Abstract
Background:
The number of ulnar collateral ligament (UCL) reconstructions in adolescent athletes has increased over the past 2 decades. Clinical results in this population have not been well studied.
Purpose/Hypothesis:
The purpose of this study was to evaluate the outcomes and return to sport after UCL reconstruction in a large group of adolescent baseball players. We hypothesized that excellent clinical outcomes and high rates of return to sport would be observed in this population at a minimum 2-year follow-up.
Study Design:
Case series; Level of evidence, 4.
Methods:
We reviewed 140 adolescent (aged ≤19 years) baseball players who underwent UCL reconstruction with the American Sports Medicine Institute (ASMI) technique by a single surgeon. Medical records were reviewed for patient demographics, injury characteristics, operative details, and surgical complications. Patient-reported outcomes were assessed using the Conway scale, the Andrews-Timmerman (A-T) score, the Kerlan-Jobe Orthopaedic Clinic (KJOC) score, and a 0- to 100-point subjective scale for elbow function and satisfaction. Return to sporting activity was assessed using a custom-designed questionnaire.
Results:
The mean age at the time of surgery was 18.0 years (range, 13-19 years), and the mean follow-up was 57.9 months (range, 32.4-115.4 months). Over half (60%) of patients were high school athletes. The mean duration of symptoms before surgery was 6.9 months (range, 0.5-60.0 months). Partial tears were identified in 57.9% of patients, and 41.3% of patients had preoperative ulnar nerve symptoms. Graft type included the ipsilateral palmaris in 77.1% of patients. Concomitant procedures were performed in 25% of patients. Outcomes on the Conway scale were “excellent” in 86.4% of patients. The mean A-T and KJOC scores were 97.3 ± 6.1 and 85.2 ± 14.6, respectively. Mean patient satisfaction was 94.4. Overall, 97.8% of patients reported returning to sport at a mean of 11.6 months (range, 5-24 months), and 89.9% of patients returned to sport at the same level of competition or higher. A total of 11.6% of patients went on to play professional baseball.
Conclusion:
UCL reconstruction with the ASMI technique is an effective surgical option in adolescents, with excellent outcome scores. At a minimum of 2-year follow-up, nearly 90% of patients returned to their preinjury level of sport.
Keywords: ulnar collateral ligament, UCL reconstruction, adolescent, elbow
Athletic participation is common among adolescents, with more than half of all high school students participating in school-sanctioned sports during the 2014-2015 academic year.1 Of the 7.8 million student-athletes in the United States, baseball is the fourth most popular boys’ program, with nearly 500,000 participants.1 Sport participation is beneficial to overall health but unfortunately carries an inherent risk of injury. Among the most common are overuse injuries to the throwing arms of pitchers, thought to be a result of cumulative microtraumatic stresses from the repetitive overhand-throwing motion used to pitch a baseball.7,20,31 In addition, approximately one-fourth of high school baseball players pitch,18 and the number of high school pitchers who require surgery for pitching-related injuries has significantly increased.24
Ulnar collateral ligament (UCL) reconstruction among baseball pitchers has increased dramatically over the past 20 years. A recent analysis in the state of New York found a 343% increase in the number of UCL reconstructions performed annually from the years 2003 to 2014.21 Previously, a single institution reported a 22-fold increase in the number of UCL reconstruction procedures from the years 1994 to 2010.14 Both studies also revealed that the adolescent population was the fastest growing subgroup of athletes undergoing UCL reconstruction. According to the study by Mahure et al,21 the annual incidence of UCL reconstructions among 15- to 19-year-old athletes is projected to increase from 6.3 per 100,000 to 14.6 per 100,000 by 2025. Another study analyzing the demographic distribution of UCL reconstructions from the years 2007 to 2011 found that adolescents (aged 15-19 years) accounted for 56.8% of all UCL reconstructions, with an annual growth rate of 9.84%.13
The many risk factors contributing to elbow injuries in this population add complexity to our understanding of the epidemiology of UCL injuries. Among the many proposed risk factors include increased weight, lifting weights during the season, absence of glenohumeral internal rotation, preseason supraspinatus weakness, overuse, fatigue, high pitch velocity, throwing of breaking pitches (curveballs and sliders), participation in showcases (events for student-athletes to show off their baseball skills in front of college coaches), and geographic location (ie, pitchers in warm weather climates).19,20,24,29,33 Risk factors also include pitching more games, months, and pitches per year; more innings and pitches per game; more warm-up pitches before a game; and players who were more frequently started as pitchers.24 Despite efforts to stem the epidemic of adolescent elbow injuries through risk factor education and enforcement of pitch counts, the number of adolescent athletes undergoing UCL reconstruction continues to increase.
