Abstract
Ectopic hamartomatous thymoma (EHT) is a rare benign neoplasm of the lower neck suggesting branchial origin. Despite use of the term thymoma in the nomenclature, there is no evidence of thymic origin or differentiation. It affects middle-aged adults with a remarkable male predominance. To date less than 80 cases have been reported in the English literature. We present here two additional cases of EHT. The first is a benign case in a 31-year-old man, showing typical histological features. The second is a malignant case in a 70-year-old woman, showing intraductal carcinoma arising in intimate association with an EHT. These cases are presented in the context of a review of cases reported in the English literature. The exact origin has not been identified, but is considered to be of branchial apparatus, creating a quandary about the best terminology. Recently, the designation “branchial anlage mixed tumor” or “thymic anlage tumor” were proposed, but do not quite reflect the true nature of the neoplasm. To avoid taxonomic confusion, international consensus on terminology is desired. As this entity is a neoplasm that shows dual mesoderm and endoderm derivation/differentiation, we propose a new name “biphenotypic branchioma.”
Keywords: Ectopic hamartomatous thymoma, Biphenotypic branchioma, Carcinoma, Branchial pouch, Head and neck, Soft tissue
Introduction
Ectopic hamartomatous thymoma (EHT) is a rare benign neoplasm that almost exclusively occurs in the lower neck area of adult patients with a remarkable male predominance [1]. Histologically, EHT is characterized by an admixture of spindle cells, epithelial islands, and adipocytes. Since the first description in 1982 by Smith and McClure [2] and recognition as a disease entity by Rosai et al. [3], 77 cases have been reported in the English literature [2–38]. We herein describe two additional cases of EHT, one benign and one malignant, and present the clinicopathological and immunohistochemical characteristics. We also reviewed all previously reported EHT in the English literature, and address the recent discussion regarding the tumor nomenclature.
Case Reports
Case 1
A 31-year-old man presented with a 2-year history of a mass in the right lower neck. No other abnormal clinical symptoms or laboratory data were found. Physical examination revealed a well-defined mass in the right supraclavicular area. Ultrasonography showed a well-demarcated heterogeneous mass. The clinical impression included a lipoma, dermoid cyst, or some other neck mass. The patient underwent surgical resection of the tumor, and the postoperative course was uneventful, without disease at 1 year.
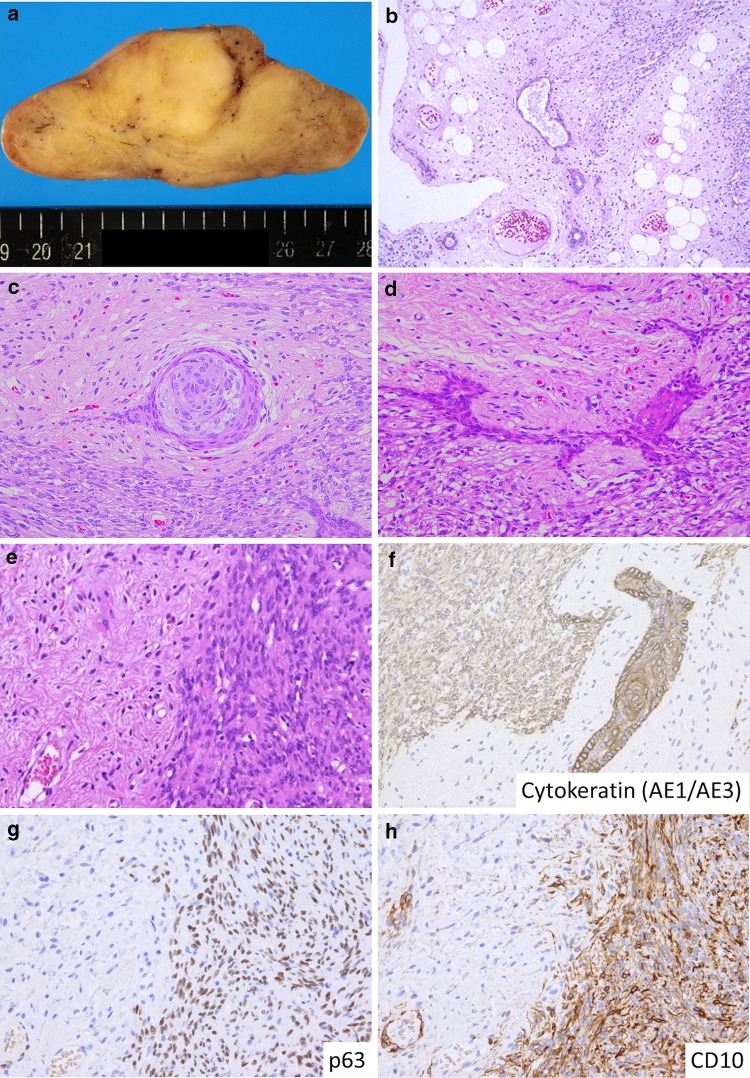
On gross examination, the mass was encapsulated and lobulated, measuring 9 × 6.5 × 4.3 cm. The cut surface was solid and yellowish (Fig. 1a). Microscopically, the tumor was composed of spindle and epithelial cells, and mature adipocytes (Fig. 1b). The nests of epithelial cells formed non-keratinizing squamoid islands or glandular structures (Fig. 1b–d). Two types of spindle cells were recognized, namely, plump and delicate (small) (Fig. 1e). The plump spindle cells proliferated in a fascicular pattern. These areas were densely cellular but without significant cellular atypia. The nuclear chromatin was fine, and nucleoli were indistinct. Delicate spindle cells found between the fascicles had small nuclei and scanty cytoplasm. Immunohistochemically, the plump spindle cells and epithelial cells were positive for cytokeratin (CK) (Fig. 1f), with the plump spindle cells also immunoreactive for smooth muscle actin, HHF-35, CK5/6, p63, p40, D2-40, and CD10 (Fig. 1g, h) while negative for desmin, S-100 protein, CD31, and SOX10. The delicate spindle cells were only positive for CD34 and vimentin.
