Abstract
A biopsy specimen from the nasal mucosa of a 37-year-old man disclosed a subepithelial accumulation of black granules mainly running parallel to the surface in the absence of any inflammatory infiltrate. Since the mucosal pigment was negative with Perls’ stain and resisted to melanin bleach, an exogenous pigmentation was suspected. The biopsy specimen had been taken because of a diffuse steel-blue pigmentation of the nasal mucosa, incidentally discovered during routine clinical examination. A diagnosis of occupational argyria of the nasal mucosa was finally made since the patient was a silver cleaner. Argyria is a rare cause of nasopharyngeal mucosal pigmentation; it is not a precancerous condition, but it can be mistaken for a melanosis or a melanocytic tumor both clinically and histopathologically. Clinicopathological correlation is mandatory, since the final diagnosis is based on a history of chronic silver exposure.
Keywords: Nasal cavity, Argyria, Histopathology, Pigment
Background
Localized and generalized argyria are rare conditions in which a lifelong steel-gray pigmentation of the skin and/or the mucosa membrane is found as a result of occupational or pharmacological exposure to silver or silver compounds. Since silver accumulation in the nasal mucosa is much rarer than other types of mucosal pigmentation, the histopathological diagnosis of nasal argyria can be very challenging and clinicopathological correlation is mandatory.
Case Presentation
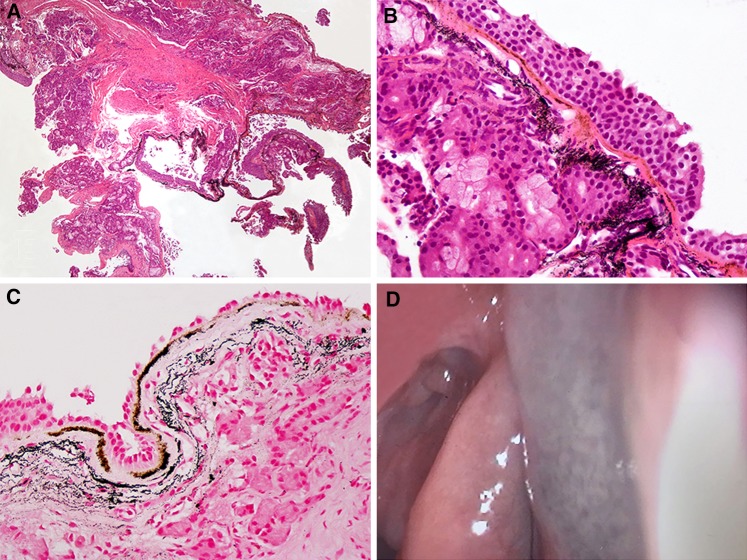
A biopsy specimen taken during routine outpatient clinical examination in a 37-year-old man was sent to our Pathology department with a clinical working diagnosis of ‘pigmented nasal mucosa: rule out melanoma’. The histopathologic picture (Fig. 1a, b) featured striking extracellular deposits of granules, lying both as a brownish band parallel to the mucosal surface and as a diffuse black granular hue in the absence of any inflammatory infiltrate. The pigment was negative to Perls’ stain (Fig. 1c) for iron and resisted to melanin bleach with potassium permanganate–oxalic acid; thus an exogenous pigmentation was histopathologically suspected.
Fig. 1.
a Histopathological picture featuring an extensive subepithelial deposition of pigment. b The mucosal pigmentation characterized by a brownish subepithelial band associated with deeper diffuse cloud-like black granular deposits. Of note is the absence of any inflammatory cell infiltrate. c The same features as in (b), with Perls’ stain
The patient was then referred to a new clinical examination: rhynoscopy disclosed a diffuse steel-gray pigmentation of the anterior part of the nose (Fig. 1d) and, since the patient had been working as a silver cleaner for about 15 years, a final diagnosis of occupational argyria was made.
Discussion
Pigment accumulation within the nasal mucosa may be ascribed to several clinicopathological entities, as shown in Table 1. As a rule of the thumb, an exogenous pigmentation may be suspected if the pigment seen on routinely stained tissue sections resists to melanin bleach and is negative to Perls’ stain for iron; and once endogenous pigmentation has been excluded, clinicopathological correlation is mandatory in order to establish the final etiologic diagnosis.
