Abstract
Natural disasters, such as hurricanes and floods, are increasing in frequency and scope. Youth exposed to disasters are at risk for developing posttraumatic stress symptoms (PTSS). However, not all youth who report initially elevated PTSS report persistent PTSS that last beyond the first three to six months postdisaster. Thus, it is crucial to understand how and why youth differ in their patterns of PTSS. This study reviewed the literature on children’s postdisaster PTSS, evaluating the typical number and types of patterns for children’s PTSS trajectories, as well as risk and protective factors predicting trajectory membership. This review identified eight empirical studies on youth PTSS trajectories following natural disasters; these studies included 8,306 children aged 3 to 18 years. All studies identified resilience, recovery, and chronic trajectories. Evidence for a delayed trajectory was mixed. Proportions of children falling into each trajectory varied widely across studies, but overall, resilience was the most prevalent trajectory. These findings were consistent across study factors (i.e., analytic strategy, assessment timing, and study selection criteria). Female gender, disaster exposure, negative coping, and lack of social support were significant risk factors for chronic trajectories across several studies. Future research should combine individual level participant data across studies of children’s responses to disasters to better understand PTSS trajectories.
Youth are the largest age group affected by disasters (e.g., hurricanes, floods, wildfires, droughts) around the world (United Nations Office for Disaster Risk Reduction [UNISDR], 2015). Worldwide, over 100 million children are exposed to disasters each year (UNISDR, 2011). Disasters may be defined as large-scale, single incident potentially traumatic events. In the United States alone, 14.0% of children report experiencing a disaster during childhood (Becker-Blease, Turner, & Finkelhor, 2010). This is concerning, given that natural disasters are expected to increase in frequency and intensity (U.S. Global Change Research Program, 2016).
Disasters present a significant threat to children’s mental health (La Greca et al., 2013; McDermott, Cobham, Berry, & Kim, 2014). Posttraumatic stress symptoms (PTSS) are the primary presenting problem in children after disasters (Furr, Comer, Edmunds, & Kendall, 2010). Across studies of disasters, rates of elevated PTSS vary widely, with some estimates being higher than 70.0% when assessed within the first 3 months postdisaster (Kucukoglu, Yildirim, & Dursun, 2015). The presence of PTSS may be debilitating for children, and in the long term PTSS are associated with poor life outcomes in terms of education, jobs, physical health, and mental health (Hadi, Lai, & Llabre, 2014). The purpose of the current study was to review the literature on children’s patterns of risk and resilience postdisaster as well as the factors that predict these patterns or trajectories.
Disaster management experts advocate that stepped care models of intervention are needed to effectively address post-disaster mental health needs (Pfefferbaum & North, 2016). Stepped care models triage children based on their mental health needs so that children at the highest risk for chronic distress (i.e., PTSS that are clinically elevated more than three to six months after disasters) receive the most intensive, and therefore most costly, interventions. This approach is necessary due to the large numbers of children exposed to disasters and the limited funding available to address children’s postdisaster mental health needs (Wizemann, Reeve, & Altevogt, 2014).
To date, it is not clear how to stratify children based on their risk for chronic postdisaster PTSS. Few studies have assessed children at multiple time points after disasters, and even fewer have assessed children beyond the first 12 months postdisaster (Pfefferbaum et al., 2013). The few existing longitudinal studies that have followed children postdisaster have primarily focused on understanding children’s average responses to disasters through the use of traditional, variable-centered approaches (e.g., analysis of variance). Although informative, these approaches assume that all children in disaster-affected areas follow a similar pattern of PTSS postdisaster.
With recent advances in analytic approaches, we now have the ability to examine how and when children’s postdisaster PTSS arise and develop, and which children may be at highest risk for persistent distress. Person-centered approaches, such as growth mixture modeling and group categorization, can identify heterogeneous patterns of disaster response and provide information about whether and why children differ in their responses to disasters over time.
A growing body of literature documents heterogeneity among adults’ responses to potentially traumatic events (Bonanno, Brewin, Kaniasty, & La Greca, 2010; Bonanno & Mancini, 2008). Across studies, these trajectories are (a) chronic (persistent elevated PTSS over time); (b) recovery (initial elevated PTSS, followed by a decrease in PTSS at later time points); (c) resilience (persistent low PTSS over time); and (d) delayed (initial subclinical PTSS, followed by an increase in PTSS at later time points).
To date, several studies have examined whether these four trajectories may be directly applied to children, using a priori categorization (e.g., choosing cutoff scores to categorize children into chronic, recovery, resilience, and delayed trajectories; Fan, Long, Zhou, Zheng, & Liu, 2015; Kronenberg et al., 2010; Liu et al., 2011; McDermott et al., 2014). However, trajectories identified among adults may provide limited insight into children’s postdisaster responses, given that children’s experiences during and after potentially traumatic events are distinct from those of adults (Fothergill & Peek, 2015). Bonanno et al. (2010) also highlight that displays of disaster-related stress differ by age. Many factors related to resilience may differ by age (e.g., the term community may hold a different meaning for a child than an adult).
Person-centered approaches are being utilized in child disaster research, but to date no clear consensus regarding the number and type of children’s PTSS trajectories has emerged. This is due in part to the fact that person-centered approaches are data-driven. Consensus may only be developed by examining findings from multiple studies across multiple disasters, which has not yet been done. This work is needed to help identify risk and protective factors that influence and distinguish children’s likelihood of falling into various PTSS trajectories; this work will aid in early identification of subgroups of children at increased risk for mental distress (i.e., before symptoms become chronic). In the disaster literature, conceptual frameworks highlight several factors as influencing children’s postdisaster PTSS: preexisting child characteristics, disaster exposure, ongoing loss/disruption, other stressors, and social support (Furr et al., 2010).
This review of children’s trajectories of PTSS postdisaster helps fill critical gaps in knowledge about the number and type of PTSS trajectories among children. Our first aim was to evaluate the typical number and types of child postdisaster PTSS trajectories identified in the literature. We examined whether analytic strategy, assessment timing, and study selection criteria influenced findings. Our second aim was to evaluate risk and protective factors that distinguished PTSS trajectories.
