Abstract
Cardiac rehabilitation (CR) is a commonly used treatment for men and women with cardiovascular disease. To date, no single study has conclusively demonstrated a comprehensive benefit of CR. Numerous individual studies, however, have demonstrated beneficial effects such as improved risk-factor profile, slower disease progression, decreased morbidity, and decreased mortality. This paper will review the evidence for the use of CR and discuss the implications and limitations of these studies. The safety, relevance to special populations, challenges, and future directions of CR will also be reviewed.
Keywords: cardiac rehabilitation, cardiovascular disease, exercise therapy, lifestyle interventions, secondary prevention
Despite a trend towards decreasing mortality, cardiovascular disease (CVD) remains the major cause of death in the western world [1,2]. Improved management of acute myocardial infarction (MI), earlier diagnostic procedures, and advanced intervention techniques have resulted in an increasing number of CVD survivors. Early rehabilitation and risk-factor management for these individuals is essential to regain function and reduce the risk of a second adverse cardiac event.
The use of exercise therapy in post-MI survivors began gaining momentum in the late 1970s when it became clear that immobilization and reduced activity, which was standard therapy at that time, resulted in poor long-term prognosis and survival [3]. Over the past 30 years, exercise therapy has evolved into the multifactorial programs we know today as CR. These programs, which include nutrition counselling, smoking cessation, weight management, psychosocial counselling and metabolic risk-factor management, can be found in many hospitals and communities. The target population for CR has expanded, and includes men and women of all ages and those presenting with nonischemic CVD (Table 1). Several national organizations have published extensive recommendations and guidelines for CR [4,5,6].
Table 1.
Target populations for participation in cardiac rehabilitation programs
| Ischemic heart disease |
| Post-MI, coronary artery bypass graft, percutaneous |
| transluminal coronary angioplasty |
| Stable angina |
| Other heart conditions |
| Compensated heart failure |
| Controlled dysrhythmias |
| Automatic implanted cardioverter-defibrillate/pacemaker |
| Post-valve replacement |
| Cardiomyopathy |
| Myocardial aneurysm resection |
| Pre- and post-heart transplant |
| Congenital heart defects |
| Other chromic diseases |
| Stroke |
| Peripheral vascular disease |
| High risk of developing CVD |
CVD, Cardiovascular disease; MI, myocardial infarction.
The World Health Organization has defined CR as: "... the sum of activity required to ensure cardiac patients the best possible physical, mental and social conditions so that they may, by their own effort, regain as normal a place in the community, and lead an active life" [7].
The goals of CR are restoration of optimal physiological, psychological and vocational status, and reduction of risk of cardiac morbidity and mortality.
As CVD is a multifactorial disease, the beneficial outcomes from CR are numerous. Possible outcomes include improvement in lifestyle, CVD risk-factors, cost of care, disease progression, morbidity, and mortality. To date, no single study has conclusively demonstrated a comprehensive benefit of CR. However, such a study is unlikely to ever be conducted, as it would be unethical to assign individuals with CVD to a non-CR control group. Instead, the data from various studies, each investigating one or two outcomes, must be compiled to identify the overall benefit of CR.
The present review will trace the evidence from studies on exercise therapy in post-MI survivors to the comprehensive programs we know today. Excellent reviews of dietary and smoking interventions have been written, and the reader is directed to these [8,9]. At the end of this review, evidence in other populations will be discussed, as well as the challenges facing CR programs today and areas requiring further study.
The modern CR program
Figure 1 outlines the multidisciplinary nature of the modern CR program. CR comprises three distinct phases: inpatient, outpatient, and in the community/home. Participation in these programs is determined by appropriate risk stratification to maximize health care resources and benefits. The inpatient program consists of low-level activities that gradually progress throughout the hospital stay to prevent reconditioning. Education and counselling also begin at this time. The outpatient program is the most common CR model in use and may last from 2 to 4 months. These programs combine physician-supervised exercise sessions with cardiovascular risk reduction, commonly using a case management model. A full risk-factor and lifestyle assessment is conducted both at the beginning and end of the program. On completion of the out-patient program, patients can then continue in a local community center CR program. Patients who are at low risk may appropriately continue their program in a home-based setting.
Figure 1.
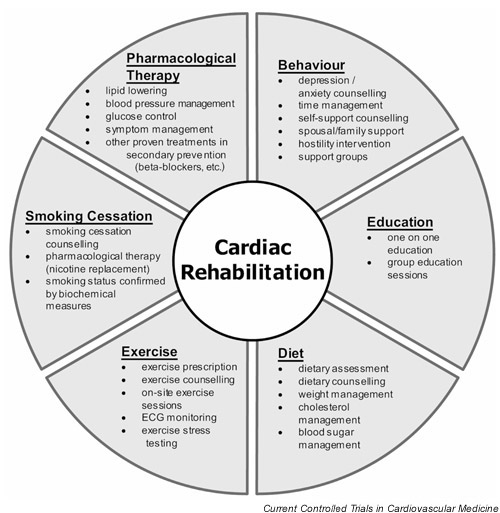
Diagrammatic outline of the modern cardiac rehabilitation program.
ECG, Electrocardiography.
Evidence for the benefits of CR
Mortality trials
The benefits of physical activity and exercise have been recognized for centuries. Numerous epidemiological studies have associated physical activity participation with reduced CVD risk and mortality [10,11,12]. Based on this association, early investigations set out to determine the survival benefits of exercise therapy and CR. These studies were mainly restricted to middle-aged men who had experienced a prior MI. Interventions lasted from 6 weeks to 3 years and consisted of mainly exercise therapy, while a few included other lifestyle strategies (dietary, smoking cessation and psychosocial counselling). The results of these studies have varied. Some have reported nonsignificant changes in mortality [13,14,15,16,17], while others have demonstrated significant reductions in mortality [18,19,20,21]. Sample sizes in these studies varied from 167 to 651 participants, much smaller than other mortality trials, which may account for some of the nonsignificant findings. Differences in the intervention method, the duration, and the follow-up period also confound comparisons between studies.
Much of the evidence to support reduced mortality from CR is provided by two meta-analyses that have been conducted to combine the results of the earlier exercise therapy and CR studies [13,14,15,16,17,18]. These investigations were restricted to studies of men and women post-MI. Oldridge et al included data from 20 studies totalling 4347 patients (2202, intervention; 2145, control) [22], while O'Connor et al included 22 studies totalling 4554 patients (2310, intervention; 2244, control) [23]. All-cause and cardiovascular mortality in the exercise therapy group were significantly reduced compared with the control group (Table 2). No significant difference in nonfatal MI was reported in either analysis; in fact, slightly more occurrences were noted in the intervention group. The authors speculated that those participants in the exercise therapy group were more likely to survive a repeat MI than those in the control group. The similar finding between these two meta-analyses is not surprising since 16 of the studies analyzed were common to both; the results should therefore not be considered independent of one another. Because women accounted for less than 3% of the patients, gender-related outcomes were not analyzed. The relative reduction of all-cause and cardiovascular mortality (approximately 20–25%) is similar to the reduction in mortality observed in lipid-lowering trials [24].
Table 2.
Summary of major findings from two meta-analyses of randomized exercise therapy and cardiac rehabilitation trials
| Oldridge | O'Connor | |
| et al [22] | et al [23] | |
| All-cause mortality | 0.76 (0.63–0.92)* | 0.80 (0.66–0.96)‡ |
| Cardiovascular mortality | 0.75 (0.62–0.93)† | 0.78 (0.63–0.96)‡ |
| Sudden death | Not reported | 0.92 (0.69–1.23) |
| Nonfatal myocardial infarction | 1.15 (0.93–1.42) | 1.09 (0.88–1.34) |
Data presented as odds ratio (95% confidence intervals). Values below 1.00 favor cardiac rehabilitation intervention. *P = 0.004, †P = 0.006; ‡ significantly lower than comparison group, no P values reported.
Since these two meta-analyses were completed, four other studies have been published reporting outcomes from 2 to 19 years of follow-up (summarized in Table 3) [20,21,25,26]. Three of these studies reported results of earlier follow-up periods that were incorporated into the previous meta-analyses [14,18,27], while the fourth had not been previously reported [20].
