Abstract
Background
Gastric electrical stimulators (GESs) have been used to treat refractory gastroparesis in patients who fail initial therapies such as dietary modifications, control of psychological stressors and pharmacologic treatment. More recently, gastric peroral endoscopic pyloromyotomy (G-POEM) has emerged as a novel endoscopic technique to treat refractory gastroparesis. We present a case series of patients with refractory gastroparesis who failed treatment with an implanted GES that were safely treated with G-POEM performed under fluoroscopy as a salvage therapy.
Methods
Cases of G-POEM performed on patients with refractory gastroparesis who failed treatment with a GES were retrospectively reviewed. All G-POEM procedures were performed under fluoroscopic guidance with the GES still in place. Gastroparesis Cardinal Symptoms Index (GCSI) and gastric emptying scintigraphy were assessed before and after the procedure. Patients were followed up for up to 18 months post procedure.
Results
Five patients underwent G-POEM after failing treatment with a GES. Under fluoroscopy, the GES and their leads were visualized in different parts of the stomach. One GES lead was observed at the antrum near the myotomy site. All procedures were successfully completed without complications. Patients’ GCSI decreased by an average of 62% 1 month post procedure. Patients also had notable improvements in gastric emptying 2 months post procedure.
Conclusion
In patients with refractory gastroparesis who have failed treatment with a GES, G-POEM can be safe and effective without removing the GES. To visualize the GES and avoid cutting GES leads during myotomy, the procedure should be performed under fluoroscopy.
Keywords: gastroparesis, G-POEM, pyloromyotomy, gastric electrical stimulator, fluoroscopy
Introduction
Gastroparesis is a condition resulting from many factors including reduced gastric motility, poor fundal accommodation and pylorospasm leading to delayed gastric emptying. It is a chronic motility disorder with limited therapeutic options [1]. The most common etiologies of gastroparesis include diabetes mellitus and intestinal surgery; however, many cases are idiopathic. Initial treatment strategies involve dietary modification, control of psychological stressors and pharmacologic therapies. More invasive interventions such as laparoscopic pyloroplasty or gastrostomy can be performed in patients who fail primary treatment. However, these invasive measures are often not very effective [2]. Gastric electrical stimulators (GESs) have also been used to treat refractory gastroparesis, and it has become a treatment option in patients who fail initial therapies [3].
More recently, gastric peroral endoscopic pyloromyotomy (G-POEM) has emerged as a novel endoscopic technique to treat refractory gastroparesis [4–11]. Early experience with G-POEM has demonstrated promising results, though data on its procedural safety and long-term efficacy are limited [4–8]. Our earlier studies have shown successful use of G-POEM in treating different subtypes of gastroparesis (post-infectious, post-surgical and idiopathic) with sustained control of symptoms and improved quality of life over a follow-up period of 6 months [9,10]. A multicenter study of 30 patients has also demonstrated effective use of G-POEM in treating refractory gastroparesis [11]. We present a case series of patients with refractory gastroparesis who failed treatment with an implanted GES (Enterra, Medtronic, Minneapolis, MN) who were subsequently treated with G-POEM performed under fluoroscopy as a salvage therapy.
Patients and methods
Patients
Cases of G-POEM performed on patients with refractory gastroparesis who failed treatment with a GES were retrospectively reviewed. The GES was not removed or turned off prior to the procedure. We used the Gastroparesis Cardinal Symptoms Index (GCSI) to assess the severity of patients’ symptoms of nausea/vomiting, post-prandial fullness and bloating. GCSI (2-week recall period) and gastric emptying scintigraphy were assessed before and after the procedure. Procedure-related adverse events were also recorded. All patients were very ill with nausea and vomiting and could not obtain an appointment with surgery in time to remove the GES before G-POEM.
G-POEM procedure
To visualize the GES and its leads, all G-POEM procedures were performed under fluoroscopy by a single expert endoscopist with an advanced endoscopy trainee under an IRB-approved protocol. Patients received a single dose of prophylactic intravenous (IV) antibiotics prior to the procedure (4.5 grams of piperacillin/tazobactam or 0.5 grams of levofloxacin). General anesthesia was used in all cases. Cardiac rhythm, pulse oximetry and blood pressure were monitored throughout the procedure. Patients’ GESs were not turned off prior to the procedure.
