Abstract
Burn care often involves procedures that result in significant pain experiences for patients which, in turn, can lead to poorer physical and psychological health outcomes. Distraction and virtual reality (VR) are an effective adjunct to pharmacological interventions in reducing pain. Much of the research that has demonstrated efficacy for VR in burn care has involved expensive and extensive technology. Thus, identifying cost-effective, feasible, acceptable, and effective approaches to apply distraction within routine burn care is important. The objective of this mixed-methods study was to evaluate key stakeholder (i.e., patients, providers) perceptions of feasibility, acceptability, and effectiveness for the use of low-cost VR technology during routine burn care with adult patients. Ten adult patients used VR during burn care dressing changes in an outpatient clinic setting, after which they completed a satisfaction survey and individual qualitative interview. Providers also completed a satisfaction/perception survey after each participant’s care. Quantitative and qualitative results from both patient and provider perspectives consistently supported the feasibility and utility of applying low-cost VR technology in this outpatient burn clinic setting. Special considerations (e.g., aspects to consider when choosing an apparatus or application) stemming from stakeholder feedback are discussed.
Keywords: Burn care, Adults, Virtual reality, Distraction
1. Introduction
Treatment of burn-related wounds routinely involves dressing changes and other procedures that cause discomfort and excruciating pain [1,2]. Although efforts are made to reduce the experience of pain for burn survivors receiving these treatments, such as the use of pharmacological therapy and supportive care by the healthcare team, patients continue to experience significant pain during standard care procedures in the weeks following a burn injury. Research indicates that pain is associated with post-treatment outcomes. For instance, patients who report experiencing higher levels of pain during hospitalization also report poorer physical and psychological functioning at one month, one year, and/or up to two years after discharge [3,4]. Considering these short- and long-term consequences of experiencing pain during treatment, it is imperative to identify low-cost, feasible ways to temper the pain experience for patients with burn injuries so that they may be used widely.
Given the repetitious yet time-limited nature of wound debridement, dressing changes, and similar procedures, psychological coping strategies for pain are suited uniquely for burn survivors. For example, hypnosis can be used as an analgesic intervention [5,6], with evidence for its use specifically in the burn care setting [7]. Cognitive and behavioral psychological approaches such as distraction, reappraisal, information provision, relaxation training, and operant conditioning are also relevant strategies for coping with acute pain, with distraction being particularly efficacious [8]. Distraction alters pain perception by (1) orienting attention away from painful stimuli (e.g., Ref. [9]) and/or (2) reducing anxiety associated with pain stimuli or the pain situation (e.g., Ref. [10]). Distraction has been systematically employed in a variety of settings for effective pain reduction and management, including procedural pain in cancer treatment (e.g., Ref. [11]), organ transplant pain (e.g., Ref. [12]), and dental care-related pain (e.g., Ref. [13]).
Although several strategies are available for producing therapeutic distraction (e.g., imagery, attention tasks, music, electronic gaming), virtual reality (VR) technology appears to be particularly engaging, providing a potent shifting of attention that allows patients to benefit strongly from this coping strategy. VR involves the “use of computer technology to create the effect of an interactive three-dimensional world in which the objects have a spatial presence” [14]. Because VR technology is immersive and affords such a high degree of distraction, it is ideal for use in the management of significant acute pain. In fact, VR has been utilized effectively in medical and dental settings for the management of procedure-related pain (e.g., Refs. [15,16]). Specifically, VR technology has been used successfully in burn care settings, with results of multiple studies indicating reductions in pain associated with routine burn-related procedures such as wound care [17], wound debridement [18], dressing changes [19], and physical therapy [20,21].
Though clearly useful for inducing distraction in the management of significant acute treatment-related pain for burn injuries, traditional VR technology is not widely used, most notably because of cost. Individual VR equipment components used in published research and with patient care in some burn centers total over $35,000, which may be cost prohibitive for some clinics [22]. Recently, however, VR technology has become more accessible to the layperson and healthcare professionals alike. Application developers have created software that allows consumers to use a small electronic device (e.g., mobile smartphone, iPod) to display VR images when fastened in front of their eyes with a comfortable, wearable device (known generically as “Google Cardboard”) [23]. Many of these wearable devices cost less than $20. A complete, portable VR apparatus would include the wearable goggles, a small electronic device (iPod, smartphone), headphones, and free or inexpensive VR applications; these components may be assembled for less than $200, which is considerably less expensive than traditional VR technology platforms currently in use for clinical and research purposes.
The availability of such inexpensive and accessible VR technology introduces unique opportunities for dissemination to and implementation within healthcare settings in which patients experience significant acute pain, such as burn centers. If it is feasible to utilize this technology in the burn center setting, and if the technology provides adequate immersion for clinically effective distraction, a relatively inexpensive and accessible VR technology may provide an exceptional pain management option for burn survivors who are undergoing treatment for their injuries. Therefore, the aims of the present study were to use a mixed-methods approach to assess key stakeholder (i.e., patient & provider) perceptions of feasibility, acceptability, and effectiveness for the use of low-cost VR technology during routine burn care with adult patients.