Table 3.
Summary of recent randomized exercise therapy and cardiac rehabilitation (CR) trials investigating the effects on long-term mortality
| Follow-up | |||||
| Cohort | Intervention | Comparison group | (years) | Relative risk reduction* | |
| Hedback | 305 men and women, | Multifactorial, 2 x per week | Nonrandomized reference | 10 | 27% all-cause mortality |
| et al [21] | post-MI, < 65 years | exercise sessions, 3 months | with no CR | (P < 0.01) | |
| 24% cardiovascular mortality | |||||
| (P <0.001) | |||||
| 33% nonfatal MI (P <0.001) | |||||
| PRECOR | 182 men post-MI, | Multifactorial, 3 x per week | Control (usual care, | 2 | 7% absolute reduction in |
| Group [20] | < 65 years | exercise sessions; or | no intervention) | all-cause mortality† (P = 0.08) | |
| counselling only, 6 weeks | |||||
| Hamalainen | 375 men and women, | Multifactorial, exercise | Randomized control group | 15 | 4% all-cause mortality |
| et al [25] | post-MI, < 65 years | sessions, 3 years | (not significant) | ||
| 18% cardiovascular mortality | |||||
| P = 0.04) | |||||
| 43% sudden death | |||||
| (P = 0.006) | |||||
| NEHDP [26] | 651 men, post-MI, | Exercise only, 2 years | Control (usual care, | 19 | No reported benefits |
| < 65 years | no intervention) |
MI, Myocardial infarction; NEHDP, The National Exercise and Heart Disease Project. * Relative risk reduction in favor of intervention. † No deaths occurred in CR intervention. results are based on comparison of CR intervention with counselling intervention and control (usual care, no intervention) combined.
First, the PRECOR group randomized men to either a 6-week CR, a counselling program, or control (usual care, no intervention) [20]. No difference in all-cause mortality was observed between the three groups after 2 years follow-up but, when the counselling program and control groups were combined and compared with the CR group, a significant difference did exist in favor of CR.
In the second study, Hedback and Perk found no difference in all-cause or cardiovascular mortality after 5 years of follow-up between the nonrandomized CR and reference groups [27]. At 10 years, significant reductions were observed in these outcomes as well as in sudden death and nonfatal MI [21].
Hamalainen et al randomized 375 participants to either a multifactorial CR intervention or control (usual care, no intervention for 10 years [19]. The authors reported significant reductions in sudden death and cardiovascular mortality, with no difference in all-cause mortality or nonfatal MI. After 15 years of follow-up, these reductions in the intervention group persisted for sudden death and cardiovascular mortality [25].
Finally, the National Exercise and Heart Disease Project had the longest follow-up period to date (19 years), yet failed to demonstrate any reduction comparing exercise therapy with control (usual care, no intervention), in all-cause or cardiovascular mortality, with no report on nonfatal MI [26]. This result was consistent during the five follow-up periods from 3 to 19 years. It is possible that the duration of the exercise-only intervention, 8 weeks, was not long enough to produce lasting benefits and therefore not as effective as the interventions of the other studies.
Despite the lack of a consistent reduction in mortality and the myriad of differences in these studies, there is a trend towards reduced all-cause and cardiovascular mortality. Owing to the study populations being overwhelmingly limited to men younger than 65 years post-MI, investigation of gender-related results was not possible. The possible benefit of CR in older adults and in those who have CVD but have not experienced a previous MI is also unclear.
Comprehensive disease regression trials
More recent CR trials have focused on other clinical outcomes such as atherosclerotic progression (summarized in Table 4). This is due to the high correlation between disease progression and cardiac events [28]. The use of disease progression as an outcome allows for a smaller sample size and follow-up period than required by a mortality trial.
Table 4.
Summary of comprehensive cardiac rehabilitation trials that used coronary atherosclerotic disease progression as the primary outcome
| Results | ||||
| Study | Follow-up duration | Control | Intervention | P* |
| Schuler et al [29]† | 1 year (n = 36) | 33% progression, | 28% progression, | < 0.05 |
| 61% no change, | 33% no change, | |||
| 6% regression | 39% regression | |||
| Niebauer et al [30]† | 5 years (n = 25) | 75% progression, | 38% progression, | ns |
| 13% no change, | 38% no change, | |||
| 13% regression | 25% regression | |||
| Schuler et al [31]† | 1 year (n = 113) | 48% progression, | 23% progression, | < 0.05 |
| 35% no change, | 45% no change, | |||
| 17% regression | 33% regression | |||
| Niebauer et al [33]† | 6 years | 74% progression, | 59% progression, | < 0.0001 |
| 26% no change, | 22% no change, | |||
| 0% regression | 19% regression | |||
| The Lifestyle Heart Trial [34,35]‡ | 1 year (n = 41) | 2.28 (-3.00 to 4.86) (n = 15) | -1.75 (-4.08 to 0.58) (n = 18) | 0.02 |
| (53% progression, | 18% progression, | |||
| 5% no change, | (0% no change, | |||
| 42% regression) | 82% regression) | |||
| 5 years (n = 35) | 11.77 (3.40–20.14) (n = 15) | -3.07 (-5.91 to -0.24) (n = 20) | 0.001 | |
| SCRIP [36]§ | 4 years (n = 246) | -0.045 ± 0.073 | -0.024 ± 0.067 | 0.02 |
| (50% progression, | (50% progression, | |||
| 20% no change, | 18% no change, | |||
| 10% regression, | 20% regression, | |||
| 21% mixed changes) | 12% mixed changes) | |||
* Between-group comparisons; ns, not significant. † Progression, ≥ 10% decrease; no change, ≤ 10% change; regression, ≥ 10% increase in percent minimal diameter. Patient assigned an average score when multiple stenoses analyzed. ‡ Average percent diameter stenosis change from baseline; 186 lesions analyzed (77 control, 109 intervention) by quantitative coronary angiography. Results reported from participants completing a 5-year follow-up. § Absolute change in minimal diameter stenosis (mm) per year as assessed by quantitative coronary angiography.
Schuler at al studied a group of 36 men with stable angina and coronary artery stenosis, and assigned them to either CR (dietary counselling, twice-weekly exercise sessions, and a home exercise program) intervention or to control (usual care, no intervention) for 12 months based on proximity to the study site [29]. Participants were asked not to use lipid-lowering medications for the duration of the study. When participants were grouped according to progression – no change or regression of stenosis – the intervention group underwent significantly less progression than the control group. The authors also noted significantly improved myocardial perfusion during maximal stress testing and decreased total cholesterol in the intervention group.
This cohort was again followed-up 4 years later, at which time the significant differences in disease progression between groups no longer existed [30]. An increase in weight and total cholesterol between years 1 and 5, possibly the result of decreased dietary adherence, may have attenuated the differences in disease progression between groups.
Limitations of the previous study (small sample size, group assignment of convenience) led the authors to conduct a second study in 113 men with coronary artery stenosis [31]. The intervention was identical to the previous study but participants were randomly assigned to either intervention or control (usual care, no intervention). Participants in the intervention group underwent significantly greater reductions in dietary fat and total cholesterol, and a significantly greater increase in maximal oxygen consumption, compared with the control group. This resulted in a more favorable lipid profile, and reduced weight, compared with control. Significantly fewer participants in the intervention group experienced disease progression compared with the control group at 1 year (23% versus 48%, respectively; P <0.05). Further investigation of this cohort did not determine any difference in coronary collateral formation between groups [32].
Five years later, there was still a significant difference between the intervention and control groups with respect to disease progression (59% versus 74%, respectively; P <0.05) [33]. This difference was significant for 'per lesion' and 'per patient' comparisons. No significant differences existed in clinical events, and the significant differences in lipid profile and weight that occurred at 12 months were no longer evident at 6 years. The authors reported a significant correlation between exercise capacity and relative stenosis diameter (r = 0.319, P <0.01). In contrast to the previous study, the exercise capacity of the intervention participants continued to improve between years 1 and 6.