Method
A literature search was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines (Moher, Liberati, Tetzlaff, & Altman, 2009) to examine PTSS trajectories in children following disasters. This search was broad, in that we allowed for the inclusion of both natural disasters (e.g., hurricanes, floods) and man-made disasters (e.g., terrorist events, oil spills). The literature search was conducted in May 2016 and June 2016 using PubMED and all databases available through the EBSCOhost database (a total of 92 individual databases at the time of the search, including PsycINFO, PsycARTICLES, and MEDLINE). The following search terms were used: (1) trajector*; (2) posttraumatic stress, PTSD, depress*, or anxiety; (3) child* or adolescent; and (4) trauma, traumatic, incident, or disaster. Because disasters may be defined as large-scale potentially traumatic events (Furr et al., 2010), search terms were intentionally broad (i.e., included trauma and incident) to ensure that the literature search encompassed all types of disasters, including man-made disasters which may not specifically use the term disaster as a description of the event.
Three additional search strategies were conducted to ensure all relevant articles were included (see complete details in Appendix A in the online Supporting Information). First, the authors searched prominent child and trauma journals. Second, the first three authors generated a list of experts in the field of child PTSS trajectories; searches were performed for each identified expert. Third, reference lists of electronically identified studies were manually searched for relevant literature.
Studies were selected based on six inclusion criteria: (1) participants must have been under 18 years of age, (2) articles must have been written in English, (3) articles must have been published in an academic journal, (4) trajector* must have appeared in the abstract for the article, (5) trauma type must have been a natural or man-made disaster, and (6) studies must have been quantitative studies specifically focusing on PTSS trajectories of children and/or adolescents.
A diagram of data extraction is depicted in Figure 1 in the online Supporting Information. After initial article identification, the title and abstract of each article were read to determine if the article met inclusion criteria, resulting in eight articles for inclusion in this review. Each study was coded by the first three authors. Trauma type, age of participants, time points of assessment, symptoms assessed, significant and nonsignificant risk and protective factors, and number of trajectories and percent of the sample following each trajectory were noted. Inconsistencies were discussed by the first three authors until consensus was reached.
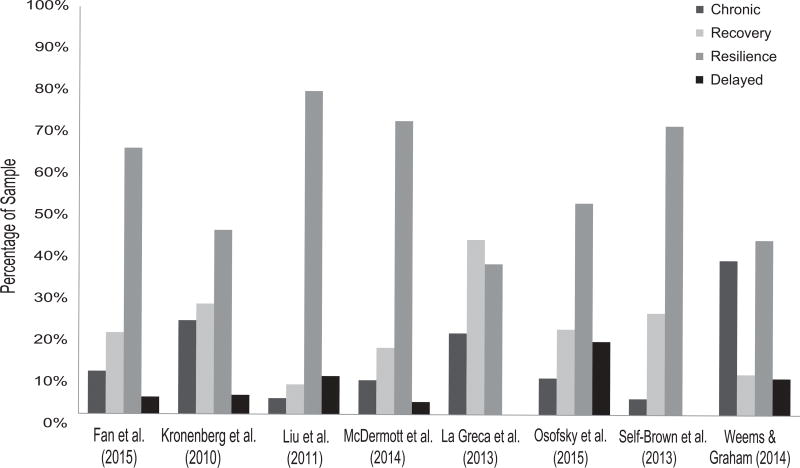
Figure 1.
Youth posttraumatic stress symptom (PTSS) trajectories identified in the literature. McDermott et al. (2014) assessed primary school and secondary school students separately; trajectory totals from each age group were combined for this review. La Greca et al. (2013), Osofsky et al. (2013), Self-Brown et al. (2013), and Weems and Graham (2014) utilized person-centered approaches rather than a priori categorization.
The primary goal was to evaluate trajectory patterns of PTSS after disasters among children. Results have been described as a narrative.
Terminology
Trajectories
Terminology for trajectories in this article was standardized based on shapes described in previous articles (Bonanno & Mancini, 2008). Trajectories were defined by PTSS patterns over time: chronic (persistent elevated PTSS over time); recovery (initial elevated PTSS, followed by a decrease in PTSS at later time points); resilience (persistent low PTSS over time); and delayed (initial low PTSS, followed by an increase in PTSS at later time points).
Analytic strategy: Trajectory categories chosen a priori
Studies were categorized as choosing trajectories a priori if they assigned children to trajectory classes based upon predetermined categories. Limitations to this approach include the inability to test underlying taxonomic theory (because categories are assumed a priori) and overfitting, the creation of trajectory categories that reflect random variation. In addition, this approach does not allow for calibrating precision of child classification to trajectories (Nagin, 1999).
Analytic strategy: Person-centered approaches
Person-centered approaches recognize patterns in PTSS trajectories using person-level data without the use of a priori cutoff scores. Results are data-driven, and thus results should be informed by theory and evidence from research using a priori trajectory categorization. This analytic technique is especially advantageous over a priori categorization methods for correctly identifying children with symptoms near the preselected defined cutoff scores. Person-centered approaches can correctly identify these children (Bainter & Curran, 2015). In addition, these techniques allow for modeling uncertainty related to group membership (Nagin, 1999).
Social support
Social support consists of perceived care and emotional support from family members, teachers, friends, and others. All social support measures used in the studies reviewed for this article were validated for use with child populations (Table 1). Measures focused on perceptions of emotional support from others, such as having parents who understand you, or having a close friend. Social support may also be defined as connectedness to others (McDermott et al., 2014), such as having friends to play with during school breaks.
Table 1.