2. Method
2.1. Participants
Patients receiving treatment for burns at West Penn Burn Center Clinic in Pittsburgh, PA were recruited. Patients were eligible for participation if they: (a) were aged 18 years or older; (b) were undergoing either a dressing change or debridement for a burn injury below the shoulders; (c) were English-speaking; and (d) had sufficient visual acuity (because sight of the electronic device screen is a key component of the VR experience). Patients with glasses and contacts were permitted to participate as long as they could view the screen. Exclusion criteria included: (a) having a burn injury to the face and/or neck (i.e., the location of these injuries precludes the use of the VR goggles); and (b) significant cognitive impairments (e.g., intellectual disability).
In total, 10 patients participated in the study (M=47.10 years, SD=14.71). Table 1 displays demographic and burn injury information by participant. In summary, the sample was 60% Caucasian/White, 30% Black/African American, and 10% American Indian/Alaskan Native. Most participants were male, high school educated, and from low-income families. The sample was varied across a range of TBSA, burn depth, and history of graft surgery.
Table 1.
Sample description.
| Sex | Age | Race | Education | Annual income | Location of burns | % TBSA | Burn degree | Skin graft |
|---|---|---|---|---|---|---|---|---|
| M | 39 | White, Asian | Bachelor’s degree | >$100,000 | Right hand | <1 | 2nd | No |
| M | 30 | Black | NR | $20,000 –$29,000 | Right shoulder, arm, & hand; chest, abdomen | 18 | 3rd | Yes |
| F | 62 | White | Some college | $20,000 –$29,000 | Left arm & hand; abdomen | 5 | 2nd | Yes |
| F | 49 | Black | High school GED | $20,000 –$29,000 | Left shoulder, arm, & hand; back | 5 | 3rd | No |
| M | 33 | American Indian/ Alaskan Native | Some college | NR | Right hand | 40 | 2nd | No |
| M | 53 | Black | Some high school | $10,000 –$19,000 | Bilateral legs | 5 | 2nd | No |
| M | 69 | White | Some college | NR | Bilateral arms & hands | 15 | 2nd | Yes |
| M | 30 | White | NR | $10,000 –$19,000 | Bilateral hands; chest | 7.5 | 2nd | Yes |
| M | 41 | White | High school graduate | $10,000 –$19,000 | Right foot | <1 | 3rd | Yes |
| M | 65 | White | High school graduate | <$10,000 | Neck; right shoulder | 9 | 3rd | Yes |
NR=not reported.
To assess medical provider perceptions of the use of VR, the providers who delivered the burn care while participants were experiencing VR also were recruited to take part in this study. In total, eight medical providers were recruited, including one attending physician, one physician’s assistant, two medical residents, one certified nurse practitioner, one nurse, and two physician’s assistant students.
2.2. Procedure
After participants were consented, psychology graduate students introduced participants to the VR equipment. Participants then chose which specific application they would like to view from a document containing a screenshot of each one available. Other than being shown the VR equipment and a list of possible VR applications, participants did not start the VR experience until the medical procedure began. Thus, participants were familiarized with VR by the research staff for less than five minutes before the start of the VR experience. Next, the medical provider(s) explained the burn care procedure that would be performed. Research staff reminded participants that they were welcome to take off the VR mask and/or the headphones at any point in time during burn care. Then, the researcher began the VR application, and the medical provider conducted burn care. Research staff noted how long the participant wore the mask, whether or not the participant asked to remove the VR mask or the headphones, and whether the participant wanted to change to a different application. After the medical procedure, participants completed brief surveys and took part in a semi-structured interview. Participants were provided with a $10 gift card to compensate them for their time. Finally, the medical provider (s) completed a brief survey on their experience with the patient.
2.3. Apparatus
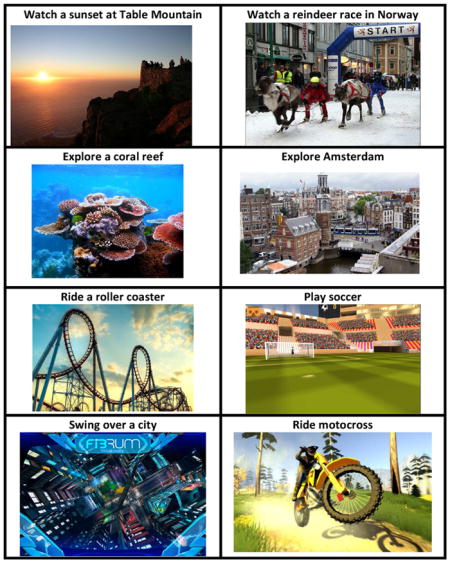
A refurbished, fifth generation iPod Touch [24] was used to deliver the VR videos. The participants chose between a list of eight VR applications: Table Mountain sunset, reindeer race in Norway, scuba diving at a coral reef, exploring Amsterdam, riding a roller coaster, playing soccer, and swinging through a city, and riding motocross. Appendix A displays screenshots of each application. These applications were organized such that those involving substantial movement were listed separate from those that did not, in case participants had a concern about motion sickness sensation. To create the VR experience, the iPod was placed inside of a Sunnypeak VR headset. Participants also were given the option to listen to the sound of the VR application on Sentey Flow LS 422 headphones. These particular apparatuses were chosen due to their relative low cost. The total cost of all VR equipment for this study was approximately $200 (US dollars).