Table 1.
Clinicopathologic conditions associated with pigmentation of the nasal mucosa
| Pigment | Histologic features | Localized | Generalized |
|---|---|---|---|
| Hemosiderina | Granular/crystalline, refractile golden to yellow–brown; positive with Perls’s stain | Gross or minute hemorrhages | Hemochromatosis |
| Melanina | Finely granular, pale to dark brown; stained in black with Fontana-Masson and in black with Schmorl methods; bleached with potassium permanganate–oxalic acid or with hydrogen peroxide | Lentigo, nevi (comprising nevus of Ota), and melanoma | Addison’s disease; Peutz-Jegher’s disease |
| Lipofuscina | Finely granular, yellow–brown, intracytoplasmic (often perinuclear); PAS-positive; variably acid-fast | Aging-related change | |
| Goldb | Relatively large and irregular round–oval black granules, mainly within macrophages; orange–red birefringence on polarized light | Not reported | Systemic drug therapy (usually intramuscular injections) with gold-containing compounds |
| Silverb | Small brown–black granules in a ‘band-like’ deposition; stained in reddish-brown with rhodamine on frozen sections | Occupational; topical silver-containing drugs | Systemic drug therapy with silver-containing compounds |
| Mercuryb | Very small, brown–black refractile particles within macrophages and around blood vessels | Exposure to mercury vapors | Systemic drug therapy with mercury-containing compounds; chronic poisoning (infantile acrodynia) |
| Bismuthb | Small carbon-like particles | Not reported | Systemic drug therapy with bismuth-containing compounds |
aEndogenous pigmentation
bExogenous pigmentation
Argyria is the result of a chronic exposure to silver compounds in either medical or industrial settings and is characterized by permanent bluish-black discoloration of the skin and/or the mucous membranes. Generalized argyria arises after a total dose of 6 g p.o. or 1 g i.v. [1]: characteristically, the sun-exposed areas of the face and upper limbs develop a dark slate-grey color, which is uniform in distribution and varies in depth depending on the degree of the exposure. Slit lamp examination of eye appears to be the best method to measure body burden to silver, whereas blood silver levels appear to reflect recent exposure only [2]. Silver can also accumulate in the liver, the spleen, and the kidneys [3], but such an accumulation probably does not cause any organ failure [4]. There are also isolated reports of associating silver exposure and neuropathy [5].
Drug-induced argyria was thought to be a clincopathological entity going to disappear after withdrawal of silver-containing oral compounds. However, silver can also penetrate through the skin and the mucous membranes after prolonged exposure to silver-containing local antiseptics, nasal drops, dental amalgam, absorbable sutures, and acupuncture needles. In such cases, silver absorption does not primarily follow the systemic route; thus clinical signs of argyria are confined, at least at the beginning, within the site of exposure (local argyria) [6].
Occupational argyria may be systemic or localized as well. Extensive silver deposition in the nasal mucosa can be found in silver refiners and solderers, silver nitrate, silverware, tableware, coins, and jewelry manufacturers, producers of electrical apparatus, mirrors, indelible inks, hair dyeing, porcelain coloring, ivory etching, and silver alloys [7]. Histopathological examination shows an accumulation of brown-black granules with no appreciable inflammatory infiltrate; such granules lie in compact bands parallel to the mucosal surface and/or in black cloud-like aggregates close to the surface. The basic requirements to identify such granules as an exogenous pigment are their Perls’ stain negativity plus their persistence after tissue section bleaching. Exogenous granules can be suspected as silver because of:
Their size: they are smaller than gold and larger than mercury deposits;
Their location: they are free within the connective tissues, whereas gold and mercury particles are mainly found within macrophages.