Two controlled studies that demonstrated the benefits of comprehensive CR are (Table 4) the Lifestyle Heart Trial (LHT) [34,35] and the Stanford Coronary Risk Intervention Project (SCRIP) [36]. Both of these studies included men and women with documented coronary artery disease, and used disease progression (assessed by quantitative coronary angiography) as the outcome.
The LHT
The unique approach of the LHT was to demonstrate the effectiveness of aggressive lifestyle management, with no lipid-lowering medications, to induce disease regression. Eligible men and women were identified from their hospital charts and randomly assigned either to the intervention or control (usual care, no intervention) without prior consent. These individuals were then contacted by the study coordinator, informed of their group assignment and asked to provide informed consent. Of the 93 individuals contacted, only 48 (five women) agreed to participate. The intervention consisted of an initial 1-week retreat, a low-fat vegetarian diet, twice-weekly group support meetings, stress management, and monitored weekly exercise.
Adherence to the intervention was reported to be high. After 1 year, significant reductions in weight and lipid values were noted in the intervention group. All detectable lesions were included in the final analysis. With respect to percent diameter stenosis, disease regression occurred in the intervention group while the control group experienced disease progression. This difference was significant, even when lesions less than 50% stenosed were excluded. The authors also noted a dose-dependent relationship between program adherence and change in percent diameter stenosis.
After 5 years, adherence to the program decreased modestly for the intervention participants [35]. There was also a modest deterioration of lipid values between years 1 and 5 in the intervention group and participants gained back one-half of the weight lost in the first year. Despite this, participants in the intervention group continued to undergo further disease regression (7.9% relative regression) while the control group underwent disease progression (27.7% relative progression). The authors again noted a dose-dependent relationship between program adherence and change in percent diameter stenosis. Participants in the control group experienced nearly double the amount of cumulative combined cardiovascular events than in the intervention group (2.25 versus 0.89 events per patient).
This study identified the importance of lifestyle modification for the treatment of CVD and demonstrated its feasibility in a self-selected population. However, incorporation of this program into daily practice may prove difficult because it requires a great deal of resources per patient and highly motivated individuals; over 50% of those participants randomized to the intervention program refused participation and were not followed on an intent to treat basis.
SCRIP
The SCRIP continues to be one of the largest, randomized, long-term multifactorial CR studies to date [36]. The intervention used in this study is markedly different from that of previous studies; participants randomized to the intervention underwent counselling sessions by a nurse and a dietician every 2–3 months only, and no on-site exercise sessions were conducted. During the counselling sessions, participants were prescribed a home exercise program, prescribed lipid-lowering medications, and underwent a smoking cessation program as required. Unlike previous studies, the SCRIP did not include an on-site exercise program; however, exercise capacity increased significantly in the intervention group compared with in the control (usual care, no intervention) group (1.7 ± 2.4 versus 0.7 ± 2.1 metabolic equivalents [METs] above baseline values, respectively; P = 0.001). The inclusion of lipid-lowering medications is also a departure from the other studies, but this reflects changes in clinical practice and the use of all clinical tools at the disposal of the CR program.
After 4 years, lipids, systolic blood pressure, body composition, and fasting glucose all significantly improved in the intervention group compared with the control group. There was no change in the proportion of smokers after 4 years. Participants in the intervention group underwent significantly less absolute change in the minimal, and mean, diameter of diseased vessels compared with the control group. This was significant for both 'per patient' and 'per vessel' analyses, and remained significant after adjusting for age and baseline segment diameter.
Although not an a priori endpoint, the intervention group experienced significantly fewer cardiac events compared to participants in the control group (n = 44 versus n = 25, respectively; P = 0.05). This finding is similar to that of the LHT. The majority of the events experienced by the intervention group occurred during the study's first year, which were mostly percutaneous transluminal coronary angioplasty (PTCA) procedures. The authors speculated that the increased contact with the intervention staff might have uncovered the need for these patients to undergo the procedure at an earlier stage.
This study is unique in that it used a physician-supervised, nurse-managed intervention, a method that is easily replicable in other clinics and does not require on-site exercise sessions. However, the SCRIP intervention used risk-factor targets to guide treatment strategies, which were considered to be aggressive at the time and beyond current guidelines. This may have resulted in a bias towards success for the intervention group.
These studies have demonstrated that CR with or without lipid-lowering medication use is effective at reducing disease progression. The reduction of progression observed in the SCRIP is equivalent or superior to a number of trials investigating the effects of lipid-lowering only [28,37,38], and reflects the benefit of multifactorial CR interventions utilizing all clinical tools. The mean regression demonstrated in the LHT by lifestyle changes alone has not been realized in most pharmacological interventions. In spite of the small sample size and self-selected population in the LHT, these results are impressive. The reduction in events reported in the LHT and the SCRIP attests to the benefit of disease regression by CR.
Risk-factor modification
CR studies investigating clinically relevant endpoints have been limited to those previously discussed. As with other CVD interventions, CR is aimed at modifying various CVD risk-factors based on the evidence that risk-factor reduction will reduce morbidity and mortality. The SCRIP demonstrated that CR is effective at comprehensive risk-factor modification, resulting in reduced disease progression and clinical events. Table 5 summarizes the strength of evidence for the use of CR for CVD risk-factor modification and quality of life improvements.
Table 5.
Strength of evidence ratings for modification of various outcomes and cardiovascular disease risk-factors as a result of cardiac rehabilitation participation
| Strength of | Highlighted | |
| Outcome | evidence* | references |
| Smoking cessation, relapse prevention | B | [39,79] |
| Improved lipid profile | A | [31,36] |
| Decreased blood pressure | B | [19] |
| Improved blood sugar control | B | [80] |
| Increased exercise capacity | A | [81,82] |
| Increased physical activity | B | [83] |
| Decreased body weight | B | [36] |
| Improved psychosocial well-being | A | [84,85] |
| Improved social functioning | B | [86] |
* A, Evidence provided by well-designed, controlled trials with statistically significant results consistent across trials; B, evidence provided by observational studies or controlled trials with less consistent results; C, opinion of expert consensus due to a lack of controlled trials and/or consistent results.
The case management model
With the growing number of CVD survivors, traditional exercise-based CR programs will not have the resources to meet the demand for their services. Exercise-based programs may not be necessary for patients at low and moderate risk. The SCRIP demonstrated that CR could be effective without a supervised exercise component. The SCRIP and other studies have led to the development of the nurse case management system.
The MultiFit model is a physician-supervised, nurse-managed intervention. DeBusk et al studied this model in 585 patients (20% women) who were recruited while recovering in hospital from a recent MI [39]. Participants were randomized to either an intervention or a control group. The intervention was based on social learning theory, which consisted of goal setting for lifestyle behaviours based on the participants' motivation to change, identification of possible barriers to change and relapse prevention strategies. The intervention began with lifestyle counselling during the hospital stay. Following discharge, contact with intervention participants was restricted to telephone and mail, with a maximum of four visits with the nurse during the 12-month intervention. The intervention focused on smoking cessation, diet, exercise, and lipid-lowering therapy (limited to bile acid resins and niacin).
Exercise capacity was greater at 6 months in the intervention group than in the control (usual care, no intervention) group (9.3 and 8.4 METs, respectively). No report on exercise capacity was provided at 12 months. At the end of 12 months, smoking cessation rates (70% versus 53%, P = 0.03), total cholesterol (-0.64 mmol/l versus -0.09 mmol/l, P <0.001) and low-density lipoprotein cholesterol (-0.65 mmol/l versus -0.14 mmol/l, P <0.001) reductions were significantly greater in the intervention group than in the control group.
This novel intervention strategy demonstrates effective risk-factor management without requiring numerous patient visits. The use of telephone and mail contact greatly reduced the nurse intervention time (average 9 hours per patient), and allowed for a greater number of participants (nearly double) in the intervention than any other study.
As the study was only conducted for 1 year, it does not provide additional information on clinical outcomes. However, the 24% relative reduction of low-density lipoprotein cholesterol is similar to that observed in long-term lipid-lowering trials that demonstrated significant reductions in mortality [40]. The authors of this intervention have already reported on the benefits of its use in clinical practice [41].