2.4. Measures
2.4.1. Patient information form
On this study-specific form, participants reported on demographic variables. Additionally, research staff recorded injury details from a medical record review.
2.4.2. Patient perception form
This 5-item survey was devised for the purpose of the study to measure satisfaction with various aspects of the VR experience. Respondents rated items on a 4-point Likert-type scale (see Table 1).
2.4.3. Semi-structured interview
One of the authors (CF) conducted a brief semi-structured interview with each patient to assess perceived feasibility, acceptability, and effectiveness of VR in burn care. Participants were asked what they liked and disliked about the general experience with VR in burn care and their experience with the specific VR applications that they viewed. They also were asked how the use of VR in burn care could be improved. Specifically, participants were asked what would make using the technology easier in burn care, how VR could be used with other burn survivors, and how staff could make the VR experience better. Participants were then asked to list some reasons why they would and would not use VR again in burn care. Next, participants were asked how comfortable they felt while wearing the VR equipment. Lastly, participants were provided time to note any other comments that were not addressed in the questions above. The researcher recorded in writing all verbal responses on the interview form.
2.4.4. Provider perception form
The medical provider who performed burn care for the participant completed a brief survey measure on his or her perceptions of the feasibility of the VR procedures. This study-specific survey consisted of five items, each rated on a 4-point Likert-type scale (see Table 2). Some medical providers provided survey responses for multiple participants. Moreover, when possible, multiple providers completed a survey for a given patient. Thus, while eight providers were recruited for the study, a total of 12 provider surveys were completed.
Table 2.
Descriptive statistics of patient perceptions of virtual reality.
| Not at all | A little bit | Some | A lot | |
|---|---|---|---|---|
| How much did the virtual reality experience distract you during burn care? | 0% | 10% | 60% | 30% |
| How much did the virtual reality experience help decrease your pain during burn care? | 30% | 10% | 30% | 30% |
|
| ||||
| Very unlikely | Unlikely | Likely | Very likely | |
|
| ||||
| If given the change to do so, how likely would you be to ask to use virtual reality for your next burn care procedure? | 10% | 0% | 40% | 50% |
| How likely would you be to recommend virtual reality to another patient like you? | 0% | 0% | 40% | 60% |
|
| ||||
| Very unsatisfied | Unsatisfied | Satisfied | Very satisfied | |
|
| ||||
| Overall, how satisfied were you in using virtual reality during your burn care? | 0% | 0% | 50% | 50% |
Note. The statistics shown represent the frequency each response option was chosen (N=10).
3. Results
3.1. Quantitative analysis
3.1.1. Virtual reality use
Participants chose to view the scuba diving at coral reef application 5 times, the riding a roller coaster application 3 times, the exploring Amsterdam application 3 times, and the reindeer race in Norway one time. No participants chose to use Table Mountain sunset, playing soccer, or swinging applications. The total number of views exceeds the number of participants in the study because two participants elected to view multiple applications.
On average, participants wore the VR mask for 8.30min (SD=7.02). Three participants opted not to wear the headphones, and thus did not experience the audio in the VR application. One participant did not want to wear the headphones at the start of the VR application, but later decided to wear the headphones. The other six participants wore the headphones throughout the duration of the VR experience.
3.1.2. Patient perception of virtual reality
Descriptive statistics for patient responses on the patient perception form are shown in Table 2. A majority of participants reported that the VR experience distracted them and decreased pain “some” or “a lot.” Additionally, a majority of participants reported that were “likely” or “very likely” to use VR in their next burn care and to recommend VR to another patient. Overall, half the participants reported they were “satisfied” with use of VR during their burn care, and half the participants reported they were “very satisfied.”
3.1.3. Provider perceptions of virtual reality
Descriptive statistics for participant responses on the provider perception form are displayed in Table 3. A majority of the medical providers indicated that VR provided at least “some” distraction and offered at least “some” relief from pain and distress for patients. All of the providers reported that the VR procedure had no impact on their ability to perform the wound care procedure. A majority of the providers indicated that they would “probably” or “definitely” consider using VR again with the patient in future burn care procedures. Additionally, all providers reported that they were at least “satisfied” in using VR for the patient.
Table 3.
