Abstract
We report a case of delayed recovery from general anesthesia following a routine parathyroidectomy. Our objectives are to describe the process of establishing a differential diagnosis and subsequent management of a patient presenting with atypical neurological signs from an unknown etiology and to increase awareness about the potential for serotonin syndrome and neurotoxicity due to known interactions between methylene blue and selective serotoninnoradrenaline re-uptake inhibitors. ICU management of Serotonin Toxicity is briefly described.
Keywords: serotonin syndrome, neurotoxicity, general anesthesia
Introduction
Methylthioninium chloride (methylene blue; C16H18N3SCl), a chemical dye with numerous industrial applications, is widely used to stain tissues to aid localization of the abnormal parathyroid glands on the basis that it is cost effective and allows rapid visualization [1]. As a guanylatecyclase inhibitor it reduces nitric oxide production in septic shock. It has been used for the treatment of methhemoglobinaemia, malaria, cancer, as an antidote for cyanide poisoning, among others. A systematic review published in the British Journal of Surgery (2012) found that its effectiveness as a peri-operative localization technique has yet to be established [2]. Moreover, neurotoxicity was reported in 25 patients taking serotonergic medication from 39 observational studies. Methylene blue is a potent MAO inhibitor of both the subtypes, A and B; inhibiting MAO-B at higher doses, and it is known to precipitate serotonin toxicity in patients taking selective serotonin-noradrenaline re-uptake inhibitors (SSRI/SnRI) [3].
Clinical presentation
A 58 year-old obese female (BMI 34) undergoing an elective parathyroidectomy had a 500 mg infusion of 5mg/kg of methylene blue pre-operatively. Her background included severe depression and suicidal tendencies for which she was receiving high dose venlafaxine, 225 mg MR, and nitrazepam 10 mg. She was a controlled hypertensive on Ramipril. She had no other significant co-morbidities and had never had any operations or general anaesthetics.
Due to severe in-hospital anxiety she received anxiolytic premedication with benzodiazepines (Temazepam 10 mg). Throughout induction and intra-operatively there were no complications. She received fentanyl 100 mcg, morphine 10 mg for analgesia, Rocuronium 50 mg to facilitate intubation and the anti-emetic ondansetron 4 mg.
Postoperatively she remained intubated due to delayed initiation of spontaneous breathing and deep sedation, despite adequate reversal of muscular blockade. Subsequently she exhibited decreased responsiveness, agitation, dystonia and abnormal eye movements, followed by tachycardia, sweaty, pyrexial and had rigidity of her neck and limbs. Blood biochemistry was essentially normal except for an abnormal thyroid profile: T3 was 12.4 mmol/l (3.5-6.5); T4 was 17.9 mmol/l (14-19).
After administration of flumazenil (400 micrograms) and naloxone (200 micrograms) in incremental doses, and after showing a slight improvement in her respiratory efforts and level of consciousness, a trial of extubation was attempted. The patient remained deeply unresponsive and after an arterial blood gases sample revealed a worsening hypercapnia, the patient was reintubated. The ICU physicians were alerted and a prolonged intubation and ventilation support was advised until a diagnosis was reached.
A number of diagnoses were considered at the time. After a second trial of extubation, 8 hours post-induction, she continued to demonstrate atypical eye movements, dystonia and inducible clonus; all signs that classically fit into the Hunter Serotonin Criteria for serotonin syndrome. A laryngeal mask airway was inserted; sedation with low-dose Propofol and supportive ventilation was continued.
Finally, 10-12 hrs after the operation finished, the laryngeal mask was successfully removed and the patient admitted to the surgical HDU for overnight observation. At that point she had a Glasgow trauma Score [GCS] of 9. She made a complete neurological recovery and was discharged back to the Mental Health Unit later in the day.
Discussion
On the basis of the history, clinical presentation and blood biochemistry three main differentials diagnosis were considered: malignant hyperthermia, thyroid storm and drug interaction.
Malignant hyperthermia
Although extremely rare, but often lethal, it was considered on the basis of her clinical presentation: first anaesthetics, raised temperature, tachycardia, hypertension, hypercapnia, triggering agent (sevoflurane) and neck and limb rigidity.
Thyroid storm
It was considered due to the clinical signs, thyroid manipulation and raised T3/T4 profile. There are reports in the literature of thyroid storm after thyroid manipulation or trauma.