Fig. 1.
"Case 1". a Grossly, the tumor was a well-circumscribed yellowish solid mass. b Histologically, the tumor was composed of an admixture of spindle cells, epithelial islands, and adipocytes. c Nonkeratinizing squamous cell nest with small glandular structure. d Squamous islands with anastomosing network. e Two types of spindle cells were observed. The plump cells in the right, and delicate cells in the left. f Cytokeratin was positive for epithelial islands and plump spindle cells, but not for delicate spindle cells. g, h Myoepithelial markers, such as p63 (g) and CD10 (h), were positive for plump spindle cells but negative for delicate cells
Case 2
The second case presented in the low midline-suprasternal notch area in a 70-year-old woman, who had no other symptoms and no history of other tumors. The tumor measured 3.5 × 2.5 × 0.8 cm. Microscopically, the tumor showed an intimate blending of two different processes. The first was an EHT. There was a very well marginated and circumscribed periphery to the lesion. There were numerous cysts lined by squamous and respiratory-type epithelium (Fig. 2a). There was no atypia to this epithelial lining (Fig. 2b). Several squamous cysts, inclusions and eddies were noted in the surrounding soft tissues, also lacking any atypia. There was a spindled shaped fascicular to storiform proliferation of unremarkable epithelioid spindle cells (Fig. 2b). There were islands of mature adipose tissue along with areas that showed mature lymphocytes. Blended with the EHT was an intraductal adenocarcinoma, showing a spectrum of changes that mimicked a breast lesion: typical ductal hyperplasia, atypical ductal hyperplasia, with a continuum to an increased degree of pleomorphism to yield an intraductal carcinoma that greatly expanded the ductal spaces (Fig. 2c–f). The areas of atypical intraductal proliferation coalesced and merged, expanding the ductal spaces and filling them with the more atypical population of neoplastic cells. Islands of atypical epithelium were noted distant from the rest of the lesion, interpreted to represent invasion. However, there was no desmoplastic stromal reaction or individual cell infiltration. The tumor showed a biphasic appearance, with a thin and attenuated layer of myoepithelial cells highlighted by the smooth-muscle actin, p63 and p40 at the periphery, surrounding the atypical luminal epithelial cells (Fig. 2h). There was a ‘Roman Bridge’ appearance in some areas, micropapillary architecture in others, and more of a glandular appearance to the rest of the lesion. These epithelial cells were enlarged, with an increased nuclear to cytoplasmic ratio. The cytoplasm was eosinophilic to opacified to focally vacuolated. Granular cytoplasm was noted in some areas (Fig. 2g), while more opacified in others. Mucicarmine positive vacuoles were noted. The nuclei were irregular with coarse nuclear chromatin and prominent, easily identified nucleoli (Fig. 2e, f). There were apocrine features, with luminal cytoplasmic blebs. While pleomorphism was present, it was not profound. Mitoses were low, with only 1 per 10 high power fields, complemented by a 2% Ki-67 index. Tumor necrosis was not appreciated. The spindled cells within the EHT were strongly immunoreactive with MSA androgen receptor, while the intraductal carcinoma was also positive with androgen receptor but negative with S-100 protein. The patient is alive, although with less than 1 year of follow-up.