Descriptive statistics of provider perceptions of virtual reality.
| Not at all | A little bit | Some | A lot | |
|---|---|---|---|---|
| From your perspective, how much did the virtual reality experience distract the patient during burn care? | 0% | 8.33% | 33.33% | 58.33% |
| From your perspective, how much did the virtual reality experience help decrease your patient’s pain and distress during burn care? | 8.33% | 16.66% | 58.33% | 16.66% |
| Did the patient’s use of virtual reality interfere with your ability to complete your patient’s wound care? | 100% | 0% | 0% | 0% |
|
| ||||
| Not at all | Possibly | Probably | Definitely | |
|
| ||||
| Overall, if it were an option, would you recommend using this specific technique (virtual reality) for this particular patient for future burn care? | 0% | 8.33% | 41.67% | 50% |
|
| ||||
| Very unsatisfied | Unsatisfied | Satisfied | Very satisfied | |
|
| ||||
| Overall, how satisfied were you in using virtual reality for this particular patient? | 0% | 0% | 58.33% | 41.67% |
Note. The statistics shown represent the frequency each response option was chosen (N=12).
3.2. Qualitative analysis
Results from the semi-structured interview were analyzed using a thematic, qualitative analysis as outlined by Braun and Clarke [25]. First, dictations from participant verbal responses during the interview were compiled and read several times by two of the authors (CF & EM) who double-coded all data. Next, all dictations were coded to identify the fundamental elements of each comment. Then, all the codes were grouped based on similarities to form overarching themes. Ultimately, four themes emerged from the data: (1) tolerance of procedure, (2) medical provider interactions, (3) logistical concerns, and (4) potential VR applications.
3.2.1. Tolerance of procedure
At some point during the interview, all participants described the VR experience as having some positive impact on their burn care procedure. Most participants (n=8) mentioned that VR distracted them from the burn care procedure. Some noted that VR was distracting because it gave them something else to direct attention to rather than the pain. For example, one participant stated:
“It was able to distract my mind from the pain even though I had a tough time paying attention to it because of the pain. It was a good distractor.”
Similarly, another participant remarked:
“The video competed for my attention.”
Participants also indicated that VR was distracting mainly because it prevented them from looking at the procedure. One participant stated:
“It closed off everything and I couldn’t see what was going on.”
Another burn survivor said:
“Virtual reality keeps your mind on something else instead of the dressing changes.”
In contrast, however, one participant remarked that he wanted to remove the mask at times to view his burn care procedure.
“I wanted to be able to look at what he was doing.”
This particular participant was unable to remove the VR mask himself because both of his hands were burned and being treated. Therefore, VR diverts visual attention away from the burn and its care procedure; however, some patients may view this as being helpful while others may see it as a potential drawback.
Additionally, participants indicated that their experience with VR was generally pleasant. Many participants (n=5) described the VR experience as being soothing, calming, or relaxing. In particular, the scuba diving application was typically described as being a soothing experience. For example, one participant stated that the diving and the water were “relaxing.” Another participant commented that water is a relaxing and peaceful thing. Patients also reported that they enjoyed the VR experience because the applications that they chose were related to one of their hobbies or to their personal goals. For instance, one participant enjoyed the scuba diving application because she swims to relieve stress at the end of her day.
Water is [a] relaxing and peaceful thing.
Another participant stated that he had a phobia of swimming in water, so he “chose it [scuba diving app] to be bold.” Similarly, participants enjoyed the novelty of the technology and immersive quality of VR. Thus, VR helped participants tolerate the burn care procedure because it helped to promote a state of relaxation and because the applications were related to participants’ personal interests.
3.2.2. Participant-provider interactions
Participants reported that the manner in which medical providers generally interact with patients affects their overall level of satisfaction with their care (e.g., explaining burn care procedures before performing them). Participants further mentioned a few important aspects of the participant-provider interactions that facilitated the use of VR in burn care. Namely, participants indicated appreciation for the voluntary aspect of taking part in the VR experience. In fact, one participant noted that that the friendliness of the staff and the fact that the staff members were not “pushy” on implementing VR was appreciated. Additionally, participants were grateful for the option to remove and restart the VR experience when desired. One participant conveyed that the virtual experience was made better because he was given the opportunity to take off the mask, as desired, thereby knowing he was “not stuck with the mask.” Ensuring the voluntary nature of participating in VR was a critical aspect of VR implementation according to participants.
Additionally, participants noted that the use of VR during burn care could be improved if the VR was introduced and delivered to participants more efficiently. That is, some participants raised concern that there may have been too many providers present during the VR and burn care procedure. Participants offered a few suggestions about how to implement VR more efficiently. One participant noted that communication between psychology staff (those researchers providing the VR) and medical staff (those providing medical care) could be improved. Another participant suggested that VR could be implemented more efficiently if the medical staff were familiar with its technology and could deliver VR as part of burn wound care (i.e., without additional assistance from research staff). Specifically, this participant stated:
“Someone could educate staff about what virtual reality is so that they can convey it to patients.”
3.2.3. Logistical concerns
Several participants discussed some logistical concerns with the VR equipment used. For example, one participant noted multiple times throughout the interview that that the equipment felt too bulky. Similarly, another participant felt that there were too many wires in the apparatus, adding that wireless headphones may make participants feel more comfortable. Also of note, one participant wore glasses while experiencing VR, which made it more uncomfortable to wear the VR mask. This participated reported:
“My glasses were moving around inside and I felt like I had to hold them in place.”
Thus, VR in burn care could be improved if the apparatus was better equipped for individuals with glasses.