The direct identification of silver on tissue sections can be achieved with rhodamine stain on frozen sections, with silver granules appearing as reddish-brown [8], and/or with X-ray microanalysis [1, 9]. Both techniques, however, may be not feasible: thus, a detailed history of drug and/or industrial exposure is the easy and inexpensive mainstay for the final diagnosis. There are no safe ways of removing the mucosal pigmentation; on the other hand, excessive silver absorption does not appear to produce any conclusive and recognizable disturbance of health, probably because of the silver binding with selenide and sulfide [9, 10]. In spite of sporadic harmful reports [11], there seems to be no association of silver accumulation with an increased risk of oral-nasopharyngeal cancer [12]. Nevertheless the diagnosis is important in order to stop using silver-containing drugs and/or to ensure that workplace occupational exposure standards are met.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from the patient included in the study.
Research Involving Animal Participants
This article does not contain any studies with animals performed by any of the authors.
Contributor Information
Gerardo Ferrara, Phone: +3907332572460, Email: gerardo.ferrara@libero.it.
Alessandra Filosa, Email: alessandrafilosa@yahoo.it.
Maria Paola Mariani, Email: paola.mariani@sanita.marche.it.
Luigi Fasanella, Email: luigi.fasanella@sanita.marche.it.
References
- 1.Bleehen SS, Gould DJ, Harrington CI, et al. Occupational argyria; light and electron microscopic studies and X-ray microanalysis. Br J Dermatol. 1981;104:19–26. doi: 10.1111/j.1365-2133.1981.tb01706.x. [DOI] [PubMed] [Google Scholar]
- 2.Armitage SA, White MA, Wilson HK. The determination of silver in whole blood and its application to biological monitoring of occupationally exposed groups. Ann Occup Hyg. 1996;40:331–338. doi: 10.1016/0003-4878(95)00076-3. [DOI] [PubMed] [Google Scholar]
- 3.Cho EA, Lee WS, Kim KM, Kim SY. Occupational generalized argyria after exposure to aerosolized silver. J Dermatol. 2008;35:759–760. doi: 10.1111/j.1346-8138.2008.00562.x. [DOI] [PubMed] [Google Scholar]
- 4.Pifer JW, Friedlander BR, Kintz RT, Stockdale DK. Absence of toxic effects in silver reclamation workers. Scand J Work Environ Health. 1989;15:210–221. doi: 10.5271/sjweh.1860. [DOI] [PubMed] [Google Scholar]
- 5.Vik H, Andersen KJ, Julshamin K, et al. Neuropathy caused by silver aborption from arthroplasty cement. The Lancet. 1985;1:872. doi: 10.1016/S0140-6736(85)92230-5. [DOI] [PubMed] [Google Scholar]
- 6.Sarsfueld P, White JE, Theaker JM. Silverworker’s finger: an unusual occupational hazard mimicking a melanocytic lesion. Histopathology. 1992;20:73–75. doi: 10.1111/j.1365-2559.1992.tb00921.x. [DOI] [PubMed] [Google Scholar]
- 7.Rosenman KD, Moss A, Kon S. Argyria: clinical implications of exposure to silver nitrate and silver oxide. J Occup Med. 1979;21:430–435. [PubMed] [Google Scholar]
- 8.Churukian CP. Pigment and minerals. In: Bancroft JD, Gamble M, editors. Theory and practice histological techniques. 8th ed. Philadelphia: Churchill-Livingstone Elsevier. pp 257–8.
- 9.Matsumura T, Kumakiri T, Ohkawara A, et al. Detection of selenium in generalized and localized argyria: report of four cases with X-ray microanalysis. J Dermatol. 1992;19:87–93. doi: 10.1111/j.1346-8138.1992.tb03186.x. [DOI] [PubMed] [Google Scholar]
- 10.Humphreys SDM, Routledge PA. The toxicology of silver nitrate. Advers Drug React Toxicol Rev. 1998;178:115–143. [PubMed] [Google Scholar]
- 11.Stammberger H. Argyrosis of the nasal mucosa. Laryng Rhinol Otol. 1982;61:234–237. doi: 10.1055/s-2007-1008563. [DOI] [PubMed] [Google Scholar]
- 12.Williams N. Longitudinal medical surveillance showing lack of progression of argyrosis in a silver refiner. Occup Med. 1999;49:397–399. doi: 10.1093/occmed/49.6.397. [DOI] [PubMed] [Google Scholar]