Fig. 2.
"Case 2". a Low-power view of the tumor showed numerous cysts lined by squamous and respiratory-type epithelium. b There was no atypia to this epithelial lining. The spindle cell component of ectopic hamartomatous thymoma was also observed. c Low-power view of the carcinoma area. d Adenocarcinoma component, showing relatively low-grade atypia. e Adenocarcinoma, showing papillary and glandular patterns. The cancer cells showed prominent nucleoli. f Adenocarcinoma, showing solid and cribriform patterns. g Some tumor cells had granular cytoplasm. h Immunohistochemical stain of smooth muscle actin highlightened myoepithelial cells around the atypical luminal epithelial cells
Discussion
"Case 1" showed typical clinical and morphological features of EHT. Histologically, the tumor was composed of an admixture of spindle cells, epithelial islands, and adipocytes. Two types of spindle cells were observed as previously reported [22]. The epithelial nature of plump spindle cells was demonstrated by the strong and diffuse positivity for CK. The plump spindle cells also stained positively for myoepithelial markers, such as CK5/6, p63, p40, D2-40, and CD10. These findings indicate that EHT is a tumor composed of epithelial and myoepithelial cells, while other myoepithelial and neuroectodermal markers, such as S-100 protein and SOX10, were absent.
"Case 2" demonstrated an intraductal adenocarcinoma arising within an EHT. Malignancy arising in EHT is extremely rare, with only three cases previously reported (Table 1) [10–12]. The adenocarcinoma component in our case mimicked intraductal carcinoma of the breast (ductal carcinoma in situ). The degree of pleomorphism of the tumor cells was variable within the tumor, with several areas showing well developed glandular differentiation, similar to findings reported by Michal et al. [12].
Table 1.
Clinicopathological features of reported ectopic hamartomatous thymoma (in English)
| Reference | Age/sex | Location | Size (cm) | Comments |
|---|---|---|---|---|
| Smith et al. [2] | 55/F | L supraclavicular area | 8.0 | |
| Rosai et al. [3] | 35/M | L supraclavicular area | 4.0 | |
| 26/M | L supraclavicular area | 6.0 | ||
| 40/M | Suprasternal area | 2.0 | ||
| 55/F | L supraclavicular area | 8.0 | ||
| 43/F | R supraclavicular area | 5.0 | ||
| Fetsch et al. [4] | 79/M | Superior chest wall sternoclavicular joint | 19.0 | |
| 38/M | Beneath SCM, above medial clavicle | 5.5 | ||
| 37/M | Superficial sternoclavicular joint | 3.5 | ||
| 65/M | Superficial sternoclavicular joint | 10.0 | ||
| Saeed et al. [5] | 42/M | Surprasternal area | 5.0 | |
| Kim et al. [6] | 49/M | Above the sternal notch | 5.0 | |
| Chan et al. [7] | 66/M | Surprasternal area | 7.0 | |
| 58/M | Surprasternal area | na | ||
| 47/M | L supraclavicular area | 3.8 | ||
| Adult/M | Supraclavicular area | 3.0 | ||
| 68/M | L sternoclavicular area | 3.0 | ||
| Armour et al. [8] | 47/M | L supraclavicular area | 3.8 | |
| Doctor et al. [9] | 49/F | Suprasternal area | 2.4 | |
| Michal et al. [10–12] | 31/M | R supraclavicular area | 6.0 | Adenocarcinoma |
| 39/M | R supraclavicular area | 5.5 | Adenocarcinoma | |
| 38/M | Suprasternal area | 3.0 | ||
| 36/M | Suprasternal area | 1.5 | Resembling squamous cell carcinoma with a spindle cell component | |
| Eulderink et al. [13] | 27/M | Presternal area | 3.5 | |
| Hirokawa et al. [14] | 63/M | Suprasternal area | 3.5 | |
| Michal et al. [15] | 43/M | R suprasternal area | 3.0 | |
| Henderson et al. [16] | 39/M | R sternoclavicular area | 1.4 | |
| Zhao et al. [17] | 71/M | L supraclavicular area | 9.0 | |
| 52/M | R supraclavicular area | 3.5 | ||
| Marschall et al. [18] | 22/M | Supraclavicular area | 5.0 | |
| Fukunaga [19] | 52/M | L supraclavicular area | 1.5 | |
| Lee et al. [20] | 59/M | L supraclavicular area | 3.5 | |
| Kazakov et al. [21] | 71/F | Interface of the posterior axillary region and back | 3.5 | |
| Fetsch et al. [22] | 28/M | L neck | 2.0 | |
| 29/M | Suprasternal area | 3.5 | ||
| 30/M | Suprasternal area | 7.0 | ||
| 35/M | Chest wall, near sternal notch | 7.0 | ||
| 36/M | L infraclavicular area | 4.0 | ||
| 36/M | Supraclavicular fossa | 5.0 | ||
| 40/M | L supraclavicular area | 6.2 | ||
| 40/M | Medial clavicular area | 6.5 | ||
| 47/M | R supraclavicular area | 4.0 | ||
| 47/M | L sternoclavicular joint area | 2.5 | ||
| 48/M | L sternoclavicular joint area | 2.5 | ||
| 48/M | L sternoclavicular joint area | 2.5 | ||
| 63/M | L clavicular region area | 2.5 | ||