Additionally, participants expressed logistical concerns about the specific VR applications and videos used in the study. Though participants were given the option to choose between eight VR applications, half of the participants indicated that the VR experience could be improved if participants were given more variety. For example, participants desired more VR options and more personalization in their VR choices. Participants (n=4) also reported that some of the VR videos were too brief in duration, causing the experience to involve pausing and restarting a new application. Some specific comments related to this concern were as follows:
“I didn’t like restarting it.”
“I got into it, but then the scene changed too soon.”
“The roller coaster was good but too short. It ended and I felt pain. Instantly, my mind went back to pain.”
Thus, it seems that increasing the variety of applications and their duration could enhance the feasibility, acceptability, and effectiveness of VR.
Lastly, participants had mixed opinions as to whether the audio component of the VR experience was helpful or detrimental. That is, three participants indicated that the music was an integral part of the VR experience. These participants described the audio and the headphones as adding to the immersive nature of VR. A participant noted:
“Music made the video come alive.”
However, two other participants expressed some concern that they were not able to hear the medical provider well during burn care because of the headphones. These two participants reported preferring to have the ability to hear the medical team during burn care procedures, and that that audio component of the VR interfered with these interactions. One of these participants summarized the issue:
“I liked the headphones and think it’s better to wear them, but I did have to take one off to talk to the doctor, but it was still helpful to encapsulate me.”
In contrast, one participant who wore the headphones throughout the VR experience noted:
“I like being able to talk with the doctor and to listen to him, so he can explain what he is doing. I wore the headphones the whole time but I could still hear the doctor.”
Along similar lines, another participant reported that she could still hear the VR audio although she was not wearing the headphones. She specifically suggested that perhaps “an external speaker is best” so that participants can hear both the VR application and the medical provider.
3.2.4. Future directions for VR
Six participants described enthusiasm for the use of VR in burn care by recommending other settings in which VR could be utilized. Participants believed that VR could be especially useful in pediatric burn care. Participants thought that children could be effectively distracted from burn care procedures using VR, especially if VR applications involved cartoons. One patient stated:
“Definitely use it with kids.”
Other participants stated that VR in burn care could be improved if it were more available to patients. For example, one participant recommended the following:
“Virtual reality should be kept in all rooms as an option for patients.”
Nevertheless, there were mixed opinions as to whether VR would be recommended for individuals with very large or extremely painful burns. One patient reported:
“It might be more effective with bigger burns.”
Another participant stated:
“I don’t know how I would react with more pain. Might’ve been irritating.”
4. Discussion
VR technology, which can efficaciously provide acute pain relief via distraction in burn care and other settings (e.g., Refs. [16,21,26]), has become more accessible with recent advances in technology (e.g., Ref. [22]). Consequently, a relatively simple VR setup (e.g., iPod, GC apparatus, and VR application) has the potential to be easily integrated into medical settings where distressing pain frequently is experienced. For this study of adult outpatients undergoing painful routine burn care, results suggest promise for the use of such low-cost VR technology to achieve pain-relieving distraction during wound debridement and/or dressing change. Importantly, results further suggest use of the VR technology also has little to no impact on delivery of usual burn care. Thus, this mixed methods pilot study provides initial support for the feasibility, acceptability, and effectiveness for the use of inexpensive and accessible VR technology as an adjunct strategy for pain management during routine burn care.
Quantitative and qualitative analysis of patient and provider data regarding the impact of VR use in burn care provided an indirect measure of effectiveness. Similar to findings of studies involving much more complex and costly VR setups [27], a majority (i.e., 90%) of patient participants of this study experienced distraction when using the low-cost VR technology, with 60% achieving meaningful associated pain reduction. This result is consistent with a growing body of literature suggesting VR is efficacious and effective for acute pain management, generally (see Refs. [28,29] for systematic reviews), and provides additional evidence for potential analgesic benefit.
Still, while all patient participants described the VR technology as having some positive impact on their burn care experience, not all found the intervention to offer analgesia. In those cases, it may have been that the VR did not offer sufficient or persistent distraction. Increasing the level of immersion in VR may improve outcomes for these patients (e.g., Ref. [29]). For instance, magnitude of interactivity [30], including the illusion of presence [31], can affect the degree to which pain experience is influenced by use of VR. Though low-cost VR technology in its current form may not provide ample immersion for all patients, it may be possible to increase the immersion and distraction by giving patients the opportunity to choose a virtual environment that is most interesting and/or pleasing (as was done in this study) and to allow them to trial different environments to find the one that demands the most attention. Though yet to be determined, specific VR applications may be particularly effective in providing optimal distraction via immersion or some other characteristic(s) as a function of match with patient factors. For example, applications that afford patients’ perceived control may be especially immersive and thus more effective than others. Those same applications may be even more effective for patients with a preference for control in anxiety-provoking or otherwise uncertain situations, given the role perceived control and locus of control can have in coping with acute/procedural pain and other stressful aspects of medical care (e.g., Refs. [32,33]). While beyond the scope of this study, determining which existing VR applications are most effective (and why) and/or developing new VR applications with pain management efficacy in mind will be an important next step in this line of research.
