Summary
Background
Reliable information on the incidence of induced abortion in India is lacking. Official statistics and national surveys provide incomplete coverage. Since the early 2000s, medication abortion has become increasingly available, improving the way women obtain abortions. The aim of this study was to estimate the national incidence of abortion and unintended pregnancy for 2015.
Methods
National abortion incidence was estimated through three separate components: abortions (medication and surgical) in facilities (including private sector, public sector, and non-governmental organisations [NGOs]); medication abortions outside facilities; and abortions outside of facilities and with methods other than medication abortion. Facility-based abortions were estimated from the 2015 Health Facilities Survey of 4001 public and private health facilities in six Indian states (Assam, Bihar, Gujarat, Madhya Pradesh, Tamil Nadu, and Uttar Pradesh) and from NGO clinic data. National medication abortion drug sales and distribution data were obtained from IMS Health and six principal NGOs (DKT International, Marie Stopes International, Population Services International, World Health Partners, Parivar Seva Santha, and Janani). We estimated the total number of abortions that are not medication abortions and are not obtained in a health facility setting through an indirect technique based on findings from community-based study findings in two states in 2009, with adjustments to account for the rapid increase in use of medication abortion since 2009. The total number of women of reproductive age and livebirth data were obtained from UN population data, and the proportion of births from unplanned pregnancies and data on contraceptive use and need were obtained from the 2015–16 National Family Health Survey-4.
Findings
We estimate that 15·6 million abortions (14·1 million–17·3 million) occurred in India in 2015. The abortion rate was 47·0 abortions (42·2–52·1) per 1000 women aged 15–49 years. 3·4 million abortions (22%) were obtained in health facilities, 11·5 million (73%) abortions were medication abortions done outside of health facilities, and 0·8 million (5%) abortions were done outside of health facilities using methods other than medication abortion. Overall, 12·7 million (81%) abortions were medication abortions, 2·2 million (14%) abortions were surgical, and 0·8 million (5%) abortions were done through other methods that were probably unsafe. We estimated 48·1 million pregnancies, a rate of 144·7 pregnancies per 1000 women aged 15–49 years, and a rate of 70·1 unintended pregnancies per 1000 women aged 15–49 years. Abortions accounted for one third of all pregnancies, and nearly half of pregnancies were unintended.
Interpretation
Health facilities can have a greater role in abortion service provision and provide quality care, including post-abortion contraception. Interventions are needed to expand access to abortion services through better equipping existing facilities, ensuring adequate and continuous supplies of medication abortion drugs, and by increasing the number of trained providers. In view of how many women rely on self-administration of medication abortion drugs, interventions are needed to provide women with accurate information on these drugs and follow-up care when needed. Research is needed to test interventions that improve knowledge and practice in providing medication abortion, and the Indian Government at the national and state level needs to prioritise improving policies and practice to increase access to comprehensive abortion care and quality contraceptive services that prevent unintended pregnancy.
Funding
Government of UK Department for International Development (until 2015), the David and Lucile Packard Foundation, the John D. and Catherine T. MacArthur Foundation, and the Ford Foundation.
Introduction
Reliable, current information on the incidence of induced abortion in India is not available. The only two approximate national estimates1,2 that exist are now very dated. In 2010–14, the abortion incidence in the south and central Asian subregion, which includes India, was estimated to be 37 abortions per 1000 women aged 15–44 years.3 However, this study did not provide country-level measures, and its modelled estimates are affected by data from all countries in each subregion and by available country-level data. Statistics compiled by the Indian Government on the number of abortions provided in facilities are known to greatly underestimate abortion incidence because coverage of facility-based services is incomplete and in addition, many abortions occur outside of a facility setting.4 In some surveys, women in India are asked about abortion experience, but direct questions to women are known to result in very high under-reporting because of stigma.5-7 This evidence gap not only hinders the government’s ability to design policies and programmes on reproductive health but also weakens global estimates of abortion incidence.
Since the passage of the Medical Termination of Pregnancy Act in 1971, abortion has been legally available in India under a broad range of criteria, including to save a woman’s life, to protect her physical and mental health, in cases of economic and social necessity, and if contraception has failed between married couples.8 The act also requires abortion services to be provided by trained, certified doctors in registered facilities. In the case of medication abortions, a prescription is required. However, access to safe, legal abortion services has lagged, so women now commonly obtain medication abortion from pharmacists, chemists, and informal vendors, and the information they receive on how to use the drugs and on recommended gestational limits is often inaccurate or absent.9-12 Yet since the early 2000s, with the increased availability of medication abortion in India, a steady improvement in providing access to abortion has been facilitated by the passage in 2002 of an amendment to the Medical Termination of Pregnancy Act, permitting medication abortion up to 7 weeks’ gestation, and in 2003 by a further amendment, allowing certified abortion providers to prescribe medication abortion drugs outside of a registered facility as long as emergency facilities were available to them.13,14 Surgical abortion procedures continue to be provided in health facilities, and some women continue to use unsafe methods to self-induce.9
To address the evidence gap on abortion incidence in India, we provide national estimates of the incidence of abortion, pregnancy, and unintended pregnancy for India in 2015.
Methods
Data sources
The 2015 Health Facilities Survey (HFS), fielded from March to August, 2015, collected data on the number of induced abortions provided annually, by type of procedure (surgical and medication), from 4001 public and private health facilities in Assam, Bihar, Gujarat, Madhya Pradesh, Tamil Nadu, and Uttar Pradesh (appendix). These six states were selected for the survey on the basis of geographical location, population size, and key sociodemographic characteristics. The HFS represents facility-based provision of reproductive health care for about 45% of all women in India aged 15–49 years. Sampled facilities in the public sector were at or above the primary health centre level. Facilities in the private sector (registered or unregistered) had basic operating theatre capacity (ie, are equipped to provide vacuum aspiration procedures). Doctors’ consultation rooms and health posts were not included in the HFS (table 1). Respondents for the HFS were senior staff who had worked in the facility for at least 6 months and who were identified as most knowledgeable about abortion provision at their facility. Further details about the sample are provided in the appendix.
Table 1.