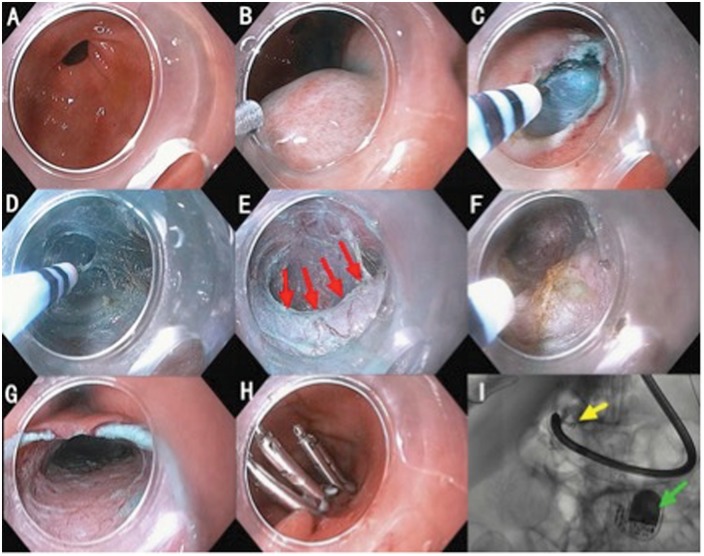
Patients were placed in a supine position after being kept on liquid diet for 2 days and nil per os (NPO) for 12 hours. The stomach was lavaged with water and any gastric residues were removed by endoscopic suction. A routine upper endoscopic evaluation was performed, after which a mucosal entry site was identified at the gastric antrum on the greater curvature of the stomach. Fluoroscopic guidance was used to identify the site of the GES and the leads. This entry site was approximately 5 cm proximal to the pylorus. A premixed solution of methylene blue and normal saline was injected at the identified site with a sclerotherapy needle (23G, NM4004–042, Olympus, Japan) to raise a mucosal bleb. A 2-cm mucosal incision was made with a hook knife (KD-620LR, Olympus, Japan) or hybrid knife (ERBE Hybrid Knife, ERBE USA Incorporated, Marietta, GA, USA). A submucosal tunnel was then created from the mucosal entry site to about 1 cm distal to the pylorus. Selective myotomy of the pyloric circular muscle was subsequently performed, starting 0.5 cm beyond the pylorus and extending about 2–3 cm proximally into the antrum. After myotomy, the tunnel was rinsed with saline and the mucosal entry site was closed with hemostatic clips (Figure 1).
Figure 1.
G-POEM procedure steps and a fluoroscopy image. (A) Pylorus. (B) Mucosal bleb. (C) Mucosotomy. (D) Submucosal tunneling. (E) Pyloric ring (red arrows). (F) Pyloromyotomy. (G) Submucosal tunnel. (H) Mucosotomy closure with endoclips. (I) Fluoroscopy image demonstrating implant gastric electrical stimulator (green arrow) and its leads (yellow arrows).
Post-procedure follow-up
All patients were admitted to the hospital after the procedure and kept NPO. During this period, patients received IV piperacillin/tazobactam or levofloxacin, as well as an IV proton pump inhibitor (PPI). A gastrograffin swallow study was performed on post-operative day 1. If no leakage of gastric contents was observed, the patient’s diet was advanced to liquid diet and then soft diet as tolerated. The patients were discharged on post-operative day 2 with 5 days of oral antibiotics with either amoxicillin/clavulanate or levofloxacin. Patients were also prescribed 2 months of PPI therapy. Patients were followed up in clinic 1 month post procedure and underwent repeat gastric emptying study 2 months post-procedure. Patients were subsequently followed up at 6, 12 and 18 months post procedure to assess their symptom control.
Results
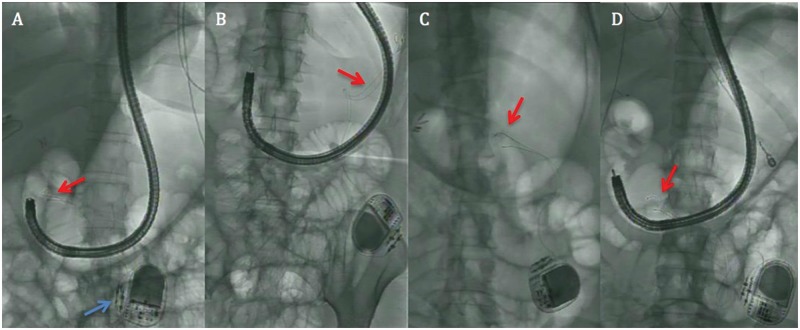
Five patients successfully underwent fluoroscopic G-POEM after failing treatment with a GES that had been in place for at least 3 years prior to the procedure (Table 1). There were no complications. Apart from one case, whose fluoroscopic images were not available, the other four GESs and their leads were visualized under fluoroscopy during the procedure. No spastic or abnormal contractions were encountered during submucosal tunneling. The leads in one case were directly at the myotomy site (Figure 2A). The myotomy length in four procedures was 3 cm and 2 cm during one case. All mucosal entry sites were closed using three to five hemostatic clips without difficulty. The mean procedure time was 45 minutes (range 31–55 minutes).