Sound has been described as one variable that increases immersion and the distracting effects of VR [34]; however, participants of this study reported mixed opinions about whether the audio component of the VR experience was important for the effectiveness of the intervention. Some patients may find attention-consuming sound from noise cancelling headphones to make VR more immersive and effective, but others may prefer to hear or even communicate with the medical team during a procedure. Thus, it is important to consider patient preferences for VR-related audio to ensure effectiveness and ultimate utility. Similarly, it may be important to consider providers’ preferences regarding the use of sound as distraction during burn care. Some providers may be less amenable to the use of sound during burn care because sound may limit or negatively impact patient-provider interactions and communication. Future research is necessary to determine the provider acceptability of the use of sound as a component of VR technology for distraction during burn care.
All but one patient indicated they would be likely or very likely to use VR during their next burn care procedure, and all patients reported that they would recommend use of VR to another patient, demonstrating both effectiveness and acceptability. Indeed, there generally was a high degree of acceptability of the low-cost VR technology as rated and discussed by patient and medical provider participants. Specifically, all patients and providers were satisfied or very satisfied with the VR experience, and it seems that enjoyment and acceptability were bolstered by the voluntary and personalized nature of the protocol’s implementation. For example, participants appreciated the freedom to use the VR technology when and how they wanted as well as the opportunity to select a virtual environment that matched their personal interests, certainly making the intervention palatable.
Acceptability may be poor, however, when the use of VR is not well matched to patient preferences about involvement in care and/or desire to consume health information. For instance, some patients may experience an increase in anxiety if they are unable to see and/or hear while a medical procedure is being completed, and thus may find an intervention such as the one used here to be iatrogenic and thus unacceptable. It is important to consider patient preferences in determining whether VR for anxiety and pain management is indicated and appropriate. In the spirit of treatment acceptability, it also may be useful to offer patients the option to remove the VR mask or to otherwise participate in care. Likewise, as referenced by some participants, acceptability of and satisfaction with the use of VR technology are secondary to the way in which providers engage in interpersonal interactions with patients, providers’ familiarity/comfort with the technology and the associated efficiency of implementation, and providers’ insistence that use of the technology for pain management is voluntary.
From both patient and provider perspectives, it was generally feasible to use low-cost VR technology during routine burn care. All patients were able to use the VR technology while burn care was completed, and there were no significant problems with use. Still, results suggest feasibility from the patient standpoint may be impacted by bulky equipment and presence of wires, so choosing an apparatus that is as streamlined as possible is optimal. Additionally, special consideration should be given to patients who wear glasses to ensure proper fit of the apparatus and comfortable access to the technology. Selecting VR applications that have long enough videos to provide distraction through an entire procedure also may be a critical issue for patient feasibility. A key finding of the study was that all providers indicated use of the VR technology had no impact on their ability to carry out the burn care procedure, and results suggest that uptake by the clinic was good, demonstrating feasibility from the provider standpoint. Of note, psychology research staff who were familiar with the VR apparatus, specifically, and VR for distraction and pain management, generally, introduced and administered VR to the patients. Therefore, it remains unknown whether or not patient perceptions of VR utility would differ if patients were introduced to VR by the medical provider, or whether provider perceptions potentially could impact patient acceptability. That being said, it is recommended that providers who wish to use VR during burn care first familiarize themselves with the technology and apparatus before introducing VR to patients. Additionally, familiarizing providers with the potential benefits of VR during burn care is likely to increase uptake and use of low cost VR. Of course, use of this or similar technology in an outpatient setting should be adapted specifically for each clinic so that it can be successfully adopted for patient pain relief without interfering with medical care.
Limitations of the current study include sampling from only one clinic and enrolling only adult participants, which may limit the generalizability of findings. Additionally, the study involved a relatively small sample of providers, so further work is necessary to establish more definitively that use of low-cost VR technology in an outpatient burn clinic is widely acceptable and feasible at the provider level. Furthermore, participants were not asked whether or not they had prior experience with VR. Future research involving VR should inquire about prior VR use, as one’s degree of experience with VR may affect its utility for pain management. Lastly, the study was focused on outpatients, so it is not possible to make firm inferences about how low-cost VR technology could be used on inpatient burn units given the unique characteristics of those settings.
Future studies should address these limitations to expand on this pilot work. For example, to more comprehensively assess the providers’ acceptability of VR in burn care, future research might employ a qualitative research design and sample from a variety of provider types (nurses, physician’s assistants, physicians, etc.). Such a study would provide detailed insight as to whether acceptability of VR varies as a function of provider type and could guide more widespread implementation of low-cost VR. Furthermore, the literature would benefit from future studies that: include pediatric patients; assess degree of immersion and associated pain relief provided by use of low-cost VR technology; identify specific applications that provide optimal distraction or result in the development of new applications tailored to the clinical problem; address how use of the technology is implemented in clinics and whether there is adequate uptake by patients and providers; determine whether the technology can provide pain management for other treatments (e.g., physical therapy [21]) and/or in similar (i.e., non-burn) settings; and, whether other, adjunctive psychological strategies (e.g., hypnosis, a la [35]) can be paired with VR intervention to further enhance analgesia, anxiety reduction, and/or general coping. Moreover, once the use of low-cost VR therapy in routine burn care is further supported in larger scale randomized controlled trials, future research might explore patient characteristics (e.g., coping style) that may moderate treatment effectiveness.