Universe of facilities and completed interviews in the Health Facilities Survey from six states in India, 2015
| Assam
|
Bihar
|
Gujarat
|
Madhya Pradesh
|
Tamil Nadu
|
Uttar Pradesh
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Universe | Completed interviews |
Universe | Completed interviews |
Universe | Completed interviews |
Universe | Completed interviews |
Universe | Completed interviews |
Universe | Completed interviews |
|
| Facility ownership | ||||||||||||
| Public | 1307 | 150 | 2127 | 320 | 1557 | 262 | 1897 | 383 | 2264 | 393 | 5092 | 538 |
| Private | 381 | 46 | 2919 | 337 | 2270 | 218 | 3422 | 277 | 3853 | 393 | 8695 | 684 |
| Facility type | ||||||||||||
| Public hospitals | 40 | 30 | 82 | 56 | 62 | 42 | 124 | 87 | 284 | 76 | 96 | 64 |
| Community health centres | 151 | 28 | 70 | 37 | 311 | 71 | 334 | 81 | 385 | 86 | 773 | 144 |
| Primary health centres | 1014 | 78 | 1874 | 210 | 1142 | 137 | 1152 | 186 | 1361 | 178 | 3482 | 263 |
| Other public urban facilities | 97 | 9 | 92 | 8 | 31 | 2 | 278 | 20 | 211 | 30 | 726 | 57 |
| Private hospitals | 89 | 19 | 582 | 81 | 1517 | 160 | 1556 | 130 | 2031 | 200 | 2718 | 202 |
| Private nursing or maternity homes | 171 | 19 | 926 | 104 | 539 | 39 | 1078 | 83 | 859 | 84 | 1308 | 101 |
| Private clinics | 121 | 8 | 1409 | 150 | 211 | 16 | 782 | 58 | 941 | 87 | 4652 | 369 |
| Medical colleges | 5 | 5 | 11 | 11 | 14 | 13 | 15 | 15 | 45 | 45 | 32 | 22 |
| Public | 5 | 5 | 9 | 9 | 11 | 10 | 9 | 9 | 23 | 23 | 15 | 10 |
| Private | 0 | 0 | 2 | 2 | 3 | 3 | 6 | 6 | 22 | 22 | 17 | 12 |
| Total number of facilities | 1688 | 196 | 5046 | 657 | 3827 | 480 | 5319 | 660 | 6117 | 786 | 13 787 | 1222 |
Universes for public hospitals, community health centres, and primary health centres are from comprehensive lists obtained from the Indian Government Health Management Information System. Universes for medical colleges are from lists published by the Medical Council of India. Because no comprehensive lists exist for private health facilities and certain public health facilities (see other public urban facility), the study team did a listing exercise in a random sample area in each of the six states to identify facilities of these types that at least had a minor operating theatre and provided reproductive health services. The ratio of facility to population of women aged 15–49 years (specific to each type of such facilities within four categories of town or city sizes and rural areas) was used to scale up from the number listed to estimate the total number of each category of facilities in the six states and, from these, to major regions and summed to provide a national estimate.
Data on the quantity of medication abortion drugs sold within India by the commercial (ie, for-profit) market in 2015 were obtained from IMS Health, a company that regularly surveys a national sample of 5600 stockists. These data cover the two main types of medication abortion drugs used: a combination drug regimen of mifepristone and misoprostol packaged in the correct dosage for early terminations (hereafter referred to as MA Combipacks); and mifepristone, a drug that is used only to induce abortion (sold as pills and used in combination with misoprostol). IMS Health assesses its coverage to be 95% of all for-profit drug sales.15
Additionally, we obtained data from the six principal non-profit organisations that provide medication abortion drugs: DKT International, Marie Stopes International, Population Services International, World Health Partners, Parivar Seva Santha, and Janani. The two largest non-profit organisations, DKT International and Marie Stopes International, provided data for 2015 on their MA Combipack distribution by state.
The number of livebirths in 2015 was estimated from UN population data,16 and the number of women aged 15–49 years was estimated by projections done by the International Institute for Population Sciences (Mumbai, India) using census data. The proportion of births that were from unplanned pregnancies and other contextual measures such as contraceptive use and unmet need were extracted from the 2015–16 National Family Health Survey-4 (NFHS-4).
Abortion incidence
National abortion incidence was estimated through three separate components: (1) facility-based abortions; (2) medication abortions outside of facilities; and (3) abortions outside of facilities and with methods other than medication abortion (other abortions).
For the first component, facility-based abortions, we used data collected by the HFS on the number of women who received induced abortion services (surgical and medication abortion) at that health facility during the past month or year and the typical month or year. The annual number of abortions done in each facility is estimated as the average of the past year and typical year totals (appendix). The total number of facility-based abortions for each surveyed state was estimated by applying sample weights (appendix).
Data from the six surveyed states were the basis for estimating the number of facility-based abortions provided in non-surveyed states. Scaling up findings to the national level required three assumptions. First, each surveyed state represented the non-surveyed states in its region. Second, for the private sector (clinics of all sizes, maternity and nursing homes, and hospitals) and for certain types of public sector facilities (railway hospitals, military hospitals, municipal hospitals, urban health centres, and urban family welfare centres), data were not available on the universe of such facilities. We estimated the universe of these facility types by assuming that surveyed states have the same ratio of women of reproductive age per facility as non-surveyed states (specific to each region). For the public sector, data on the universe of facilities are available for all other facility types other than those mentioned above for all states from the Ministry of Health & Family Welfare’s Health Management Information System (HMIS). Third, scaling up findings from the six states included in the HFS to other states in their respective regions required the assumption that the average caseload in surveyed states is the same as in non-surveyed states for each type of facility.
On the basis of these assumptions, the national total number of facility-based abortions was obtained by combining the total number of abortions provided in public and private sector facilities with the number of abortions provided by NGO facilities (appendix).
Several steps are required to estimate the second component of abortion incidence, medication abortions outside of health facilities. First, the total amount of MA Combipacks distributed in India in 2015 was obtained by combining the quantities provided by the for-profit and non-profit sectors. Each MA Combipack is used to induce one abortion. In addition to MA Combipacks, the quantity of mifepristone pills sold by the for-profit sector was converted to the equivalent number of abortions. Although one pill of mifepristone (200 mg) is medically indicated for one abortion, evidence suggests that some women are instructed by their providers to take more than one pill for one induced abortion.17 To account for this, we used the following assumption: 80% of women who use mifepristone pills sold separately used one pill per abortion; 10% used two pills per abortion; and 10% used three pills per abortion (Sheriar N, Hinduja Healthcare Surgical and Holy Family Hospitals, personal communication). This is equivalent to every 130 mifepristone pills accounting for 100 abortions. The total number of medication abortions is the sum of MA Combipacks and equivalent number of mifepristone-only abortions, from both the for-profit and the non-profit sectors.