The surgical technique used by the senior author (J.R.A.) has been referred to as the American Sports Medicine Institute (ASMI) technique3 and is a modification of the original technique described by Jobe et al.16 In the largest case series to date by Cain et al5 on UCL reconstructions involving this technique from 1988 to 2006, 82.4% of 131 high school athletes returned to the same or higher level of competition; 50% went on to play in college, and 6% advanced to professional play in the minor leagues. Despite the number of studies in the young adult population using the ASMI and other techniques, there are limited published reports focusing specifically on the outcomes of UCL reconstruction in adolescents.17,26
The purpose of this study was to evaluate the clinical results of UCL reconstruction utilizing the ASMI technique in a large group of adolescent baseball players. We sought to identify any patient or surgical factors affecting patient-reported functional outcomes. Secondarily, we sought to characterize the success of return to sport. On the basis of prior studies, we hypothesized that excellent clinical outcomes and high rates of return to sport would be observed in this young population at a minimum 2-year follow-up.
Methods
Patient Selection
Ethics approval was obtained from our local institutional review board before the initiation of this study. We retrospectively reviewed a consecutive series of adolescent patients who underwent UCL reconstruction according to the technique described by Andrews and colleagues.3 All surgical procedures were performed by the senior author, a fellowship-trained sports medicine surgeon, between January 2007 and March 2014. A total of 301 patients were identified through a Current Procedural Terminology (CPT) code search of an institutional computerized database using the code 24346 (reconstruction medial collateral ligament, elbow, with tendon graft). The search was limited to patients aged 10 to 19 years, consistent with the World Health Organization’s definition of adolescence.32
Patients were included in the study if they had a UCL tear confirmed with magnetic resonance imaging (MRI) and underwent primary UCL reconstruction. Those with associated lesions were also included, and there were no limits regarding concomitant procedures. Exclusion criteria for this study were participation in a sport other than baseball and those unable to be contacted or not wishing to be involved in a research study.
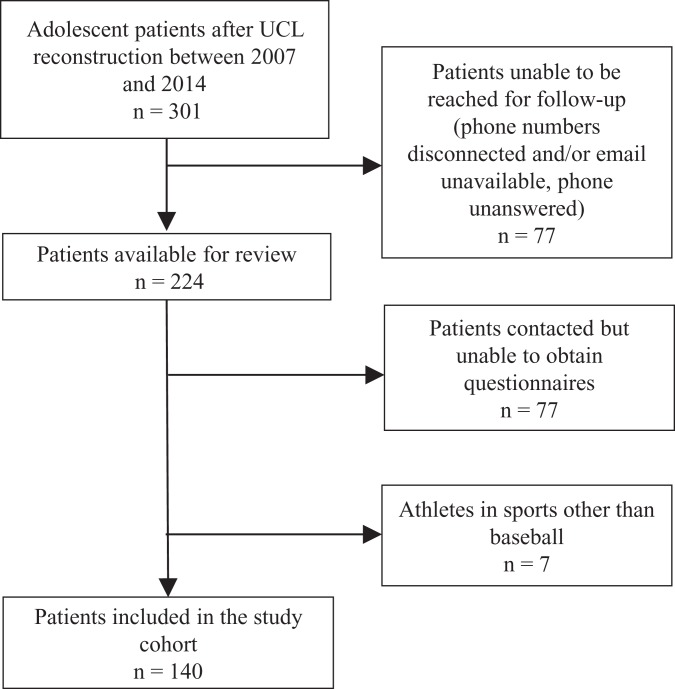
Patient-reported outcome data were obtained by contacting all patients via telephone ≥2 years after surgery. Research assistants, all of whom had not been involved in the original surgery or care of the patients, performed the telephone questionnaires. A total of 161 patients failed to meet the appropriate criteria and were excluded from the cohort. Ultimately, 140 patients were contacted for a follow-up evaluation. A detailed flow diagram is included in Figure 1.