This study provides early, promising evidence that low-cost VR technology can be harnessed for pain relief via distraction. Importantly, for both patients and providers, acceptability of the technology and feasibility of its use were established. Given that such technology now is easy to procure and use — a noteworthy strength — it can be used as an adjunctive to routine burn care when pain management is an issue and where other VR systems are cost prohibitive. Thus, providers working in outpatient burn clinics might consider whether their patients may benefit from VR-driven distraction for pain relief, particularly given that low-cost VR technology is so accessible, and especially as future research refines recommendations for its use.
Acknowledgments
The authors gratefully acknowledge the time and effort of the patients and medical providers who took part in this stakeholder-engaged project. They also appreciate the assistance of Sarah Hayes Addicks, MPH, MA, who helped to develop this project.
Appendix A
Footnotes
Conflict of interest
The authors have no conflict of interest to declare.
References
- 1.Latarjet J, Choinere M. Pain in burn patients. Burns. 1995;21(5):344–8. doi: 10.1016/0305-4179(95)00003-8. [DOI] [PubMed] [Google Scholar]
- 2.Summer GJ, Puntillo KA, Miaskowski C, Green PG, Levine JD. Burn injury pain: the continuing challenge. J Pain. 2007;8(7):533–48. doi: 10.1016/j.jpain.2007.02.426. doi: http://dx.doi.org/10.1016/j.jpain.2007.02.426. [DOI] [PubMed] [Google Scholar]
- 3.Patterson DR, Tininenko J, Ptacek JT. Pain during burn hospitalization predicts long-term outcome. J Burn Care Res. 2006;27(5):719–26. doi: 10.1097/01.BCR.0000238080.77388.FE. doi: http://dx.doi.org/10.1097/01.bcr.0000238080.77388.fe. [DOI] [PubMed] [Google Scholar]
- 4.Ptacek JT, Patterson DR, Montgomery BK, Heimbach DM. Pain, coping, and adjustment in patients with burns: preliminary findings from a prospective study. J Pain Symptom Manag. 1995;10(6):446–55. doi: 10.1016/0885-3924(95)00083-b. [DOI] [PubMed] [Google Scholar]
- 5.Montgomery GH, DuHamel KN, Redd WH. A meta-analysis of hypnotically induced analgesia: how effective is hypnosis? Int J Clin Exp Hypn. 2000;48:138–53. doi: 10.1080/00207140008410045. [DOI] [PubMed] [Google Scholar]
- 6.Patterson DR, Jensen MP. Hypnosis and clinical pain. Psychol Bull. 2003;129:495–521. doi: 10.1037/0033-2909.129.4.495. [DOI] [PubMed] [Google Scholar]
- 7.Patterson DR, Everett JJ, Burns GL, Marvin JA. Hypnosis for the treatment of burn pain. J Consult Clin Psychol. 1992;60:713–7. doi: 10.1037//0022-006x.60.5.713. [DOI] [PubMed] [Google Scholar]
- 8.Everett J, Patterson D, Chen AC. Cognitive and behavioural treatments for burn pain. Pain Clin. 1990;3(3):133–45. [Google Scholar]
- 9.Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol Bull. 1999;125(3):356–66. doi: 10.1037/0033-2909.125.3.356. [DOI] [PubMed] [Google Scholar]
- 10.Ploghaus A, Narain C, Beckmann CF, Clare S, Bantick S, Wise R, et al. Exacerbation of pain by anxiety is associated with activity in a hippocampal network. J Neurosci. 2001;21(24):9896–903. doi: 10.1523/JNEUROSCI.21-24-09896.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwekkeboom KL. Music versus distraction for procedural pain and anxiety in patients with cancer. Oncol Nurs Forum. 2003;30(3):433–40. doi: 10.1188/03.ONF.433-440. doi: http://dx.doi.org/10.1188/03.onf.433-440. [DOI] [PubMed] [Google Scholar]
- 12.Madson AT, Silverman MJ. The effect of music therapy on relaxation, anxiety, pain perception, and nausea in adult solid organ transplant patients. J Music Ther. 2010;47(3):220–32. doi: 10.1093/jmt/47.3.220. [DOI] [PubMed] [Google Scholar]
- 13.Aitken JC, Wilson S, Coury D, Moursi AM. The effect of music distraction on pain, anxiety and behavior in pediatric dental patients. Pediatr Dent. 2002;24(2):114–8. [PubMed] [Google Scholar]
- 14.Association NAaS. Virtual reality: definition and requirements. Secondary virtual reality: definition and requirements. 2015 https://www.nas.nasa.gov/Software/VWT/vr.html.
