Abstract
Patient: Male, 20
Final Diagnosis: LCx agenesis
Symptoms: Chest pain • syncope
Medication: —
Clinical Procedure: —
Specialty: Cardiology
Objective:
Congenital defects/diseases
Background:
This case study demonstrated that although highly symptomatic, agenesis of the left circumflex artery was a benign finding. Anomalies of the coronary arteries were found to be the cause of sudden death in a young individual. Left circumflex anomalies were not associated with major cardiac events.
Case Report:
A 20-year-old male was admitted due to syncope preceded by chest pain. His electrocardiogram (ECG) showed global ST segment elevation as well as biphasic T waves in anterior precordial leads. Troponin T values were normal. Echocardiography was normal. Computerized axial tomography (CAT) scan showed agenesis of the circumflex artery with a super-dominant right coronary artery. Myocardial scintigraphy showed no perfusion defects. Exercise test did not present any arrhythmias. Tilt table test displayed stable blood pressure and pulse response. A reveal recorder registered no malignant arrhythmias. A coronary angiography confirmed the finding of the CAT scan and showed no collateral vessel development.
Conclusions:
This case demonstrated that agenesis left circumflex artery although presenting with severe symptoms, such as chest pain, is a benign finding. Chest pain was not correlated to perfusion defects in this case. Although the patient experienced loss of consciousness, there was no objective support for cardiac origin as no malignant arrhythmias were found.
MeSH Keywords: Angina Pectoris, Congenital Abnormalities, Syncope
Background
Anomalies of the coronary arteries are found in 1% of coronary angiographies [1,2] and 0.3% of autopsies [3]. Although these autopsy findings can be incidental, they are in general considered to be the cause of sudden death [4–7]. For instance, coronary anomalies are found more frequently in young individuals who die during exercise and in sudden cardiac death in individuals younger than 30 years of age [8]. Left circumflex (LCx) anomalies, however, are relatively common and considered benign [9] in that the absence of LCx has not been associated with major cardiac events [10]. A congenital absence of the LCx artery is a very rare vascular anomaly with a frequency of 0.003% of all patients undergoing angiography [11]. The absence of LCx with super-dominant right coronary artery (RCA) can result in inferior, posterior, and lateral wall myocardial infarction – a 2-vessel disease equivalent when acute occlusion of the RCA occurs. Complete absence results from agenesis of LCx and in this instance the lateral wall of the left ventricle is supplied by a super-dominant right coronary artery or multiple diagonal branches of left anterior descending artery (LAD) [12]. Although a benign finding it is associated with significant clinical symptoms in 20% of patients, with the most typically symptom exertional chest pain. This is due to the steal phenomenon - an increased metabolic demand in the LCx territory resulting in ischemic alteration in territories of LAD or RCA [12,13].
Case Report
A 20-year-old male was admitted to the Department of Cardiology due to syncope preceded by chest pain. A careful analysis of prior medical history revealed that the actual incidence was one of several. In fact, he had at least 5 incidences with similar symptomatology: Chest pain during moderate physical exercise followed by slight palpitations and sudden loss of consciousness for several minutes. Information of prior medical investigations were limited as these were conducted in another country. Moreover, investigations, such as implantation of a reveal recorder and coronary angiography (CAG) were not completed as the parents opposed further diagnostic endeavors at a time when the patient was underage. An echocardiography was accepted and deemed normal. The patient denied any usage of tobacco or illicit drugs.