Figure 1.
Flow diagram outlining patient selection. UCL, ulnar collateral ligament.
Surgery and Postoperative Management
Reconstruction of the UCL was performed using the ASMI technique,3 a modification of the Jobe procedure,16 with a free autologous graft and subcutaneous ulnar nerve transposition in all cases. Postoperative rehabilitation was initiated the day after surgery and consisted of 5 separate phases. Postoperatively, the patient’s elbow was immobilized in a posterior splint at 90° of flexion to allow initial healing. Approximately 5 to 7 days postoperatively, the splint was removed, and a hinged elbow brace was applied. Active range of motion exercises were begun to achieve full extension by 2 weeks. Shoulder isometrics were begun during the first week, but external rotation was not performed until the third week. Shoulder conditioning exercises began at the third week. Elbow flexion and extension strengthening began during the fourth week with the elbow at the side. The brace was discontinued at the fifth week. Shoulder and elbow strengthening was progressed at the 6-week point with the initiation of the Thrower’s Ten Program.30 This was continuously progressed throughout the rehabilitation process. Plyometric and sport-specific training followed strengthening during weeks 10 to 16. An interval hitting program was started at around 12 weeks. A 2-week rainbow throwing program typically began around week 16 after successful completion of the previous phases. If symptom-free, the athlete began a formal interval throwing program. For pitchers, a 6- to 8-week progressive, long-toss flat-ground program preceded an interval mound program. The timing and goals of each phase are presented in Table 1.
TABLE 1.
Rehabilitation Protocola
| Phase | Timing | Goals |
|---|---|---|
| 1 | Weeks 1-3 | Protect healing tissue, assess and address ROM/stability needs of whole body, retard muscle atrophy, diminish pain and inflammation |
| 2 | Weeks 4-7 | Gradually increase to full ROM, promote healing of repaired tissue, regain and improve muscular strength, restore full function of graft site |
| 3 | Weeks 8-24 | Improve muscular strength, power, and endurance; maintain full elbow ROM; gradually initiate prethrowing drills |
| 4 | Weeks 25-36+ | Increase strength, power, and endurance; restore mobility/stability throughout body; gradually progress to competitive throwing/sports |
| 5 | Months 9-12 | Gradually return to sport activities |
aROM, range of motion.
Clinical Evaluation
Operative and clinical notes were reviewed for all patients. Data regarding age at presentation, side, sex, sport/position(s), physical examination findings, details of surgical intervention, postoperative follow-up information, complications, and subsequent operative procedures on the involved elbow were recorded. UCL tears were classified as partial or complete based on MRI findings as documented in the medical records. Patient-reported outcome measures (PROMs) included the Conway scale,8 the subjective Andrews-Timmerman (A-T) score,4 and the Kerlan-Jobe Orthopaedic Clinic (KJOC) score.2 Patient satisfaction was assessed with a 0- to 100-point scale, where 0 was considered “completely dissatisfied” and 100 considered “completely satisfied.” Patients were asked if they would elect to undergo surgery again. Return to sport was directly assessed using a special questionnaire. Patients were asked to provide details regarding the sport practiced and its level (competitive or recreational) before symptom onset and at the latest follow-up as well as the time to return to sport when applicable. Patients were also asked to describe their limiting reasons if they returned at a decreased level or were unable to return at all.
Statistical Analysis
Means ± SDs and ranges were calculated for continuous variables (ie, age). Categorical variables (ie, side) were expressed as numbers and percentages. The normality of distribution of dependent variables (A-T and KJOC scores) was assessed using the Shapiro-Wilk normality test. The associations between dichotomous and continuous variables were analyzed using Spearman correlations. The correlations between categorical variables were examined using the chi-square or Fisher exact test as appropriate. Statistical significance was set at P ≤ .05. All data were tabulated in Excel (version 2012; Microsoft), and analyses were conducted using STATA 14.2 (StataCorp).
