Abstract
Although the association between adverse childhood experiences (ACEs) and adult mental health is becoming well established, less is known about the complex and multiple pathways through which ACEs exert their influence. Growing evidence suggests that adversity early in life conveys not only early impacts, but also augments risk of stress-related life course cascades that continue to undermine health. The present study aims to test pathways of stress proliferation and stress embodiment processes linking ACEs to mental health impairment in adulthood. Data are from the 2011 Behavioral Risk Factor Surveillance Survey, a representative sample of Washington State adults ages 18 and over (N=14,001). Structural equation modeling allowed for testing of direct and indirect effects from ACEs though low income status, experiences of adversity in adulthood, and social support. The model demonstrated that adult low income, social support and adult adversity are in fact conduits through which ACEs exert their influence on mental health impairment in adulthood. Significant indirect pathways through these variables supported hypotheses that the effect of ACEs is carried through these variables. This is among the first models that demonstrates multiple stress-related life course pathways through which early life adversity compromises adult mental health. Discussion elaborates multiple service system opportunities for intervention in early and later life to interrupt direct and indirect pathways of ACE effects.
Keywords: Adverse childhood experiences, trauma, mental health, stress proliferation, stress embodiment
Experiences of adversity in childhood, such as maltreatment and caregiver dysfunction, are well known to have life-long, often severe implications for mental health. Adverse childhood experiences (ACEs) are also relatively common, with estimates of adult population prevalence of having at least one ACE ranging from 52% to 67% (CDC, 2010; Felitti et al., 1998; Wade et al., 2016). Childhood adversity puts individuals at risk for the development of psychological disorders not only in childhood and adolescence but into adulthood (Green et al., 2010; Nurius, Green, Logan-Greene, & Borja, 2015). More specifically, individuals who have experienced ACEs are at increased risk of depression, anxiety, aggression, suicide risk (Anderson, Tiro, Price, Bender & Kaslow, 2002; Chapman et al., 2004; Turner, Finkelhor, & Ormrod, 2006), behavioral disorders (McLaughlin et al., 2012), and substance abuse (Mersky, Topitzes, & Reynolds, 2013).
Although association between adverse childhood experiences and later mental health outcomes is now established, we are in early stages of testing complex and multiple pathways through which ACEs operate. Interim stress and social support are known to be important to these pathways, yet few studies have formally tested their mediation (Font & McGuire-Jack 2016; Raposa, Hammen, Brennan, O-Callaghan & Najman, 2014). Income status is also associated with ACEs, but the role that low income plays in structuring these childhood circumstances and pathways into adulthood is less well understood (Font & McGuire-Jack, 2016). Researchers have called for integrative models to investigate relationships between multiple resource and stress pathways (Wickrama, Lee, O’Neal, & Kwon, 2014). To address these gaps, we set out to formally investigate whether adult adversity, social support, and adult income status serve as mediators. The present study integrates theories of stress embodiment and stress proliferation, and tests associated psychosocial mechanisms to create a snapshot of cumulative life course adversity effects that are catalyzed by early life exposures to ACEs (Maschi, Baier, Morrissey & Moreno, 2013; Moos, Schutte, Brennan, & Moos, 2005).
Stress is a consequence of early adversity as well as a risk factor for subsequent mental health problems, a reciprocal relationship whereby stress begets additional stress (Hazel, Hammen, Brennan, & Najman, 2008; Moos et al., 2005). Continuous exposure to stress degrades physiological resources (Wickrama et al., 2014), and is associated with increased allostatic load. Allostatic load is an index of physiological dysregulation, and prolonged exposure to stress increases stress hormone levels and hypothalamic–pituitary–adrenal (HPA) axis dysregulation (Doan, Dich, & Evans, 2014). Adults who experienced child maltreatment have been shown to have increased levels of inflammation and HPA-axis activation (Danese & McEwen, 2012), and increased inflammation biomarkers distinguish individuals who experienced child maltreatment and were depressed from those who were depressed without maltreatment (Danese et al., 2008). Toxic stress resulting from ACEs can cause physiological dysregulation that can lead to impairments in learning and the ability to adapt to new adversities, and sets the physiologic stage for stress-related health and mental health problems (Shonkoff et al., 2012).
Risky social environments mold coping styles, emotion regulation and social cognitions, all of which are involved with shaping stress responses (Hager & Runtz, 2012; McCrory, Dooley, Layte & Kenny, 2015; Raposa et al., 2014). These impairments limit success in systems such as education and the workforce as well as undermine healthy social development, increasing the risk of subsequent exposure to environmental stressors, the perception of stress, and reactions that escalate stress or complicate adaptive coping. Thus, these social environmental effects likely have biological underpinnings that can be explained through the effect of toxic stress on physiological systems.
ACEs and Low Income in Adulthood
Although an association between childhood adversity and lower income in adulthood has been documented, less has been established about the role of adult economic disadvantage in the association between ACEs and adult mental health outcomes (Font & McGuire-Jack, 2016). While income is a strong determinant of physical and mental health, its effects are largely indirect, operating through differential exposure to adverse conditions (Adler & Newman, 2002). Adverse exposures tend to co-vary, be cumulative in nature, and undermine cognitive, emotional, and behavioral development (Edwards, Holden, Felitti, & Anda, 2003; Hankin, 2005). Households with low income may struggle to provide adequate nutrition and supportive parenting, and structural constraints make health care access and choosing healthy behaviors more difficult, leading to diminished emotional resources (Wickrama, Conger & Abraham, 2005).