| 64/F | Suprasternal to manubrium | 3.0 | ||
| 65/M | R sternoclavicular joint area | 2.5 | ||
| 78/M | L clavicular area | 2.0 | ||
| Kushida et al. [23] | 19/M | L supraclavicular area | 5.0 | |
| Iida et al. [24] | 89/F | L supraclavicular area | 6.0 | |
| Seok et al. [25] | 47/M | Suprasternal area | 7.0 | |
| Weinreb et al. [26] | 77/M | L supraclavicular area | 4.5 | |
| Choi et al. [27] | 44/M | L sternoclavicular area | 7.5 | |
| Zhou et al. [28] | 53/M | L sternoclavicular area | 7.0 | |
| Sakurai et al. [29] | 26/M | L supraclavicular area | 2.0 | |
| Shim et al. [30] | 34/M | L supraclavicular area | 6.0 | |
| Liang et al. [31] | 29/F | Beneath L SCM | 4.0 | |
| 31/M | Beneath L SCM | 8.0 | ||
| 47/M | Anterior chest | 4.5 | ||
| 53/F | R supraclavicular area | 8.5 | ||
| Cheng et al. [32] | 31/M | R supraclavicular area | 8.0 | |
| Huang et al. [33] | 40/M | L clavicular area | 4.0 | |
| Jing et al. [34] | 28/M | L supraclavicular area | 3.0 | |
| Reusens et al. [35] | 45/F | Presternal area | 3.5 | |
| Parihar et al. [36] | 44/F | Lower neck | na | |
| Weissferdt et al. [37] | 47/M | L lower neck, sternoclavicular joint | 5.0 | |
| 52/M | L lower neck, sternoclavicular joint | 4.5 | ||
| 43/F | R lower neck, sternoclavicular joint | 8.0 | ||
| 38/M | R lower neck, sternoclavicular joint | 5.0 | ||
| 42/F | L lower neck, sternoclavicular joint | 4.5 | ||
| 34/M | R lower neck, sternoclavicular joint | 6.5 | ||
| 47/F | L lower neck, sternoclavicular joint | 5.5 | ||
| 38/F | R lower neck, sternoclavicular joint | 3.5 | ||
| 49/M | R lower neck, sternoclavicular joint | 6.0 | ||
| Kondo et al. [38] | 60/F | L lower neck | 6.0 | |
| 24/F | L lower neck | 4.8 | ||
| Present cases | 31/M | R supraclavicular area | 9.0 | |
| 70/F | Suprasternal area | 3.5 | Adenocarcinoma, intraductal type |
F female, M male, L left, R right, SCM sternocleidomastoid muscle, na not available
Thus far, a total of 79 cases of EHT have been reported in the English literature, including the current two cases (Table 1). In aggregate, EHT shows a predilection for middle-aged adults (age range: 19–89 years; mean: 46 years) (n = 78). The male to female ratio is 3.4:1 (61:18), highlighting a significant male predominance. While no conclusion can be made, the presence of strong androgen receptor reactivity in the spindled tumor cells [26] may suggest a hormone sensitive growth, a finding similar to nasopharyngeal angiofibroma and salivary duct carcinoma, where there are ligand-independent AR splice variants, mutations, and extra AR gene copies, although usually no AR gene amplification [39, 40]. The most common locations of EHT include the supraclavicular, suprasternal, and sternoclavicular areas. Other sites rarely reported include the chest wall and posterior axilla [4, 13, 21, 31]. It is well known that the branchial plexus development can result in many normal anatomic variations as well as significant anomalies. Many of the nerves (C5-T1 trunks) may innervate muscles and tissues of the region in an aberrant fashion. Since the cranial nerves and laryngeal nerves are associated with pouch derivatives, it does not seem far-fetched that an isolated tumor may develop in an unusual location like the posterior axilla. Clinically, the vast majority of supraclavicular masses represent metastatic tumors or lymphoma, with the majority of tumors primary carcinomas below the clavicles, with genitourinary primaries affecting the left side disproportionately [41]. If we classify “suprasternal” and “presternal” as “midline”, the ratio of left-sided : midline : right-sided is 35 (51%):17 (25%):16 (24%) (n = 68). Therefore, the left side is more commonly affected. Interestingly, there are known laterality differences in the neck, with cell mediated immune hypersensitivity reported to be stronger in the left side of humans and different cancer rate asymmetries, especially for head and neck Merkel cell carcinomas [42–44]. Further, the left supraclavicular space contains the thoracic duct and jugular lymphatic trunk, a distinctly different anatomy to the left side of the low neck than the right side. Thus, during embryologic development, these complex differences in anatomy may play a role in the development of the tissues which give rise to this tumor. The tumor size ranged from 1.4 to 19.0 cm (mean: 4.9 cm) (n = 77). The molecular evaluation of EHT is limited to a few reports, but one such study showed the absence of PLAG1 rearrangements in EHT, distinctly different from lipomatous pleomorphic adenoma [31].