Results
Patient Characteristics
Patient characteristics are summarized in Table 2. Sixty percent of patients were high school athletes, and 94.3% of patients were pitchers. The mean age of all patients at the time of surgery was 18.0 years (range, 13-19 years), and the mean follow-up was 57.9 months (range, 32.4-115.4 months). The mean duration of symptoms before surgery was 6.9 months (range, 0.5-60.0 months). Partial tears were identified in 57.9% of patients. Preoperatively, 41.3% of patients had subjective neurological symptoms (intermittent paresthesia in the ulnar nerve distribution) at the time of presentation or physical examination findings consistent with ulnar nerve sensitivity (tenderness to palpation of the ulnar nerve and/or positive Tinel test result).
TABLE 2.
Patient Characteristicsa
| Characteristic | Value |
|---|---|
| Age at surgery, mean ± SD, y | 18.0 ± 1.3 |
| Right hand dominance/side | 119 (85.0) |
| Duration of symptoms, mean ± SD, mo | 6.9 ± 9.0 |
| Follow-up, mean ± SD, mo | 57.9 ± 16.3 |
| Level of sport before surgery | |
| High school | 84 (60.0) |
| College | 52 (37.1) |
| Professional | 3 (2.1) |
| Middle school | 1 (0.7) |
| Primary position | |
| Pitcher | 132 (94.3) |
| Infielder | 4 (2.9) |
| Catcher | 2 (1.4) |
| Not applicable | 2 (1.4) |
| Tear characteristics on magnetic resonance imaging | |
| Partial | 81 (57.9) |
| Complete | 52 (37.1) |
| Other | 7 (5.0) |
aData are reported as n (%) unless otherwise indicated.
Surgical Findings
Surgical findings are reported in Table 3. A palmaris longus tendon autograft harvested from the ipsilateral forearm was used in 77.1% of patients. Gracilis tendons from the contralateral extremity were used in 21.4% of patients with insufficient or absent palmaris longus tendons. Concomitant procedures were performed in 25% of patients. The most common procedure was excision of a posteromedial olecranon osteophyte in 12.9% of patients.
TABLE 3.
Surgical Findings
| Characteristic | n (%) |
|---|---|
| Graft type | |
| Ipsilateral palmaris | 108 (77.1) |
| Contralateral gracilis | 30 (21.4) |
| Othera | 2 (1.4) |
| Associated lesions | |
| Olecranon tip osteophytes | 22 (15.7) |
| Ulnar collateral ligament calcifications/ossicles | 21 (15.0) |
| Fractures/nonunion | 4 (2.9) |
| Loose bodies | 2 (1.4) |
| Other | 2 (1.4) |
| Other procedures | |
| Osteophyte excision | 18 (12.9) |
| Excision of calcifications/ossicles | 13 (9.3) |
| Loose body removal | 2 (1.4) |
| Other | 9 (6.4) |
aIncluded contralateral semitendinosus and ipsilateral gracilis.
Clinical Outcomes
Outcomes on the Conway scale were “excellent” in 86.4% of patients. The mean A-T and KJOC scores were 97.3 ± 6.1 and 85.2 ± 14.6, respectively (Table 4). Mean patient satisfaction was 94.4. There was a statistically significant positive correlation between the use of a palmaris autograft and the A-T score (P = .05), but the correlation was not statistically significant with other PROMs (Conway, P = .77; KJOC, P = .20; satisfaction, P = .18). Independent variables shown to have no significant relationship to PROMs included age, level of sport at the time of surgery, and associated lesions.
TABLE 4.