The following additional adjustments were needed to estimate the number of medication abortions. First, for-profit sales were increased by 5% to account for IMS Health’s incomplete data coverage. Second, total medication abortions (for-profit and non-profit) were reduced: (1) by 10% to account for wastage on the basis of available data of drug wastage in general (data on medication abortion drug wastage are unavailable);18,19 (2) by 5% of all facility-based abortions to avoid double counting women who attempted a medication abortion outside of a facility but eventually received a successful abortion within a facility, where they are already counted in the HFS;20 and (3) by 72 000 medication abortions in states that have borders with Nepal (Puri M, Center for Research on Environment Health and Population Activities, personal communication)21 and by 21 000 medication abortions in states that have borders with Bangladesh (A Hossain, Bangladesh Association for Prevention of Septic Abortion, personal communication)22 to account for cross-border exports of medication abortion drugs to these countries.
Finally, we subtracted all relevant categories of facility-based medication abortions (those occurring in private and NGO facilities and those given as prescriptions in public sector facilities) from total medication abortion sales to obtain the number of medication abortions occurring outside health facilities. Public sector medication abortions for which women are given the medication abortion drug by the provider are not subtracted because the public sector procures its own supplies of drugs directly from manufacturers. In our estimates, medication abortions that occur outside facilities are heterogeneous and include abortions that are self-sourced directly from informal sector providers, especially chemists, and some abortions that are initiated or prescribed in private doctors’ offices or consultation rooms because this type of provider is not covered by the HFS and the number of such abortions was not quantified.
The third component of abortion incidence includes abortions outside of health facilities with methods other than medication abortion. These abortions are performed by untrained providers using unsafe methods such as insertion of sticks and roots, ingestion of herbal medicines, abdominal massage, or those performed under unhygienic conditions.23,24 Unlike the previous two components, it was not possible to obtain data on the number of other abortions. We therefore used an indirect technique based on a 2009 community-based study in two states in which the average proportion of women having these types of abortions was estimated to be 7%.9,10 However, we adjusted this estimate because the rapid increase in use of medication abortion since 2009 probably reduced women’s use of other unsafe methods. We used the increase in medication abortion drug sales in 2009–15 (almost a 30% increase) as a proxy for estimating the decrease in the proportion of women having other abortions since 2009. We estimated that by 2015, 5% of abortions could be classified as other abortions. The HFS data confirmed that a small proportion of women having abortions continue to use damaging methods. Across the six surveyed states, 4–16% of patients receiving post-abortion care (a fraction of all women having abortions) were being treated for serious complications (including infection of the uterus, injury, perforation, sepsis, and shock).
To account for uncertainty in our estimates, we did sensitivity analyses to estimate upper and lower bound ranges, which we refer to as high and low estimates, around the medium estimate. The first component (facility-based abortions) relies entirely on survey data, so confidence intervals based on the HFS provide lower and upper limits. The second component (medication abortions outside of facilities) relies on several adjustments, so upper and lower bounds were calculated for each adjustment made, depending on the certainty of the data underlying each. For example, adjustments for cross-border export of medication abortion drugs to Nepal and Bangladesh are based on large-scale HFS surveys, so we assumed a relatively low level of uncertainty for these two adjustments when calculating upper and lower bounds. Adjustments for the percentage of women who unsuccessfully use medication abortion outside a facility and then obtain an abortion in a facility is based on a small study in one state,20 so we assumed a relatively high level of uncertainty for this adjustment with a wider range for the upper and lower bound estimates. For the third component (other abortions), where the medium estimate is based on community-based studies in two states and national data on trends in the use of medication abortion, we assumed a level of uncertainty that is intermediate between these two in the sensitivity analysis. We aggregated ranges across all three components and their subcomponents to obtain upper and lower bounds around the estimated total number of abortions (referred to as the medium estimate; appendix).
Incidence of intended and unintended pregnancies
The total number of pregnancies includes births, abortions, and miscarriages. We applied NFHS-4 estimates of unwanted and wanted fertility to the number of livebirths to estimate planned and unplanned births. All abortions are assumed to be unplanned pregnancies (appendix).25 The number of miscarriages was estimated based on natural patterns of pregnancy loss: 20% of livebirths and 10% of abortions.26-28 Because miscarriages are highly under-reported in face-to-face survey interviews, it is necessary to use data from clinical studies to estimate this component (appendix). Intended pregnancies are the sum of planned births and miscarriages resulting from intended pregnancies (ie, 20% of planned births), and unintended pregnancies are the sum of unplanned births, induced abortions, and miscarriages that resulted from unintended pregnancies (20% of unplanned births and 10% of abortions).
Statistical analysis
We used SPSS version 22 for statistical analyses of HFS data and SAS version 9.3 to compute standard errors around facility-based abortions estimates. We used STATA version 13.1 to analyse supplementary data from the NFHS-4.
Role of the funding source
The sponsors of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
We estimated that 15·6 million abortions (range 14·1 million–17·3 million) took place in India in 2015 (table 2), giving an abortion rate of 47·0 (42·2–52·1) per 1000 women aged 15–49 years (table 3).
Table 2.
Medium, low, and high estimates of total number of abortions, by source and type, India, 2015
| Medium estimate | Low estimate | High estimate | |
|---|---|---|---|
| Facility-based abortions (Component 1) | |||
| Public* | 813 503 | 671 684 | 955 423 |
| Private* | 2 464 476 | 2 034 839 | 2 894 417 |
| NGO facilities† | 97 273 | 97 273 | 97 273 |
| Total abortions provided in facilities | 3 375 252 | 2 803 795 | 3 947 114 |
|
| |||
| Medication abortions outside facilities‡ (Component 2) | |||
| For-profit medication abortion drug sales reported§ | 11 119 855 | 11 119 855 | 11 119 855 |
| Adjusted for differential use of mifepristone-only¶ | 10 711 137 | 10 570 199 | 10 888 840 |
| Adjusted for illegal export to Bangladesh and Nepal∥** | 10 587 694 | 10 413 324 | 10 794 330 |
| Increased by 5% to account for incomplete data coverage | 11 117 079 | 10 933 990 | 11 334 046 |
| Not-for-profit medication abortion drug distribution reported†† | 2 923 221 | 2 923 221 | 2 923 221 |
| Total medication abortion sales and distribution | 14 040 300 | 13 857 211 | 14 257 267 |
| Adjustment to account for wastage‡‡ | 1 404 030 | 1 801 437 | 998 009 |
| Adjustment to account for failed medication abortion use before facility-based abortion§§ | 168 289 | 223 656 | 78 726 |
| Removed medication abortion users counted in HFS that overlap with medication abortion drug sales data¶¶ | 1 005 736 | 1 005 736 | 1 005 736 |
| Total medication abortion outside of facilities (after adjustments above) | 11 462 245 | 10 826 382 | 12 174 797 |
|
| |||
| Total number of medication abortion and facility-based abortions (Component 1 + Component 2) | 14 837 497 | 13 630 178 | 16 121 911 |
|
| |||
| Other types of abortions (Component 3)∥∥ | 807 251 | 421 552 | 1 213 477 |
|
| |||
| Total number of induced abortions | 15 644 748 | 14 051 729 | 17 335 388 |
NGO=non-governmental organisation. HFS=Health Facilities Survey. A few subcomponents of the estimates are from comprehensive datasources (NGO statistics, and drug sales data are from for-profit and non-profit data sources). Other subcomponents are based on HFS results, expert opinion, or published data. These subcomponents involve assumptions and have a degree of uncertainty. To take this into account, we did sensitivity analyses and estimated lower and upper bound estimates for each of these subcomponents, providing a range around each. The total number of induced abortions for the medium estimate and the range around the medium estimate are the result of aggregating the medium, lower, and upper bound estimates across all subcomponents.
