime K., Bounoua B., Messouli M., Boussaa S., Boumezzough A. Evaluation of eco-adaptation strategies of health to climate change: case of zoonotic cutaneous leishmaniasis (ZCL) as vulnerability indicator in pre-Saharan region of Morocco. In: Behnassi M., editor. Environmental Change and Human Security in the Middle East and Africa. GECS. Springer/Cambridge University Press; 2012. Conference Proceedings. forthcoming. [Google Scholar]
- Kahime K., Boussaa S., Bounoua L., Ouanaimi F., Messouli M., Boumezzough A. Leishmaniasis in Morocco: diseases and vectors. Asian Pac. J. Trop. Dis. 2014;4:530–534. [Google Scholar]
- Kahime K., Boussaa S., Laamrani-El Idrissi A., Nhammi H., Boumezzough A. Epidemiological study on acute cutaneous leishmaniasis in Morocco. JADA. 2015 [Google Scholar]
- Kahime K., Boussaa S., Ouanaimi F., Boumezzough A. Species composition of phlebotomine sand fly fauna in an area with sporadic cases of Leishmania infantum human visceral leishmaniasis, Morocco. Acta Trop. 2015;148:58–65. doi: 10.1016/j.actatropica.2015.04.006. [DOI] [PubMed] [Google Scholar]
- Lakhdar Idrissi M., El Ouardi M., Atmani S. La leishmaniose visceral infantile: à propos de 209 cas. J. Pédiatr. Puéric. 2007;20:136–141. [Google Scholar]
- Lemrani M., Nejjar M., Pratlong F. A new Leishmania tropica zymodeme — causative agent of canine visceral leishmaniasis in northern Morocco. Ann. Trop. Med. Parasitol. 2002;96(6):637–638. doi: 10.1179/000349802125001645. [DOI] [PubMed] [Google Scholar]
- Moroccan Ministry of Health . Directorate of Epidemiology and Disease Control, Ministry of Health; Rabat, Morocco: 2014. A Report on Progress of Control Programs Against Parasitic Diseases.http://www.sante.gov.ma/departements/delm/index-delm.htm Available at. [Google Scholar]
- Moroccan Ministry of Health (MMH) Ministry of Health; Rabat: 2015. The CL Data is Provided by the Directorate of Epidemiology and Disease Control.http://www.sante.gov.ma/Pages/ADM_Centrale/DELM.aspx [Online] Available from. [Accessed on 25th May, 2015] French. [Google Scholar]
- Ready P.D. Epidemiology of visceral leishmaniasis. Clin. Epidemiol. 2014;6:147–154. doi: 10.2147/CLEP.S44267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhajaoui M. Human leishmaniases in Morocco: a nosogeographical diversity. Pathol. Biol. 2011;59:226–229. doi: 10.1016/j.patbio.2009.09.003. [DOI] [PubMed] [Google Scholar]
- Tamimy H. Sidi Mohammed Ben Abdellah University, Faculty of Medicine and Pharmacy; 2011. The Infantile Visceral Leishmaniasis (About 73 Cases)http://scolarite.fmp-usmba.ac.ma/cdim/mediatheque/e theses/89-11.pdf (Ph.D. in Medicine) [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2010. Control of the Leishmaniasis: Report of a Meeting of the WHO Expert Committee on the Control of Leishmaniases.http://whqlibdoc.who.int/trs/WHO_TRS_949_eng.pdf [Online] Available from: [Accessed on 15th July, 2014] [Google Scholar]
- World Health Organization (WHO) Urbanization: An increasing risk factor for Leishmaniasis. Wkly. Epidemiol. Rec. 2002;77:365–372. [PubMed] [Google Scholar]
- Zarrouk A., Kahime K., Boussaa S., Belqat B. Ecological and epidemiological status of species of the Phlebotomus perniciosus complex (Diptera: Psychodidae, Phlebotominae) in Morocco. Parasitol. Res. 2015 doi: 10.1007/s00436-015-4833-0. [DOI] [PubMed] [Google Scholar]