Clinical Outcomesa
| Outcome Measure | Value |
|---|---|
| Conway | |
| Excellent | 121 (86.4) |
| Good | 5 (3.6) |
| Fair | 8 (5.7) |
| Poor | 6 (4.3) |
| Andrews-Timmerman, mean ± SD | 97.3 ± 6.1 |
| Kerlan-Jobe Orthopaedic Clinic, mean ± SD | 85.2 ± 14.6 |
| Global satisfaction (0- to 100-point subjective scale) | 94.4 |
| Would elect to undergo surgery again | 131 (93.6) |
| Graft reinjury | 5 (3.6) |
aData are reported as n (%) unless otherwise indicated.
Return to Sport
A total of 138 patients attempted to return to sport postoperatively (Table 5). Of those, 97.8% reported returning to sport at a mean of 11.6 months (range, 5-24 months); 89.9% of patients were able to return to sport at the same level of competition or higher for at least 1 season, and 11.6% of patients went on to play professional baseball. The most common reason for failure to return to sport or returning at a deceased level was elbow pain/discomfort (9 patients).
TABLE 5.
Return to Sport
| Outcome Measure | n (%) |
|---|---|
| Did not attempt return | 2 (1.4) |
| Attempted return | 138 (98.6) |
| Able to return | 135 (97.8) |
| Higher level | 86 (63.7) |
| Same level | 38 (28.1) |
| Decreased level | 11 (8.1) |
| Unable to return | 3 (2.2) |
| Reason for no/decreased return to sport | |
| Elbow pain/discomfort | 9 (6.4) |
| Fear of reinjury | 2 (1.4) |
| Reinjury | 2 (1.4) |
| Personal | 2 (1.4) |
| Other medical conditions | 1 (0.7) |
Complications
There was 1 case of an intraoperative nerve injury. Subsequent surgical procedures within 12 months of the index procedure were performed in 4 patients. Two of these patients sustained fractures of the medial epicondyle, requiring open reduction and internal fixation at 7 and 12 months, respectively. One patient developed heterotopic ossification and arthrofibrosis 5 months postoperatively, requiring elbow arthroscopic surgery, lysis of adhesions, extensive debridement, and manipulation under anesthesia. One patient underwent excision of a calcium deposit.
Discussion
This study represents the largest investigation of outcomes after UCL reconstruction in adolescent athletes. The principal findings of this study suggest that UCL reconstruction with the ASMI technique is an effective treatment option for UCL tears in this young, at-risk population, with a low rate of complications. Excellent patient-reported outcomes were seen at a minimum of 2-year follow-up. Overall, 89.9% of patients returned to the same or higher level of play, with 11.6% progressing to professional play. Athletes in our study achieved functional outcomes comparable with the results previously reported in the adolescent and young adult population. Statistical analysis of graft type, associated lesions, and level of play (high school vs college) found no significant correlation to patient-reported outcomes.
Considerable forces are placed on the young elbow throughout the throwing motion, and prolonged repetitive trauma can lead to adaptive changes about the elbow.15,22,28 Hurd et al15 examined the throwing elbows of 23 uninjured, asymptomatic high school pitchers using MRI. The authors noted that 61% had posteromedial subchondral sclerosis of the ulnotrochlear articulation, including 35% with a posteromedial olecranon osteophyte. Using dynamic ultrasound in the throwing elbows of 22 asymptomatic high school pitchers, Marshall et al22 identified posteromedial olecranon spurring in 36%. Furthermore, they found calcifications of the UCL present in 32% of athletes. In contrast, our review of 140 throwing elbows of adolescent baseball players requiring UCL reconstruction identified posteromedial olecranon osteophytes and UCL calcifications/ossifications in 15.7% and 15.0%, respectively. The reasons for the lower number of associated findings in our study are unclear but may be partly related to our larger sample size compared with Marshall et al.22 While it seems apparent that these bony and soft tissue changes occur in response to the repetitive stresses experienced by the young elbow during throwing, they may not be predictive of future ligamentous injuries.