Moreover, the social contexts in which childhood adversity occur are rarely time-limited. Higher levels of early life adversity tend to be associated with relatively persistent structural contexts that elevate risk that children will be exposed to subsequent stressful experiences, resulting in a continuity of stress exposures (Pearlin, Schieman, Fazio, & Meersman, 2005; Raposa et al., 2014). ACEs can also influence social contexts more proximal to traumatic events, so that adversity impacts one’s school outcomes, leading to lower educational attainment, and lower socioeconomic achievement in adulthood (Raposa et al., 2014). Economic disadvantage is also a factor in influencing the quality and depth of one’s social network, as well as social cohesion in the broader environment (Adler & Newman, 2002). Previous studies have documented the detrimental effects that ACEs have on adult socioeconomic achievement (Font & McGuire-Jack, 2016).
Adult Adversity
In order to better understand the effects of early life adversity, more attention to processes of stress accumulation is needed. As noted, the effect of childhood adversity is not limited to childhood, but leads to accumulation of stressors across development, in a chain reaction of adversity (Shira, 2012; Turner & Butler, 2003). Exposure to adversity may result in a pessimistic explanatory style and cognitive attributional biases which lead to depression vulnerability (Rutter, Kim-Cohen & Maughan, 2006). Growing up in negative social environments likely influences the selection of similar social environments in adulthood (Raposa et al., 2014). Adults with psychopathology have higher levels of ACEs as well as more high-risk behaviors, substance use disorders, exposure to trauma in adulthood, psychiatric problems, medical service utilization, incarceration and homelessness (Lu, Mueser, Rosenberg, & Jankowski, 2008). In addition, these experiences of stress proliferation are known to operate through biological pathways by increasing HPA-axis reactivity resulting in neurobiological dysregulation (Juster, McEwen & Lupien, 2010).
Social Support
Significant evidence supports the critical role that social support plays in protecting against mental health problems and in buffering stress exposure (Thoits, 2011). Social support may act to buffer stress by providing coping assistance and emotional sustenance (Thoits, 2011). Social contexts in which ACEs occur are often associated with poor systems of social support. This may be because experiences of adversity implicate parents or caregivers, or due to loss of support related to the adversity itself; i.e., parental death or separation, relocation etc. (Turner & Butler, 2003). ACEs are also associated with unhealthy lifestyles characterized by more risk-taking behaviors, including substance abuse and risky sexual behavior, which in turn, are associated with worse social support networks (Shonkoff et al., 2012). Those with higher levels of ACEs may then become socially isolated as their ability to sustain relationships might be affected by their distress. Thus, experiences of childhood adversity impact individuals’ ability to build social support networks, and directly negatively impact the social context making positive social support relationships more difficult to find and sustain (Turner & Butler, 2003).
The present study aims to test direct and indirect pathways through which ACEs transmit their influence over the life course to impair mental health. We draw upon prior work specifying stress embodiment and stress proliferation as processes through which early adversity fosters trajectories of continued risk. We used structural equation modeling to formally test adult SES, adult adversity and social support as mediating mechanisms linking ACEs to mental health impairment in a state population sample. We hypothesize that elevated ACE exposures will adversely impact mental health directly, and via indirect pathways: through lower adult income, greater adult adversity, and lower social support.
Methods
Sample
Data were from the 2011 Behavioral Risk Factor Surveillance System (BRFSS) for Washington State (n = 14,001) —a cross-sectional, random-digit-dialed population-based state telephone survey administered through state health departments in collaboration with the Centers for Disease Control (CDC). BRFSS is a publicly available state health surveillance survey administered by the state Department of Health (DOH) in cooperation with the CDC. The state DOH provided de-identified data and approved the use of the data. Due to being a secondary data analysis, this study was exempt from ethics review. The study cohort consisted of non-institutionalized English or Spanish speaking adults aged 18 years or older, living in a household with a working landline telephone. BRFSS-recommended sampling weights were followed to adjust for a variety of sample demographic characteristics to construct a representative sample.
The study sample consisted of 59.8% female adults with the following racial/ethnic composition: 86.8% Caucasian, 5.0% Latino/a, 2.2% Asian, 1.3% African American, 1.0% Native American, 0.2% Hawaiian/Pacific Islander, and 3.5% mixed or other race/ethnicity. Average sample age was 58.2 years (SD = 16.0), with approximately 36% age 65 or older and 20% age 44 or younger. In addition, 23.7% of the sample’s household income was $25,000 or less, and 27.7% was $75,000 or more. About 5.9% of the sample never received a high school diploma, 23.9% had a high school education only, 31.1% attended some college, and 39.1% had a college degree and/or advanced training.
Measures
Adverse Childhood Experiences score is the sum of dichotomized “yes” responses across the eight CDC categories of adverse experiences before the age of 18: lived with a person with serious mental illness, with substance abuse (alcoholic or illegal drugs), who had been incarcerated, experienced parental divorce or separation, witnessed domestic violence in the childhood household, or experienced physical, sexual, or verbal abuse by a parent or adult in the home (range: 0–8). The CDC index varies from the original ACE index in that neglect questions were not asked (CDC, 2016).