Summary of Child Postdisaster Posttraumatic Stress Symptoms (PTSS) Trajectory Research
| Study | Disaster | Baseline age (years) |
Children included in analyses (n) |
Assessments (months postdisaster) |
Measure of PTSS | Additional measure(s) |
|---|---|---|---|---|---|---|
| Trajectory categories chosen a priori: | ||||||
| Fan et al. (2015) | Wenchuan Earthquake | 12–16 | 1,573 | 6, 12, 18, 24 | PTSD Self-Rating Scaleb | SCSQb; SSRSb; ASLECb |
| Kronenberg et al. (2010) | Hurricane Katrina | 9–18 | 387 | 24, 36 | NCTSN HARTb, based on the PTSD-RI | Unnamed measure for life stressorsb |
| Liu et al. (2011) | Sichuan Earthquake | 8–11 | 330 | 6, 12 | TSCC-Ab | N/A |
| McDermott et al. (2014) | Cyclone Larry | 8–15 | 262 | 3, 18 | PTSD-RIb | Unnamed measures for Cyclone Exposure, Connectednessb; SDQb |
| Trajectories chosen via person-centered modeling: | ||||||
| La Greca et al. (2013) | Hurricane Andrew | 8–11 | 568 | 3, 7, 10 | PTSD-RIb | HURTEb; RCMASb; Kidcopeb; SSSCb; LESb |
| Osofsky et al. (2015) | Hurricane Katrina; Hurricane Gustav; Gulf Oil Spill | 3–18 | 4,619 | 12, 24, 37, 49a | LSU KIDSc, based on the PTSD-RI | Unnamed measures for hurricane exposure, oil spill stressc |
| Self-Brown et al. (2013) | Hurricane Katrina | 8–16 | 426 | 3, 13, 19, 25 | PTSD-RI – Revision 1b | HURTEb; SSSCb; SAVEb; KID-SAVEb |
| Weems & Graham (2014) | Hurricane Katrina; Hurricane Gustav | 8–15 | 141 | -12 (predisaster), −6 (predisaster); 1 (postdisaster)a |
PTSD-RIb | Hurricane Exposure measure based on HURTEb; CCSCb |
Note. PTSS = posttraumatic stress symptoms; PTSD = posttraumatic stress disorder; SSRS = Social Support Rate Scale; SCSQ = Simplified Coping Style Questionnaire; ASLEC = Adolescent Self-Rating Life Events Checklist; NCTSN = National Child Traumatic Stress Network; HART = Hurricane Assessment and Referral Tool for Children and Adolescents; PTSD-RI = University of California at Los Angeles PTSD Reaction Index for Children; N/A = not applicable; TSCC-A = Traumatic Symptom Checklist for Children–Alternate Version; SDQ = Strengths and Difficulties Questionnaire; LSU KIDS = Louisiana State University Health Sciences Center Katrina-inspired disaster screenings; HURTE = Hurricane-Related Traumatic Experiences Scale; RCMAS = Revised Children’s Manifest Anxiety Scale; SSSC = Social Support Scale for Children; LES = Life Events Schedule; SAVE = Screen for Adolescent Violence Exposure; KID-SAVE = SAVE for children in third to seventh grades; CCSC = Children’s Coping Strategies Checklist.
Timing given in relation to Hurricane Gustav;
Refers to a self-report measure;
For children under 8 years of age, measures were completed by a parent, otherwise self-reported.
Coping
After a disaster, coping refers to the way in which an individual deals with disaster exposure and/or related stressors, such as perceived life threat, death of a family member, or relocation. Negative coping refers to destructive ways of dealing with exposure and stressors, whereas positive coping refers to constructive ways of dealing with exposure and stressors. Three specific examples of negative coping were examined in the studies included in this review. Blame coping is blaming oneself or others for causing a “bad thing” to occur (in this context, a disaster). Anger coping involves yelling, screaming, and/or getting mad as a result of the disaster (La Greca et al., 2013). Avoidant coping is trying to stay away from reminders of the disaster and from things that make one upset (Weems & Graham, 2014). Positive coping as a general concept was discussed in one study (Fan et al., 2015); however, no specific examples of positive coping were examined in the studies included in this review.
Results
Figure 1 in the online Supporting Information outlines the number of articles yielded at each stage of data extraction. A total of 166 articles were identified in the initial literature search, and 138 were selected for further screening. Among these studies, eight articles eligible for inclusion in this review on child postdisaster PTSS trajectories were identified (k = 8, with k representing number of articles included in the present review). These studies included 8,306 children aged 3 to 18 years. Table 1 provides an overview of the characteristics of these studies.
Study Selection Criteria
Inclusion criteria for all eight studies were based on child enrollment at schools involved in the study. For seven studies, schools chosen for inclusion were directly affected by a disaster, whereas in the eighth study (Liu et al., 2011), students were sampled from a camp school erected after the 2008 Sichuan Earthquake in China. No explicit exclusion criteria were used at enrollment. However, four studies excluded participants from analyses: Self-Brown, Lai, Thompson, McGill, and Kelley (2013) excluded participants who did not provide PTSS-related responses on any assessment; Weems and Graham (2014) excluded participants who were missing one assessment; and Osofsky, Osofsky, Weems, King, and Hansel (2015) and Kronenberg et al. (2010) both excluded participants who only completed one assessment. To accommodate missing data, McDermott et al. (2014) used estimation maximization procedures; Osofsky et al. (2015) used multiple imputation; Self-Brown et al. (2013) used maximum likelihood estimation; La Greca et al. (2013) used full information maximum likelihood (FIML).
Assessment Timing
Timing of first assessments in the studies reviewed ranged from 12 months predisaster (Weems & Graham, 2014) to 24 months postdisaster (Kronenberg et al., 2010). Final assessment timing ranged from 1 month postdisaster (Weems & Graham, 2014) to 49 months postdisaster (Osofsky et al., 2015). The number of time points also varied by study, with three studies administering two assessments, two studies administering three assessments, and three studies administering four assessments (see Table 1).
PTSS Measures
Multiple instruments were used to evaluate PTSS (see Table 1). Across studies, child report of PTSS was used for children 8 years of age or older. Parent report was used in one study (Osofsky et al., 2015) for children aged 3 to 7 years. Six studies used either the University of California at Los Angeles (UCLA) Posttraumatic Stress Disorder (PTSD) Reaction Index for Children (PTSD-RI; La Greca et al., 2013; McDermott et al., 2014; Self-Brown et al., 2013; Weems & Graham, 2014) or a variation (Kronenberg et al., 2010; Osofsky et al., 2015). The PTSD-RI is considered appropriate for children aged 7 years and older; children are asked to rate endorsement of statements related to PTSS on a scale of 0 (none of the time) to 4 (most of the time). One study (Liu et al., 2011) used the Trauma Symptoms Checklist for Children–Alternate Version (TSCC-A). The TSCC-A is designed for children aged 8 to16 years and consists of 44 items presented as thoughts, feelings, and behaviors. Children are asked to rate endorsement of items on a scale of 0 (never) to 3 (almost all of the time). One study (Fan et al., 2015) used the PTSD Self-Rating Scale (PTSD-SS). In this measure, children are asked to rate endorsement of 24 symptoms on a scale of 1 (not at all) to 5 (extremely severe).
Aim 1: Evaluate the Typical Number and Types of Child Postdisaster PTSS Trajectories
All of the studies reviewed included at least three trajectories (see Figure 1): chronic, recovery, and resilience. Evidence for a delayed trajectory was mixed. Three studies (37.5% of k = 8 studies; k refers to number of articles included in the present review) identified a delayed trajectory, but two found no evidence for a delayed trajectory, and three found only limited evidence (i.e., less than 5.0% of the children studied fell in a delayed trajectory). Given differences in analytic strategy and selection criteria, we examined trajectory patterns based on (a) analytic strategy (i.e., trajectories chosen a priori versus person-centered approaches); (b) assessment timing (i.e., all assessments completed within the first year versus final assessments completed beyond the first year); and (c) study selection criteria (i.e., elementary school–aged youth, secondary school–aged youth, broad age ranges).
