Abstract.
Given limited data on norovirus vaccine acceptance, we performed an exploratory survey in a rural Guatemalan community on knowledge, interest, and willingness to pay (WTP) for a norovirus vaccine. Cluster-randomized households with children aged 6 weeks to 17 years were enrolled into one of two norovirus surveillance studies: 1) a prospective cohort (N = 207 households) and 2) two separate, community-based, cross-sectional surveys (N = 420 households). After completion of the surveillance study, vaccine surveys were completed by 564 (90%) of 627 households. Most households correctly answered questions regarding norovirus symptoms and transmission; 97% indicated interest in a hypothetical norovirus vaccine. Households with higher education had greater WTP for a vaccine (prevalence ratios = 2.2, 95% confidence interval: 1.2–3.1) and households with lower WTP were more likely to use pharmacies, the Ministry of Health, and radios for health care and information. These results suggest that a future norovirus vaccination program could be acceptable and feasible even in rural areas.
Noroviruses cause an estimated 18% of acute gastroenteritis (AGE) globally and more than 200,000 deaths each year, with children under 5 years bearing the greatest disease burden.1,2 An effective norovirus vaccine has the potential to greatly reduce AGE-associated morbidity and mortality. Currently, there are several norovirus vaccines in development, with the most advanced demonstrating safety, immunogenicity, and efficacy against severe diseases in Phase 1 trials.3,4 As the scientific community advances toward an effective norovirus vaccine, it is essential to characterize acceptability and willingness to pay (WTP) for such a vaccine, especially in low- and middle-income countries (LMICs), where it is most needed.
Vaccine hesitancy appears to be an increasing problem in LMICs and can be categorized into contextual (i.e., political and cultural barriers) individual/group (i.e., risk/benefit and knowledge), and vaccine-specific (i.e., schedule and cost) influences.5–7 Although several studies have identified risk factors for vaccine hesitancy in general, data on vaccines against norovirus and other diarrheal diseases are limited.6,8–11 Like many LMICs, Guatemala has a high burden of enteric diseases, including norovirus.12,13 In anticipation of forthcoming vaccines, we characterized norovirus vaccine attitudes in this population and explored associations between sociodemographic factors, vaccine hesitancy, and WTP.
A cross-sectional vaccine knowledge and attitude survey was administered to 627 households who had recently participated in a norovirus surveillance study, which was performed among 13 communities within a 200-km2 catchment area along the coastal lowlands of southwest Guatemala. The people living in this region suffer from high levels of food insecurity, poverty, low access to health care, and high levels of diarrheal and respiratory disease.12,14
Households with children aged 6 weeks to 17 years were randomly selected and enrolled in one of two surveillance programs: 1) a prospective participatory surveillance system (PSS) conducted from April 2015 to September 2016 in which, after enrollment and baseline sampling, children were monitored for AGE using a weekly smartphone-based symptom diary, with diagnostic testing performed for self-reported AGE (norovirus); or 2) two separate rapid active cross-sectional sampling (RAS) surveys conducted in October–November 2015 and January–February 2016 in which children in randomly selected households were screened for AGE symptoms in the previous week and tested for AGE regardless of a symptom report.12 Randomization and enrollment of the households were conducted using a two-stage cluster sampling strategy in which 30 clusters of seven households each were enrolled in the PSS cohort and each of the two RAS cycles separately, as previously described.12 Households in both arms received an information brochure about norovirus at the time of enrollment. The vaccine knowledge and attitude survey was administered at the conclusion of this study, in September 2016.
A 66-question vaccine knowledge and attitude survey (“Survey”) was administered to the heads of households via in-person interview by local study nurses. The survey was adapted, in part, from a previously validated World Health Organization Strategic Advisory Group of Experts on Vaccine Hesitancy Report and a survey assessing knowledge and attitudes about dengue virus and vaccine hesitancy.5,15 The survey collected household demographic information and asked about vaccine hesitancy, knowledge of norovirus, acceptability of a norovirus vaccine, and participant WTP for a hypothetical norovirus vaccine.