Table 1.
Report of patient demographics with clinical details, procedure details, as well as description of clinical improvement after gastric peroral endoscopic pyloromyotomy (G-POEM)
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Age | 34 | 45 | 36 | 41 | 35 |
| Gender | Female | Female | Female | Female | Female |
| Etiology of gastroparesis | Post-infectious | Idiopathic | Idiopathic | Idiopathic | Idiopathic |
| Duration of gastroparesis, years | 2 | 6 | 7 | 3 | 1.7 |
| Year gastric electrical stimulator placed | 2014 | 2013 | 2013 | 2013 | 2013 |
| Number of hospitalizations in the year prior to G-POEM | 3 | 4 | 2 | 4 | Unknown |
| Number of ER visits in the year prior to G-POEM | 2 | 8 | 5 | 0 | Unknown |
| Procedure time, minutes | 55 | 45 | 31 | 47 | 56 |
| Myotomy length, centimeters | 3 | 3 | 3 | 2 | 3 |
| Pre-procedure GCSI | 23 | 26 | 32 | 23 | 37 |
| GCSI at 1 month post procedure | 6 | 8 | 16 | 9 | 13 |
| Pre-procedure gastric emptying scintigraphya | 95% | 38% | 49% | 90% | 64% (at 2 hours) |
| Gastric emptying scintigraphy at 2 months post procedurea | 45% | 8% | 2% | 16% | 5% |
| Length of follow-up post procedure, months | 18 | 18 | 12 | 6 | 1 |
| Number of hospitalizations after G-POEM | None | None | None | None | None |
| Number of ER visits after G-POEM | 1 | None | None | None | None |
GCSI, Gastroparesis Cardinal Symptoms Index; ER, emergency room.
aMean % gastric residual after 4 hours during gastric-emptying scintigraphy.
Figure 2.
Fluoroscopic images of the gastric electrical stimulator (GES) and its leads during G-POEM. A series of fluoroscopic images, each from a different G-POEM case, show the implanted gastric electrical stimulator (blue arrow) and its leads (red arrow). The GES leads are located in different parts of the stomach during each case. Frame (A) shows the leads of the stimulator at the antrum of the stomach directly at the myotomy site (red arrow). Fluoroscopic images were not available for one of the five cases.
All five patients reported significant improvement in symptoms of nausea, vomiting and postprandial fullness, with their GCSI decreasing by an average of 62% 1 month post procedure, which was statistically significant using the t-test method (p = 0.001). Gastric emptying scintigraphy performed prior to G-POEM revealed that the patients’ mean gastric residual at 4 hours was around 71% in four patients. This decreased to 18% during gastric emptying scintigraphy performed 2 months post procedure in the same four patients (Table 1). There was no significant improvement in pain at 1, 6 and 12 months post procedure. One patient subsequently underwent removal of the gastric stimulator 6 months post procedure and continues to do well. In the year prior to undergoing G-POEM, our patients had on average 3.3 hospitalizations as well as 3.75 additional emergency room (ER) visits for gastroparesis-related issues. Post procedure, none of the patients was hospitalized and only one patient presented to the ER once for gastroparesis symptoms. Following their procedures, two patients were followed for 18 months, one patient for 12 months, one for 6 months and one for 1 month. All patients demonstrated sustained control of their symptoms of nausea, vomiting, bloating and early satiety (Figure 3). We were unable to test for statistical significance on the improvement in GCSI at 6, 12 and 18 months post procedure due to the small sample size. However, the aim of this study was to visualize the stimulator lead during the procedure and therefore avoid cutting on it.
Figure 3.