Adult Adversity is an index (range: 0–6) including (1) caregiving burden (0 = not providing care, 1 = provide regular care to others with illness, disability, or to an unrelated child (2) incarceration (0 = never, 1 = incarcerated), (3) intimate partner violence, such as slap, hit, kick, punch, beat by intimate partner (0 = never, 1 = hurt by adult), (4) sexual assault, such as attempted or completed forced sex (0 = never, 1 = sexually assaulted by adult), (5) homelessness (any “yes” responses to residing in a transitional housing, a shelter, or voucher lodging and/or a vehicle, abandoned building, or public outdoors; range), and (6) health status requiring special equipment, such as a cane, a wheelchair, a special bed, or a special telephone (0 = none, 1 = used special equipment).
Low Income Status was an index of the sum of “yes” responses to indicators of low socioeconomic status (SES), with higher values indicating lower income (range: 0–4): (1) annual low-income household (0 = $25,000 or more, 1 = $0 to ≥$25,000), (2) inability to work (0 = employed, self-employed, homemaker, student, and retiree, 1 = unemployed or unable to work due to other reasons), (3) medical cost barrier (0 = none, 1 = needed see a doctor but not able because of cost) and (4) food insecurity (0 = none, 1 = experienced at least one of 5 indicators that over the past 12 months within respondent’s household: 1) sometimes or often food didn’t last, 2) ate unbalanced meals, 3) cut meal size or skipped meal, 4) ate less than needed, or 5) was left hungry).
Social Support was assessed as the number of people respondents trusted for practical help, plus an additional value of 1 if respondents report being married or partnered.
Control Variables included educational attainment (1= Less than high school, 2= High school graduate, 3= Some college, 4=College graduate), male or female gender (included as dummy variable of female=1), race with mutually exclusive categories of White or Caucasian, Black or African American, Hispanic, other race or Multiracial (included as dummy variables).
Mental Health Impairment (MH) factor included three indicators. These included (1) serious mental illness index based on the Kessler 6 (Kessler et al., 2003) with six items asking about respondents’ feelings over the past 30 days of being nervous, hopeless, restless, depressed, that everything was an effort or worthless assessed on a 5 point Likert scale (none to all the time; range: 0–24), (2) number of days in the past month the respondent missed usual activities such as work or self-care due to a mental condition or emotional problem, and (3) number of days in the past 30 the respondent reported felt they had poor mental health (the above two ranged: 0–30).
Analytic Strategy
Theory testing in structural equation modeling (SEM) is performed by two steps (Rizzo & Kintner, 2013): (1) the measurement model was tested through a confirmatory factor analysis (CFA) to assess the construct validity of the latent factor of mental health impairment; and (2) test of a theory-driven model through a structural equation modeling (SEM) which examined the hypothesized relationships among both the manifest measures and the latent factors.
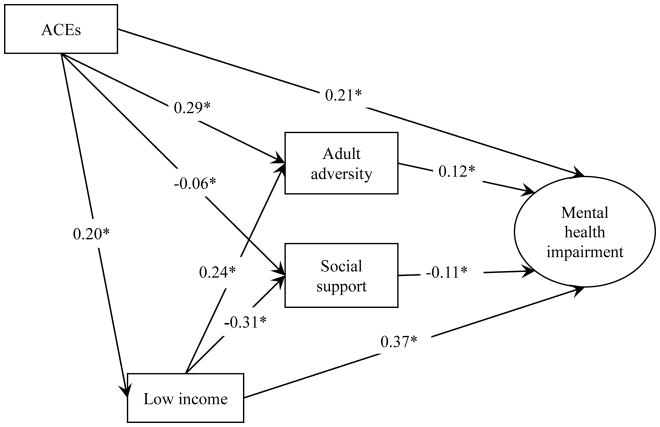
First, a latent factor was created of the three mental health impairment items, controlling for demographic factors. Four additional manifest variables (ACEs, adult adversity index, low income status, and social support) were included in the full structural model. The full structural model consisted of main pathways from the ACE index to low income, adult adversity and social support, to mental health impairment. Detailed results about parameter estimates and fit indices are presented in Table 2 and Figure 1. The indirect or non-adjacent relationships among ACEs, low income, and mental health were computed to examine the total effects of the two indicators on the main outcome. Control variables were regressed on all model variables.
Table 2.
Direct, Indirect, and Total Effects of ACEs on Mental Health Impairment
| Pathway | Direct effects | Indirect effects | Total effects |
|---|---|---|---|
| ACE → Adult adversity | 0.29* | - | 0.44* |
| ACE → Low income | 0.20* | - | 0.20* |
| ACE → Social support | −0.06* | - | −0.06* |
| ACE → MH impairment | 0.21* | 0.13* | 0.34* |
| ACE → Adult adversity → MH impairment | - | 0.04* | - |
| ACE → Social support → MH impairment | - | 0.01* | - |
| ACE → Low income → MH impairment | - | 0.08* | - |
| ACE → Low income → Adult adversity → MH impairment | - | 0.01* | - |
| ACE → Low income → Social support → MH impairment | - | 0.01* | - |
| Low income → Adult adversity | 0.24* | - | 0.39* |
| Low income → Social support | −0.31* | - | −0.29* |
| Low income → MH impairment | 0.37* | 0.06* | 0.43* |
| Low income → Adult adversity → MH impairment | - | 0.03* | - |
| Low income → Social support → MH impairment | - | 0.03* | - |
| Adult adversity → MH impairment | 0.12* | - | 0.12* |
| Social Support → MH impairment | −0.11* | - | −0.11* |
Notes. ACE= Adverse childhood experience, MH=mental health
p<.001
Figure 1.