Safety of CR
The use of exercise therapy for patients with CVD has proven effective, but also carries a burden of risk. Physical exertion has been reported to be a trigger of MI and sudden cardiac death in individuals both without known CVD [42,43] and with CVD [44,45,46]. Previous documentation of CVD did not appear to increase the risk of MI during exercise [44,45]. Mittleman et al reported an increased risk of 5.9 times for MI during physical exertion in 1228 men and women. When stratified by activity levels, this risk was reduced to 2.4 for individuals who were 'active' more than five times per week, and increased to a remarkable 107 for sedentary individuals [44]. Other studies have similarly reported a reduced risk of MI during exercise in the habitually active compared with sedentary individuals [43,45]. The issue of complications during CR has been reported in several studies [36,47,48,49]. These studies report complication rates from 1.23 to 2.88 and fatalities from 0.13 to 0.86 per 100,000 patient-hours. There is a trend towards less frequent events reported in the more recent studies, suggesting that current CR programs may be safer than the earlier ones. Electrocardiographic telemetry is widely used in CR programs as a safety precaution; however, its use has not been demonstrated to be superior to traditional CR supervision [47,48].
CR for congestive heart failure
Coincident with the increased number of survivors of CVD is the increase in individuals suffering from congestive heart failure (CHF). It is predicted that CHF will become the cardiovascular epidemic of the future [1]. Two randomized studies have demonstrated the benefits of exercise therapy [50,51].
In one study, 73 men were randomized to an intervention of daily-prescribed home exercise or to control (usual care, no intervention) [50]. After 6 months, the intervention group had significant improvement in exercise capacity, New York Heart Association functional class, maximal ventilation, mean total peripheral resistance, and stroke volume. Left ventricular ejection fraction (LVEF) improved from 30 ± 8% at baseline to 35 ± 9% at 6 months.
The second study randomized 99 men and women with CHF to a supervised intervention of twice-weekly exercise sessions or to control (usual care, no intervention) for 14 months [51]. Exercise capacity increased from baseline to 14 months to a greater extent in the intervention group (15.7 ± 2 ml/kg/min to 19.9 ± 1 ml/kg/min) compared with the control group (15.2 ± 2 ml/kg/min to 16 ± 2 ml/kg/min, P <0.001). Much of the increase in exercise capacity in the intervention group occurred during the initial 2 months. Quality of life also increased significantly in the intervention group as measured by the Minnesota Living with Heart Failure Questionnaire. However, no changes were reported in the control group. In contrast to the previous study, LVEF did not change significantly in the intervention group. Despite this, a significant difference in combined cardiac events (17 versus 37, P = 0.006), CHF readmission (5 versus 14, P = 0.02), and cardiac mortality (9 versus 20, P = 0.01) was observed between groups at 14 months. These studies provide definite support for the inclusion of CHF patients in CR programs.
Efficacy in other populations
The majority of CR studies to date have been restricted to middle-aged men who suffered a recent MI, yet patients enrolled in CR programs comprise a much broader population. Only recently have these populations been included in CR studies and, as a result, outcome data is limited.
Several of the more recent studies have included women, but these numbers have been too small to separately determine morbidity and mortality rates. Women have traditionally had lower rates of CVD than men but it is anticipated that this discrepancy will decrease in the future [2]. The limited number of CR studies investigating women has found significant risk-factor modification, similar to that observed in men [52,53].
Individuals older than 65 years are also often excluded from studies. When compared with younger adults, elderly individuals demonstrate similar benefits to CVD risk-factors, and exercise capacity [53,54,55].
A growing population of CR participants has undergone a prior revascularization procedure without experiencing a previous MI. Evidence suggests that patients who have undergone PTCA have different perceptions of their own health and their need for risk-factor reduction [56,57]. However, these patients can benefit from CR participation [58]. Patients who have undergone previous coronary artery bypass graft can also effectively reduce their risk-factors as a result of CR [59].
Other groups that participate in CR programs include those with post-heart transplantation, or those with atrial fibrillation and valve disorders. One randomized trial has been conducted investigating the benefits of exercise therapy following heart transplantation. Twenty-seven men and women were assigned to either a 6-month supervised exercise intervention or to control (usual care, no intervention) which included written instructions for exercise [60]. Both groups showed improved exercise capacity, but the intervention group improved to a greater extent than the control group (from 9.2 ml/kg/min to 13.6 ml/kg/min versus from 10.4 ml/kg/min to 12.3 ml/kg/min, respectively; P = 0.01).
Much less information has been reported on patients with atrial fibrillation and valve disorders. Those studies that do exist suggest these populations can benefit from participation in CR [61,62].
Challenges of CR
Despite the numerous benefits of CR, several challenges exist that are common to most programs. These challenges include low participation rates, gender-biased referral and participation, problems with adherence/drop-outs, and resource management (Fig. 2). Participation rates in CR programs by those patients who are eligible are disappointing, ranging from 8.7% to nearly 50% [63,64,65,66]. Possible reasons for low participation include lack of referral, distance to CR facility (current CR programs are commonly restricted to urban centers), lack of motivation, and patient's unwillingness to attend.
Figure 2.
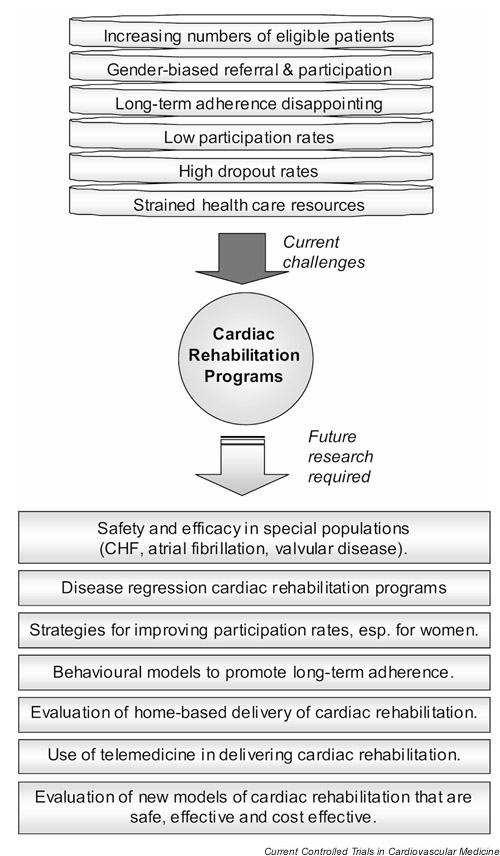
Current challenges faced by today's cardiac rehabilitation programs and recommended future directions of study. CHF, Congestive heart failure.
Demographic predictors of attendance were younger age, male gender, employment, and education. Women who do attend CR programs have been found to present at a higher CVD risk than men [67]. This is consistent with reported gender discrepancies for other CVD interventions [68]. It is possible that referral rates are lower for women than men; however, it has also been reported that women are more likely to drop out of a CR program once referred [69].
The benefits of CVD risk reduction are only realized through long-term lifestyle, and risk-factor management. CR drop-outs and adherence continue to pose a challenge to the success of CR. In many of the studies described, drop-outs were directly related to the intervention. These drop-out rates tend to be higher than those reported in controlled pharmacological intervention trials [70]. A number of articles have described the problem of CR drop-outs [71,72,73]. Even after CR participation, adherence rates to favorable lifestyle behaviors have been reported to decline [74,75]. However, good comprehensive data on adherence following completion of CR and its influence on risk-factor modification have not been reported.
To this end, the present authors have completed a pilot study of CR graduates. Six months following CR, adherence to exercise and diet remained high, and the risk-factor benefits of the CR program persisted [76]. Similar results were observed 6 months after completing CR in a study of 15 individuals [77].
Only one other study has reported CVD risk-factor trends following completion of CR. Willich et al described risk-factor changes 12 months following CR [78]. In the 2441 patients followed, risk-factors significantly improved as a result of the CR program, but these changes were later attenuated at 12 months.