Demographic variables and survey responses were compared between the PSS and RAS cohorts using χ2 tests. Logistic regression was used to explore associations between sociodemographic factors (independent variables), comparing those who indicated WTP > 25 Quetzales (∼$3.40 US) for a potential norovirus vaccine versus WTP < 25 Quetzales. Logistic regression was also used to explore associations between independent variables and interest in a norovirus vaccine. A survival analysis was performed that examined WTP for a vaccine as the price level increased.16,17 No variables met the criteria to be considered a confounder. All analyses were conducted using SAS version 9.4 (Cary, NC). The study was approved by the Colorado Multiple Institutional Review Board and the Universidad del Valle de Guatemala Institutional Review Board.
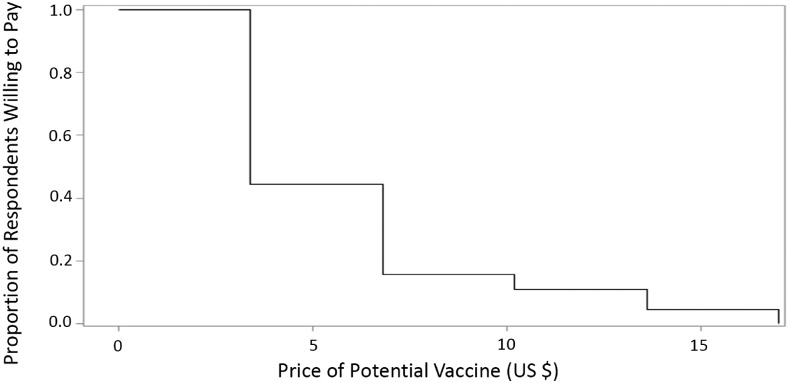
The surveys were completed by 564 (90%) of 627 households. Sociodemographic variables were similar between the PSS and RAS households, and most households demonstrated an appropriate understanding of norovirus transmission and symptoms regardless of their exposure to study personnel (Table 1). Most respondents (84%) reported receiving health information from the Ministry of Health (MOH), 65 (12%) stated a household member had been recently hospitalized with diarrhea, and 544 (97%) indicated interest in a norovirus vaccine. Of those interested in a vaccine, more than half (54%) were willing to pay $0–$3.40 for the vaccine and nearly 30% were willing to pay $3.40–$6.80 (Table 1, Figure 1).
Table 1.
Norovirus and vaccine hesitancy survey participant characteristics and responses in southwest Guatemala, September 2016
| Survey question | Response | PSS, n (%) | RAS, n (%) | Total, n (%) | P Value |
|---|---|---|---|---|---|
| 179 (32) | 385 (69) | 564 | |||
| Demographics | |||||
| Mother’s education | None | 33 (18) | 60 (16) | 93 (17) | 0.66 |
| Primary | 114 (64) | 252 (66) | 366 (65) | ||
| Secondary/university | 32 (18) | 73 (19) | 105 (19) | ||
| # Children per HH | 1 | 56 (31) | 87 (23) | 143 (25) | 0.26 |
| 2 | 46 (26) | 130 (34) | 176 (31) | ||
| 3 | 38 (21) | 78 (20) | 116 (21) | ||
| ≥ 4 | 39 (22) | 90 (23) | 129 (23) | ||
| # Adults per HH | 1 | 15 (8) | 23 (6) | 38 (7) | 0.35 |
| 2 | 93 (52) | 178 (46) | 271 (48) | ||
| 3 | 35 (20) | 74 (19) | 109 (19) | ||
| ≥ 4 | 36 (20) | 110 (29) | 146 (26) | ||
| Father’s employment | Self-used | 82 (46) | 173 (45) | 255 (45) | 0.16 |
| Used | 74 (41) | 142 (37) | 216 (38) | ||
| Unemployed | 9 (5) | 15 (4) | 24 (4) | ||
| Other | 14 (8) | 55 (14) | 69 (12) | ||
| Health attitude | |||||
| Where do you seek medical care?* | Public health post | 120 (67) | 249 (68) | 369 (65) | 0.92 |