Full structural model of pathways from ACEs to mental health impairment.
Note. Oval represents latent construct and squares represent measured indicators. All estimates are standardized. Fit: CFI=0.99, TLI=0.98, RMSEA=0.01.
*p<.001.
All analyses were conducted in Mplus 7.4 (Muthén, & Muthén, 1998–2015). Less than 9% of exogenous variables were missing. To address categorical indicators with missingness, mean and variance-adjusted weighted least squares (WLSMV) estimation using a pairwise-present approach to missing data was used. In addition, to take into account the stratified nature of our sample, the STRATIFICATION option along with TYPE=COMPLEX was used to provide more accurate standard errors (Muthén, & Muthén, 1998–2015).
Results
Table 1 shows bivariate correlations among all observed variables. All variables were significantly correlated (p<.001) and in the hypothesized directions. One latent factor for mental health impairment was formed, adjusting for all control variables. The resulting measurement model fit well (CFI=0.99, TLI=0.99, RMSEA=0.01) with standardized factor loadings ranging from 0.68 to 0.87. Results of the CFA suggest that the measurement model adequately confirms the factor structure of these variables for our sample before performing the substantive latent variable SEM (Bowen & Guo, 2012).
Table 1.
Correlations, Means, and Standard Deviations for Observed Variables (N=14,001)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. ACEs | - | ||||||
| 2. Adult SES | 0.23* | - | |||||
| 3. Social support | −0.13* | −0.31* | - | ||||
| 4. Adult adversity index | 0.35* | 0.27* | −0.15* | - | |||
| 5. Serious mental illness | 0.32* | 0.42* | −0.23* | 0.08* | - | ||
| 6. Missed work | 0.22* | 0.33* | −0.17* | 0.06* | 0.58* | - | |
| 7. Number of days mentally ill | 0.22* | 0.33* | −0.17* | 0.11* | 0.61* | 0.48* | - |
|
| |||||||
| Mean | 1.73 | 0.78 | 3.09 | 0.65 | 3.14 | 1.08 | 3.84 |
| Standard deviation | 1.95 | 1.09 | 0.96 | 0.80 | 3.81 | 4.56 | 7.89 |
Note.
p<.001
Table 2 and Figure 1 present the results of the full structural model. Table 2 shows standardized direct, indirect, and total effect sizes of the structural model. Figure 1 diagrams the structural paths of the final model; fit indices (CFI=0.99, TLI=0.98, RMSEA=0.01) indicate a good fit of data with the hypothesized structural model. Our findings indicate that low income, social support and adult adversity are indeed mechanisms linking ACEs in childhood to adult mental health impairment.
We found that ACEs in childhood was positively associated with mental health impairment through multiple significant pathways. 1) ACEs significantly increased adult adversity, which in turn increased mental health impairment The indirect effects of ACEs through this pathway were also significant (β=0.04, p<.001). 2) ACEs were significantly associated with low income as an adult, which then led to increased mental health impairment. ACEs exerted significant indirect effects through low income to mental health impairment (β=0.08, p<.001). 3) ACEs significantly reduced social support, and exerted significant indirect effects on mental health impairment through low income (β=0.01, p<.001). and social support (β=0.01, p<.001). 4) A significant direct effect from ACEs to mental health impairment remained, even after accounting for all other variables in the model.
Low income in adulthood also demonstrated direct and indirect pathways to increased mental health impairment. 1) Low income significantly increased adult adversity and exerted indirect effects through this pathway as well (β=0.03, p<.001). 2) Low income also reduced social support, and low income also had small but significant indirect effects through social support (β=0.03, p<.001). 3) Finally, low income also demonstrated significant direct effect of increasing mental health impairment, beyond the influence of all other variables in the model.
Both of our mediators had a significant influence on mental health impairment, with adult adversity contributing to and social support protecting against mental health impairment in adulthood.
Discussion
The present study offers a significant contribution to our knowledge of the mechanisms through which ACEs accumulate adversity in adulthood by integrating theories of stress embodiment and proliferation. This study is among the first to apply structural equation modeling in testing both direct and mediated effects of ACEs on adult mental health. ACEs evidenced a significant direct pathway to later mental health, controlling for the contributions of adult income, social support, and continuity of stress through adult adversities. Each of these intervening variables demonstrated significant pathways of their own to mental health outcomes, with indirect pathways from ACEs through adult income and adult adversity also achieving significance. These findings provide important information about pathways—both direct and indirect—that are consistent with integration of stress embodiment and stress proliferation processes that, without buffering or interruption, tend to cascade throughout a life course to progressively undermine health and functioning.