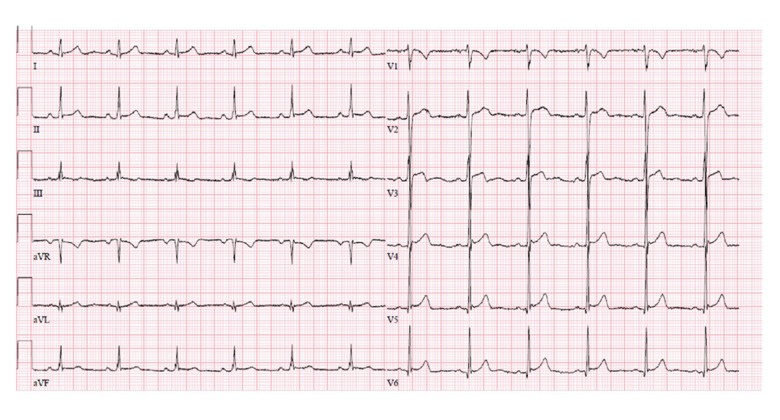
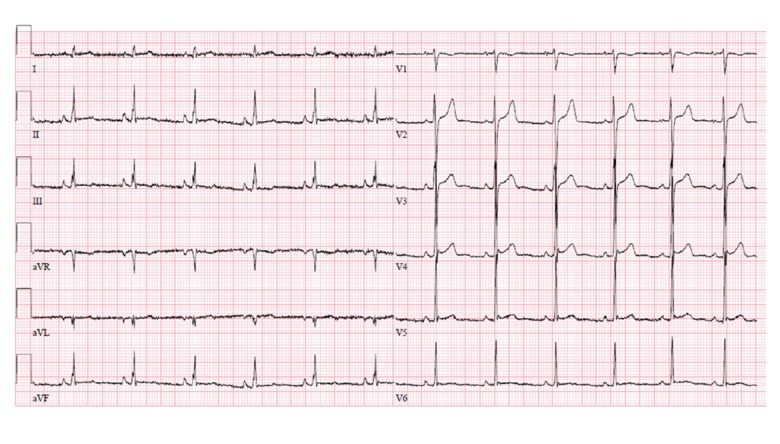
Stethoscopy of heart and lungs was normal. Blood pressure, pulse, and respiration frequency were within normal range. An ECG was taken at admission and was strongly pathological with global ST segment elevation as well as biphasic T waves in anterior precordial leads (Figure 1). The ECG displayed some level of dynamic changes as a second ECG taken after several days showed alterations of the ST segments (Figure 2). Troponin T obtained at admission and after 6 hours were normal. Also, echocardiography was normal with no structural abnormalities, normal ejection fraction and no regional dyskinesia.
Figure 1.
ECG showing global discrete ST elevations and negative T waves in several leads. ECG – electrocardiography.
Figure 2.
Second ECG taken at admission, which was taken after several days, showing dynamic changes of the ST-segments. ECG – electrocardiography.
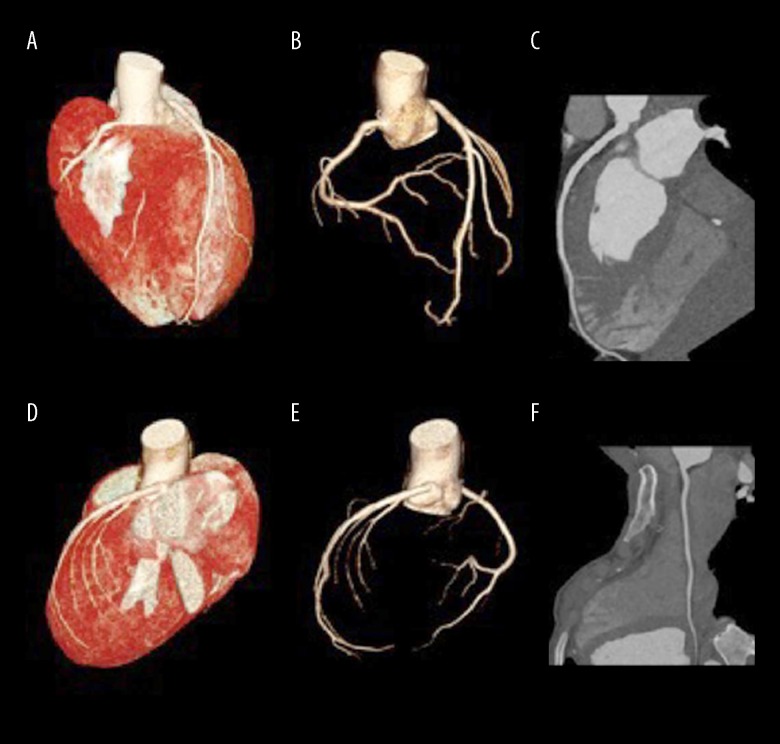
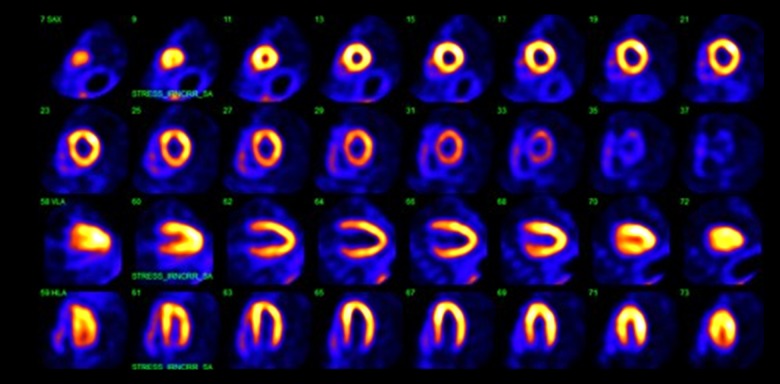
Due to symptoms exacerbated during physical activity, a CAT scan was indicated in order to rule out coronary artery aberrancy. The scan showed agenesis of LCx with a super-dominant RCA (Figure 3). To gain a more profound understanding of the coronary anatomy as well as perfusion status a CAG was proposed, but the patient declined. Instead a myocardial scintigraphy was carried out showing no perfusion defects (Figure 4).