Analytic strategy
A priori categorization
Four studies predetermined the number and type of PTSS trajectories they expected to observe among children exposed to disasters (see Table 1). Two studies (Fan et al., 2015; Kronenberg et al., 2010) defined their trajectories based on previous literature (e.g., Bonanno & Mancini, 2008; Masten & Obradovic, 2008), whereas two studies (Liu et al., 2011; McDermott et al., 2014) did not reference particular theorists. Of note, three of these studies only assessed children at two time points. Limited follow-up assessments may have influenced the choice to use categories chosen a priori, as advanced longitudinal modeling strategies generally require at least three time points (Kline, 2016).
Among the studies that utilized categories chosen a priori, the percent of children falling in the chronic trajectory ranged from 3.9% to 23.0%; the recovery trajectory ranged from 7.3% to 27.1%; the resilience trajectory ranged from 45.2% to 79.4%; and the delayed trajectory ranged from 3.1% to 9.4%. The largest trajectory group was the resilience trajectory in all 4 studies utilizing a priori categorization.
Person-centered modeling
Among the four studies that used person-centered modeling techniques, the percentage of children falling in the chronic trajectory ranged from 4.0% to 38.0%; the recovery trajectory ranged from 10.0% to 43.0%; the resilience trajectory ranged from 37.0% to 71.0%; and the delayed trajectory ranged from 0.0% (i.e., no evidence) to 18.0%. The resilience trajectory was the largest group in three studies that utilized person-centered modeling, whereas the recovery trajectory was the largest group in the La Greca et al. (2013; 43.0%) study.
Of the four studies that used person-centered methods, two studies used growth mixture modeling (La Greca et al., 2013; Self-Brown et al., 2013), and two studies used cluster analyses to identify PTSS trajectories (Osofsky et al., 2015; Weems & Graham, 2014). All four studies referenced prior research and theory on PTSS trajectories. In the La Greca et al. (2013) study, unconditional latent growth mixture models (with no predictors) were estimated for one to five trajectories. In the Self-Brown et al. (2013) study, unconditional latent class growth analysis models (with no predictors) were estimated for one to four trajectories. In both of these studies, a decision to retain three trajectories was made; neither found evidence for a delayed trajectory. In the Osofsky et al. (2015) study, cluster analyses utilizing a Euclidian distance measure indicated that four trajectories provided a good fit for the data; hierarchical linear modeling analyses were also completed in order to examine PTSS trends over time. In the Weems and Graham (2014) study, cluster analyses using a log-likelihood distance measure indicated that five trajectories would be optimal for the data. Because the “moderate” and “stable high” trajectories presented by Weems and Graham (2014) both consisted of persistent elevated PTSS across time points, these trajectories were combined into a single “chronic” trajectory for the results of this review.
A key design feature of studies using person-centered modeling is sample size. Although there is no general rule of thumb for sample sizes in person-centered modeling, larger sample sizes are preferred. For growth modeling, sample sizes of at least 100 are needed, depending on study factors such as the number of assessment time points (Curran, Obeidat, & Losardo, 2010). Both studies that used this type of analysis included over 400 participants. For cluster analysis, there is no heuristic for determining an appropriate sample size, but larger sample sizes are also recommended (Siddiqui, 2013). One study (Weems & Graham, 2014) had a relatively small sample size (n = 141), whereas the other (Osofsky et al., 2015) had a larger sample size (n = 4,619).
Assessment timing
Assessments completed within the first year
Three studies completed all assessments within the first year postdisaster. Across these studies, the percentage of children falling in the chronic trajectory ranged from 3.9% to 38.0%; recovery trajectory ranged from 7.3% to 43.0%; resilience trajectory ranged from 37.0% to 79.4%; and delayed trajectory ranged from 0.0% (i.e., no evidence) to 9.4%. Two of the studies (Liu et al., 2011; Weems & Graham, 2014) reported the resilience trajectory was the largest trajectory group. La Greca et al. (2013; 43.0%) found the recovery trajectory to be the largest trajectory group.
Final assessment completed after the first year
Among the five studies that followed children beyond one year after a disaster, the percent of children falling in the chronic trajectory ranged from 4.0% to 23.0%; recovery trajectory ranged from 16.4% to 27.1%; resilience trajectory ranged from 45.2% to 72.1%; and delayed trajectory ranged from 0.0% (i.e., no evidence) to 18.0%. All five studies reported that the resilience trajectory was the largest group.
Study selection criteria
Elementary school–aged children
In two studies, selection criteria for inclusion in the study focused on elementary school–aged children, specifically those who were 8 to 11 years of age at first assessment. These two studies (La Greca et al., 2013; Liu et al., 2011) found, respectively, the percentage of children in the chronic trajectory was 20.0% and 3.9%; the recovery trajectory was 43.0% and 7.3%; the resilience trajectory was 37.0% and 79.4%; and the delayed trajectory was 0.0% (i.e., no evidence) and 9.4%. The findings from these two studies were not consistent. Liu et al. (2011) found the largest group to be the resilience trajectory (79.4%), whereas La Greca et al. (2013) found the largest group to be the recovery trajectory (43.0%).
Secondary school–aged children
Only one study focused exclusively on secondary school–aged children (12 to 16 years of age at baseline). Fan et al. (2015) reported that children fell into trajectories as follows: 10.5% were chronic; 20.0% recovery; 65.3% resilience (the largest trajectory group in this study); and 4.2% delayed.
Broad age range
Five studies focused on a broad age range (i.e., not exclusively elementary or secondary school aged children). These studies found the percentage of children falling in the chronic trajectory ranged from 4.0% to 38.0%; recovery trajectory ranged from 10.0% to 27.1%; resilience trajectory ranged from 43.0% to 72.1%; and delayed trajectory ranged from 0.0% (i.e., no evidence) to 18.0%. All five studies found the resilience trajectory to be the largest group.
Aim 2: Evaluate Risk and Protective Factors That Distinguished PTSS Trajectories
There was limited evidence for a delayed trajectory across studies. Thus, we focused on factors that distinguished likelihood of falling in chronic, recovery, and resilience trajectories.