Low Income Status: A Robust Pathway
Low adult income served as a significant mediating pathway to mental health impairment through both amplified adult adversity and more impoverished social support. Poor academic success and school behavior have been predicted by higher ACEs (Raposa et al., 2014), and serve as preludes to the significant role of adult economic disadvantage in the process of stress proliferation. As Doan et al. (2014) have noted, low income status is associated with suboptimal physical and social environments such as substandard housing, schools, or workplaces that involve stressors such as noise, crowding, vermin, toxins, and unsafe or abusive behavior by others (Adler & Newman, 2002). Moreover, although household income in childhood was not available here, childhood households with risk factors such as caretaker mental illness, substance abuse, or incarceration or maltreatment, are homes less likely to be experiencing social and economic success, stability or stress-buffering parenting—setting the stage for psychophysiological and socioemotional impairments to take root (Evans & Kim, 2013).
Low income in our model may thus be thought of as a proxy for multiple sources of stress exposure and represents an accumulation of poverty indicators. Poverty predicts elevated physiologic dysregulation in adulthood irrespective of concurrent adult risk exposures (Evans & Kim, 2012), suggesting that some of the pathway from adult SES to mental health may be carrying biological as well as socio-structural effects from early adversities of maltreatment, family dysfunction, and poverty.
Adult Adversity and Social Support
Following stress proliferation effects through socioeconomic status, ACEs demonstrated continued direct and indirect pathways both to other significant adversity exposures in adulthood (e.g., victimization, incarceration) that elevated mental health impairment. The significance of indirect pathways suggests that adult adversities for the current respondents layer atop a trajectory of stressors with the effect of compounding deleterious effects of early adversity (Hazel et al., 2008). These patterns of stress exposures hamper acquiring the cognitive, emotional, and behavioral skills and resources to effectively cope and to be successful in interpersonal, education, work force, and related contexts (Turner & Lloyd, 1995). As recurring and cumulative stress cultivate mental health symptoms and disordered functioning, these, in turn, can serve to elicit interpersonal conflict, evasion, and other stressful circumstances that add to the cumulative adversity burden, and extend the impact to others through problems in life partnerships, parenting, and weakening of interpersonal supports (Hammen, 2006).
Social cognitive mechanisms undergird these processes. The brain plays a range of roles in the stress process including subjective perception that an event or condition poses danger and, thus, the risk of harm. These appraisal processes shape subsequent behavioral responding as well as physiologic response sequences, such as the stress hormone cortisol through the HPA axis and continuing through subsequent biological processes as the systems works to re-establish balance in neurophysiological functioning (Juster et al., 2010). Hager and Runtz (2012) found that greater exposure to childhood adversity such as maltreatment led to elevated levels of both perceived stress from adult life events and maladaptive emotion-focused coping (e.g., blaming oneself) which carried indirect effects of early adversity in mediated pathways to adult health concerns. Those with histories of early adversity are then often more susceptible to effects of later stress through greater likelihood of adversity exposure, to perceiving life events as stressful, and to be negatively affected by stressors through exacerbating coping responses as well as through stress sensitization wherein both the stress activation link between stress exposure and psychopathological symptoms (e.g., anxiety, depression) is strengthened as well as the magnitude of those effects (Morris, Ciesla, & Garber, 2010; Thakkar & McCanne, 2000).
Social support is a critical resource in buffering the effects of stressors on mental health, and yet a resource that is vulnerable to erosion by the adversities that spawn the stress. People maltreated as children tend, for example, to have smaller support networks, less support satisfaction, and without benefit of healthy models, less adaptive scripts and skills to build sustaining relationships as youth, which then jeopardize adult social support resources (Hill, Kaplan, French, & Johnson, 2010; Turner & Butler, 2003). ACEs were significantly associated with lower social support and carried mediated effects from low income, to mental health impairment. Vranceanu, Hobfoll, and Johnson (2007) argue that early adversities may interfere with individuals’ ability to develop appropriate social support structures as well as increase their likelihood of encountering both personal and material losses and deficits, which, in turn, can overwhelm coping capacity and even further erode successful social support accrual.
ACEs, Mental Health Impairment, and Implications
Our findings point to intervention implications across multiple points in the life course and at multiple ecological levels. Turner, Thomas and Brown (2016) consider whether the health and mental health effects of ACEs are immutable, or whether they might be adaptable by exposure to healthier social contexts across development or through intervention. The presence of a significant direct pathway from ACEs to mental health impairment in our model indicates involvement of mechanisms beyond those directly assessed in the model, or that portions of stress pathways are in fact enduring. Research with younger children, adolescents and young adults indicates that the association between ACEs and mental health symptoms begins appearing early (McLaughlin et al., 2012; Wilkes et al., 2012), with effects particularly pronounced among youth with exposures sufficiently severe for child welfare system involvement, including social development deficits such as interpersonal relationships and coping skills (Kerker et al., 2015). Epidemiological evidence indicates that most adults with psychological disorders report multiple ACEs, significant adult stressors and greater risk for maladaptive coping, consistent with life course pathways reflected in the current findings (Lu et al., 2008).