Figure 3.
(A) VRT reconstruction, anterior view. LAD is seen including RCA. (B) Coronary CT angiography, anterior aspect, vessel view only. The LAD as well as RCA is visible. LCx is clearly missing. (C) Coronary CT angiography, curved multiplanar reconstruction of LAD. (D) VRT reconstruction, posterior view. The missing LCx is evident. (E) Coronary CT angiography, posterior aspect. Vessel view only. LCx is missing. (F) Coronary CT angiography, curved multiplanar reconstruction of RCA. VRT – volume rendered technique; LAD – left anterior descending artery; RCA – right coronary artery; LCx – left circumflex; CT – computed tomography.
Figure 4.
Myocardial stress scintigraphy was normal without development of perfusion defects.
In order to establish whether the missing LCx could lead to malignant arrhythmias upon exercise, an exercise test was carried out. A normal blood pressure and pulse response was obtained and no ischemic changes on the ECG were observed nor did the patient present any arrhythmias.
Also, aiming to assess whether the transient loss of consciousness is due to a cardio-inhibitory or vasodilatory response, the patient also underwent a tilt table test which did not convey further information due to stable blood pressure and pulse response.
The patient exhibited characteristic symptoms of angina and very few differential diagnoses were taken into consideration. Acute myocardial infarction was ruled out due to normal troponin values. Symptoms and ECG changes, as well as echocardiography and troponin, did not support perimyocarditis. Also considered were musculoskeletal pain which was not found during careful examination, and aberrant coronary arteries.
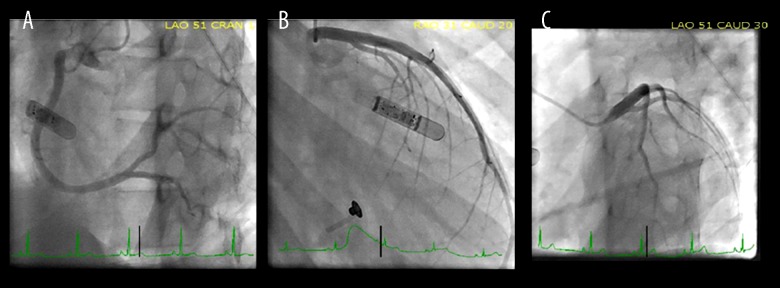
A reveal recorder was implanted, and the patient was discharged from the hospital and follow-up was planned. The patient was readmitted several times since the discharge, with similar symptoms as the original admission. The reveal recorder data suggested sinus tachycardia with no malignant arrhythmias registered by the device. A CAG was offered a second time, which the patient accepted, and which then confirmed the findings of the coronary CAT-scan: absence of LCx. No collateral vessels formation was found (Figure 5). Due to several readmissions, isosorbide mononitrate was administered with symptomatic improvement.
Figure 5.