Longer studies are currently in progress. As a follow-up to our pilot study, the authors are currently following 302 CR graduates in the Extensive Lifestyle Management Intervention Trial. Participants have been randomized to a modest intervention or control, and have been followed for 4 years. The results of this study will provide comprehensive lifestyle and risk-factor trends following CR, and the effect of a follow-up intervention on these factors.
Coincident with the challenge of adherence is that of resource management in light of the predicted increase in eligible participants. As the eligible population for CR services grows, CR programs will need to treat more patients without similar increases in health care resources. The MultiFit study demonstrated that significant risk-factor modification could occur with limited contact between patient and health care provider [39]. Whether these benefits can persist beyond 1 year is unknown.
Future directions of CR
As CR has evolved in the past 30 years, it has proven its value in the treatment of patients following MI. In the coming years, the challenges will be no less demanding (Fig. 2). As new target patient populations are recruited into CR programs, the safety and efficacy of CR in these populations needs to be established, particularly in those with CHF, atrial fibrillation, and valvular disease. Strategies for improving participation rates need to be developed, focusing on education of patients and health care providers. Extra efforts should be directed towards reducing the gender inequity. The possibility of disease regression needs to be explored in larger populations using clinically relevant practices.
Our program is currently evaluating atherosclerotic regression through aggressive lifestyle and risk-factor management in a group of 150 men and women over a 2-year period using carotid artery intima–media thickness as an outcome.
New models of CR need to be developed and studied for both safety and efficacy – preferably in randomized trials compared with standard CR programs. These new CR programs will need to address issues of promoting long-term adherence, improving accessibility, particularly for patients in suburban and rural communities, and addressing the growing need for CR in an ageing population. Future CR programs will also need to be resource sparing, as current health care organizations cannot meet the demand of all eligible patients. These new models will need to maximize delivery of resources to those who require them. For those patients living in rural areas, new communication technologies may prove useful in delivering CR through telemedicine initiatives. Appropriate risk stratification will aid in health care resource management, restricting outpatient CR programs to those patients at high risk and utilizing less frequent contact for low and moderate risk patients. Greater reliance on existing community resources will be required, allowing low and moderate risk patients to exercise at community centers or at home while remaining in contact with the outpatient CR center. Integration with patients' family physicians and other health care providers, such as the pharmacist, is a potential strategy to improve adherence, as are behavior strategies aimed at patient empowerment. Other forms of contact than the traditional face-to-face session can be incorporated into CR as a method of continued follow-up and reaching those patients in nonurban areas. The growth of telemedicine can play a vital role; from the simple use of the telephone, to the Internet, to the use of personal digital assistants. Integration of these and other tools can address a number of the issues of CR (Fig. 3).
Figure 3.
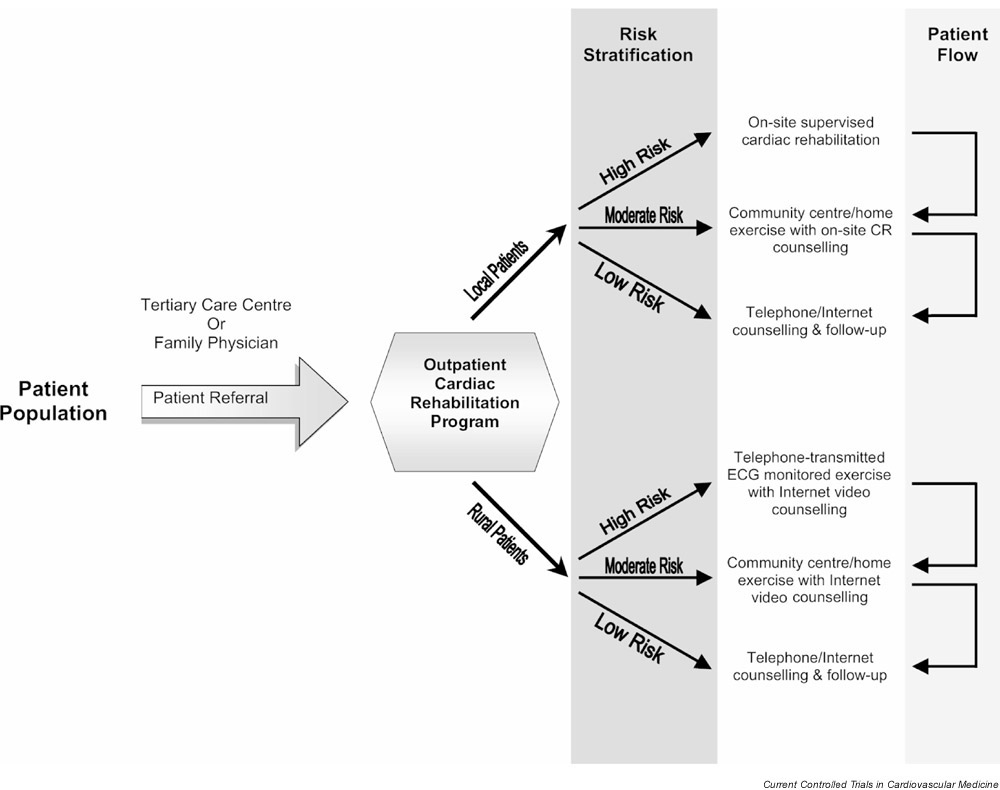
Proposed organizational structure for new cardiac rehabilitation (CR) models. ECG, Electrocardiography.
Conclusion
The numerous studies investigating exercise therapy and CR have each demonstrated some beneficial effect, whether it is an improved CVD risk-factor profile, slower disease progression, reduced morbidity, or mortality. Owing to the multifactorial nature of CVD and the design of these studies, it is difficult to extrapolate any one study to the CVD population at large. Some studies have also used interventions that have limited relevance to day-to-day clinical practice. Aggressive lifestyle/CVD risk-factor management and multiyear interventions are not practical for most health care settings. Limitations of current CR research include the lack of large randomized trials and inconsistent interventions (duration and methodology) that have not been previously validated. This is due in part to the heterogeneity of the CVD population, the numerous resources required to effectively conduct a CR intervention, and the difficulty with blinding participants and investigators.
In spite of some limitations, the accumulative evidence strongly supports the use of exercise therapy and CR for the treatment of men and women with ischemic heart disease. Through effective lifestyle and CVD risk-factor management, CR has been demonstrated to lead to slow disease progression, and even regression in some individuals, resulting in a decrease in cardiovascular morbidity, and mortality. Despite several studies restricting the use of lipid-lowering medications (demonstrating the efficacy of the lifestyle interventions), it is important for the CR health care professional to make use of all treatment tools at their disposal. Comprehensive CR programs should integrate lifestyle and pharmacological treatment as appropriate. A limited number of studies have shown CR to be beneficial in other cardiovascular populations, and it is recommended that these individuals be included in CR programs. Future research should be directed at characterizing the full benefits in other populations as well as investigating new models of CR delivery to meet the anticipated increase in eligible participants.
Competing interests
None declared.
Abbreviations
CHF = congestive heart failure; CR = cardiac rehabilitation; CVD = cardiovascular disease; LVEF = left ventricular ejection fraction; MET = metabolic equivalents; MI = myocardial infarction; PTCA = percutaneous transluminal coronary angioplasty. LHT = The Lifestyle Heart Trial; SCRIP = The Stanford Coronary Risk Intervention Project.
Acknowledgments
Acknowledgements
Scott Lear is supported by the Heart and Stroke Foundation of Canada/Medical Research Council of Canada Partnership Challenge Fund. The authors gratefully acknowledge Francois Bowden, Ph.D., for editorial support in preparation of this manuscript.
References
- American Heart Association 2001 Heart and Stroke Statistical Update Dallas, TX: American Heart Association; 2000.
- Heart and Stroke Foundation of Canada The changing face of heart disease and stroke in Canada 2000. 1999.
- Klein RF, Dean A, Willson LM, Bogdonoff MD. The physician and postmyocardial infarction invalidism. JAMA. 1965;194:143–148. [PubMed] [Google Scholar]
- Ignaszewski A, Lear SA. Cardiac rehabilitation programs. Can J Cardiol. 1999;15(suppl G):110G–113G. [PubMed] [Google Scholar]
- American Association of Cardiovascular and Pulmonary Rehabilitation Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs Champaign, IL: Human Kinetics Publishers; 1999.