Medium estimate is the HFS-based weighted value. Low and high estimates are based on 95% CI calculated from the HFS (2 SD).
NGO service statistics (comprehensive count, no range around the medium estimate).
Outside facilities means outside of all facility types covered by the Health Facilities Survey.
For-profit medication abortion drug sales data, as reported by IMS Health (comprehensive count, no range around the medium estimate).
Medium estimate is based on expert opinion and literature and assumes that 80% of women use one mifepristone pill to induce abortion, 10% use two pills, and 10% use three pills; the low estimate assumes that 70% of women use one pill, 15% using two pills, and 15% use three pills, and the high estimate assumes that 90% of women use one pill, 5% use two pills, and 5% use three pills.
Medium estimate reduces for-profit medication abortion units in Assam and West Bengal by 10% of illegal medication abortion in border divisions of Bangladesh to account for black market export, based on in-country abortion research expert opinion and 2014 Bangladesh HFS results; the low estimate assumes a reduction by 13%, and the high estimates assume a reduction by 7%.
Medium estimate reduces for-profit medication abortion drug units by 72 000 to account for black market export to border regions in Nepal, distributed evenly across Bihar, Uttar Pradesh, West Bengal, and Uttarakhand, based on in-country abortion research expert opinion; the low estimate assumes a reduction by 72 000 medication abortion drug units plus 25%, and the high estimates assumes a reduction by 72 000 medication abortion drug units minus 25%.
Non-profit medication abortion distribution provided by Marie Stopes International and DKT International (comprehensive count, no range around the medium estimate).
Medium estimate reduces all medication abortion drugs for drug wastage by 10%, based on available literature sources; the low estimate assumes a reduction by 13%, and the high estimate assumes reduction by 7%.
Medium estimate assumes 5% of all facility-based abortion clients attempted a medication abortion outside a facility before obtaining an abortion in a facility, based on a study of abortion seekers in two states; the low estimate assumes that 8% of women were in this situation, and the high estimate assumes that 2% of women were in this situation.
Medium, low, and high estimates reduce medication abortion drugs by the number of medication abortions occurring in private and NGO facilities and those provided as a prescription in public facilities but filled at a pharmacy, to avoid double counting.
Medium estimate assumes that 5% of abortions are by methods other than medication abortion and from sources other than facility types covered in the HFS, based on community-based study findings from two states and national data on the increase in drug sales between 2009 and 2015; the low estimate assumes 3%, and the high estimate assumes 7%.
Table 3.
Abortion rate by type and source in India, 2015
| Medium estimate and recommended central point estimate of abortions (per 1000 women aged 15–49 years) | Range around medium estimate of abortions (per 1000 women aged 15–49 years)* | ||
|---|---|---|---|
|
|
|||
| Lower bound | Upper bound | ||
| Facility-based abortion | 10·1 | 8·4 | 11·9 |
| Surgical | 6·5 | 5·4 | 7·6 |
| Medication abortion | 3·6 | 3·0 | 4·2 |
|
| |||
| Medication abortions outside of facilities | 34·4 | 32·5 | 36·6 |
|
| |||
| Other types of abortion† | 2·4 | 1·3 | 3·6 |
|
| |||
| Total | 47·0 | 42·2 | 52·1 |
The lower bound and upper bound estimates represent the likely range of variation around the medium estimate, obtained by aggregating ranges around each subcomponent of abortion incidence (table 2).
Abortions from methods other than medication abortions and from sources other than facility types included in 2015 Health Facility Survey.
3·4 million abortions (range 2·8 million–3·9 million; 22%) were provided in health facilities. 64% of facility-based abortions were surgical, and the remaining were medication abortions. Public sector facilities accounted for 24% of these abortions, whereas private sector facilities accounted for 73% of all facility-based procedures, and NGO facilities accounted for the remainder (data not shown).
11·5 million induced abortions (range 10·8–12·2 million; 73%) were medication abortions that took place outside of health facilities (table 2). MA Combipacks were used for 87% of these medication abortions, and the remainder were induced with mifepristone and misoprostol sold separately (data not shown). The estimated number of medication abortions provided outside of health facilities includes some medication abortions that are provided by doctors working in private practice; these were not captured by the HFS. 0·8 million abortions (0·4 million–1·2 million; 5%) are estimated to be done outside of facilities and with methods other than medication abortion.
12·7 million abortions (81%) were medication abortions obtained either in or outside facilities (figure 1). 2·2 million abortions (14%) were by surgical methods, and 0·8 million abortions (5%) were done outside of facilities by methods other than medication or surgical abortion.
Figure 1.
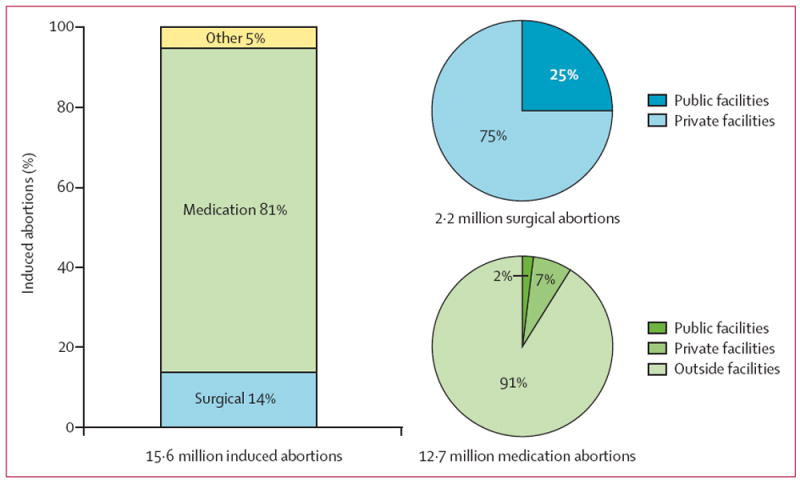
Distribution of abortions by method and source
With an estimated total of 48·1 million pregnancies (figure 2), the rate was 144·7 pregnancies per 1000 women aged 15–49 years. 25·8 million pregnancies (54%) resulted in births, 33% of pregnancies ended in induced abortions, and 14% of pregnancies ended in a miscarriage. 52% of all pregnancies were intended, (ie, births occurring at the time they were wanted and miscarriages resulting from planned pregnancies). The rate of unintended pregnancy was estimated at 70·1 pregnancies per 1000 women aged 15–49 years.