Drug interaction
We focused on methylene blue and venlafaxine, on the basis of known published interactions, [3] but the vagueness and extent of the symptoms made it difficult to attribute the diagnosis to direct drug interaction.
As the case progressed and the signs and symptoms abated we ruled out Malignant Hyperthermia and a thyroid storm was considered extremely improbable as the causal event. In the absence of an accurate diagnosis, treatment was supportive and a searched for a more coherent diagnosis was undertaken.
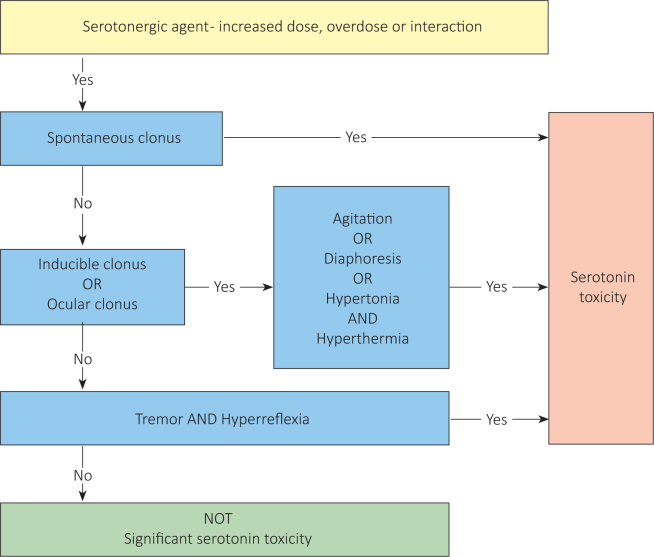
The diagnosis of serotonin toxicity was only considered much later after the patient’s admission to the ICU. This was based on a literature search of the signs that classically fit into the Hunter Serotonin Criteria for serotonin toxicity and published reports in the literature of interactions between methylene blue and SSRI/ SnRI (table 1, figure 1).
Table 1.
Hunter serotonin toxicity criteria — decision rules [4]
| Hunter Serotonin Toxicity Criteria: Decision Rules |
|---|
| In the presence of a serotonergic agent: |
| 1 IF (spontaneous clonus = yes) THEN serotonin toxicity = YES |
| 2 ELSE IF (inducible clonus = yes) AND [(agitation = yes) OR (diaphoresis = yes)] THEN serotonic toxicity = YES |
| 3 ELSE IF (ocular clonus = yes) AND [(agitation = yes) OR (diaphoresis = yes)] THEN serotonic toxicity = YES |
| 4 ELSE IF (tremor = yes) AND (hyperreflexia = yes) THEN serotonin toxicity = YES |
| 5 ELSE IF (hypertonic = yes) AND (temperature>380C) AND [(ocular clonus = yes) OR (inducible clonus = yes)] then serotonin toxicity = YES |
| 6 ELSE serotonin toxicity = NO |
Figure 1.
A flow diagram based on the Hunter Serotonin Toxicity Criteria
A classical triad of autonomic and neuromuscular instability and altered mental status in a patient taking SSRI /SnRI and receiving methylene blue points to the diagnosis of serotonin toxicity. The 30th report of the American Association of Poison Control Centre’s National poison database system published in 2013 showed that SSRI were responsible for 47,115 of the 2.3 million toxic exposures, with a 3% death rate [5].
A case report and literature review published in June 2013 in the American Association of Nurse Anesthetists identified 31 cases of methylene blue-associated encephalopathy post parathyroidectomy from 1999 to 2013 of which 84% of cases involved women [6]. These patients were being treated with SSRI/SnRI and received methylene blue in doses ranging between 1.75-7.5 mg/kg.
In 2007 Khan et al reported a case of post-operative confusion, agitation and altered mental status in a patient who received 5mg/kg methylene blue for a parathyroidectomy [7]. This patient was being treated with clomipramine for depression, had a very similar post-operative presentation as our patient, normal biochemistry and deranged thyroid functions, and made a complete mental recovery to pre-operative level in 2 days. Johnson et al [2012] describes the clinical presentation of serotonin syndrome precipitated by methylene blue in a patient taking SSRI after routine parathyroidectomy. This patient had a three week stay in ICU and made a complete neurological recovery, myoclonus persisting for two weeks [8].
The Medical Journal of Australia published a case of serotonin toxicity reported by Khavandi et al [2008]. In this case, the antidepressant was Citalopram [9].