The exact origin of EHT remains controversial. The current tumor appellation was introduced by Rosai et al. [3] in 1984 with the designation “ectopic hamartomatous thymoma,” reflecting a belief that these tumors were derived from the third branchial arch and were composed of abnormal thymic tissue. However, the name EHT is a misnomer and potentially misleading. The lesion is not a hamartoma, but is instead a neoplasm; it is not ectopic, as the components are normal for the location embryologically (eutopic); and it is not a form of thymoma. The almost exclusive occurrence of the tumors in the lower neck has prompted the belief that they are a result of a developmental abnormality of the third or fourth branchial pouches, the cervical sinus of His, and the ultimobranchial body [2–4, 7, 8]. Given that the precise histogenetic origin of EHT remains uncertain, the best terminology to describe these tumors is still debated. Fetsch et al. [22] proposed the nomenclature of “branchial anlage mixed tumor” because of its epithelial and myoepithelial features, but it has thus far not gained widespread adoption. Mixed tumor means too many things already, and so this name is confusing. Recently, Weissferdt et al. [37] proposed the designation “thymic anlage tumor” not only to more accurately classify these lesions, but, also to highlight their difference from true thymomas or mixed tumors. They insisted that the histologic and immunohistochemical features were reminiscent of thymic derivation and suggested possible origin from remnant of the thymic anlage. However, in their immunohistochemical study, none of the cases showed expression of PAX8, which is positive in thymic epithelial cells and neoplasm [37]. In addition to the absence of normal thymic tissue in these tumors, the presence of myoepithelial differentiation is abnormal for thymic tumors, and the absence of EHT in the mediastinum or thymus, makes it very difficult to continue to include “thymic” in the name of this entity.
The general consensus remains that it originates from a branchiogenic origin. Embryologically, there are three germ layers (triploblast), with the endoderm and ectoderm giving rise to the mesoderm. The ectoderm forms neural crest, the latter involved in brain and facial development. Primarily involved in nerve tissue development (neurulation), tissues from this layer include brain, spinal cord, peripheral nerves, epidermis, mammary glands and subcutaneous glands. The endoderm is a much simpler layer, giving rise to epithelial linings, including the thyroid, parathyroid, thymus, foregut, midgut and hindgut. The mesoderm results in the formation of skeletal muscle, bone, and connective tissue (fat), among other organs, via somites, which represent mesoderm on either side of the neural tube in embryos that will determine the migratory pathways of neural crest tissues. Further, mesenchyme is a concept related to the mesoderm, describing the loose cells found in association with proteins and fluids, an extracellular matrix type material. Of course, human somatic cells can create pluripotent stem cells, that may give rise to a multitude of different tissues [45]. The branchial apparatus is formed by a complex interaction of the branchial pouches, clefts and arches. These structures play a significant role in ear, neck and facial development, with each portion of the apparatus contributing to the ultimate development of specific organs or tissues. In this context, the tumor currently called EHT is a neoplasm involving tissues derived from the branchial apparatus, but not fully expressing the tissues of the final organ. As it is tissues from the mesoderm and endoderm that are involved in this branchial apparatus tumor, the term biphenotypic branchioma more closely encompasses the origins and tissue types seen in this tumor (which include epithelium, spindled cells and fat, but only two primordial layers). The term mixed tumor is inculcated in the literature of the head and neck region for a salivary gland tumor type that shows epithelial, myoepithelial and chondromyxoid features, findings that are not seen in this tumor. Similarly, branchial anlage mixed tumor suggests the branchial mechanism of origin, but the “mixed tumor” does not convey the tissue types involved as accurately or concisely. Thymic anlage tumor can also be exclude due to the lack of true thymic tissue origin. Taxonomy is always fraught with significant controversy and debate, but in an effort to yield a more biologically and histologically accurate term, biphenotypic branchioma is suggested to replace ectopic hamartomatous thymoma, branchial anlage mixed tumor and thymic anlage tumor. Biphenotypic is based on the presence of mesoderm and endodermal germ layer derivatives even though represent by three components histologically (epithelium, spindled cells and fat). “Branchi” implies branchial apparatus origin while “oma” supports the concept of a neoplasm. When carcinoma develops, the type of carcinoma can be added to the term, such as “intraductal carcinoma arising within biphenotypic branchioma”. To avoid confusion, international consensus of terminology is still desired, with active dialogue around this proposed diagnostic term.