Figure 2.
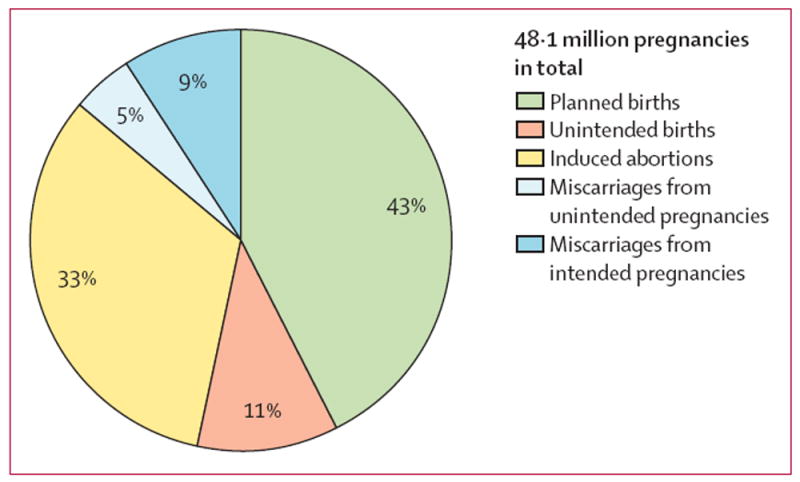
Distribution of pregnancies by outcome, India, 2015
Discussion
This study is the first large-scale study specifically designed to estimate abortion incidence in India. At 47·0 abortions per 1000 women aged 15–49 years, the abortion rate in India is within the range of reported estimates of abortion incidence in three other south Asian countries (figure 3).21,22,29 Additionally, our estimate of 3·4 million facility-based abortions in 2015 is nearly five times the number that was reported4 to government sources in 2014–15 (701 415 abortions). The difference was expected because official data on abortion are known to be highly underreported.
Figure 3.
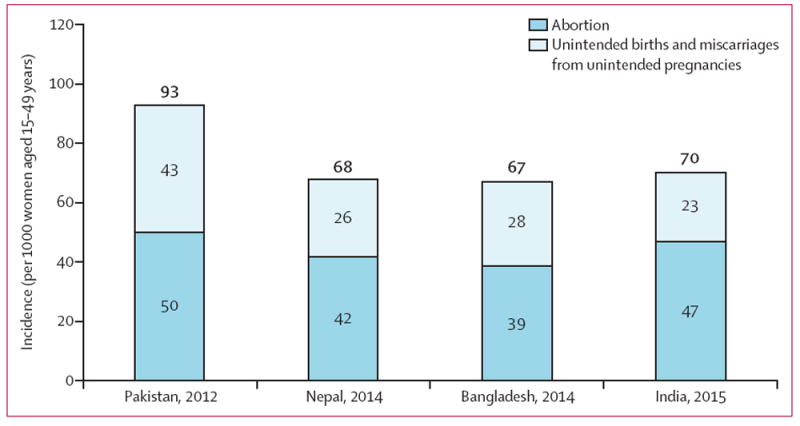
Incidence of unintended pregnancy, unplanned birth, and abortion in India, Pakistan, Nepal, and Bangladesh
47 abortions per 1000 women is, however, a substantially higher rate than the model-based estimate for the south Asian subregion (37 abortions per 1000 women aged 15–44 years).2,3 This is partly because the model necessarily used the only national estimate of abortion incidence available for India at the time it was developed, for 2002 (26 abortions per 1000 women) that is probably an underestimate because the study was not designed to estimate abortion incidence and used a very rough calculation based on a small sample of facilities. Nevertheless, our estimated abortion incidence is within the uncertainty interval around the model-based estimate for the subregion (uncertainty interval 30–50 abortions per 1000 women aged 15–44 years). If the subregional abortion incidence of 37 abortions per 1000 women were applied to the whole country in 2015, there would be an estimated 11·2 million abortions in that year.
Direct measurement is preferable to indirect estimation techniques when estimating abortion incidence because it is more robust and reliable. Indirect estimation techniques are applied in countries that restrict abortion by law and where measurement must necessarily rely on a number of assumptions. We relied on two direct sources of data that together accounted for 95% of all abortions: a large-scale survey of health facilities in six states that provide reproductive health services for about 45% of women of reproductive age in the country (scaled up to represent all states); and available data on the quantity of medication abortion drugs distributed in the entire country (no scaling up needed). Indirect methods were used to estimate the incidence of other abortions, the third component in our calculation of abortion incidence, which accounts for a very small proportion of all abortions (5%). The methodology used to estimate the incidence of abortion in India might be considered an improvement compared with previous indirect estimation methodologies.30 However, these improved approaches were feasible because abortion is broadly legal in India, facilitating the collection of abortion service provision data from facilities. The broadly legal status of abortion in India also means that mifepristone is an authorised drug. That a very high proportion of current use of medication abortion is in the form of MA Combipacks (mifepristone plus misoprostol), with each package used for a single abortion, made it feasible to estimate number of abortions from the number of sold packages. Quantities of mifepristone distributed as a separate drug were used to estimate the number of abortions with an assumption of the number of pills women were likely to use to induce abortion. The estimates do not integrate use of misoprostol alone for abortion because the many uses of this drug meant that it was not feasible to determine the quantity used to induce abortions. Although the widespread availability of the MA Combipack suggests that use of misoprostol alone to induce abortion is likely to be relatively infrequent, to the extent that misoprostol is still used, the estimated rate of 47 abortions per 1000 women of reproductive age is an underestimate.
This new estimate of abortion incidence also permits estimation of unintended pregnancy. 70 unintended pregnancies per 1000 women aged 15–49 years in India is within the range of incidence of unintended pregnancies in other south Asian countries (figure 3). Unintended pregnancy is a strong indicator of the need for improvement in contraceptive services. This rate of unintended pregnancy is consistent with the level of unmet need for effective contraception in 2015–16. The unmet need for contraception among married women in India was 13%, and an additional 6% of married women used traditional methods of contraception with relatively high failure rates. Other factors that might be contributing to both unintended pregnancy and abortion include contraceptive failure from incorrect and inconsistent use, sexual activity among unmarried women, and women’s and couples’ strength of motivation to have small families. The latter factor alone will probably reflect a number of other broader factors such as urbanisation, educational attainment, and the changing status and roles of women in society.