Factors distinguishing between the chronic and resilience trajectories
Various factors distinguished the chronic trajectory from the resilience trajectory, including age, gender, severe PTSD at Time 1, general anxiety symptoms, numerous exposure and recovery stressors, less social support, less positive coping, and more negative coping (see Table 2). Of note, female gender was identified by four studies to be a risk factor that increased the likelihood of falling into the chronic rather than the resilience trajectory. Additionally, community/neighborhood violence was identified by two studies to be a risk factor that increased the likelihood of falling into the chronic rather than the resilience trajectory. Interestingly, findings regarding age were conflicting: Kronenberg et al. (2010) found that younger children had higher odds of falling into the chronic trajectory; however, Osofsky et al. (2015) reported that older adolescents had higher odds of falling into the chronic trajectory compared to the resilience trajectory.
Table 2.
Across Studies, Risk Factors That Significantly Increased Likelihood of Children Falling Into More Severe Posttraumatic Stress Symptom (PTSS) Trajectories versus a Comparison Trajectory
| Likelihood of a falling into a more severe trajectory versus a comparison trajectory
|
|||
|---|---|---|---|
| Domain | Chronic vs. Resilience | Recovery vs. Resilience | Chronic vs. Recovery |
| Child characteristics | Younger age (Kronenberg et al., 2010)a | Older age (Osofsky et al., 2015)c | Younger age (Kronenberg et al., 2010) |
| Older age (Osofsky et al., 2015) | Female gender (Fan et al., 2015; La Greca et al., 2013b; Kronenberg et al., 2010; Osofsky et al., 2015) | Older age (Osofsky et al., 2015) | |
| Female gender (Fan et al., 2015; La Greca et al., 2013; Kronenberg et al., 2010; Osofsky et al., 2015) | General anxiety (La Greca et al., 2013) | Female gender (Osofsky et al., 2015) | |
| Severe baseline PTSD (McDermott et al., 2014) | Severe baseline PTSD (McDermott et al., 2014) | ||
| General anxiety (La Greca et al., 2013) | General anxiety (La Greca et al., 2013) | ||
| More than 1 child in family (Fan et al., 2015) | More than 1 child in family (Fan et al., 2015) | ||
| Exposure stressors | Loss of family members (Fan et al., 2015) | Loss of family members (Fan et al., 2015) | Loss/injury of family members (Fan et al., 2015) |
| Witnessed traumatic scenes (Fan et al., 2015) | Witnessed traumatic scenes (Fan et al., 2015) | Witnessed traumatic scenes (Fan et al., 2015) | |
| Previous loss/trauma (Kronenberg et al., 2010) | Previous loss/trauma (Kronenberg et al., 2010) | Previous loss/trauma (Kronenberg et al., 2010) | |
| Perceived life threat (McDermott et al., 2014) | High hurricane exposure (Weems & Graham, 2014) | Perceived life threat (McDermott et al., 2014) | |
| Perceived threat to parentsd (McDermott et al., 2014) | Both hurricane exposure and oil spill stress (Osofsky et al., 2015) | Perceived threat to parentsd (McDermott et al., 2014) | |
| Experience of evacuationd (McDermott et al., 2014) | Experience of evacuationd (McDermott et al., 2014) | ||
| High hurricane exposure (Weems & Graham, 2014) | High hurricane exposure (Weems & Graham, 2014) | ||
| Both hurricane exposure and oil spill stress (Osofsky et al., 2015) | Both hurricane exposure and oil spill stress (Osofsky et al., 2015) | ||
| Recovery stressors | More negative life events (Fan et al., 2015) | More negative life events (Fan et al., 2015) | More negative or intervening life events (Fan et al., 2015; La Greca et al., 2013) |
| More loss or trauma (Kronenberg et al., 2010) | More loss, trauma, or disruption events (Self-Brown et al., 2013; Kronenberg et al., 2010) | More loss or trauma (Kronenberg et al., 2010) | |
| Problems with family, school, friends, or finances (Kronenberg et al., 2010) | Problems with school or friends (Kronenberg et al., 2010) | Problems with family, school, friends, or finances (Kronenberg et al., 2010) | |
| Mental health consult (Kronenberg et al., 2010) | Exposure to community violence (Self-Brown et al., 2013) | Mental health consult (Kronenberg et al., 2010) | |
| Housing disruptione (Kronenberg et al., 2010) | Housing disruptione (Kronenberg et al., 2010) | ||
| Exposure to community or neighborhood violence (Self-Brown et al., 2013; Kronenberg et al., 2010) | Exposure to neighborhood violence (Kronenberg et al., 2010) | ||
| Social support | Low family connectedness (Kronenberg et al., 2010) | Low family connectedness (Kronenberg et al., 2010) | |
| Low social connectedness (McDermott et al., 2014) | Low social connectedness (McDermott et al., 2014) | ||
| Less social support (Self-Brown et al., 2013) | Less social support (Fan et al., 2015; La Greca et al., 2013) | ||
| Less peer support (Self-Brown et al., 2013) | |||
| Coping | Less positive coping (Fan et al., 2015) | Less positive coping (Fan et al., 2015) | Blame/anger coping (La Greca et al., 2013) |
| More negative coping (Fan et al., 2015) | More negative coping (Fan et al., 2015) | ||
| Blame/anger coping (La Greca et al., 2013) | Blame/anger coping (La Greca et al., 2013) | ||
| Avoidant coping (Weems & Graham, 2014) | |||
Note. PTSD = posttraumatic stress disorder.
Studies listed in parentheses indicate those articles in which factors were found to be significant.
Risk factors included in this table were found to be significant in the full model in La Greca et al. (2013). A follow-up analysis was performed by La Greca et al., including only disaster-related exposure and stressor variables, and additional risk factors (not included in this table) were significant in this reduced model;
Osofsky et al. (2015) and Weems and Graham (2014) did not make odds ratio comparisons between groups;
Significant predictor of falling into the chronic trajectory among primary school children in McDermott et al. (2014), but not significant among secondary school children;
Housing disruption includes living in a greater number of places postdisaster, housing others due to disaster, living in a trailer postdisaster, and endorsing housing problems or worries.
Factors distinguishing between the recovery and resilience trajectories
Multiple factors distinguished the recovery trajectory from the resilience trajectory, including older age, general anxiety symptoms, numerous exposure and recovery stressors, less positive coping, and more negative coping (see Table 2). Of note, female gender was identified by four studies to be a risk factor that increased the likelihood of falling into the recovery rather than into the resilience trajectory. Two studies found that more loss, trauma, or disruption events increased the odds of falling into the recovery rather than the resilience trajectory.