There are limited published reports on patient-reported outcomes after UCL reconstruction in adolescents. Petty26 was among the first to address clinical outcomes after UCL reconstruction using the ASMI technique in this younger group of athletes. The author evaluated 27 high school baseball players with a mean age 17.4 years. At a final follow-up of 35 months, Petty reported “excellent” results on the Conway scale in 74% of patients. O’Brien et al23 reviewed the outcomes after UCL reconstruction with the docking and modified Jobe techniques in an overhead-throwing population; 19 of the 33 athletes were adolescents younger than 20 years. The authors reported a mean KJOC score of 76 at a mean follow-up of 3.7 years. In a recent large study of 55 high school athletes, Jones et al17 evaluated results after UCL reconstruction using the docking technique. The mean age in their cohort was 17.6 years (range, 15-18 years). At a mean of 31 months’ follow-up, they noted “excellent” outcomes using the Conway scale in 87%, a mean A-T score of 83.6, and a mean KJOC score of 88.0. Our study represents the largest investigation of UCL reconstruction solely among adolescent athletes to date, and our study design utilized similar functional metrics to maintain consistency across studies. The results of our investigation were comparable with the findings of previous authors, with “excellent” outcomes using the Conway scale in 86.4% of patients, a mean A-T score of 97.3, and a mean KJOC score of 85.2.
Of patients who attempted to return to sport (n = 138), the overall rate of successful return was 97.8% at a mean of 11.6 months. Moreover, 89.9% of patients who attempted to return were ultimately able to return to baseball at the same level. In a systematic review examining return to sport after UCL reconstruction, Erickson and colleagues12 reported a similar rate of return to sport for the ASMI technique at 93.3%. The authors also reported that the overall rate of return to sport including all techniques was slightly lower at 86.5%. The return-to-sport rate was highest among college players (95.5%), lower among higher school players (89.4%), and lowest among professional players (86.4%). Petty26 reported a return-to-sport rate of 74% after UCL reconstruction using the ASMI technique in 27 high school baseball players. The average time to return to sport was 11 months, and 37% were still playing competitively at the time of follow-up (average, 35 months). The author noted “loss of interest” and “lack of opportunity” as the primary reasons for players failing to return to play. This is in contrast to our findings of “elbow pain/discomfort” as the most common reason for failure of returning to sport or returning at a deceased level.
The largest study of athletes after UCL reconstruction was reported by Cain et al,5 who included 1281 cases from a single institution. All surgical procedures were performed with the ASMI technique, and the cohort included 131 high school athletes. The average rate of return to sport was 83% at the same or higher level of play at 11.6 months. Fifty percent went on to compete in college, and 6% advanced to professional play. A more recent large-scale study by Osbahr and colleagues25 evaluated 256 competitive baseball players at an average of 12.6 years postoperatively to determine the long-term career impact after undergoing UCL reconstruction with the ASMI technique. The average rate of return to sport was also 83%, and the average career duration after surgery was 3.6 years. Career duration was slightly shorter for the high school and college subgroups, at 2.9 and 2.5 years, respectively. Injuries that led to early retirement were more often related to the shoulder (22%) rather than the elbow (14%). Our results reflect the findings of previous studies, with 89.9% of athletes who attempted to do so returning to baseball at the same level of competition or higher and 11.6% of patients going on to play professional baseball.
UCL reconstruction remains the gold standard for treating attritional and complete UCL tears.6 However, less invasive alternatives for treating partial UCL tears have shown promising results and continue to be an active area of research. With approximately 58% of our adolescent patients having partial tears, effective nonreconstruction options such as platelet-rich plasma and UCL repair with internal brace augmentation could be ideal alternatives to UCL reconstruction for young patients.9–11,27 As future research continues to shift the paradigm of UCL injury treatment, the outcomes in our study will serve as a standard against which newer techniques can be judged.
Limitations
The results of our study should be interpreted based on the following limitations. This was a retrospective study with a short follow-up interval of only 2 years minimum, making long-term conclusions difficult to make. Outcome data were primarily obtained by a telephone interview, introducing possible recollection bias, and we did not obtain radiographic or physical examination follow-up data. Also, there was no comparison group with a different method of UCL reconstruction with which to contrast our technique. Further, these results reflect the outcomes of a single surgeon with a nationwide referral practice consisting of a large volume of young, high-level throwing athletes with financial resources, and as such, these results might not be generalizable to the broader orthopaedic community.