- Canadian Association of Cardiac Rehabilitation Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention Winnipeg, Man: Canadian Association of Cardiac Rehabilitation; 1999.
- World Health Organization Rehabilitation of patients with cardiovascular disease: Report of a WHO expert committee WHO Technical Report Series No 270; 1964. [PubMed]
- Brousseau ME, Schaefer EJ. Diet and coronary heart disease: clinical trials. Curr Atheroscler Rep. 2000;2:487–493. doi: 10.1007/s11883-000-0048-6. [DOI] [PubMed] [Google Scholar]
- Wilson K, Gibson N, Willan A, Cook D. Effect of smoking cessation on mortality after myocardial infarction: meta-analysis of cohort studies. Arch Intern Med. 2000;160:939–944. doi: 10.1001/archinte.160.7.939. [DOI] [PubMed] [Google Scholar]
- Paffenbarger RS, Jr, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- Morris JN, Everitt MG, Pollard R, Chave SP, Semmence AM. Vigorous exercise in leisure-time: protection against coronary heart disease. Lancet. 1980;2:1207–1210. doi: 10.1016/s0140-6736(80)92476-9. [DOI] [PubMed] [Google Scholar]
- Sherman SE, D'Agostino RB, Cobb JL, Kannel WB. Physical activity and mortality in women in the Framingham Heart Study. Am Heart J. 1994;128:879–884. doi: 10.1016/0002-8703(94)90583-5. [DOI] [PubMed] [Google Scholar]
- Wilhelmsen L, Sanne H, Elmfeldt D, Grimby G, Tibblin G, Wedel H. A controlled trial of physical training after myocardial infarction. Effects on risk factors, nonfatal reinfarction, and death. Prev Med. 1975;4:491–508. doi: 10.1016/0091-7435(75)90035-3. [DOI] [PubMed] [Google Scholar]
- Shaw LW. Effects of a prescribed supervised exercise program on mortality and cardiovascular morbidity in patients after myocardial infarction. The National Exercise and Heart Disease Project. Am J Cardiol. 1981;48:39–46. doi: 10.1016/0002-9149(81)90570-1. [DOI] [PubMed] [Google Scholar]
- Carson P, Phillips R, Lloyd M, Tucker H, Neophytou M, Buch NJ, Gelson A, Lawton A, Simpson T. Exercise after myocardial infarction: a controlled trial. J R Coll Phys Lond. 1982;16:147–151. [PMC free article] [PubMed] [Google Scholar]
- Roman O, Gutierrez M, Luksic I, Chavez E, Camuzzi AL, Villalon E, Klenner C, Cumsille F. Cardiac rehabilitation after acute myocardial infarction. 9-year controlled follow-up study. Cardiology. 1983;70:223–231. doi: 10.1159/000173598. [DOI] [PubMed] [Google Scholar]
- Marra S, Paolillo V, Spadaccini F, Angelino PF. Long-term follow-up after a controlled randomized post-myocardial infarction rehabilitation programme: effects on morbidity and mortality. Eur Heart J. 1985;6:656–663. doi: 10.1093/oxfordjournals.eurheartj.a061917. [DOI] [PubMed] [Google Scholar]
- Kallio V, Hamalainen H, Hakkila J, Luurila OJ. Reduction in sudden deaths by a multifactorial intervention programme after acute myocardial infarction. Lancet. 1979;2:1091–1094. doi: 10.1016/s0140-6736(79)92502-9. [DOI] [PubMed] [Google Scholar]
- Hamalainen H, Luurila OJ, Kallio V, Knuts LR, Arstila M, Hakkila J. Long-term reduction in sudden deaths after a multifactorial intervention programme in patients with myocardial infarction: 10-year results of a controlled investigation. Eur Heart J. 1989;10:55–62. doi: 10.1093/oxfordjournals.eurheartj.a059381. [DOI] [PubMed] [Google Scholar]
- Anonymous Comparison of a rehabilitation programme, a counselling programme and usual care after an acute myocardial infarction: results of a long-term randomized trial. PRECOR Group. Eur Heart J. 1991;12:612–616. doi: 10.1093/oxfordjournals.eurheartj.a059948. [DOI] [PubMed] [Google Scholar]
- Hedback B, Perk J, Wodlin P. Long-term reduction of cardiac mortality after myocardial infarction: 10-year results of a comprehensive rehabilitation programme. Eur Heart J. 1993;14:831–835. doi: 10.1093/eurheartj/14.6.831. [DOI] [PubMed] [Google Scholar]
- Oldridge NB, Guyatt GH, Fischer ME, Rimm AA. Cardiac rehabilitation after myocardial infarction. Combined experience of randomized clinical trials. JAMA. 1988;260:945–950. [PubMed] [Google Scholar]
- O'Connor GT, Buring JE, Yusuf S, Goldhaber SZ, Olmstead EM, Paffenbarger RS, Hennekens CH. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation. 1989;80:234–244. doi: 10.1161/01.cir.80.2.234. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- Hamalainen H, Luurila OJ, Kallio V, Knuts LR. Reduction in sudden deaths and coronary mortality in myocardial infarction patients after rehabilitation. 15 year follow-up study. Eur Heart J. 1995;16:1839–1844. doi: 10.1093/oxfordjournals.eurheartj.a060837. [DOI] [PubMed] [Google Scholar]
- Dorn J, Naughton J, Imamura D, Trevisan M. Results of a multicenter randomized clinical trial of exercise and long-term survival in myocardial infarction patients: the National Exercise and Heart Disease Project (NEHDP). Circulation. 1999;100:1764–1769. doi: 10.1161/01.cir.100.17.1764. [DOI] [PubMed] [Google Scholar]
- Hedback B, Perk J. 5-year results of a comprehensive rehabilitation programme after myocardial infarction. Eur Heart J. 1987;8:234–242. doi: 10.1093/oxfordjournals.eurheartj.a062265. [DOI] [PubMed] [Google Scholar]
- Pitt B, Mancini GB, Ellis SG, Rosman HS, Park JS, McGovern ME. Pravastatin limitation of atherosclerosis in the coronary arteries (PLAC I): reduction in atherosclerosis progression and clinical events. PLAC I investigation. J Am Coll Cardiol. 1995;26:1133–1139. doi: 10.1016/0735-1097(95)00301-0. [DOI] [PubMed] [Google Scholar]
- Schuler G, Hambrecht R, Schlierf G, Grunze M, Methfessel S, Hauer K, Kubler W. Myocardial perfusion and regression of coronary artery disease in patients on a regimen of intensive physical exercise and low fat diet. J Am Coll Cardiol. 1992;19:34–42. doi: 10.1016/0735-1097(92)90048-r. [DOI] [PubMed] [Google Scholar]
- Niebauer J, Hambrecht R, Schlierf G, Marburger C, Kalberer B, Kubler W, Schuler G. Five years of physical exercise and low fat diet: effects on progression of coronary artery disease. J Cardiopulm Rehab. 1994;15:47–64. doi: 10.1097/00008483-199501000-00007. [DOI] [PubMed] [Google Scholar]
- Schuler G, Hambrecht R, Schlierf G, Niebauer J, Hauer K, Neumann J, Hoberg E, Drinkmann A, Bacher F, Grunze M, Kubler W. Regular physical exercise and low-fat diet. Effects on progression of coronary artery disease. Circulation. 1992;86:1–11. doi: 10.1161/01.cir.86.1.1. [DOI] [PubMed] [Google Scholar]
- Niebauer J, Hambrecht R, Marburger C, Hauer K, Velich T, von Hodenberg E, Schlierf G, Kubler W, Schuler G. Impact of intensive physical exercise and low-fat diet on collateral vessel formation in stable angina pectoris and angiographically confirmed coronary artery disease. Am J Cardiol. 1995;76:771–775. doi: 10.1016/s0002-9149(99)80224-0. [DOI] [PubMed] [Google Scholar]