Coronary arteriography. (A) LAO cranial view (LAO 51; CRAN 1) showing RCA. (B) RAO caudal view (RAO 31; CAUD 20) showing absent LCx and LAD. The implanted reveal recorder is the device partially obstructing the view. (C) LAO caudal view (LAO 51; CAUD 30) showing absent LCx. LAO – left anterior oblique; RCA – right coronary artery; RAO – right anterior oblique; LCx – left circumflex; LAD – left anterior descending artery.
Discussion
When differential diagnoses of chest pain in young individuals can be ruled out, such as pericarditis, perimyocarditis myocardial infarction, or musculoskeletal tenderness, then coronary anomalies should be considered. This case study demonstrated that LCx agenesis, although presenting with severe symptoms such as chest pain, was a benign finding. Chest pain was not correlated with perfusion defects as the myocardial scintigraphy did not support this. However, a case study in the literature described a case in which emotional stress caused chest pain not related to physical activity and troponin elevation in a 55-year-old female with agenesis of LCx, indicating myocardial hypo-perfusion [10]. Usually, infarction in relation to agenesis of LCx is related to occlusion of remaining vessels. In a recent review of 21 cases, only 3 had myocardial infarction, which was associated with thrombi or stenosis of remaining vessels, e.g., a case of inferior acute myocardial infarction in a 52-year-old male was reported with LCx agenesis but was as an extension of an occlusion of super-dominant right coronary artery [14]. Although there was no evidence of hypoperfusion on the myocardial scintigraphy, the patient experienced significant chest pain. Exertional or non-exertional chest pain is a typical symptom in these patients. In a review of 21 patients with missing LCx, 18 patients experienced chest pain [15]. In our case, the administration of nitroglycerin or isosorbide mononitrates had a beneficial effect on symptoms, suggesting that pharmacological antianginal treatment should be considered in patients with LCx agenesis.
Although a benign finding in our case, in that LCx agenesis was not associated with sudden cardiac death or loss of consciousness due to malignant arrhythmias, several instances of loss of consciousness did occurred. No objective findings could support the cause being of cardiac origin as no malignant/ventricular arrhythmias were found. An excellent case report and review of the literature on LCx agenesis has been published recently. A 46-year-old male was described with an episode of transient loss of consciousness. While monitoring of the patient in the emergency department, frequent premature ventricular were noticed as well as on subsequent Holter monitoring. No ventricular arrhythmias were detected [15]. As with our case, no apparent etiology for the loss of consciousness was found, albeit extensive investigations were undertaken, including stress test, tilt table test, and reveal recording. In another case report, a 70-year-old male with a super-dominant right coronary artery with agenesis of LCx and anomalous origin of the LAD from the right sinus experienced syncope after normal effort. This event, however, was considered to be due to severe aortic stenosis and not arrhythmias [16].
In our case, the ejection fraction was preserved. In the aforementioned review of the literature where echocardiography was performed, 3 out of 10 cases had reduced ejection fractions. This reduction was due to stenosis or thrombi of remaining vessels in 2 out of the 3 cases. Thus, agenesis of LCx was usually associated with preserved ejection fraction, which is in agreement with our findings.
The young patient in our case presented with abnormal and dynamic ST segments changes on ECG. Similarly, a case was reported of a 51-year-old male with missing LCx with T wave inversion in leads V3-4-5-6 as well as isoelectric T wave in leads II, III, aVF and I, and aVL [17]. Also, a case of a 46-year-old male with congenital absence of LCx was described with T wave inversions on the ECG [15], indicating that congenital absence of LCx is associated with ECG changes.
Conclusions
Angina in very young individuals can be due to coronary vessel anomalies. Although agenesis of LCx is an extremely rare coronary artery anomaly it should be considered, as LCx agenesis can by highly symptomatic with pronounced chest pain and result in several readmissions to the hospital. Administration of nitrates with prolonged action can alleviate these symptoms. ECG changes such as ST segment elevation/abnormal repolarization or negative T waves may be seen, and echocardiography is most often normal with preserved ejection fraction, unless associated with stenosis of remaining vessels and myocardial infarction. In this context, lest the remaining coronary vessels are stenotic, LCx agenesis rarely leads to myocardial infarction. While highly symptomatic, LCx agenesis is a benign finding in that it has not been reported to be associated with sudden cardiac death, albeit LCx agenesis has, in few cases, been associated with loss of consciousness. These events, however, have occurred without evidence of malignant arrhythmias.