Although the mental health burden of ACEs may be significant, many experiences considered to be adverse childhood experiences are either preventable, or with appropriate supports, their impacts can be mitigated. Significant research has documented evidence-based strategies for preventing the occurrence of child maltreatment (Mikton & Butchart, 2009). Contacts in the public systems where individuals receive health care, education, childcare, and related services are also potential points of intervention. These child-serving systems are increasingly developing trauma informed approaches to service provision through increased knowledge in the workforce of the impact of trauma and linkages to mental health care (Ko et al., 2008). Schools and their associated health support systems are a particularly important public system where ACE exposed youth might experience reparative social environments. Progress is being made with developing trauma-informed school models focused on creating predictable, support school environments responsive to additional needs of students who may have experienced ACEs (Wiest-Stevenson & Lee, 2016).
Despite the known life course detriments associated with early ACE exposure, the mediators in our model are suggestive of opportunities for intervening in stress proliferation processes in adulthood. Although low income was a robust mediator, processes larger than one’s own choices and behaviors often influence one’s broader socioeconomic standing. Interventions and policies aimed towards increasing the availability, quality, stability, and supports for employment might serve to break down structural barriers limiting individuals’ earning potential. Interventions across the life course such as early learning opportunities, dropout prevention, advanced education and workforce preparation as well as family and economic supports may be particularly consequential toward interrupting income-related life conditions that increase risk of psychopathology for ACE-exposed individuals.
Given the breadth of mental disorders that have been associated with early life adversity, a transdiagnostic approach that focuses on impairments of emotional processing and executive functioning—targets relevant to curbing psychosocial dimensions of stress proliferation-- as intervention priorities is emerging (McLaughlin, 2016). Many with disorders are not in treatment, underscoring the importance of assessing adversity exposure along the life course, through childcare, educational, vocational, primary care and related filtering service sites to assess for needs. Use of cognitive-behavioral therapies, skill building (e.g., coping and interpersonal skills) and resilience-oriented mindfulness approaches also show considerable promise toward attenuating symptomology as well as more effective long-term stress management (Korotana, Dobson, Pusch, & Josephson, 2016).
Limitations
Our findings are based on cross-sectional data including retrospective assessment of ACEs which, like most studies in this arena, raise questions of recall bias. Considerable testing of retrospective measures of ACEs has indicated adequate variance, stability of linear trends between retrospectively assessed adversity and subsequent outcomes, and weak to no evidence of current mood state effects on reporting (Hardt, Vellaisamy, & Schoon, 2010; Yancura & Aldwin, 2009). Findings of underreporting of actual occurrence of ACEs may serve to attenuate linear associations, such that effects may be stronger than are evident. Cross sectional data also prevents us from testing time ordering, thus mental health impairment may in fact predict adult adversity and social support. Future research using longitudinal data are required to test the potential for reciprocal relationships.
Another limitation relates to measurement availability within secondary analysis. Indicators available to represent the constructs of adult adversity, social support, and mental health reflect, for example, only a small portion of those possible domains. That said, the construction of latent constructs and multi-indicator indices should serve to increase the stability of the measures and trends in the results. Our sample may also be biased by the fact that all respondents had to have a landline, and there may also be bias in who is willing to answer telephone interview questions. Finally, population characteristics of Washington State will vary in some respects from those of other states. These variations may or may not bear upon generalizability of the findings reported here.
Conclusion
The results from this study highlight the long and complex reach of early life adversity in compromising mental health far into adulthood. The patterns of association modeled here represent stress proliferative pathways through which ACE effects become embedded in multiple dimensions of development and functioning from early life to later adulthood. Indeed the majority of effects on mental health derivative of ACEs were mediated, suggesting targets of intervention to foster turning points in these trajectories of stress continuity and health erosion. Elevated exposures to early adversity among high risk samples (e.g., homeless, victims, system involved) argues for routine attention to this aspect of history assessment in services for these vulnerable, targeted groups. Establishing the existence of life course pathways from ACEs within a representative community-based sample suggests the value of broader public health commitment toward more universal screening, preventive, and treatment strategies aimed at curbing mental health impairment and fostering resilience.
There are considerable benefits in drawing upon population-based surveys within a nationally integrated system. Use of these types of surveillance data offers a practical and replicable strategy for developing a multi-pathway understanding of life course adversities and their bearing upon mental health that is not confined to clinical settings. Embedding maltreatment and other toxic stressors into routine health surveys opens access to community-based samples that are more representative of the general population than typically available, yielding insights that might be translated into interventions across a range of sectors and settings.
Acknowledgments
This research was supported in part by a grant from a Eunice Kennedy Shriver National Institute of Child Health and Human Development research infrastructure grant, R24 HD042828, to the Center for Studies in Demography & Ecology at the University of Washington as well as a grant from the Gates Foundation to the Foundation for Healthy Generations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Affairs. 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- Anderson PL, Tiro JA, Price AW, Bender MA, Kaslow NJ. Additive impact of childhood emotional, physical, and sexual abuse on suicide attempts among low income African American women. Suicide and Life-Threatening Behavior. 2002;32(2):131–138. doi: 10.1521/suli.32.2.131.24405. [DOI] [PubMed] [Google Scholar]
- Bowen NK, Guo S. Structural equation modeling. Oxford: Oxford University Press; 2012. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Adverse childhood experiences reported by adults---five states, 2009. MMWR Morbidity and mortality weekly report. 2010;59(49):1609. [PubMed] [Google Scholar]
- Center for Disease Control and Prevention (CDC) About Behavioral Risk Factor Surveillance System ACE Data. 2016 Retrieved from: https://www.cdc.gov/violenceprevention/acestudy/ace_brfss.html.