- Niebauer J, Hambrecht R, Velich T, Hauer K, Marburger C, Kalberer B, Weiss C, von Hodenberg E, Schlierf G, Schuler G, Zimmermann R, Kubler W. Attenuated progression of coronary artery disease after 6 years of multifactorial risk intervention: role of physical exercise. Circulation. 1997;96:2534–2541. doi: 10.1161/01.cir.96.8.2534. [DOI] [PubMed] [Google Scholar]
- Ornish D, Brown SE, Scherwitz LW, Billings JH, Armstrong WT, Ports TA, McLanahan SM, Kirkeeide RL, Brand RJ, Gould KL. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336:129–133. doi: 10.1016/0140-6736(90)91656-u. [DOI] [PubMed] [Google Scholar]
- Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280:2001–2007. doi: 10.1001/jama.280.23.2001. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Alderman EL, Fair JM, Maron DJ, Mackey SF, Superko HR, Williams PT, Johnstone IM, Champagne MA, Krauss RM, Farquhar JW. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP). Circulation. 1994;89:975–990. doi: 10.1161/01.cir.89.3.975. [DOI] [PubMed] [Google Scholar]
- Teo KK, Burton JR, Buller CE, Plante S, Catellier D, Tymchak W, Dzavik V, Taylor D, Yokoyama S, Montague TJ. Long-term effects of cholesterol lowering and angiotensin-converting enzyme inhibition on coronary atherosclerosis: The Simvastatin/ Enalapril Coronary Atherosclerosis Trial (SCAT). Circulation. 2000;102:1748–1754. doi: 10.1161/01.cir.102.15.1748. [DOI] [PubMed] [Google Scholar]
- Bestehorn HP, Rensing UF, Roskamm H, Betz P, Benesch L, Schemeitat K, Blumchen G, Claus J, Mathes P, Kappenberger L, Wieland H, Neiss A. The effect of simvastatin on progression of coronary artery disease. The Multicenter coronary Intervention Study (CIS). Eur Heart J. 1997;18:226–234. doi: 10.1093/oxfordjournals.eurheartj.a015224. [DOI] [PubMed] [Google Scholar]
- DeBusk RF, Miller NH, Superko HR, Dennis CA, Thomas RJ, Lew HT, Berger WE, Heller RS, Rompf J, Gee D, Kraemer HC, Bandura A, Ghandour G, Clark M, Shah RV, Fisher L, Taylor CB. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–729. doi: 10.7326/0003-4819-120-9-199405010-00001. [DOI] [PubMed] [Google Scholar]
- Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- Miller NH, Warren D, Myers D. Home-based cardiac rehabilitation and lifestyle modification: the MULTIFIT model. J Cardiovasc Nurs. 1996;11:76–87. doi: 10.1097/00005082-199610000-00009. [DOI] [PubMed] [Google Scholar]
- Thompson PD, Funk EJ, Carleton RA, Sturner WQ. Incidence of death during jogging in Rhode Island from 1975 through 1980. JAMA. 1982;247:2535–2538. [PubMed] [Google Scholar]
- Siscovick DS, Weiss NS, Fletcher RH, Lasky T. The incidence of primary cardiac arrest during vigorous exercise. N Engl J Med. 1984;311:874–877. doi: 10.1056/NEJM198410043111402. [DOI] [PubMed] [Google Scholar]
- Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329:1677–1683. doi: 10.1056/NEJM199312023292301. [DOI] [PubMed] [Google Scholar]
- Willich SN, Lewis M, Lowel H, Arntz HR, Schubert F, Schroder R. Physical exertion as a trigger of acute myocardial infarction. Triggers and Mechanisms of Myocardial Infarction Study Group. N Engl J Med. 1993;329:1684–1690. doi: 10.1056/NEJM199312023292302. [DOI] [PubMed] [Google Scholar]
- Burke AP, Farb A, Malcom GT, Liang Y, Smialek JE, Virmani R. Plaque rupture and sudden death related to exertion in men with coronary artery disease. JAMA. 1999;281:921–926. doi: 10.1001/jama.281.10.921. [DOI] [PubMed] [Google Scholar]
- Van Camp SP, Peterson RA. Cardiovascular complications of outpatient cardiac rehabilitation programs. JAMA. 1986;256:1160–1163. doi: 10.1001/jama.256.9.1160. [DOI] [PubMed] [Google Scholar]
- Vongvanich P, Paul-Labrador MJ, Merz CN. Safety of medically supervised exercise in a cardiac rehabilitation center. Am J Cardiol. 1996;77:1383–1385. doi: 10.1016/s0002-9149(96)00215-9. [DOI] [PubMed] [Google Scholar]
- Franklin BA, Bonzheim K, Gordon S, Timmis GC. Safety of medically supervised outpatient cardiac rehabilitation exercise therapy: a 16-year follow-up. Chest. 1998;114:902–906. doi: 10.1378/chest.114.3.902. [DOI] [PubMed] [Google Scholar]
- Hambrecht R, Gielen S, Linke A, Fiehn E, Yu J, Walther C, Schoene N, Schuler G. Effects of exercise training on left ventricular function and peripheral resistance in patients with chronic heart failure: A randomized trial. JAMA. 2000;283:3095–3101. doi: 10.1001/jama.283.23.3095. [DOI] [PubMed] [Google Scholar]
- Belardinelli R, Georgiou D, Cianci G, Purcaro A. Randomized, controlled trial of long-term moderate exercise training in chronic heart failure: effects on functional capacity, quality of life, and clinical outcome. Circulation. 1999;99:1173–1182. doi: 10.1161/01.cir.99.9.1173. [DOI] [PubMed] [Google Scholar]
- Warner JG, Brubaker PH, Zhu Y, Morgan TM, Ribisl PM, Miller HS, Herrington DM. Long-term (5-year) changes in HDL cholesterol in cardiac rehabilitation patients. Do sex differences exist? Circulation. 1995;92:773–777. doi: 10.1161/01.cir.92.4.773. [DOI] [PubMed] [Google Scholar]
- Balady GJ, Jette D, Scheer J, Downing J. Changes in exercise capacity following cardiac rehabilitation in patients stratified according to age and gender. Results of the Massachusetts Association of Cardiovascular and Pulmonary Rehabilitation Multicenter Database. J Cardiopulm Rehab. 1996;16:38–46. doi: 10.1097/00008483-199601000-00005. [DOI] [PubMed] [Google Scholar]
- Ades PA, Waldmann ML, Gillespie C. A controlled trial of exercise training in older coronary patients. J Gerontol A Biol Sci Med Sci. 1995;50A:M7–M11. doi: 10.1093/gerona/50a.1.m7. [DOI] [PubMed] [Google Scholar]
- Lavie CJ, Milani RV. Effects of cardiac rehabilitation programs on exercise capacity, coronary risk factors, behavioral characteristics, and quality of life in a large elderly cohort. Am J Cardiol. 1995;76:177–179. doi: 10.1016/s0002-9149(99)80054-x. [DOI] [PubMed] [Google Scholar]
- Gaw-Ens B, Laing GP. Risk factor reduction behaviours in coronary angioplasty and myocardial infarction patients. Can J Cardiovasc Nurs. 1994;5:4–12. [PubMed] [Google Scholar]
- Bunker S, McBurney H, Cox H, Jelinek M. Identifying participation rates at outpatient cardiac rehabilitation programs in Victoria, Australia. J Cardiopulm Rehab. 1999;19:334–338. doi: 10.1097/00008483-199911000-00001. [DOI] [PubMed] [Google Scholar]
- Wallner S, Watzinger N, Lindschinger M, Smolle KH, Toplak H, Eber B, Dittrich P, Elmadfa I, Klein W, Krejs GJ, Wascher TC. Effects of intensified lifestyle modification on the need for further revascularization after coronary angioplasty. Eur J Clin Invest. 1999;29:372–379. doi: 10.1046/j.1365-2362.1999.00456.x. [DOI] [PubMed] [Google Scholar]
- Engblom E, Korpilahti K, Hamalainen H, Puukka P, Ronnemaa T. Effects of five years of cardiac rehabilitation after coronary artery bypass grafting on coronary risk factors. Am J Cardiol. 1996;78:1428–1431. doi: 10.1016/s0002-9149(96)00629-7. [DOI] [PubMed] [Google Scholar]