This study has several limitations. The nationwide incidence of facility-based abortions was estimated from survey data collected from health facilities in six states (selected to represent the six large regions of the country). These health facilities provide reproductive health services to about 45% of women of reproductive age in the country. A number of assumptions were made to generalise estimates from these six surveyed states to other states within each of the six large regions of India. Although these are plausible assumptions and similar assumptions have been used in an earlier study of abortion incidence in India (based on a much smaller sample of facilities), the 2015 estimates are an approximation of the true national number of facility-based abortions. Additionally, although data on medication abortion drugs were national, which is a strength of this study, several assumptions were necessary to obtain the best estimate of the proportion of these drugs that were actually used to induce abortions. In estimating the number of abortions within the component we referred to as other abortions, assumptions were also necessary because large-scale data on this component are scarce. These assumptions are based on existing relevant data or on expert opinion, so further research on these factors is needed to provide solid empirical data. We also estimated medication abortions outside of health facilities covered by the HFS. This large component includes some abortions that are legally provided by doctors in settings that were not included in the HFS (eg, private consultation rooms). When estimating the 2015 abortion incidence, we could not take into account use of misoprostol alone to induce abortion, and hence, to an unknown extent, the abortion incidence reported here is an underestimate of the true abortion incidence.
Because this is the first comprehensive study to estimate the incidence of unintended pregnancy and abortion, these new estimates for 2015 do not permit interpretation of trends in related reproductive behaviours and outcomes such as contraceptive prevalence and total fertility. The study findings also do not provide insights into reasons for abortion, including sex-biased abortion. However, it is notable that the national sex ratio at birth (number of girls per 1000 boys) has changed little in the past decade (901 girls per 1000 boys in 2005–07 vs 906 girls per 1000 boys 2012–14).31,32 Worldwide, the sex ratio is about 950 girls per 1000 boys at birth; the most recent sex ratio at birth in India (906 girls to 1000 boys) indicates that sex-biased abortion is occurring.33 More in-depth research is needed to understand these important issues, and the findings of this study can contribute to such analyses.
A number of policy and programmatic recommendations follow from the study’s results. Most abortions are happening without prescriptions and outside of facilities via chemists and informal vendors, which suggests the need to improve facility-based services. Most primary health centres and a large proportion of community health centres do not provide abortion services, and the shortage of trained staff and inadequate supplies are the primary reasons survey respondents gave for not providing this service. A first step is therefore to address these shortages through increased training and better logistical support for supplies. Examples of these improvements include expanding the provider base by: (1) training and certifying more medical doctors (ie, general practitioners) to perform abortions; (2) permitting and training practitioners who are trained in traditional or alternative medicine, midwifery, nursing, or auxiliary nursing–midwifery (ie, mid-level providers) to offer medication abortion services; (3) streamlining the process for approving private-sector facilities to provide abortion care; (4) ensuring adequate supplies of medication abortion pills and manual vacuum aspiration equipment in public-sector facilities; and (5) improving the quality of abortion and contraceptive services in the public sector by training providers to offer women confidential and respectful services and in-depth counselling.
Many of these recommendations are particularly needed at primary health centres because these facilities are the most accessible to the majority of women who live in rural areas and who are least likely to be able to afford private services. Some women might only have access to medication abortion from chemists and informal vendors, so it is also important for policy makers to consider adopting harm reduction strategies to support women’s self-use of medication abortion. Self-administration of medication abortion can be a safe and effective option if women have accurate information and access to health care if complications arise. Interventions are needed to provide women with accurate information on self-use of medication abortion, and on the availability of services in public facilities; also, research is needed to test interventions to improve chemists’ and informal vendors’ knowledge and practice in providing medication abortion. Studies in other countries have shown some measure of success with this type of intervention.34-36 Additionally, the Indian Government needs to increase attention to improving policies and practice regarding provision of contraceptive services to improve the ability of women and couples to prevent unintended pregnancy.
A rate of 70 unintended pregnancies per 1000 women and the finding that nearly half of all pregnancies are unintended suggest that there is great need for improvements in contraceptive services for women and for couples in general and in the context of abortion care. Consideration should be given to improving coverage, particularly in the public sector, and improving the quality of care (eg, by making a range of contraceptive methods available, having reliable supplies of contraceptive commodities, and ensuring that staff are trained to provide comprehensive counselling and follow-up services). With respect to abortion services, it is essential to ensure that contraceptive counselling and services are a standard component of care after abortion procedures and after treatment for abortion complications. Inadequate contraceptive services at the point of abortion care is a missed opportunity to help women prevent a subsequent unintended pregnancy and possible abortion.
Further research on the reasons women do not seek abortion care at health facilities is essential to understand how to change existing service provision practices and approaches and how to improve the abortion care that women receive outside of facilities. To monitor the effect of any efforts to improve services, better data collection systems need to be implemented, starting with training of providers and health-systems staff in the implementation of existing HMIS reporting systems.
The new estimates of incidence of abortion and unintended pregnancy in India will hopefully motivate and guide policies and programmes to improve the provision of abortion services and contraceptive care.
Supplementary Material
Research in context.
Evidence before this study
National abortion incidence in India was previously estimated in 1994 and 2002. These estimates used approximate measures based on small-scale studies that were not nationally representative or designed to capture national abortion incidence. In 1994, investigators estimated the abortion rate to be 33 abortions per 1000 women aged 15–49 years by using an assumption of the ratio of abortions to livebirths. In 2002, investigators included a small sample of providers in the formal (n=380) and informal (n=1270) sectors in six states (20% of the national population) and estimated a national rate of 26 abortions per 1000 women of reproductive age by assuming that population-per-site ratios and average caseloads per formal and informal type of facility represented the situation in all states. Notably, findings from small-scale, population-based surveys (in the states of Maharashtra and Tamil Nadu and part of the same study) with the objective of estimating state-level abortion incidence show much higher rates of abortion (45 abortions and 70 abortions per 1000 women of reproductive age, respectively).
The Ministry of Health and Family Welfare has recorded 621 000–770 000 abortions each year for the past 15 years. The most recent data are from 2014–15, when 701 415 abortions were recorded. These data greatly underestimate the incidence of abortion because they exclude abortions by private-sector doctors who are trained in abortion provision but do not work in registered facilities and abortions provided by other formally trained health professionals who do not have specific training in abortion but nonetheless provide the services. The latter include providers trained in systems other than the allopathic or Western system of medicine, principally Ayurveda, Unani, Siddha, and Homeopathy, some of whom provide abortion services. These data also exclude abortions using medication abortion drugs sold without a prescription and abortions by untrained providers.