Factors distinguishing between the chronic and recovery trajectories
Various factors distinguished the chronic trajectory from the recovery trajectory, including severe PTSD at Time 1, general anxiety symptoms, use of blame and anger coping, and multiple exposure and recovery stressors (see Table 2). Two studies found that adolescents with a higher number of negative or intervening life events were more likely to fall into the chronic than the recovery trajectory. Additionally, two studies identified less social support, a third study identified low social connectedness, a fourth study identified low family connectedness, and a fifth study identified less peer support as factors that increased the likelihood of falling into the chronic rather than the recovery trajectory. Findings regarding age were again conflicting.
Discussion
This study is the first to review the literature on children’s postdisaster PTSS trajectories. Understanding how and why children differ in their responses to disasters is critical. Based on this review, it is clear that children exhibit multiple responses to disasters. Across all studies, children reported at least three trajectories of PTSS: resilience, recovery, and chronic. This represents a fundamental shift in understanding children’s responses to disasters, as research to date has largely focused on identifying children’s average response to disasters (e.g., Martin, Felton, & Cole, 2016). Given these findings, future researchers should consider using person-centered approaches to study children’s disaster responses.
Across studies, the resilience trajectory tended to be the largest trajectory group, similar to the adult literature (e.g., Orcutt, Bonanno, Hannan, & Miron, 2014). However, across studies, there was no clear consensus regarding the proportion of children falling into various trajectories. Several potential reasons may account for these differences. Studies differed in terms of analytic approach. Studies that used a priori categorization were not able to test whether a four-trajectory model was the best fit for the data. It would be interesting to reanalyze data from a priori categorization studies to see if person-centered approaches achieve the same results. However, three of the four studies that used a priori categorization approaches only included two assessment time points, limiting their ability to use different analytic approaches.
Assessment time points varied widely across studies, ranging from 12 months predisaster to 49 months postdisaster. This heterogeneity in design is common in the disaster literature, due to the challenges of conducting postdisaster research (Pfefferbaum et al., 2013). In general, studies with assessments beyond the first year postdisaster showed that the resilience trajectory was the most prevalent and the delayed trajectory the least prevalent. Further, participant age range varied by study. The studies that included participants of broad age ranges showed, in general, that the resilience trajectory was the largest trajectory group. In contrast, studies involving elementary school–aged children were divided (one showed the resilience trajectory as the most prevalent, the other showed the recovery trajectory as the most prevalent).
Studies also varied in their assessment methods. For example, Liu et al. (2011) was the only study to use the TSCC-A and found the highest prevalence of the resilience trajectory. All other studies used the PTSD-RI or a modified version of this instrument. The studies also examined a diverse set of disasters, ranging from smaller scale disasters with fewer physical impacts (e.g., Cyclone Larry, which made landfall in Australia in 2006) to large-scale disasters in socially vulnerable regions (e.g., Hurricane Katrina, which hit the Gulf Coast in the United States in 2005) and in developing nations (e.g., the 2008 Sichuan Earthquake in China). Future studies that integrate individual-level data would allow for cross-study comparisons of the role of differing assessment time points, measures used for assessment, methods used for analysis, and scale of disaster.
Another major finding from this review is that evidence was very limited for a delayed trajectory among children. In most of the studies (i.e., 62.5% of the studies), less than 5.0% of children were classified in a delayed trajectory, in contrast with the abundant evidence supporting the presence of delayed PTSS trajectories among adults after potential traumatic events (Bonanno et al., 2010; Orcutt et al., 2014). Among the three studies that found evidence for delayed PTSS trajectories (i.e., more than 5.0% of children were classified in a delayed trajectory; Liu et al., 2011; Osofsky et al., 2015; Weems & Graham, 2014), one used a priori cutoffs to identify children falling into that trajectory. It is not clear how many of the “delayed” children may have been close to clinical cutoffs at the first assessment time point. In other words, it is not clear if children truly displayed delayed symptom presentation or merely a small increase in PTSS (from subclinical to clinical levels). Among the four studies that used person-centered approaches, the more statistically rigorous approaches, two studies failed to identify a delayed trajectory. The lack of evidence for delayed trajectories suggests that very few children are likely to develop clinically significant PTSS after initial screening periods.
However, it remains an important challenge to distinguish between children who are likely to fall into a chronic versus a recovery trajectory. This review suggests that only a very small proportion of children are likely to exhibit chronic trajectories and be in need of intensive mental health services. Stratifying children based on early symptom levels may misclassify children and provide costly intensive services to children who do not need them (i.e., for children who will recover). Thus, more information is needed on risk factors that may help distinguish children likely to fall in chronic trajectories.
This review provides important novel information about factors that distinguished between the chronic and recovery trajectories across studies, including perceived life threat, perceived threat to parents, experience of evacuation, housing disruption, violence exposure, and low social support or family connectedness. These risk factors are highlighted because they specifically distinguished the chronic versus recovery trajectories as well as the chronic versus resilience trajectories, although not necessarily the recovery versus resilience trajectories. Thus, these risk factors provide new information beyond what is already known about how risk factors generally relate to elevated postdisaster distress (La Greca, Lai, Silverman, & Jaccard, 2010). Although further study is needed, the trajectory modeling approach has the potential to change our view of theory-based approaches to assessment as they apply to children affected by disasters. Based on these findings, the risk factors mentioned here may be especially important in distinguishing children likely to report chronic PTSS trajectory responses, before children experience chronic symptoms.
Further, social support was the main protective factor identified across studies. This represents a hopeful finding, as this may be a modifiable protective factor for children. This suggests that disaster preparedness and intervention programs should focus on increasing children’s social support networks. This is particularly important because disasters tend to damage social networks for children (e.g., La Greca et al., 2010).
Despite the strengths of this review, several limitations should be considered. First, risk of publication bias is always present in reviews (Torgerson, 2006). This work may be biased toward published findings where researchers were able to identify more than one trajectory. We view this possibility as unlikely, given that all of the papers reviewed found at least three PTSS trajectories among their samples. Second, the present review is subject to the limitations of the individual studies included. This study only included eight studies, and this review is limited by the limitations of those articles. The most common limitations reported throughout the included articles were (a) data that were self-reported and subject to response bias, (b) lack of generalizability due to the use of a homogenous sample, (c) incomplete information (i.e., data related to baseline or predisaster functioning, disaster exposure, and interventions), and (d) naturalistic designs limiting the ability to make causal claims. Third, retention rates for individual studies and missing data handling may have influenced results for individual studies. It is possible that certain groups (e.g., delayed and chronic) may have been more likely to drop out of studies; in this way, differential attrition rates for trajectories would influence our understanding of proportions and forms of trajectory groups. Additionally, many studies used “modern” methods to handle missing data, such as FIML and multiple imputation. However, some studies used “traditional” methods for missing data handling such as listwise deletion, which may have produced biased results (Enders, 2011). This may make growth mixture modeling more appealing in the future, as there are numerous robust strategies within mixture modeling for handling missing data. Fourth, this review searched for articles related to natural and man-made disasters. All articles in this study included exposure to natural disasters, whereas only one article also included exposure to a man-made disaster (i.e., children who were exposed to the Gulf Oil spill were also exposed to Hurricanes Katrina and Gustav, which hit the Gulf Coast in the United States in 2005 and 2008, respectively). It will be important for future studies to include examinations of children’s responses to other types of disasters. Finally, the number of studies included in the present review is small, but by reviewing these studies collectively, the sample is more heterogeneous, improving the generalizability of the results beyond what can be concluded from any single study alone. This is important, as several studies listed the use of a homogenous sample as a potential limitation.