Funding
No external funding was obtained for this study.
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflict of interest as it relates to this research project.
Ethical Approval
All procedures performed in this retrospective data analysis involving human participants were in accordance with the ethical standards of the institutional review board, which did not require informed consent.
References
- 1.Chan JKC. Ectopic hamartomatous thymoma. In: Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F, editors. WHO classification of tumours of soft tissue and bone. Lyon: IARC Press; 2013. pp. 201–202. [Google Scholar]
- 2.Smith PS, McClure J. Unusual subcutaneous mixed tumour exhibiting adipose, fibroblastic, and epithelial components. J Clin Pathol. 1982;35:1074–1077. doi: 10.1136/jcp.35.10.1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosai J, Limas C, Husband EM. Ectopic hamartomatous thymoma: a distinctive benign lesion of lower neck. Am J Surg Pathol. 1984;8:501–513. doi: 10.1097/00000478-198407000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Fetsch JF, Weiss SW. Ectopic hamartomatous thymoma: clinicopathologic, immunohistochemical, and histogenetic considerations in four new cases. Hum Pathol. 1990;21:662–668. doi: 10.1016/S0046-8177(96)90014-3. [DOI] [PubMed] [Google Scholar]
- 5.Saeed IT, Fletcher CD. Ectopic hamartomatous thymoma containing myoid cells. Histopathology. 1990;17:572–574. doi: 10.1111/j.1365-2559.1990.tb00800.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim JM, Won NH, Paik SY. Ectopic hamartomatous thymoma: a case report. Korean J Pathol. 1990;24:50–57. [Google Scholar]
- 7.Chan JK, Rosai J. Tumors of the neck showing thymic or related branchial pouch differentiation: a unifying concept. Hum Pathol. 1991;22:349–367. doi: 10.1016/0046-8177(91)90083-2. [DOI] [PubMed] [Google Scholar]
- 8.Armour A, Williamson JM. Ectopic cervical hamartomatous thymoma showing extensive myoid differentiation. J Laryngol Otol. 1993;107:155–158. doi: 10.1017/S0022215100122509. [DOI] [PubMed] [Google Scholar]
- 9.Doctor VM, Simha MR. Ectopic hamartomatous thymoma-a case report and review of the literature. Indian J Cancer. 1993;30:192–195. [PubMed] [Google Scholar]
- 10.Michal M, Neubauer L. Carcinoma arising in ectopic hamartomatous thymoma. A previously unpublished occurrence. Report of two cases. Zentralbl Pathol. 1993;139:381–386. [PubMed] [Google Scholar]
- 11.Michal M, Neubauer L, Fakan F. Carcinoma arising in ectopic hamartomatous thymoma. An ultrastructural study. Pathol Res Pract. 1996;192:610–618. doi: 10.1016/S0344-0338(96)80113-0. [DOI] [PubMed] [Google Scholar]
- 12.Michal M, Zámecník M, Gogora M, Mukensnabl P, Neubauer L. Pitfalls in the diagnosis of ectopic hamartomatous thymoma. Histopathology. 1996;29:549–55. doi: 10.1046/j.1365-2559.1996.d01-533.x. [DOI] [PubMed] [Google Scholar]
- 13.Eulderink F, de Graaf PW. Ectopic hamartomatous thymoma located presternally. Eur J Surg. 1998;164:629–630. doi: 10.1080/110241598750005769. [DOI] [PubMed] [Google Scholar]
- 14.Hirokawa M, Tadaoka Y, Shimizu M, Monobe Y, Kanahara T, Manabe T. Ectopic hamartomatous thymoma. Report of a case with fine needle aspiration biopsy findings. Acta Cytol. 1999;43:232–234. doi: 10.1159/000330983. [DOI] [PubMed] [Google Scholar]
- 15.Michal M, Mukensnabl R. Clear cell epithelial cords in an ectopic hamartomatous thymoma. Histopathology. 1999;35:89–90. doi: 10.1046/j.1365-2559.1999.0728e.x. [DOI] [PubMed] [Google Scholar]