Another limitation was the difficulty of classifying patients who returned to sport as returning to the same or decreased level for those who entered college during their rehabilitation period. Most college sports are felt to be at a higher level than high school, but not qualifying for a Division I athletic team does not necessarily equate to not returning to the same level of competition. Patients were asked, qualitatively, if they felt that they returned to the same level of performance to help minimize the skewing of results. Finally, our follow-up was limited, with patient-reported outcome and return-to-sport data on 47% of patients. Many patients were not able to be located/contacted, despite multiple attempts via telephone and/or email. This may be caused, in part, by the nature of referrals to the senior author as well as patient mobility unique to this population as they enter into adulthood. Despite these limitations, this study represents the largest investigation of UCL reconstruction in this specific adolescent population.
Conclusion
UCL reconstruction with the ASMI technique is an effective surgical option in adolescents, with excellent outcome scores. At a minimum of 2-year follow-up, nearly 90% of patients returned to their preinjury level of sport.
Acknowledgment
The authors thank Mary Jane Robinson, LPN, and Sarah Johnson (Andrews Institute); Peter Soh, MD, Joseph Anderson, Forrest Lyons, Imran Mohiuddin, and Matthew Prevost (University of South Alabama); and Jeffrey Reese (Florida State University) for their assistance with this project.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.S. has received educational support from Arthrex and Smith & Nephew and has received grants for fellowship training from DJO. J.R.A. is a consultant for Arthrex and Halyard Health and receives educational support from Smith & Nephew.
Ethical approval for this study was obtained from the Baptist Hospital Institutional Review Board.
References
- 1. 2014-15 high school athletics participation survey results. Available at: http://www.nfhs.org/ParticipationStatics/PDF/2014-15_Participation_Survey_Results.pdf. Accessed January 18, 2016.
- 2. Alberta FG, ElAttrache NS, Bissell S, et al. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sports Med. 2010;38(5):903–911. [DOI] [PubMed] [Google Scholar]
- 3. Andrews JR, Jost PW, Cain EL. The ulnar collateral ligament procedure revisited: the procedure we use. Sports Health. 2012;4(5):438–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23(4):407–413. [DOI] [PubMed] [Google Scholar]
- 5. Cain EL, Andrews JR, Dugas JR, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow-up. Am J Sports Med. 2010;38(12):2426–2434. [DOI] [PubMed] [Google Scholar]
- 6. Clark NJ, Desai VS, Dines JD, Morrey ME, Camp CL. Nonreconstruction options for treating medial ulnar collateral ligament injuries of the elbow in overhead athletes. Curr Rev Musculoskelet Med. 2018;11(1):48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Committee on Sports Medicine and Fitness. American Academy of Pediatrics: risk of injury from baseball and softball in children. Pediatrics. 2001;107(4):782–784. [DOI] [PubMed] [Google Scholar]
- 8. Conway JE, Jobe FW, Glousman RE, Pink M. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74(1):67–83. [PubMed] [Google Scholar]
- 9. Deal JB, Smith E, Heard W, O’Brien MJ, Savoie FH. Platelet-rich plasma for primary treatment of partial ulnar collateral ligament tears: MRI correlation with results. Orthop J Sports Med. 2017;5(11):23259 6711773823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dines JS, Williams PN, ElAttrache N, et al. Platelet-rich plasma can be used to successfully treat elbow ulnar collateral ligament insufficiency in high-level throwers. Am J Orthop (Belle Mead NJ). 2016;45(5):296–300. [PubMed] [Google Scholar]
- 11. Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44(3):735–741. [DOI] [PubMed] [Google Scholar]