This review serves as a useful guide for planning future research. The number of trajectories as well as risk and protective factors discussed here can be considered when developing research protocols and analytic plans. Factors found to distinguish children in different trajectories should be included in future studies. Of note, factors were heterogeneous, and findings were not consistent across studies. Further studies are needed to clarify which factors, and under what circumstances, differentiate those who develop chronic PTSS versus those who recover. Future research may use this review as a framework for determining theoretically plausible models. Based on the results discussed in the present review, more research related to PTSS trajectories of children and adolescents specifically is needed, as their patterns of response following a disaster differ from those of adults.
Individual studies of child postdisaster PTSS can be limited in terms of their sample size, period of child development examined, postdisaster time frame, frequency of assessments, risk factors studied, and sample diversity. Meta-analysis and integrative data analysis (IDA) are both methods that could be used within the child disaster field to address these issues. Meta-analysis is an important strategy that addresses some of the limitations associated with drawing conclusions from individual studies. An important future research question is whether trajectories are similar across other types of child trauma (e.g., injury, accidents). With IDA, data is integrated at the individual level from multiple studies, creating a pooled source of data that is more powerful and diverse than any one individual study (Brown et al., 2013), and which allows researchers to address questions that are difficult to test within individual studies alone. For example, pooling assessment time points would allow researchers to examine PTSS trajectories over the multiple time points covered by individual studies. This information is critical to determine the optimal time to screen for PTSS postdisaster and distinguish between children following chronic compared to recovery trajectories. This is needed to efficiently allocate resources to children at greatest risk of experiencing chronic PTSS. Additionally, IDA could be used to analyze differences in trajectories due to disaster characteristics (e.g., large vs. small-scale disasters; natural versus man-made disasters), but IDA techniques will need to consider study-level variables, such as sample selection, and how these variables might influence findings. Research in this area will also need to evaluate how study retention rates may influence findings.
In order to conduct IDA, child trauma researchers need to build repositories of data for joint examination of children’s responses to trauma. This type of data repository effort is in progress (Kassam-Adams et al., 2012). Efforts to create consortia of interested researchers in this area who meet regularly (e.g., at national conferences) are needed. Further, IDA requires some overlap of items among pooled data sets. To support these efforts, researchers should consider using consistent measures across studies.
Finally, more work is needed that focuses on communities that are particularly vulnerable to disasters. Children in developing countries are at highest risk for experiencing negative consequences after disasters (UNICEF, 2007). In the United States, some communities, such as those in the Gulf region, are highly vulnerable to disaster due to socioeconomic factors, location, and history (Emrich & Cutter, 2011). More studies are needed in these communities in order to better inform preparedness and recovery efforts.
Supplementary Material
Acknowledgments
The authors would like to sincerely thank Ryan Savage for his thoughtful editorial comments on this manuscript. Research time for the completion of this study was partially supported by National Science Foundation grant #1634234 and the National Institute of Mental Health (1R03MH113849-01).
References
- Bainter SA, Curran PJ. Advantages of integrative data analysis for developmental research. Journal of Cognition and Development. 2015;16:1–10. doi: 10.1080/15248372.2013.871721. https://doi.org/10.1080/15248372.2013.871721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker-Blease KA, Turner HA, Finkelhor D. Disasters, victimization, and children’s mental health. Child Development. 2010;81:1040–1052. doi: 10.1111/j.1467-8624.2010.01453.x. https://doi.org/10.1111/j.1467-8624.2010.01453.x. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Brewin CR, Kaniasty K, Greca AML. Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest. 2010;11(1):1–49. doi: 10.1177/1529100610387086. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD. The human capacity to thrive in the face of potential trauma. Pediatrics. 2008;121:369–375. doi: 10.1542/peds.2007-1648. https://doi.org/10.1542/peds.2007-1648. [DOI] [PubMed] [Google Scholar]
- Brown CH, Sloboda Z, Faggiano F, Teasdale B, Keller F, Burkhart G, Perrino T. Methods for synthesizing findings on moderation effects across multiple randomized trials. Prevention Science. 2013;14:144–156. doi: 10.1007/s11121-011-0207-8. https://doi.org/10.1007/s11121-011-0207-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, Obeidat K, Losardo D. Twelve frequently asked questions about growth curve modeling. Journal of Cognition and Development. 2010;11:121–136. doi: 10.1080/15248371003699969. https://doi.org/10.1080/15248371003699969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emrich CT, Cutter SL. Social vulnerability to climate-sensitive hazards in the southern United States. Weather, Climate, and Society. 2011;3:193–208. https://doi.org/10.1175/2011WCAS1092.1. [Google Scholar]
- Enders CK. Analyzing longitudinal data with missing values. Rehabilitation Psychology. 2011;56:267–288. doi: 10.1037/a0025579. https://doi.org/10.1037/a0025579. [DOI] [PubMed] [Google Scholar]
- Fan F, Long K, Zhou Y, Zheng Y, Liu X. Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychological Medicine. 2015;45:2885–2896. doi: 10.1017/S0033291715000884. https://doi.org/10.1017/S0033291715000884. [DOI] [PubMed] [Google Scholar]
- Fothergill A, Peek L. Children of Katrina. Austin: University of Texas Press; 2015. [Google Scholar]
- Furr JM, Comer JS, Edmunds JM, Kendall PC. Disasters and youth: A meta-analytic examination of posttraumatic stress. Journal of Consulting and Clinical Psychology. 2010;78:765–780. doi: 10.1037/a0021482. https://doi.org/10.1037/a0021482. [DOI] [PubMed] [Google Scholar]