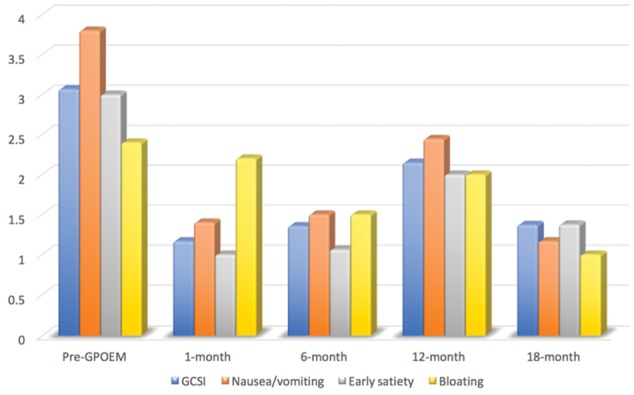
This chart shows the mean Gastroparesis Cardinal Symptoms Index (GCSI) score as well as the subsets of nausea/vomiting, early satiety and bloating in our patients prior to G-POEM and at 1, 6, 12 and 18 months’ follow-up post procedure. Of note, the GCSI score is the mean of all nine subsets, each scored on a 1–5 scale, as opposed to the sum of these subsets. There was a statistically significant improvement in GCSI score 1 month post procedure (p =0.001).
Discussion
G-POEM is emerging as a minimally invasive endoscopic procedure for the treatment of refractory gastroparesis. The first multicenter experience with G-POEM demonstrated effective treatment in 30 patients with various subtypes of gastroparesis [11]. Our center has also demonstrated sustained control of gastroparesis symptoms as well as quality of life over a 6-month follow-up period [10]. To the best of our knowledge, this study is the first to show successful use of G-POEM in patients with refractory gastroparesis who had failed treatment with an implanted GES. Furthermore, this study is the first to show that G-POEM should be performed under fluoroscopy in patients with an implanted GES to avoid cutting GES leads during myotomy.
Currently, there is a lack of consensus on the optimal technique for G-POEM. Many of the reported studies to date have had technical differences and none of them reported use of fluoroscopy [9]. Each GES has two leads that are usually placed at the antrum of the stomach above the pylorus [12,13]. G-POEM is also performed at the antrum, and it is unknown whether the GES should be removed before the procedure. We decided to perform G-POEM under fluoroscopy to visualize the GES leads and to guide the direction of the submucosal tunnel away from these leads. A two-dimensional fluoroscopic view was sufficient to provide this guidance. According to the literature, GES leads should be secured in the muscularis propria along the greater curvature of the stomach, 10 cm proximal to the pylorus [12]; therefore, we did not expect to encounter them during the submucosal tunneling process. However, during fluoroscopic G-POEM, the GES leads were visualized at different parts of the stomach (Figure 2). One GES lead was at the myotomy site and, without fluoroscopy, the lead may have been inadvertently resected.
GESs are approved for human use and have been used to treat recalcitrant gastroparesis over the last several years, with the majority of clinical experience at specific centers proficient with this procedure [3]. Though GES has been shown to improve gastroparesis symptoms, long-term studies show complication rates as high as 7–10% [14]. The most common complication is infection of the subcutaneous pocket in which the pacer is implanted [14,15]. Long-term studies have also shown gastric stimulation to maintain improved gastroparesis symptoms in select patients for up to 10 years [15]. However, individual response to GES remains unpredictable, and there are still no reliable prognostic features that indicate which patients will or will not respond well to this therapy [3].
Despite the exciting potential that G-POEM offers and the encouraging results reported, we believe it is still too early to recommend for or against implementing G-POEM earlier in the treatment approach for patients with gastroparesis. However, given the significant long-term complications and unpredictable response to GES in patients with refractory gastroparesis, G-POEM can serve as an important alternative therapy in treating this subgroup of patients who fail treatment with a GES. In addition, since GESs have a different mechanism of action than G-POEM, it is possible that both interventions may complement each other to achieve symptomatic relief in patients with refractory gastroparesis. Though additional long-term follow-up data are needed on the efficacy of G-POEM, preliminary results, including those from our study, demonstrate that G-POEM has the potential to become an alternate and less invasive treatment for refractory gastroparesis.