- 12. Erickson BJ, Chalmers PN, Bush-Joseph CA, Verma NN, Romeo AA. Ulnar collateral ligament reconstruction of the elbow: a systematic review of the literature. Orthop J Sports Med. 2015;3(12):23259 67115618914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Erickson BJ, Nwachukwu BU, Rosas S, et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43(7):1770–1774. [DOI] [PubMed] [Google Scholar]
- 14. Fleisig GS, Andrews JR. Prevention of elbow injuries in youth baseball pitchers. Sports Health. 2012;4(5):419–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hurd WJ, Eby S, Kaufman KR, Murthy NS. Magnetic resonance imaging of the throwing elbow in the uninjured, high school–aged baseball pitcher. Am J Sports Med. 2011;39(4):722–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68(8):1158–1163. [PubMed] [Google Scholar]
- 17. Jones KJ, Dines JS, Rebolledo BJ, et al. Operative management of ulnar collateral ligament insufficiency in adolescent athletes. Am J Sports Med. 2014;42(1):117–121. [DOI] [PubMed] [Google Scholar]
- 18. Lyman S, Fleisig GS. Baseball injuries. Med Sport Sci. 2005;49:9–30. [DOI] [PubMed] [Google Scholar]
- 19. Lyman S, Fleisig GS, Andrews JR, Osinski ED. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am J Sports Med. 2002;30(4):463–468. [DOI] [PubMed] [Google Scholar]
- 20. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001;33(11):1803–1810. [DOI] [PubMed] [Google Scholar]
- 21. Mahure SA, Mollon B, Shamah SD, Kwon YW, Rokito AS. Disproportionate trends in ulnar collateral ligament reconstruction: projections through 2025 and a literature review. J Shoulder Elbow Surg. 2016;25(6):1005–1012. [DOI] [PubMed] [Google Scholar]
- 22. Marshall NE, Keller RA, Van Holsbeeck M, Moutzouros V. Ulnar collateral ligament and elbow adaptations in high school baseball pitchers. Sports Health. 2015;7(6):484–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. O’Brien DF, O’Hagan T, Stewart R, et al. Outcomes for ulnar collateral ligament reconstruction: a retrospective review using the KJOC assessment score with two-year follow-up in an overhead throwing population. J Shoulder Elbow Surg. 2015;24(6):934–940. [DOI] [PubMed] [Google Scholar]
- 24. Olsen SJ, Fleisig GS, Dun S, Loftice J, Andrews JR. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006;34(6):905–912. [DOI] [PubMed] [Google Scholar]
- 25. Osbahr DC, Cain EL, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42(6):1333–1342. [DOI] [PubMed] [Google Scholar]
- 26. Petty DH. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;32(5):1158–1164. [DOI] [PubMed] [Google Scholar]
- 27. Podesta L, Crow SA, Volkmer D, Bert T, Yocum LA. Treatment of partial ulnar collateral ligament tears in the elbow with platelet-rich plasma. Am J Sports Med. 2013;41(7):1689–1694. [DOI] [PubMed] [Google Scholar]
- 28. Pytiak AV, Stearns P, Bastrom TP, et al. Are the current Little League pitching guidelines adequate? A single-season prospective MRI study. Orthop J Sports Med. 2017;5(5):232596711770485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tyler TF, Mullaney MJ, Mirabella MR, Nicholas SJ, McHugh MP. Risk factors for shoulder and elbow injuries in high school baseball pitchers: the role of preseason strength and range of motion. Am J Sports Med. 2014;42(8):1993–1999. [DOI] [PubMed] [Google Scholar]
- 30. Wilk KE, Arrigo CA, Hooks TR, Andrews JR. Rehabilitation of the overhead throwing athlete: there is more to it than just external/internal rotation strengthening. PM R. 2016;8(suppl 3):S78–S90. [DOI] [PubMed] [Google Scholar]
- 31. Wilk KE, Meister K, Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30(1):136–151. [DOI] [PubMed] [Google Scholar]
- 32. World Health Organization. Adolescent development. Available at: http://www.who.int/maternal_child_adolescent/topics/adolescence/dev/en/. Accessed February 12, 2016.
- 33. Zaremski JL, Horodyski M, Donlan RM, Brisbane ST, Farmer KW. Does geographic location matter on the prevalence of ulnar collateral ligament reconstruction in collegiate baseball pitchers? Orthop J Sports Med. 2015;3(11):23259 67115616582. [DOI] [PMC free article] [PubMed] [Google Scholar]