| Pharmacy | 59 (32) | 126 (33) | 185 (33) | ||
| Private | 49 (27) | 102 (27) | 151 (27) | ||
| Where do your children get vaccinated? | Public health post | 176 (98) | 381 (98) | 557 (99) | 0.89 |
| Private | 1 (1) | 2 (1) | 3 (1) | ||
| Pharmacy | 1 (1) | 1 (0) | 2 (0) | ||
| Where do you obtain information about diarrhea?* | MOH | 151 (84) | 324 (84) | 475 (84) | 0.95 |
| Neighbors | 37 (21) | 134 (35) | 171 (30) | < 0.001 | |
| Radio | 27 (15) | 115 (30) | 142 (25) | < 0.001 | |
| Television | 28 (16) | 111 (29) | 139 (25) | < 0.001 | |
| Doctor | 5 (3) | 22 (6) | 27 (5) | 0.13 | |
| Newspaper | 3 (2) | 5 (1) | 8 (1) | 0.72 | |
| Internet | 0 | 1 (0) | 1 (0) | 0.51 | |
| What are trustworthy information sources regarding diarrhea?* | MOH | 155 (87) | 328 (85) | 483 (86) | 0.66 |
| Radio | 23 (13) | 74 (19) | 97 (17) | 0.06 | |
| Television | 15 (8) | 70 (18) | 85 (15) | 0.003 | |
| Neighbors | 14 (8) | 28 (7) | 42 (8) | 0.82 | |
| Doctor | 5 (3) | 16 (4) | 21 (4) | 0.43 | |
| Newspaper | 1 (1) | 6 (2) | 7 (1) | 0.32 | |
| Internet | 0 | 1 (0) | 1 (0) | 0.50 | |
| Norovirus knowledge and Vaccine acceptance | |||||
| How is norovirus transmitted? | Correct response† | 142 (79) | 327 (85) | 469 (83) | 0.07 |
| Who usually gets norovirus? | Correct response‡ | 176 (98) | 369 (96) | 545 (97) | 0.13 |
| How severe is norovirus? | Serious | 159 (88) | 325 (84) | 484 (86) | 0.16 |
| Not serious | 20 (11) | 60 (16) | 80 (14) | ||
| What are the most common symptoms of norovirus? (> 1 response possible) | Vomiting | 173 (97) | 382 (99) | 555 (98) | 0.03 |
| Diarrhea | 179 (100) | 381 (99) | 560 (99) | ||
| Fever | 101 (56) | 175 (46) | 276 (49) | ||
| Cough/Cold | 0 | 1 (< 1) | 1 (< 1) | ||
| What is the most common cause of diarrhea in children? | Parasites | 88 (49) | 200 (52) | 288 (51) | 0.54 |
| Bacteria | 53 (30) | 94 (24) | 147 (26) | ||
| Virus | 32 (18) | 78 (20) | 110 (20) | ||
| Evil eye | 2 (1) | 8 (2) | 10 (2) | ||
| Has any HH member been hospitalized from diarrhea? | Yes | 17 (10) | 48 (13) | 65 (12) | 0.30 |
| If a norovirus vaccine was available, would you want it for your child? | Yes | 168 (94) | 376 (98) | 544 (97) | 0.02 |
| No or don't know | 11 (6) | 9 (2) | 20 (4) | ||
| If the vaccine was not free, how much would you be willing to pay for it for your child?§ | $0–$3.40 | 77 (46) | 219 (58) | 296 (54) | 0.005 |
| $3.40–$6.80 | 52 (31) | 110 (29) | 162 (30) | ||
| $6.80–$10.20 | 13 (8) | 14 (4) | 27 (5) | ||
| $10.20–$13.60 | 12 (7) | 22 (6) | 34 (6) | ||
| > $13.60 | 14 (8) | 11 (3) | 25 (5) | ||
HH = household; MOH = Ministry of Health; PSS = participatory syndromic surveillance cohort; RAS = rapid active sampling group.
> 1 possible answer.
Correct response: diarrhea or vomiting.
Correct response: age < 5 years.