In conclusion, we have demonstrated the technically successful, safe and effective use of fluoroscopic G-POEM in treating a select group of patients with refractory gastroparesis who have failed treatment with a GES. We feel that G-POEM should be performed under fluoroscopic guidance in this subset of patients to ensure safety, unless the GES is removed prior to G-POEM. To our knowledge, this has not been reported in the literature. Since an increasing number of patients who fail treatment with a GES may undergo G-POEM, performing fluoroscopic G-POEM should become routine practice in this subset of patients. More robust data on the long-term outcomes of G-POEM, comparative studies to other conventional therapies and better defined selection criteria for patients to undergo G-POEM are very much needed and should be the focus of future research.
Acknowledgements
An abstract of this study was presented at the proceedings of the 2016 American College of Gastroenterology conference in Las Vegas, NV, and received a Presidential Poster Award.
Conflict of interest statement: none declared.
References
- 1. Camilleri M, Parkman HP, Shafi MA. et al. Clinical guideline: management of gastroparesis. Am J Gastroenterol 2013;108:18–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Toro JP, Lytle NW, Patel AD. et al. Efficacy of laparoscopic pyloroplasty for the treatment of gastroparesis. J Am Coll Surg 2014;218:652–60. [DOI] [PubMed] [Google Scholar]
- 3. Soffer EE. Gastric electrical stimulation for gastroparesis. J Neurgastroenterol Motil 2012;18:131–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shlomovitz E, Pescarus R, Cassera MA. et al. Early human experience with per-oral endoscopic pyloromyotomy (POP). Surg Endosc 2014;29:543–51. [DOI] [PubMed] [Google Scholar]
- 5. Chaves DM, de Moura EG, Mestieri LH. et al. Endoscopic pyloromyotomy via a gastric submucosal tunnel dissection for the treatment of gastroparesis after surgical vagal lesion. Gastrointest Endosc 2014;80:164. [DOI] [PubMed] [Google Scholar]
- 6. Chung H, Dallemagne B, Perretta S. et al. Endoscopic pyloromyotomy for post-esophagectomy gastric outlet obstruction. Endoscopy 2014;46 (Suppl 1):E345–6. [DOI] [PubMed] [Google Scholar]
- 7. Gonzalez JM, Vanbiervliet G, Vitton V. et al. First European human gastric peroral endoscopic myotomy for treatment of refractory gastroparesis. Endoscopy 2015;47 (Suppl 1):E135–6. [DOI] [PubMed] [Google Scholar]
- 8. Khashab MA, Stein E, Clarke JO. et al. Gastric peroral endoscopic myotomy for refractory gastroparesis: first human endoscopic pyloromyotomy (with video). Gastrointest Endosc 2013;78:764–8. [DOI] [PubMed] [Google Scholar]
- 9. Mekaroonkamol P, Li LY, Dacha S. et al. Gastric peroral endoscopic pyloromyotomy (G-POEM) as a salvage therapy for refractory gastroparesis: a case series of different subtypes. Neurogastroenterol Motil 2016;28:1272–7. [DOI] [PubMed] [Google Scholar]
- 10. Dacha S, Makaroonkamol P, Cai Q. et al. Outcomes and quality-of-life assessment after gastric peroral endoscopic pyloromyotomy. Gastrointest Endosc 2017;86:282–9. [DOI] [PubMed] [Google Scholar]
- 11. Khashab MA, Ngamruengphong S, Carr-Locke D. et al. Gastric peroral endoscopic myotomy for refractory gastroparesis: results from the first multicenter study on endoscopic pyloromyotomy (with video). Gastroinest Endosc 2016;83:AB495. [DOI] [PubMed] [Google Scholar]
- 12. Abell T, McCallum R, Hocking M. et al. Gastric electrical stimulation for medically refractory gastroparesis. Gastroenterology 2003;125:421–8. [DOI] [PubMed] [Google Scholar]
- 13. Abell TL, Van Cutsem E, Abrahamsson H. et al. Gastric electrical stimulation in intractable symptomatic gastroparesis. Digestion 2002;66:204–12. [DOI] [PubMed] [Google Scholar]
- 14. Anand C, Al-Juburi A, Familoni B. et al. Gastric electrical stimulation is safe and effective: a long-term study in patients with drug-refractory gastroparesis in three regional centers. Digestion 2007;75:83–9. [DOI] [PubMed] [Google Scholar]
- 15. McCallum RW, Lin Z, Forster J. et al. Gastric electrical stimulation improves outcomes of patients with gastroparesis for up to 10 years. Clin Gastroenterol Hepatol 2011;9:314–19. [DOI] [PubMed] [Google Scholar]