- 16.Henderson CJ, Gupta L. Ectopic hamartomatous thymoma: a case study and review of the literature. Pathology. 2000;32:142–146. doi: 10.1080/003130200104420. [DOI] [PubMed] [Google Scholar]
- 17.Zhao C, Yamada T, Kuramochi S, Yamazaki K, Mukai M, Kameyama K, Hata J. Two cases of ectopic hamartomatous thymoma. Virchows Arch. 2000;437:643–647. doi: 10.1007/s004280000309. [DOI] [PubMed] [Google Scholar]
- 18.Marschall J, Kanthan R. The sarcomatous guise of cervical ectopic hamartomatous thymoma. Head Neck. 2002;24:800–804. doi: 10.1002/hed.10091. [DOI] [PubMed] [Google Scholar]
- 19.Fukunaga M. Ectopic hamartomatous thymoma: a case report with immunohistochemical and ultrastructural studies. APMIS. 2002;110:565–570. doi: 10.1034/j.1600-0463.2002.11007808.x. [DOI] [PubMed] [Google Scholar]
- 20.Lee SN, Cho MS, Koo H, Han WS. Ectopic hamartomatous thymoma: a case report showing CD99 + lymphocytes and a low proliferation index. Arch Pathol Lab Med. 2003;127:e37881. doi: 10.5858/2003-127-e378-EHTACR. [DOI] [PubMed] [Google Scholar]
- 21.Kazakov DV, Mukensnabl P, Hes O, Michal M. ‘Ectopic’ ectopic hamartomatous thymoma. Histopathology. 2004;45:202–204. doi: 10.1111/j.1365-2559.2004.01866.x. [DOI] [PubMed] [Google Scholar]
- 22.Fetsch JF, Laskin WB, Michal M, Remotti F, Heffner D, Ellis G, Furlong M, Miettinen M. Ectopic hamartomatous thymoma: a clinicopathologic and immunohistochemical analysis of 21 cases with data supporting reclassification as a branchial anlage mixed tumor. Am J Surg Pathol. 2004;28:1360–1370. doi: 10.1097/01.pas.0000135518.27224.3f. [DOI] [PubMed] [Google Scholar]
- 23.Kushida Y, Haba R, Kobayashi S, Ishikawa M, Doi T, Kadota K. Ectopic hamartomatous thymoma: a case report with immunohistochemical study and review of the literature. J Cutan Pathol. 2006;33:369–372. doi: 10.1111/j.0303-6987.2006.00424.x. [DOI] [PubMed] [Google Scholar]
- 24.Iida E, Okazaki M, Sarukawa S, Motoi T, Kikuchi Y. Ectopic hamartomatous thymoma in the sternocleidomastoid muscle masquerading as sarcoma. Scand J Plast Reconstr Surg Hand Surg. 2006;40:249–252. doi: 10.1080/0284431051003592. [DOI] [PubMed] [Google Scholar]
- 25.Seok SH, Lee DH, Kang SH, Bae YK. Ectopic hamartomatous thymoma: a case report along with a review of the literature concerning the histogenesis and new nomenclature. Korean J Pathol. 2006;40:292–296. [Google Scholar]
- 26.Weinreb I, O’Malley F, Ghazarian D. Ectopic hamartomatous thymoma: a case demonstrating skin adnexal differentiation with positivity for epithelial membrane antigen, androgen receptors, and BRST-2 by immunohistochemistry. Hum Pathol. 2007;38:1092–1095. doi: 10.1016/j.humpath.2007.01.029. [DOI] [PubMed] [Google Scholar]
- 27.Choi JH, Shim YR, Song SY. Fine needle aspiration cytology of ectopic hamartomatous hamartomatous thymoma. Acta Cytol. 2007;51:672–675. [PubMed] [Google Scholar]
- 28.Zhou J, Zhang HZ, Jiang ZM, Shi L. A case of ectopic hamartomatous thymoma. Arch Histopathol Differ Diagn. 2008;15:13–17. [Google Scholar]
- 29.Sakurai H, Kaji M, Mukai K, Suemasu K. Ectopic hamartomatous thymoma—a truly rare neoplasm: report of a case. Surg Today. 2010;40:146–149. doi: 10.1007/s00595-009-4019-4. [DOI] [PubMed] [Google Scholar]
- 30.Shim DB, Song JS, Baek SJ. An ectopic hamartomatous thymoma. Auris Nasus Larynx. 2012;39:110–113. doi: 10.1016/j.anl.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 31.Liang PI, Li CF, Sato Y, Lee VK, Bahrami A, Chuang SS. Ectopic hamartomatous thymoma is distinct from lipomatous pleomorphic adenoma in lacking PLAG1 aberration. Histopathology. 2013;62:518–522. doi: 10.1111/his.12022. [DOI] [PubMed] [Google Scholar]