- 15.Hoffman HG, Patterson DR, Carrougher GJ, Sharar SR. Effectiveness of virtual reality-based pain control with multiple treatments. Clin J Pain. 2001;17(3):229–35. doi: 10.1097/00002508-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Hoffman HG, Garcia-Palacios A, Patterson DR, Jensen M, Furness T, 3rd, Ammons WF., Jr The effectiveness of virtual reality for dental pain control: a case study. Cyberpsychol Behav. 2001;4(4):527–35. doi: 10.1089/109493101750527088. doi: http://dx.doi.org/10.1089/109493101750527088. [DOI] [PubMed] [Google Scholar]
- 17.Jeffs D, Dorman D, Brown S, Files A, Graves T, Kirk E, et al. Effect of virtual reality on adolescent pain during burn wound care. J Burn Care Res. 2014;35(5):395–408. doi: 10.1097/BCR.0000000000000019. doi: http://dx.doi.org/10.1097/bcr.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 18.Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. 2008;24(4):299–304. doi: 10.1097/AJP.0b013e318164d2cc. doi: http://dx.doi.org/10.1097/AJP.0b013e318164d2cc. [DOI] [PubMed] [Google Scholar]
- 19.van Twillert B, Bremer M, Faber AW. Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. J Burn Care Res. 2007;28(5):694–702. doi: 10.1097/BCR.0B013E318148C96F. doi: http://dx.doi.org/10.1097/bcr.0b013e318148c96f. [DOI] [PubMed] [Google Scholar]
- 20.Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. Clin J Pain. 2000;16(3):244–50. doi: 10.1097/00002508-200009000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Sharar SR, Carrougher GJ, Nakamura D, Hoffman HG, Blough DK, Patterson DR. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: preliminary results from 3 ongoing studies. Arch Phys Med Rehabil. 2007;88(12 Suppl 2):S43–9. doi: 10.1016/j.apmr.2007.09.004. doi: http://dx.doi.org/10.1016/j.apmr.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 22.Hoffman HG, Meyer WJ, 3rd, Ramirez M, Roberts L, Seibel EJ, Atzori B, et al. Feasibility of articulated arm mounted Oculus Rift Virtual Reality goggles for adjunctive pain control during occupational therapy in pediatric burn patients. Cyberpsychol Behav Soc Netw. 2014;17(6):397–401. doi: 10.1089/cyber.2014.0058. doi: http://dx.doi.org/10.1089/cyber.2014.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Google. Google cardboard. Secondary Google cardboard. 2017 https://vr.google.com/cardboard/
- 24.Apple. Apple iTouch. Secondary Apple iTouch. 2017 https://www.apple.com/ipod-touch/
- 25.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 26.Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin J Pain. 2014;30(12):1089–98. doi: 10.1097/AJP.0000000000000064. doi: http://dx.doi.org/10.1097/ajp.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 27.Hoffman HG, Chambers GT, Meyer WJ, 3rd, Arceneaux LL, Russel WJ, Seibel EJ, et al. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Ann Behav Med. 2011;41(2):183–91. doi: 10.1007/s12160-010-9248-7. doi: http://dx.doi.org/10.1007/s12160-010-9248-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev. 2010;30:1011–8. doi: 10.1016/j.cpr.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Shahrbanian S, Ma X, Korner-Bitensky N, Simmonds MJ. Scientific evidence for the effectiveness of virtual reality for pain reduction in adults with acute or chronic pain. Stud Health Technol Inform. 2009;144:40–3. [PubMed] [Google Scholar]
- 30.Wender R, Hoffman HG, Hunner HH, Seibel EJ, Patterson DR, Sharar SR. Interactivity influences the magnitude of virtual reality analgesia. J Cyber Ther Rehabil. 2009;2(1):27–33. [PMC free article] [PubMed] [Google Scholar]
- 31.Hoffman HG, Richards T, Coda B, Richards A, Sharar SR. The illusion of presence in immersive virtual reality during an fMRI brain scan. Cyberpsychol Behav. 2003;6(2):127–31. doi: 10.1089/109493103321640310. doi: http://dx.doi.org/10.1089/109493103321640310. [DOI] [PubMed] [Google Scholar]
- 32.Rudolph KD, Dennig MD, Weisz JR. Determinants and consequences of children’s coping in the medical setting: conceptualization, review, and critique. Psychol Bull. 1995;118:328–57. doi: 10.1037/0033-2909.118.3.328. [DOI] [PubMed] [Google Scholar]
- 33.Young KD. Pediatric procedural pain. Ann Emerg Med. 2005;45:160–71. doi: 10.1016/j.annemergmed.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 34.Johnson S, Coxon M. Sound can enhance the analgesic effect of virtual reality. R Soc Open Sci. 2016;3(3):150567. doi: 10.1098/rsos.150567. doi: http://dx.doi.org/10.1098/rsos.150567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patterson DR, Jensen MP, Wiechman SA, Sharar SR. Virtual reality hypnosis for pain associated with recovery from physical trauma. Int J Clin Exp Hypn. 2010;58:288–300. doi: 10.1080/00207141003760595. [DOI] [PMC free article] [PubMed] [Google Scholar]