- Hadi F, Lai BS, Llabre MM. Life outcomes influenced by war-related experiences during the Gulf crisis. Anxiety, Stress, and Coping. 2014;27:156–175. doi: 10.1080/10615806.2013.832219. https://doi.org/10.1080/10615806.2013.832219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassam-Adams N, Palmieri PA, Rork K, Delahanty DL, Kenardy J, McGrath C. Acute stress symptoms in children: Results from an international data archive. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:812–820. doi: 10.1016/j.jaac.2012.05.013. https://doi.org/10.1016/j.jaac.2012.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 4. New York, NY: Guilford Press; 2016. [Google Scholar]
- Kronenberg ME, Hansel TC, Brennan AM, Osofsky HJ, Osofsky JD, Lawrason B. Children of Katrina: Lessons learned about postdisaster symptoms and recovery patterns. Child Development. 2010;81:1241–1259. doi: 10.1111/j.1467-8624.2010.01465.x. https://doi.org/10.1111/j.1467-8624.2010.01465.x. [DOI] [PubMed] [Google Scholar]
- Kucukoglu S, Yildirim N, Dursun OB. Posttraumatic stress symptoms seen in children within the 3-month period after the Van earthquake in Turkey. International Journal of Nursing Practice. 2015;21:542–549. doi: 10.1111/ijn.12305. https://doi.org/10.1111/ijn.12305. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Lai BS, Llabre MM, Silverman WK, Vernberg EM, Prinstein MJ. Children’s postdisaster trajectories of PTS symptoms: Predicting chronic distress. Child and Youth Care Forum. 2013;42:351–369. doi: 10.1007/s10566-013-9206-1. https://doi.org/10.1007/s10566-013-9206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca AM, Lai BS, Silverman WK, Jaccard J. Hurricane-related exposure experiences and stressors, other life events, and social support: Concurrent and prospective impact on children’s persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Psychology. 2010;78:794–805. doi: 10.1037/a0020775. https://doi.org/10.1037/a0020775. [DOI] [PubMed] [Google Scholar]
- Liu M, Li W, Zhanbiao S, Zhen Z, Kan Z, Jianhua S. Mental health problems among children one year after Sichuan Earthquake in China: A follow-up study. Plos ONE. 2011;6(2):e14706. doi: 10.1371/journal.pone.0014706. https://doi.org/10.1371/jounal.pone.0014706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin NC, Felton JW, Cole DA. Predictors of youths’ post-traumatic stress symptoms following a natural disaster: The 2010 Nashville, Tennessee, flood. Journal of Clinical Child and Adolescent Psychology. 2016;45:335–347. doi: 10.1080/15374416.2014.982279. https://doi.org/10.1080/15374416.2014.982279. [DOI] [PubMed] [Google Scholar]
- Masten AS, Obradovic J. Disaster preparation and recovery: Lessons from research on resilience in human development. Ecology and Society. 2008;13(1):9. Retrieved from http://www.ecologyandsociety.org/vol13/iss1/art9/ [Google Scholar]
- McDermott B, Cobham V, Berry H, Kim B. Correlates of persisting posttraumatic symptoms in children and adolescents 18 months after a cyclone disaster. Australian and New Zealand Journal of Psychiatry. 2014;48:80–86. doi: 10.1177/0004867413500349. https://doi.org/10.1177/0004867413500349. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. https://doi.org/10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychological Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Orcutt HK, Bonanno GA, Hannan SM, Miron LR. Prospective trajectories of posttraumatic stress in college women following a campus mass shooting. Journal of Traumatic Stress. 2014;27:249–256. doi: 10.1002/jts.21914. https://doi.org/10.1002/jts.21914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osofsky JD, Osofsky HJ, Weems CF, King LS, Hansel TC. Trajectories of post-traumatic stress disorder symptoms among youth exposed to both natural and technological disasters. Journal of Child Psychology and Psychiatry. 2015;56:1347–1355. doi: 10.1111/jcpp.12420. https://doi.org/10.1111/jcpp.12420. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B, North CS. Child disaster mental health services: A review of the system of care, assessment approaches, and evidence base for intervention. Current Psychiatry Reports. 2016;18:5. doi: 10.1007/s11920-015-0647-0. https://doi.org/10.1007/s11920-015-0647-0. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B, Weems C, Scott B, Nitie´ma P, Noffsinger M, Pfefferbaum R, Chakraburtty A. Research methods in child disaster studies: A review of studies generated by the September 11, 2001, terrorist attacks; the 2004 Indian Ocean tsunami; and Hurricane Katrina. Child and Youth Care Forum. 2013;42:285–337. doi: 10.1007/s10566-013-9211-4. https://doi.org/10.1007/s10566-013-0211-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Self-Brown S, Lai BS, Thompson JE, McGill T, Kelley ML. Posttraumatic stress disorder symptom trajectories in Hurricane Katrina affected youth. Journal of Affective Disorders. 2013;147:198–204. doi: 10.1016/j.jad.2012.11.002. https://doi.org/10.1016/j.jad.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui KA. Heuristics for sample size determination in multivari-ate statistical techniques. World Applied Sciences Journal. 2013;27:285–287. https://doi.org/10.5829/idosi.wasj.2013.27.02.889. [Google Scholar]
- Torgerson CJ. Publication bias: The Achilles’ heel of systematic reviews? British Journal of Educational Studies. 2006;54:89–102. https://doi.org/10.1111/j.1467-8527.2006.00332.x. [Google Scholar]
- UNICEF. Climate change and children. New York, NY: United Nations Children’s Fund; 2007. [Google Scholar]
- United Nations Office for Disaster Risk Reduction (UNISDR) UNISDR says the young are the largest group affected by disasters. Brussels, Belgium: Author; 2011. Retrieved from http://www.unisdr.org/archive/22742. [Google Scholar]
- United Nations Office for Disaster Risk Reduction (UNISDR) Comprehensive school safety. Brussels, Belgium: Author; 2015. [Google Scholar]
- U.S. Global Change Research Program. The impacts of climate change on human health in the United States: A scientific assessment. Washington, DC: Author; 2016. [Google Scholar]
- Weems CF, Graham RA. Resilience and trajectories of post-traumatic stress among youth exposed to disaster. Journal of Child and Adolescent Psychopharmacology. 2014;24:2–8. doi: 10.1089/cap.2013.0042. https://doi.org/10.1089/cap.2013.0042. [DOI] [PubMed] [Google Scholar]
- Wizemann T, Reeve M, Altevogt B. Preparedness, response, and recovery considerations for children and families. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.