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Danese A, Moffitt TE, Pariante CM, Ambler A, Poulton R, Caspi A. Elevated inflammation levels in depressed adults with a history of childhood maltreatment. Archives of General Psychiatry. 2008;65(4):409–415. doi: 10.1001/archpsyc.65.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiology & Behavior. 2012;106(1):29–39. doi: 10.1016/j.physbeh.2011.08.019. [DOI] [PubMed] [Google Scholar]
- Doan SN, Dich N, Evans GW. Childhood cumulative risk and later allostatic load: Mediating role of substance use. Health Psychology. 2014;33(11):1402. doi: 10.1037/a0034790. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. American Journal of Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Evans GW, Kim P. Childhood poverty and young adults’ allostatic load: The mediating role of childhood cumulative risk exposure. Psychological Science. 2012;23(9):979–983. doi: 10.1177/0956797612441218. [DOI] [PubMed] [Google Scholar]
- Evans GW, Kim P. Childhood poverty, chronic stress, self regulation, and coping. Child Development Perspectives. 2013;7(1):43–48. doi: 10.1111/cdep.12013. [DOI] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Font SA, Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse & Neglect. 2016;51:390–399. doi: 10.1016/j.chiabu.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Archives of General Psychiatry. 2010;67(2):113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hager AD, Runtz MG. Physical and psychological maltreatment in childhood and later health problems in women: An exploratory investigation of the roles of perceived stress and coping strategies. Child Abuse & Neglect. 2012;36(5):393–403. doi: 10.1016/j.chiabu.2012.02.002. [DOI] [PubMed] [Google Scholar]
- Hankin BL. Childhood maltreatment and psychopathology: Prospective tests of attachment, cognitive vulnerability, and stress as mediating processes. Cognitive Therapy and Research. 2005;29(6):645–671. doi: 10.1007/s10608-005-9631-z. [DOI] [Google Scholar]
- Hammen C. Stress generation in depression: Reflections on origins, research, and future directions. Journal of Clinical Psychology. 2006;62(9):1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- Hardt J, Vellaisamy P, Schoon I. Sequelae of prospective versus retrospective reports of adverse childhood experiences. Psychological Reports. 2010;107(2):425–440. doi: 10.2466/02.04.09.10.16.21.PR0.107.5.425-440. [DOI] [PubMed] [Google Scholar]
- Hazel NA, Hammen C, Brennan PA, Najman J. Early childhood adversity and adolescent depression: the mediating role of continued stress. Psychological Medicine. 2008;38(4):581–589. doi: 10.1017/S0033291708002857. [DOI] [PubMed] [Google Scholar]
- Hill TD, Kaplan LM, French MT, Johnson RJ. Victimization in early life and mental health in adulthood: An examination of the mediating and moderating influences of psychosocial resources. Journal of Health and Social Behavior. 2010;51(1):48–63. doi: 10.1177/0022146509361194. [DOI] [PubMed] [Google Scholar]
- Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Kerker BD, Zhang J, Nadeem E, Stein RE, Hurlburt MS, Heneghan A, … Horwitz SM. Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Academic Pediatrics. 2015;15(5):510–517. doi: 10.1016/j.acap.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, … Zaslavsky AM. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Ko S, Ford J, Kassam-Adams N, Berkowitz S, Wilson C, Wong M, … Layne C. Creating trauma-informed systems: Child welfare, education, first responders, health care, juvenile justice. Professional Psychology: Research and Practice. 2008;39(4):396. doi: 10.1037/0735-7028.39.4.396. [DOI] [Google Scholar]
- Korotana LM, Dobson KS, Pusch D, Josephson T. A review of primary care interventions to improve health outcomes in adult survivors of adverse childhood experiences. Clinical Psychology Review. 2016;46:59–90. doi: 10.1016/j.cpr.2016.04.007. [DOI] [PubMed] [Google Scholar]
- Lu W, Mueser KT, Rosenberg SD, Jankowski MK. Correlates of adverse childhood experiences among adults with severe mood disorders. Psychiatric Services. 2008;59(9):1018–1026. doi: 10.1176/ps.2008.59.9.1018. [DOI] [PubMed] [Google Scholar]
- Maschi T, Baer J, Morrissey MB, Moreno C. The aftermath of childhood trauma on late life mental and physical health: A review of the literature. Traumatology. 2013;19(1):49–64. doi: 10.1177/1534765612437377. [DOI] [Google Scholar]
- McCrory C, Dooley C, Layte R, Kenny RA. The lasting legacy of childhood adversity for disease risk in later life. Health Psychology. 2015;34(7):687. doi: 10.1037/hea0000147. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA. Future directions in childhood adversity and youth psychopathology. Journal of Clinical Child & Adolescent Psychology. 2016;45(3):361–382. doi: 10.1080/15374416.2015.1110823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Archives of General Psychiatry. 2012;69(11):1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, Topitzes J, Reynolds AJ. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the US. Child abuse & neglect. 2013;37(11):917–925. doi: 10.1016/j.chiabu.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikton C, Butchart A. Child maltreatment prevention: a systematic review of reviews. Bulletin of the World Health Organization. 2009;87(5):353–61. doi: 10.2471/blt.08.0570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Schutte KK, Brennan PL, Moos BS. The interplay between life stressors and depressive symptoms among older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60(4):199–206. doi: 10.1093/geronb/60.4.P199. [DOI] [PubMed] [Google Scholar]