Corresponds to the following in Quetzales (Q): 0–$3.40 = Q0–25, $3.40–$6.80 = Q26–50, $6.80–$10.20 = Q51–75, $10.20–$13.60 = Q76–100, > $13.60 = > Q100.
Figure 1.
Willingness to pay (WTP) for a hypothetical norovirus vaccine among a rural population in southwest Guatemala, 2016. Legend: Survival analysis of price of norovirus vaccine (in U.S. dollars) and proportion of respondents willing to pay that price out-of-pocket.
Higher level of parental education was associated with increasing WTP for a potential vaccine. Compared with mothers with no formal education, mothers with a primary, secondary, and university education were increasingly likely to be in the higher WTP group (> $3.40), with prevalence ratios (PR) of 1.5 (95% confidence interval [CI] 1.0–2.0), 2.2 (95% CI 1.2–3.1), and 2.4 (95% CI 1.5–3.9), respectively. Similar but weaker findings were seen with the father’s education level, with a PR of 1.3 (95% CI 1.0–1.8), 1.7 (95% CI 1.3–2.2), and 1.8 (95% CI 1.1–3.0), respectively. Respondents with WTP > $3.40 for a potential vaccine were 1.5 (95% CI 1.1–2.1) times as likely to have purchased a vaccine in the past.
The 4% (N = 20) of respondents who were uninterested in a norovirus vaccine were 9.8 (95% CI 1.9–51.6) times as likely to believe that vaccines in general do not prevent serious disease and 4.3 (95% CI 1.4–13.7) times as likely to have refused a vaccine in the past. These households receive their information about diarrhea primarily from the MOH (80%), neighbors (40%), and television (25%). The MOH was also the most trusted source for information about diarrhea in this group (85%). Households with low WTP were more likely to be crowded, receive their medical care from a pharmacy, and obtain their health information from the radio and MOH (Table 2).
Table 2.
Characteristics of households with low willingness to pay (< $3.40 US) for a norovirus vaccine in southwest Guatemala, September 2016 (N = 296)
| Survey question | PR | 95% CI | P Value |
|---|---|---|---|
| Where do you obtain medical care? | |||
| Pharmacy | 1.22 | 1.05–1.42 | 0.01 |
| Private | 0.74 | 0.60–0.90 | 0.003 |
| Where do you learn about diarrhea? | |||
| Radio | 1.21 | 1.03–1.41 | 0.02 |
| MOH | 1.30 | 1.00–1.67 | 0.046 |
| Number of adults in house | 1.08 | 1.03–1.14 | 0.002 |
| Number of children in house | 1.07 | 1.04–1.10 | < 0.001 |
| Father’s employment: | |||
| Used | Ref | Ref | Ref |
| Self-used | 1.22 | 1.03–1.46 | 0.02 |
| Unemployed | 1.27 | 0.89–1.81 | 0.20 |
| Other | 1.16 | 0.90–1.50 | 0.25 |
CI = confidence interval; MOH = Ministry of Health; PR = prevalence ratio; Ref = reference variable.
This is the first study to evaluate population-level acceptability of a future norovirus vaccine in an LMIC. Our randomized sample of households from a rural Guatemalan community with recent participation in a norovirus surveillance study demonstrated a high level of knowledge of norovirus disease, recognition of local disease burden, and positive attitudes and acceptability of a potential norovirus vaccine, with 97% of participants expressing interest in such a vaccine. Households reported obtaining their health information from a variety of sources, most commonly the MOH and radio. Most respondents reported trust in the local MOH for health information and nearly all participants relied on local public health posts for routine immunizations.