Ng [2008] published a case report followed by a literature review [10] which listed seven cases of postoperative complications after methylene blue for parathyroidectomy. All seven patients exhibited symptoms fulfilling the Serotonin Toxicity Criteria, five were already on SSRI/SnRI and one patient received the tricyclic antidepressant clomipramine. Definitive diagnosis was never made in any of these seven patients and the authors concluded that the diagnosis of serotonin syndrome is largely clinical based on the triad of mental changes, autonomic and neuromuscular instability and reached after excluding all other common differentials diagnosis.
One of the main distinguishing features of serotonin toxicity is ocular clonus, and in particular ‘ping-pong’ alternating gaze, both seen in our patient. Rotational nystagmus, dilated pupils, jerky movements, agitation and fluctuating GCS in a patient on fluoxetine for anxiety and depression, who received 7.5 mg/kg of methylene blue, was reported by Martindale et al [11]. This patient made a neurological recovery after two days. Isbister in 2007 listed and simplified the process of recognizing, diagnosing and managing a patient with serotonin toxicity [12].
According to the literature, the neurotoxicity is dose related, more common at doses greater than 4 mg/kg [4] and usually self-resolving, with the patient making a complete recovery in two to three days.
The UK National Poisons Centre recommends that the dose of intravenous methylene blue should not exceed more than 4 mg/kg, and should be avoided in patients known to be on SSRI/SnRI [11].
A drug and safety update issued by the MHRA [2009] advised that methylene blue should not be administered in high intravenous doses to patients taking serotonergic medications. Based on twenty seven reported cases of neurotoxicity [13] it is recommended that if its use is unavoidable then the lowest possible dose should be administered and the patient should be monitored for neurotoxicity for four hours postadministration. However, the lowest possible dose is not specified.
On 26/07/2011, the Food and Drug Administration of the US issued a safety communication (updated on 21/10/2011) to healthcare professionals and the general public about the potential for interactions between methylene blue and serotonergic psychiatric medications on the basis of adverse events(lethargy, confusion, delirium, agitation, aggression, obtundation, and coma. These symptoms were frequently accompanied by neurological symptoms, such as myoclonus, expressive aphasia, hypertonia, and seizures, or autonomic symptoms, such as pyrexia and elevated blood pressure being reported on their Adverse Event Reporting System [14]. A similar alert (Identification number RA-170002469) was issued by Health Canada in a notice to all hospitals on 16 February 2011 [15].
ICU management of serotonin toxicity
The management of these cases is largely supportive, more so when a definite diagnosis is not reached at an early stage. The clinical features of serotonin toxicity are highly variable, reflecting the spectrum of toxicity. A doctor attending an A&E department or an ICU should be highly suspicious of serotonin toxicity especially when concurrent high doses of SSRI/SnRI are taken and possible overdose or pharmacological interactions may exist.
Depending on the context, the differential diagnosis includes neuroleptic malignant syndrome, dystonic reactions, encephalitis, tetanus, thyroid storm and sepsis; but as we have seen in our case malignant hyperthermia was a consideration well worth it in a peri-operative case.
A number of drugs used in anaesthesia have been regarded as ‘serotoninergic’, for example, ondansetron, entanyl, tramadol or pethidine. Over the counter drugs, including among others, St John’s wort or ginseng, may increase the level of serotonin, as well as poisoning by anticholinergic drugs, amphetamines, cocaine, lithium, MAOIs, salicylates and strychnine.
Based on our literature search, the majority of cases are self-limiting and with supportive treatment, range from hours to a few days. Discontinuation of SSRI/ SnRI or any serotoninergic drug is principal, airway and ventilator support, cardiovascular stability, adequate rehydration and renal function monitoring, temperature control and neurological observation should be the basis of ICU management. Hyperthermia, rhabdomyolysis, renal failure or disseminated intravascular coagulation have been reported and therefore the syndrome can be fatal. A number of serotonin antagonist have been proposed, ciproheptadin being the most promising one. An initial oral doses of 4-8 mg, increased up to 16 mg has been suggested, but should be discontinued if no response is obtained [16].
Conclusions
Though widely known, published and reviewed, methylene blue interactions with SSRI/SnRI and serotonin toxicity is still a relatively unknown entity. While methylene blue continues to be used as a visualization aid, caution and vigilance needs to be exercised by anesthetists when treating patients on anti-depressants.