- Morris MC, Ciesla JA, Garber J. A prospective study of stress autonomy versus stress sensitization in adolescents at varied risk for depression. Journal of Abnormal Psychology. 2010;119(2):341. doi: 10.1037/a0019036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles: Muthén & Muthén; 1998–2015. [Google Scholar]
- Nurius PS, Green S, Logan-Greene P, Borja S. Life course pathways of adverse childhood experiences toward adult psychological well-being: a stress process analysis. Child Abuse & Neglect. 2015;45:143–153. doi: 10.1016/j.chiabu.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L, Schieman S, Fazio E, Meersman S. Stress, health, and the life-course: some conceptual perspectives. Journal of Health and Social Behavior. 2005;46(2):205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Raposa EB, Hammen CL, Brennan PA, O’Callaghan F, Najman JM. Early adversity and health outcomes in young adulthood: The role of ongoing stress. Health Psychology. 2014;33(5):410. doi: 10.1037/a0032752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizzo V, Kintner E. The utility of the behavioral risk factor surveillance system (BRFSS) in testing quality of life theory: an evaluation using structural equation modeling. Quality Of Life Research. 2013;22(5):987–995. doi: 10.1007/s11136-012-0228-1. [DOI] [PubMed] [Google Scholar]
- Rutter M, Kim-Cohen J, Maughan B. Continuities and discontinuities in psychopathology between childhood and adult life. Journal of Child Psychology and Psychiatry. 2006;47(3–4):276–295. doi: 10.1111/j.1469-7610.2006.01614.x. [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, … Wood DL. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246. doi: 10.1542/peds.2011-2663. [DOI] [PubMed] [Google Scholar]
- Shrira A. The effect of lifetime cumulative adversity on change and chronicity in depressive symptoms and quality of life in older adults. International Psychogeriatrics. 2012;24(12):1988–1997. doi: 10.1017/S1041610212001123. [DOI] [PubMed] [Google Scholar]
- Thakkar RR, McCanne TR. The effects of daily stressors on physical health in women with and without a childhood history of sexual abuse. Child Abuse & Neglect. 2000;24(2):209–221. doi: 10.1016/S0145-2134(99)00129-5. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior. 2011;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior. 1995:360–376. doi: 10.1023/A:1021853600645. [DOI] [PubMed] [Google Scholar]
- Turner HA, Butler MJ. Direct and indirect effects of childhood adversity on depressive symptoms in young adults. Journal of Youth and Adolescence. 2003;32(2):89–103. doi: 10.1023/A:1021853600645. [DOI] [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Social Science & Medicine. 2006;62(1):13–27. doi: 10.1016/j.socscimed.2005.05.030. [DOI] [PubMed] [Google Scholar]
- Turner R, Thomas C, Brown T. Childhood adversity and adult health: Evaluating intervening mechanisms. Social Science & Medicine. 2016;156:114–124. doi: 10.1016/j.socscimed.2016.02.02. [DOI] [PubMed] [Google Scholar]
- Vranceanu AM, Hobfoll SE, Johnson RJ. Child multi-type maltreatment and associated depression and PTSD symptoms: The role of social support and stress. Child Abuse & Neglect. 2007;31(1):71–84. doi: 10.1016/j.chiabu.2006.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade R, Cronholm PF, Fein JA, Forke CM, Davis MB, Harkins-Schwarz M, … Bair-Merritt MH. Household and community-level adverse childhood experiences and adult health outcomes in a diverse urban population. Child Abuse & Neglect. 2016;52:135–145. doi: 10.1016/j.chiabu.2015.11.021. [DOI] [PubMed] [Google Scholar]
- Wickrama KAS, Conger RD, Abraham WT. Early adversity and later health: The intergenerational transmission of adversity through mental disorder and physical illness. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60(Special Issue 2):S125–S129. doi: 10.1093/geronb/60.Special_Issue_2.S125. [DOI] [PubMed] [Google Scholar]
- Wickrama KK, Lee TK, O’Neal CW, Kwon JA. Stress and resource pathways connecting early socioeconomic adversity to young adults’ physical health risk. Journal of Youth and Adolescence. 2014;44(5):1109–1124. doi: 10.1007/s10964-014-0207-7. [DOI] [PubMed] [Google Scholar]
- Wiest-Stevenson C, Lee C. Trauma-informed schools. Journal of Evidence-informed Social Work. 2016;13(5):498–503. doi: 10.1080/23761407.2016.1166855. [DOI] [PubMed] [Google Scholar]
- Wilkes TC, Guyn L, Li B, Lu M, Cawthorpe D. Association of child and adolescent psychiatric disorders with somatic or biomedical diagnoses: Do population-based utilization study results support the adverse childhood experiences study? Permanente Journal. 2012;16(2):23–26. doi: 10.7812/tpp/11-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancura LA, Aldwin CM. Stability and change in retrospective reports of childhood experiences over a 5-year period: findings from the Davis Longitudinal Study. Psychology and Aging. 2009;24(3):715–721. doi: 10.1037/a0016203. [DOI] [PubMed] [Google Scholar]