Government-sponsored, large-scale, representative, community-based surveys such as the National Family Health Survey (NFHS) collect information about abortion through face-to-face interviews with women. In the 1998–99 NFHS-2 and the 2007–08 District Level Household and Facility Survey 3, women reported that 1·7–1·8% of pregnancies ended in abortions. This approach is known to result in high levels of under-reporting.
Women’s experience with accessing abortion services has been assessed in a few state-specific studies in the past decade. Although abortion incidence was not reported, a measure of prevalence was included in some studies (eg, lifetime experience of abortion) but with some limitations (limited in coverage and with potentially high under-reporting).
Added value of this study
To the best of our knowledge, this is the first study designed to measure the national incidence of abortion in India. To estimate the total number of abortions in the country as a whole, we combined data on the number of facility-based abortions (surgical and medication), the number of medication abortions outside facilities, and the number of abortions outside facilities using methods other than medication abortion.
Implications of the findings
The new national estimate of abortion incidence in India and the distribution of abortions by component (facility-based, using medication abortion outside of facilities, and outside of facilities with methods other than medication abortion) have important implications in terms of access and safety in the provision of abortion services. Most abortions are medication abortions, and most medication abortions are obtained outside health facilities. Although the combined medication abortion protocol of mifepristone plus misoprostol is highly effective and safe when administered correctly, little is known about what kind of information women are getting when they obtain this method from chemists and informal vendors, and whether they are taking it correctly. This is an important evidence gap that should be further explored.
The public sector has a relatively small role in abortion service provision. An implication of these findings is that the broader role of the public sector in providing high-quality health care to poor and vulnerable women needs to be reviewed and assessed in terms of possible need for an expanded role in providing abortion care. Pending amendments to the Medical Termination of Pregnancy Act (including the proposal to permit trained mid-level health professionals to provide abortion services) would be a feasible option for expanding access to safe, legal abortion services.
The incidence of unintended pregnancies and incidence of abortion are consistent with the level of unmet need for contraception among women in India and underscore the need for further investment to meet women’s and couples’ contraceptive needs and ensure access to safe abortion services.
The updated estimate of abortion incidence will be incorporated into future estimates of abortion incidence at the subregional, regional, and global levels and will improve the accuracy of these estimates.
Footnotes
Contributors
SS lead conceptualisation of the project, analysis, and writing. CS and AMM participated in conceptualisation of the project. RA and MRP contributed to the study design. RA, AMM, JJF, HS, MA, RH, AS, SK, AB, and MRP participated in project planning. MV and SS led and CS, JJF, HS, and MA contributed to sample design of the HFS. CS coordinated all aspects of fielding the Health Facility Survey. MRP organised the training of field workers who implemented the listing of private health facilities. CS, AMM, MRP, HS, JJF, RH, and AS did the piloting of the study protocol and tools. CS, MRP, HS, and MA selected the fielding agencies. CS, AMM, MS, JJF, HS, AS, MV, SK, and AB cofacilitated the training of trainers and AMM, MRP, JJF, MS, HS, RH, SK, and AB participated in state-level trainings of interviewers. CS, RA, AMM, MS, JJF, and SK contributed to the literature search. RA, AS, and AB coordinated communication with IMS Health to obtain medication abortion data. AMM and AB gathered non-profit medication abortion data, and MA, MS, and AB processed all medication abortion data. SK compiled data from non-governmental organisations on abortion service provision. CS, RA, and SK liaised with the Indian Ministry of Health and Family Welfare. CS convened the Technical Advisory Committee. CS and MRP did supplementary analysis of NFHS data. SS, RH, and MS wrote the paper. RH and MS implemented analytical decisions. SS, MS, RH, MV, and JJF wrote the appendix and RA and CS reviewed the appendix. All authors contributed to the development of study tools, participated in analytical decisions, and reviewed the paper.
Declaration of interests
We declare no competing interests.
See Online for appendix
Contributor Information
Susheela Singh, Guttmacher Institute, New York, NY, USA.
Prof Chander Shekhar, International Institute for Population Sciences, Mumbai, India.
Rajib Acharya, Population Council, New York, NY, USA.
Ann M Moore, Guttmacher Institute, New York, NY, USA.
Melissa Stillman, Guttmacher Institute, New York, NY, USA.
Manas R Pradhan, International Institute for Population Sciences, Mumbai, India.
Jennifer J Frost, Guttmacher Institute, New York, NY, USA.
Harihar Sahoo, International Institute for Population Sciences, Mumbai, India.
Manoj Alagarajan, International Institute for Population Sciences, Mumbai, India.
Rubina Hussain, Guttmacher Institute, New York, NY, USA.
Aparna Sundaram, Guttmacher Institute, New York, NY, USA.
Michael Vlassoff, Guttmacher Institute, New York, NY, USA.
Shveta Kalyanwala, is an independent consultant.
Alyssa Browne, Guttmacher Institute, New York, NY, USA.