Anaesthetic departments need to work with the hospital pharmacy to put in place alerts and protocols regarding the concomitant use of methylene blue with SSRI/SnRI so as to reduce the occurrence of neurotoxic complications. As the use of SSRI/SnRI are widespread and the potential interaction still ill-defined, A&E and ICU departments should consider serotonin toxicity in their differential diagnosis in cases similar to ours.
References
- 1.Kuriloff DB, Sanborn KV.. Rapid intraoperative localization of parathyroid glands using methylene blue infusion. Otolaryngology-Head Neck Surgery. 2004(131):616–22. doi: 10.1016/j.otohns.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 2.Patel HP, Chadwick DR, Harrison BJ. Balasubramanian SP Systematic review of intravenous methylene blue in parathyroid surgery. Br J Surg. 2012(99):1345–52. doi: 10.1002/bjs.8814. [DOI] [PubMed] [Google Scholar]
- 3.Ramsay RR, Dunford C, Gilman PK.. Methylene blue and serotonin toxicity: inhibition of monoamine oxidase A (MAO A) confirms a theoretical prediction. Br J Pharmacol. 2007(152):946–51. doi: 10.1038/sj.bjp.0707430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunkley EJ, Isbister GK, Sibbritt D. et al. The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic rules for serotonin toxicity. QJM. 2003;96:635. doi: 10.1093/qjmed/hcg109. [DOI] [PubMed] [Google Scholar]
- 5.Mowry JB, Spyker DA, Cantilena LR Jr, Bailey JE, Ford M.. Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th Annual Report. ClinToxicol (Phila). 2012;2013(51):949–1229. doi: 10.3109/15563650.2013.863906. [DOI] [PubMed] [Google Scholar]
- 6.Shopes E, Wayne Gerard W, Baughman J.. Methylene blue encephalopathy: a case report and review of published cases. AANA Journal. 2013(81):215–21. [PubMed] [Google Scholar]
- 7.Khan MAS, North AP, Chadwick DR.. Prolonged Postoperative Altered Mental Status After Methylene Blue Infusion During Parathyroidectomy: A Case Report and Review of the Literature. Ann R Coll Surg Engl. 2007;89:W9–W11. doi: 10.1308/147870807X160434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson N, Soar J, Robinson S.. Concurrent administration of methylene blue and a selective serotonin reuptake inhibitor: a recipe for serotonin syndrome. Journal of the Intensive Care Society. 2012(13):256–8. [Google Scholar]
- 9.Khavandi A, Whitaker J, Gonna H.. Serotonin toxicity precipitated by concomitant use of citalopram and methylene blue. Med J Aust. 2008(189):534–5. doi: 10.5694/j.1326-5377.2008.tb02168.x. [DOI] [PubMed] [Google Scholar]
- 10.Ng BKW, Cameron AJD.. Serotonin syndrome following methylene blue infusion during parathyroidectomy: a case report and literature review. Can J Anaesthesiol. 2008(55):1–5. doi: 10.1007/BF03017595. [DOI] [PubMed] [Google Scholar]
- 11.Martindale SJ, Stedeford JC.. Neurological sequelae following methylene blue injection for parathyroidectomy. Anaesthesia. 2003(58):1041–2. doi: 10.1046/j.1365-2044.2003.03415_23.x. [DOI] [PubMed] [Google Scholar]
- 12.Isbister GK, Buckley NA, Whyte IM.. Serotonin toxicity: a practical approach to diagnosis and treatment. Med J Aust. 2007(187):361–5. doi: 10.5694/j.1326-5377.2007.tb01282.x. [DOI] [PubMed] [Google Scholar]
- 13.MHRA Drug Safety Update. 2009;2(9):3. [Google Scholar]
- 14.Methylene blue: Drug Safety Communication - Serious CNS Reactions possible when given to patients taking certain psychiatric medication. July 2011; (updated October 2011) [Google Scholar]
- 15.Lead Directorate: Marketed Health Product Directorate. Methylene blue injectable in combination with serotonin reuptake inhibitors-Association with serotonin toxicity-Notice to Hospitals. 2011 http://healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2011/14648a-eng.php Available at. [Google Scholar]
- 16.Hall M, Buckley N.. Serotonin syndrome. Australian Prescriber. 2003(26):62–3. [Google Scholar]