Households with higher levels of education had greater WTP for a potential vaccine. Because the survey did not obtain household income, we cannot state whether this was due to better understanding of norovirus risk among more educated households or if education is acting as a proxy for income, which enables them to pay more and has been found to be associated with greater WTP for other vaccines.16 Other studies have shown that affordability and parental educational level were the strongest predictors of anticipated vaccine acceptance.10,11,17 Most households in our sample were willing to pay $0–$3.40 for a norovirus vaccine, with very few willing to pay greater than $6.80. A potential price point in the $3.00–$4.00 range is consistent with prices of rotavirus vaccines.18
One small group within the population demonstrated vaccine hesitancy. There were strong associations between having refused a vaccine for a child in the past and not being interested in the norovirus vaccine. This group was also less likely to believe that vaccines can prevent serious disease. Other studies have found that low socioeconomic status is associated with poor vaccine acceptance.14 Fear of adverse effects, exposure to rumors regarding a vaccine, and lack of awareness have also been associated with decreased vaccine acceptance.19 A physician’s recommendation for a vaccine and known protection against severe diseases have previously been shown to improve vaccine acceptability.20 Although more data are needed, MOH and community-level education may offer an approach to overcome hesitancy in this community.21
Strength of this study includes the high rate of survey completion in this randomized sample. The community also represents an ideal target population for a potential norovirus vaccine, given the high vaccine interest and burden of disease.12 Limitations include possible response bias due to the population’s recent participation in a norovirus surveillance study, which provided some education about norovirus. The majority (69%) of survey respondents, however, had only a single study visit up to a year before the survey was conducted, so any educational benefit was likely minimal. Also, the survey did not include questions regarding a possible vaccine schedule or differing levels of vaccine efficacy, which have been shown to be associated with WTP in other studies.17 Finally, other confounders, such as household income, were not fully explored and should be included in future studies.
In summary, this study provides insight into a rural Guatemalan population’s norovirus knowledge, interest, and WTP for a vaccine. Although a small group (4%) demonstrated vaccine hesitancy, a large majority of survey respondents expressed interest in a norovirus vaccine, with more highly educated individuals demonstrating WTP. As norovirus and other enteric vaccines advance in their preclinical development, future studies should explore vaccine acceptability in relation to the estimated efficacy, the number of doses, additional variables (household income and ethnicity), and the behaviors and determinants of the small group expressing some vaccine hesitancy.
Acknowledgments:
We thank the local study team, including Alejandra Paniagua-Avila, Alma Zacarias, Neudy Carolina Rojop, Carmen Andrea Chacon, Jeniffer Yajaira Cardenas, Edwin Estuardo Hernandez, Edgar Eduardo Barrios, Macaria Genoveva Bail, Ruth Aide Ramirez Angel, Maria Eloin Dhaenes Vivar, Dulce Maria Camas, Dora Nineth Garcia Sanchez, and Carlos Alvarez Guillen. We specially thank the families who participated in the study.
Disclaimer: This abstract was accepted for a poster presentation at the Preventive Medicine 2017 Conference in Portland, OR, May 2017.
REFERENCES
- 1.Ahmed SM, Hall AJ, Robinson AE, Verhoef L, Premkumar P, Parashar UD, Koopmans M, Lopman BA, 2014. Global prevalence of norovirus in cases of gastroenteritis: a systematic review and meta-analysis. Lancet Infect Dis 14: 725–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pires SM, Fischer-Walker CL, Lanata CF, Devleesschauwer B, Hall AJ, Kirk MD, Duarte AS, Black RE, Angulo FJ, 2015. Aetiology-specific estimates of the global and regional incidence and mortality of diarrhoeal diseases commonly transmitted through food. PLoS One 10: e0142927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lopman BA, 2015. Global Burden of Norovirus and Prospects for Vaccine Development. Atlanta, Georgia: Centers for Disease Control and Prevention. [Google Scholar]