- 32.Cheng YS, Zhou ZR, Wang J. Ectopic hamartomatous thymoma: radiographic and clinicopathological features. Chin Med J (Engl) 2013;126:798–799. [PubMed] [Google Scholar]
- 33.Huang L, Zhao L, Chai Y. An ectopic hamartomatous thymoma compressing left jugular vein. Niger J Clin Pract. 2014;17:814–816. doi: 10.4103/1119-3077.144407. [DOI] [PubMed] [Google Scholar]
- 34.Jing H, Wang J, Wei H, Liu M, Chen F, Meng Q, Tai Y. Ectopic hamartomatous thymoma: report of a case and review of literature. Int J Clin Exp Pathol. 2015;8:11776–11784. [PMC free article] [PubMed] [Google Scholar]
- 35.Reusens H, Van den Broecke C, Creytens D, Fierens K. A rare presternal soft tissue tumor: ectopic hamartomatous thymoma (branchial anlage mixed tumor) Acta Chir Belg. 2015;115:418–422. doi: 10.1080/00015458.2015.11681144. [DOI] [PubMed] [Google Scholar]
- 36.Parihar S, Gohil R, Oparka R, Kennedy C. Benign anlage tumour: a very unusual neck mass. BMJ Case Rep. 2016 doi: 10.1136/bcr-2016-215789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weissferdt A, Kalhor N, Petersson F, Moran CA. Ectopic hamartomatous thymoma-new insights into a challenging entity: a clinicopathologic and immunohistochemical study of 9 cases. Am J Surg Pathol. 2016;40:1571–1576. doi: 10.1097/PAS.0000000000000699. [DOI] [PubMed] [Google Scholar]
- 38.Kondo T, Sato Y, Tanaka H, Sasaki T, Kawabata K, Mitani H, Yonekawa H, Fukushima H, Shimbashi W. Two cases of ectopic hamartomatous thymoma masquerading as sarcoma. Case Rep Otolaryngol. 2017 doi: 10.1155/2017/1672919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Williams L, Thompson LD, Seethala RR, Weinreb I, Assaad AM, Tuluc M, Ud Din N, Purgina B, Lai C, Griffith CC, Chiosea SI. Salivary duct carcinoma: the predominance of apocrine morphology, prevalence of histologic variants, and androgen receptor expression. Am J Surg Pathol. 2015;39:705–713. doi: 10.1097/PAS.0000000000000413. [DOI] [PubMed] [Google Scholar]
- 40.Hwang HCA, Mills SE, Patterson K, Gown AM. Expression of androgen receptors in nasopharyngeal angiofibroma: an immunohistochemical study of 24 cases. Mod Pathol. 1998;11:1122–1126. [PubMed] [Google Scholar]
- 41.Franzen A, Günzel T, Buchali A, Coordes A. Etiologic and differential diagnostic significance of tumor location in the supraclavicular fossa. Laryngoscope. 2017 doi: 10.1002/lary.26775. [DOI] [PubMed] [Google Scholar]
- 42.Yoruk O, Yuksel R, Yuksel Y, Dane S. Left-right asymmetry in neck lymph nodes distribution in patients with bilateral laryngeal cancer. Surg Radiol Anat. 2014;36:239–242. doi: 10.1007/s00276-013-1176-3. [DOI] [PubMed] [Google Scholar]
- 43.Roychoudhuri R, Putcha V, Møller H. Cancer and laterality: a study of the five major paired organs (UK) Cancer Causes Control. 2006;17:655–662. doi: 10.1007/s10552-005-0615-9. [DOI] [PubMed] [Google Scholar]
- 44.Koljonen V, Kluger N, Sihto H, Böhling T. Lateral distribution of Merkel cell carcinoma in a nationwide cohort. J Eur Acad Dermatol Venereol. 2013;27:884–888. doi: 10.1111/j.1468-3083.2012.04600.x. [DOI] [PubMed] [Google Scholar]
- 45.Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, Jonsdottir GA, Ruotti V, Stewart R, Slukvin II, Thomson JA. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318(5858):1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]