- Kobashigawa JA, Leaf DA, Lee N, Gleeson MP, Liu H, Hamilton MA, Moriguchi JD, Kawata N, Einhorn K, Herlihy E, Laks H. A controlled trial of exercise rehabilitation after heart transplantation. N Engl J Med. 1999;340:272–277. doi: 10.1056/NEJM199901283400404. [DOI] [PubMed] [Google Scholar]
- Vanhees L, Schepers D, Defoor J, Brusselle S, Tchursh N, Fagard R. Exercise performance and training in cardiac patients with atrial fibrillation. J Cardiopulm Rehab. 2000;20:346–352. doi: 10.1097/00008483-200011000-00003. [DOI] [PubMed] [Google Scholar]
- Douard H, Chevalier L, Labbe L, Choussat A, Broustet JP. Physical training improves exercise capacity in patients with mitral stenosis after balloon valvuloplasty. Eur Heart J. 1997;18:464–469. doi: 10.1093/oxfordjournals.eurheartj.a015267. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Rosamond WD, Luepker RV. Predictors of outpa-tient cardiac rehabilitation utilization: the Minnesota Heart Surgery Registry. J Cardiopulm Rehab. 1998;18:192–198. doi: 10.1097/00008483-199805000-00002. [DOI] [PubMed] [Google Scholar]
- Bittner V, Sanderson B, Breland J, Green D. Referral patterns to a University-based cardiac rehabilitation program. Am J Cardiol. 1999;83:252–255. doi: 10.1016/s0002-9149(98)00830-3. [DOI] [PubMed] [Google Scholar]
- King KM, Humen DP, Teo KK. Cardiac rehabilitation: the forgotten intervention. Can J Cardiol. 1999;15:979–985. [PubMed] [Google Scholar]
- Blackburn GG, Foody JM, Sprecher DL, Park E, Apperson-Hansen C, Pashkow FJ. Cardiac rehabilitation participation patterns in a large, tertiary care center: evidence for selection bias. J Cardiopulm Rehab. 2000;20:189–195. doi: 10.1097/00008483-200005000-00007. [DOI] [PubMed] [Google Scholar]
- Thomas RJ, Miller NH, Lamendola C, Berra K, Hedback B, Durs-tine JL, Haskell W. National Survey on Gender Differences in Cardiac Rehabilitation Programs. Patient characteristics and enrollment patterns. J Cardiopulm Rehab. 1996;16:402–412. doi: 10.1097/00008483-199611000-00010. [DOI] [PubMed] [Google Scholar]
- Lauer MS, Pashkow FJ, Snader CE, Harvey SA, Thomas JD, Marwick TH. Sex and diagnostic evaluation of possible coronary artery disease after exercise treadmill testing at one academic teaching center. Am Heart J. 1997;134:807–813. doi: 10.1016/s0002-8703(97)80003-8. [DOI] [PubMed] [Google Scholar]
- Halm M, Penque S, Doll N, Beahrs M. Women and cardiac rehabilitation: referral and compliance patterns. J Cardiovasc Nurs. 1999;13:83–92. doi: 10.1097/00005082-199904000-00008. [DOI] [PubMed] [Google Scholar]
- Anonymous Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;4:1383–1389. [PubMed] [Google Scholar]
- King KM, Teo KK. Cardiac rehabilitation referral and attendance: not one and the same. Rehab Nurs. 1998;23:246–251. doi: 10.1002/j.2048-7940.1998.tb01794.x. [DOI] [PubMed] [Google Scholar]
- Mullinax CH. Cardiac rehabilitation programs and the problem of patient dropout. Rehab Nurs. 1995;20:90–92. doi: 10.1002/j.2048-7940.1995.tb01602.x. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Fleury J. Barriers to outpatient cardiac rehabilitation participation and adherence. J Cardiopulm Rehab. 2000;20:241–246. doi: 10.1097/00008483-200007000-00005. [DOI] [PubMed] [Google Scholar]
- Suter PM, Suter WN, Perkins MK, Bona SL, Kendrick PA. Cardiac rehabilitation survey: maintenance of lifestyle changes and perception of program value. Rehab Nurs. 1996;21:192–195. doi: 10.1002/j.2048-7940.1996.tb01704.x. [DOI] [PubMed] [Google Scholar]
- Moore SM, Ruland CM, Pashkow FJ, Blackburn GG. Women's patterns of exercise following cardiac rehabilitation. Nurs Res. 1998;47:318–324. doi: 10.1097/00006199-199811000-00005. [DOI] [PubMed] [Google Scholar]
- Lear S, Ignaszewski A, Laquer E, Pritchard P, Frohlich J. Extensive Lifestyle Management Intervention Following Cardiac Rehabilitation: Pilot Study. Rehab Nurs. [DOI] [PubMed]
- Brubaker PH, Rejeski WJ, Smith MJ, Sevensky KH, Lamb KA, Sotile WM, Miller HS. A home-based maintenance exercise program after center-based cardiac rehabilitation: effects on blood lipids, body composition, and functional capacity. J Cardiopulm Rehal. 2000;20:50–56. doi: 10.1097/00008483-200001000-00009. [DOI] [PubMed] [Google Scholar]
- Willich SN, Muller-Nordhorn J, Kulig M, Binting S, Gohlke H, Hahmann H, Bestehorn K, Krobot K, Voller H. Cardiac risk factors, medication, and recurrent clinical events after acute coronary disease; a prospective cohort study. Eur Heart J. 2001;22:307–313. doi: 10.1053/euhj.2000.2294. [DOI] [PubMed] [Google Scholar]
- Engblom E, Hietanen EK, Hamalainen H, Kallio V, Inberg M, Knuts LR. Exercise habits and physical performance during comprehensive rehabilitation after coronary artery bypass surgery. Eur Heart J. 1992;13:1053–1059. doi: 10.1093/oxfordjournals.eurheartj.a060313. [DOI] [PubMed] [Google Scholar]
- Dylewicz P, Bienkowska S, Szczesniak L, Rychlewski T, Przy-warska I, Wilk M, Jastrzebski A. Beneficial effect of short-term endurance training on glucose metabolism during rehabilitation after coronary bypass surgery. Chest. 2000;117:47–51. doi: 10.1378/chest.117.1.47. [DOI] [PubMed] [Google Scholar]
- Froelicher V, Jensen D, Genter F, Sullivan M, McKirnan MD, Witztum K, Scharf J, Strong ML, Ashburn W. A randomized trial of exercise training in patients with coronary heart disease. JAMA. 1984;252:1291–1297. [PubMed] [Google Scholar]
- Miller NH, Haskell WL, Berra K, DeBusk RF. Home versus group exercise training for increasing functional capacity after myocardial infarction. Circulation. 1984;70:645–649. doi: 10.1161/01.cir.70.4.645. [DOI] [PubMed] [Google Scholar]
- Hambrecht R, Niebauer J, Marburger C, Grunze M, Kalberer B, Hauer K, Schlierf G, Kubler W, Schuler G. Various intensities of leisure time physical activity in patients with coronary artery disease: effects on cardiorespiratory fitness and progression of coronary atherosclerotic lesions. J Am Coll Cardiol. 1993;22:468–477. doi: 10.1016/0735-1097(93)90051-2. [DOI] [PubMed] [Google Scholar]
- Gulanick M. Is phase 2 cardiac rehabilitation necessary for early recovery of patients with cardiac disease? A randomized, controlled study. Heart Lung. 1991;20:9–15. [PubMed] [Google Scholar]
- Oldridge N, Guyatt G, Jones N, Crowe J, Singer J, Feeny D, McK-elvie R, Runions J, Streiner D, Torrance G. Effects on quality of life with comprehensive rehabilitation after acute myocardial infarction. Am J Cardiol. 1991;67:1084–1089. doi: 10.1016/0002-9149(91)90870-q. [DOI] [PubMed] [Google Scholar]
- Bar F, Hoppener P, Diederiks J. Cardiac rehabilitation contributes to the restoration of leisure and social activities after myocardial infarction. J Cardiopulm Rehab. 1992;12:117–125. [Google Scholar]