- 4.Baehner F, Bogaerts H, Goodwin R, 2016. Vaccines against norovirus: state of the art trials in children and adults. Clin Microbiol Infect 22 (Suppl 5): S136–S139. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization , 2014. Report of the SAGE Working Group on Vaccine Hesitancy. Geneva, Switzerland: WHO. [Google Scholar]
- 6.Cobos Munoz D, Monzon Llamas L, Bosch-Capblanch X, 2015. Exposing concerns about vaccination in low- and middle-income countries: a systematic review. Int J Public Health 60: 767–780. [DOI] [PubMed] [Google Scholar]
- 7.Dube E, Gagnon D, Nickels E, Jeram S, Schuster M, 2014. Mapping vaccine hesitancy–country-specific characteristics of a global phenomenon. Vaccine 32: 6649–6654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Larson HJ, Schulz WS, Tucker JD, Smith DM, 2015. Measuring vaccine confidence: introducing a global vaccine confidence index. Plos Curr 7, 10.1371/currents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D’Ardenne KK, Darrow J, Furniss A, Chavez C, Hernandez H, Berman S, Asturias EJ, 2016. Use of rapid needs assessment as a tool to identify vaccination delays in Guatemala and Peru. Vaccine 34: 1719–1725. [DOI] [PubMed] [Google Scholar]
- 10.Merten S, Schaetti C, Manianga C, Lapika B, Hutubessy R, Chaignat CL, Weiss M, 2013. Sociocultural determinants of anticipated vaccine acceptance for acute watery diarrhea in early childhood in Katanga Province, Democratic Republic of Congo. Am J Trop Med Hyg 89: 419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sundaram N, Schaetti C, Merten S, Schindler C, Ali SM, Nyambedha EO, Lapika B, Chaignat CL, Hutubessy R, Weiss MG, 2016. Sociocultural determinants of anticipated oral cholera vaccine acceptance in three African settings: a meta-analytic approach. BMC Public Health 16: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Olson D, Lamb MM, Lopez MR, Paniagua-Avila MA, Zacarias A, Samayoa-Reyes G, Cordon-Rosales C, Asturias EJ, 2017. A rapid epidemiological tool to measure the burden of norovirus infection and disease in resource-limited settings. Open Forum Infect Dis 4: ofx049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Estevez A, et al. 2013. Prevalence and genetic diversity of norovirus among patients with acute diarrhea in Guatemala. J Med Virol 85: 1293–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asturias EJ, et al. 2016. The center for human development in Guatemala: an innovative model for global population health. Adv Pediatr 63: 357–387. [DOI] [PubMed] [Google Scholar]
- 15.Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dube E, Schuster M, MacDonald NE, Wilson R, 2015. Measuring vaccine hesitancy: the development of a survey tool. Vaccine 33: 4165–4175. [DOI] [PubMed] [Google Scholar]
- 16.Godoi IP, Santos AS, Reis EA, Lemos LL, Brandao CM, Alvares J, Acurcio FA, Godman B, Guerra AA, Jr., 2017. Consumer willingness to pay for dengue vaccine (CYD-TDV, Dengvaxia®) in Brazil: implications for future pricing considerations. Front Pharmacol 8: 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacDougall DM, Halperin BA, Langley JM, MacKinnon-Cameron D, Li L, Halperin SA; Maritime Universal Rotavirus Vaccination Program (MURVP) , 2016. Knowledge, attitudes, beliefs, and behaviors of parents and healthcare providers before and after implementation of a universal rotavirus vaccination program. Vaccine 34: 687–695. [DOI] [PubMed] [Google Scholar]
- 18.Madsen LB, Ustrup M, Fischer TK, Bygbjerg IC, Konradsen F, 2012. Reduced price on rotavirus vaccines: enough to facilitate access where most needed? Bull World Health Organ 90: 554–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kabakama S, Gallagher KE, Howard N, Mounier-Jack S, Burchett HE, Griffiths UK, Feletto M, LaMontagne DS, Watson-Jones D, 2016. Social mobilisation, consent and acceptability: a review of human papillomavirus vaccination procedures in low and middle-income countries. BMC Public Health 16: 834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morin A, Lemaitre T, Farrands A, Carrier N, Gagneur A, 2012. Maternal knowledge, attitudes and beliefs regarding gastroenteritis and rotavirus vaccine before implementing vaccination program: which key messages in light of a new immunization program? Vaccine 30: 5921–5927. [DOI] [PubMed] [Google Scholar]
- 21.Schollin Ask L, Hjern A, Lindstrand A, Olen O, Sjogren E, Blennow M, Ortqvist A, 2017. Receiving early information and trusting Swedish child health centre nurses increased parents’ willingness to vaccinate against rotavirus infections. Acta Paediatr 106: 1309–1316. [DOI] [PubMed] [Google Scholar]