References
- 1.Chhabra R, Nuna S. Abortion in India: an overview. New Delhi, India: Veerenda Printers; 1994. [Google Scholar]
- 2.Duggal R, Ramachandran V. The abortion assessment project—India: key findings and recommendations. Reprod Health Matters. 2004;12:122–29. doi: 10.1016/s0968-8080(04)24009-5. [DOI] [PubMed] [Google Scholar]
- 3.Sedgh G, Bearak J, Singh S, et al. Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet. 388:258–67. doi: 10.1016/S0140-6736(16)30380-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministry of Health and Family Welfare. Health and family welfare statistics of India 2015. New Delhi: Ministry of Health and Family Welfare, Statistics Division; 2015. [Google Scholar]
- 5.Jones RK, Kost K. Underreporting of induced and spontaneous abortion in the United States: an analysis of the 2002 National Survey of Family Growth. Stud Fam Plann. 2007;38:187–97. doi: 10.1111/j.1728-4465.2007.00130.x. [DOI] [PubMed] [Google Scholar]
- 6.Sedgh G, Henshaw SK. Measuring the incidence of abortion in countries with liberal laws. In: Singh S, Remez L, Tartaglione A, editors. Methodologies for estimating abortion incidence and abortion-related morbidity: a review. New York: Guttmacher Institute and International Union for the Scientific Study of Population; 2010. pp. 23–33. [Google Scholar]
- 7.Rossier C. Estimating induced abortion rates: a review. Stud Fam Plann. 2003;34:87–102. doi: 10.1111/j.1728-4465.2003.00087.x. [DOI] [PubMed] [Google Scholar]
- 8.Government of India. The medical termination of pregnancy act [Act No 34, 1971] New Delhi: Government of India; 1971. [Google Scholar]
- 9.Jejeebhoy S, Zavier AJF, Acharya R, Kalyanwala S. Increasing access to safe abortion in rural Maharashtra: outcomes of a comprehensive abortion care model. New Delhi: Population Council; 2011. [Google Scholar]
- 10.Jejeebhoy S, Zavier AJF, Acharya R, Kalyanwala S. Increasing access to safe abortion in rural Rajasthan: outcomes of a comprehensive abortion care model. New Delhi: Population Council; 2011. [Google Scholar]
- 11.Powell-Jackson T, Acharya R, Filippi V, Ronsmans C. Delivering medical abortion at scale: a study of the retail market for medical abortion in Madhya Pradesh, India. PLoS One. 2015;10:e0120637. doi: 10.1371/journal.pone.0120637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tariq M, Chaudhury N, Kapoor A. Medical abortion drug dispensing behavior among pharmacists in India. XXVII IUSSP International Population Conference; Busan, South Korea. Aug 26–31, 2013; [Aug 14, 2017]. http://iussp.org/sites/default/files/event_call_for_papers/Long%20Abstract_MA%20_IUSSP_2013.pdf. [Google Scholar]
- 13.Government of India. The medical termination of pregnancy (amendment) act. New Delhi: Government of India; 2002. [Google Scholar]
- 14.Government of India. The medical termination of pregnancy rules (amendment) New Delhi: Government of India; 2003. [Google Scholar]
- 15.Kumar M. IMS Health: A brief introduction. Delhi: IMS Health; 2014. [Google Scholar]
- 16.UN, Department of Economic and Social Affairs, Population Division. [May 15, 2016];World population prospects: the 2015 revision. https://esa.un.org/unpd/wpp/
- 17.Elul B, Sheriar N, Anand A, Philip N. Are obstetrician-gynecologist in India aware of and providing medical abortion? J Obstet Gynaecol India. 2006;56:340–45. [Google Scholar]
- 18.Vlassoff M, Diallo A, Philbin J, Kost K, Bankole A. Cost-effectiveness of two interventions for the prevention of postpartum hemorrhage in Senegal. Int J Gynecol Obstet. 2016;133:307–11. doi: 10.1016/j.ijgo.2015.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seligman B, Xingzhu L. Policy and financing analysis of selected postpartum hemorrhage interventions: country summary. Cambridge, MA: Abt Associates; 2006. [Google Scholar]
- 20.Kumar R, Zavier AJ, Kalyanwala S, Jejeebhoy SJ. Unsuccessful prior attempts to terminate pregnancy among women seeking first trimester abortion at registered facilities in Bihar and Jharkhand, India. J BiosocSci. 2013;45:205–15. doi: 10.1017/S0021932012000533. [DOI] [PubMed] [Google Scholar]
- 21.Puri M, Singh S, Sundaram A, Hussain R, Tamang A, Crowell M. Abortion incidence and unintended pregnancy in Nepal. Int Perspect Sex Reprod Health. 2016;42:197–209. doi: 10.1363/42e2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh S, Hossain A, Maddow-Zimet I, Vlassoff M, Bhuiyan HU, Ingerick M. The incidence of menstrual regulation procedures and abortion in Bangladesh, 2014. Int Perspect Sex Reprod Health. 2017;43:1–11. doi: 10.1363/43e2417. [DOI] [PubMed] [Google Scholar]
- 23.Stillman M, Frost JJ, Singh S, Moore AM, Kalyanwala S. Abortion in India: a literature review. New York, NY: Guttmacher Institute; 2014. pp. 12–14. [Google Scholar]
- 24.Banerjee SK, Andersen K. Exploring the pathways of unsafe abortion in Madhya Pradesh, India. Glob Public Health. 2012;7:882–96. doi: 10.1080/17441692.2012.702777. [DOI] [PubMed] [Google Scholar]
- 25.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 26.Tietze SL, Lincoln R. Fertility regulation and the public health. New York, NY: Springer; 1987. Teenage pregnancies: looking ahead to 1984; pp. 339–43. [Google Scholar]
- 27.Bongaarts J, Potter R. Fertility, biology, and behavior: an analysis of the proximate determinants. New York, NY: Academic Press; 1983. [Google Scholar]
- 28.Darroch JE, Singh S. Adding it up: the costs and benefits of investing in family planning and maternal and newborn health—estimation methodology. New York, NY: Guttmacher Institute; 2011. [Google Scholar]
- 29.Sathar Z, Singh S, Rashida G, Shah Z, Niazi R. Induced abortions and unintended pregnancies in Pakistan. Stud Fam Plann. 2014;45:471–91. doi: 10.1111/j.1728-4465.2014.00004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Singh S, Remez L, Tartaglione A. Methodologies for estimating abortion incidence and abortion-related morbidity: a review. New York, NY: Guttmacher Institute and IUSSP; 2010. [Google Scholar]
- 31.Office of the Registrar and Census Commissioner. Sample Registration System Statistical Report 2014. New Delhi: Office of the Registrar and Census Commissioner; 2016. [Google Scholar]
- 32.Office of the Registrar and Census Commissioner. Sample Registration System Statistical Report 2007. New Delhi: Office of the Registrar and Census Commissioner; 2008. [Google Scholar]
- 33.Parazzini F, La Vecchia C, Levi F, Franceschi S. Trends in male: female ratio among newborn infants in 29 countries from five continents. Hum Reprod Oxf Engl. 1998;13:1394–96. doi: 10.1093/humrep/13.5.1394. [DOI] [PubMed] [Google Scholar]
- 34.Fetters T, Raisanen K, Mupeta S, et al. Using a harm reduction lens to examine post-intervention results of medical abortion training among Zambian pharmacists. Reprod Health Matters. 2014;22:116–24. doi: 10.1016/S0968-8080(14)43794-7. [DOI] [PubMed] [Google Scholar]
- 35.Reiss K, Keenan K, Church S, et al. Harm reduction from drug shop provision of menstrual regulation medications in Bangladesh. London: Marie Stopes International; 2015. [Google Scholar]
- 36.Tamang A, Puri M, Lama K, Shrestha P. Pharmacy workers in Nepal can provide the correct information about using mifepristone and misoprostol to women seeking medication to induce abortion. Reprod Health Matters. 2014;22:104–15. doi: 10.1016/S0968-8080(14)43785-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