References:
- 1.Hobbs R, Millit H, Raghavan P, et al. Congenital coronary artery anomalies: Clinical and therapeutic implications. Cardiovasc Clin. 1981;12(2):43–58. [PubMed] [Google Scholar]
- 2.Baltaxe H, Wixson D. The incidence of congenital anomalies of the coronary arteries in the adult population. Radiology. 1977;122(1):47–72. doi: 10.1148/122.1.47. [DOI] [PubMed] [Google Scholar]
- 3.Alexander R, Griffith G. Anomalies of the coronary arteries and their clinical significance. Circulation. 1956;14(5):800–5. doi: 10.1161/01.cir.14.5.800. [DOI] [PubMed] [Google Scholar]
- 4.Cheitlin M, De Castro C, McAllister H. Sudden death as a complication of anomalous left coronary origin from the anterior sinus of Valsalva, A notso-minor congenital anomaly. Circulation. 1974;50(4):780–87. doi: 10.1161/01.cir.50.4.780. [DOI] [PubMed] [Google Scholar]
- 5.Liberthson R, Dinsmore R, Fallon J. Aberrant coronary artery origin from the aorta. Report of 18 patients, review of literature and delineation of natural history and management. Circulation. 1979;59(4):748–54. doi: 10.1161/01.cir.59.4.748. [DOI] [PubMed] [Google Scholar]
- 6.Barth C, III, Roberts W. Left main coronary artery originating from the right sinus of Valsalva and coursing between the aorta and pulmonary trunk. J Am Coll Cardiol. 1986;7(2):366–73. doi: 10.1016/s0735-1097(86)80507-1. [DOI] [PubMed] [Google Scholar]
- 7.Goldstein P, Pittman D, Gay T, Brandt C. Anomalous origin of the right coronary artery from the ascending aorta: Case history. Angiology. 1990;41(2):164–66. doi: 10.1177/000331979004100213. [DOI] [PubMed] [Google Scholar]
- 8.Taylor A, Rogan K, Virmani R. Sudden cardiac death associated with isolated congenital coronary artery anomalies. J Am Coll Cardiol. 1992;20(3):640–47. doi: 10.1016/0735-1097(92)90019-j. [DOI] [PubMed] [Google Scholar]
- 9.Ali M, Hanley A, McFadden E, Vaughan C. Coronary artery anomalies: A practical approach to diagnosis and management. Heart Asia. 2011;3(1):8–12. doi: 10.1136/ha.2010.003244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Varela D, Teleb M, Said S, et al. Congenital absence of left circumflex presenting after an emotional stressor. Pol J Radiol. 2015;80:529–31. doi: 10.12659/PJR.895872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamanaka O, Hobbs R. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21(1):28–40. doi: 10.1002/ccd.1810210110. [DOI] [PubMed] [Google Scholar]
- 12.Hongsakul K, Suwannanon R. Congenital absence of left circumflex artery detected by computed tomography coronary angiography: A case report. Case Rep Vasc Med. 2012;2012:204657. doi: 10.1155/2012/204657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Villa A, Sammut E, Nair A, et al. Coronary artery anomalies overview: The normal and the abnormal. World J Radiol. 2016;8(6):537–55. doi: 10.4329/wjr.v8.i6.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo J, Xu M. Congenital absence of the left circumflex artery associated with inferior myocardial infarction. Intern Med. 2012;51(1):71–74. doi: 10.2169/internalmedicine.51.6141. [DOI] [PubMed] [Google Scholar]
- 15.Fugar S, Issac L, Okoh A, et al. Congenital absence of left circumflex artery: A case report and review of the literature. Case Rep Cardiol. 2017;2017:6579847. doi: 10.1155/2017/6579847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oliveira M, de Fazzio F, Mariani Junior J, et al. Superdominant right coronary artery with absence of left circumflex and anomalous origin of the left anterior descending coronary from the right sinus: An unheard coronary anomaly circulation. Case Rep Cardiol. 2015;2015:721536. doi: 10.1155/2015/721536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quijada-Fumero A, Pimienta-González R, Rodriguez-Esteban M. Absence of left circumflex with superdominant right coronary artery. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-206782. pii: bcr2014206782. [DOI] [PMC free article] [PubMed] [Google Scholar]