Abstract
Background:
Anterior cruciate ligament (ACL) injuries are frequently associated with bone bruises, and their presence may be associated with concomitant intra- and extra-articular injuries.
Purpose:
To investigate the prevalence and pattern of distribution of bone bruises in patients with acute ACL tears from noncontact sports trauma and their association with specific intra- and extra-articular injuries.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A total of 168 patients underwent magnetic resonance imaging (MRI) within 6 weeks of sustaining an ACL tear. Information regarding their demographics as well as MRI evidence of bone bruise patterns and associated injuries was carefully documented. Univariate and multivariate logistic regression analyses were performed to determine the association between bone bruises and concomitant intra- and extra-articular injuries seen on MRI.
Results:
Bone bruises were observed in 155 (92.3%) of 168 patients. The prevalence of bone bruises was 83.9%, 78.6%, 56.5%, and 29.8% on the lateral tibial plateau, lateral femoral condyle, medial tibial plateau, and medial femoral condyle, respectively. A total of 110 (65.5%) patients had bone bruises in both the medial and lateral compartments of the knee, 41 (24.4%) had isolated lateral compartment bone bruises, 4 (2.4%) had isolated medial compartment bone bruises, and 13 (7.7%) did not have any bone bruises. None of the demographic factors were significantly associated with the presence or absence of bone bruises. The presence of bone bruises was significantly associated with lateral meniscal injuries (P = .05). Lateral compartment bone bruises were significantly associated with lateral meniscal injuries (P = .034), while bone bruises affecting both the lateral and medial compartments were significantly associated with medial collateral ligament (MCL) injuries (P = .044) and lateral collateral ligament (LCL) injuries (P = .038) in addition to lateral meniscal injuries (P = .022).
Conclusion:
Bone bruises are common in patients with acute ACL tears after noncontact sports injuries. The compartmental distribution of bone bruises is associated with concomitant intra- and extra-articular injuries. Bone bruises involving the lateral compartment of the knee are associated with lateral meniscal injuries, while bone bruises involving both the lateral and medial compartments of the knee are associated with MCL and LCL injuries in addition to lateral meniscal injuries.
Keywords: bone bruise, anterior cruciate ligament, noncontact sports trauma, magnetic resonance imaging
Bone bruises are trabecular marrow edema seen on magnetic resonance imaging (MRI) and are frequently associated with anterior cruciate ligament (ACL) injuries.3,9,18,19,25 Their formation and location within specific compartments are most often the result of high-pressure collision or compression between the patient’s tibia and femur. Bone marrow edema may also be seen at the osseous attachment sites of ligaments and the joint capsule after distraction or tension injuries. The extent and severity of posttraumatic bone marrow edema are thought to be a representation of the amount of energy involved in the injury and the mechanism of injury.7,14,22,35
ACL tears are commonly associated with sports injuries and arise from both contact and noncontact injury mechanisms.1,16,33 The greater intensity and depth of bone bruising seen in association with noncontact sports injuries as compared with contact sports injuries suggest that a greater amount of energy is involved in these injuries.33 As ACL injuries are frequently associated with other intra- and extra-articular injuries of the knee, the location and extent of bone bruises within the specific compartments have been postulated to provide valuable insights regarding concomitant intra- and extra-articular injuries.2,13,23,30,34
This study aimed to investigate the demographic factors, prevalence, and pattern of distribution of bone bruises and their association with intra- (chondral/medial meniscal/lateral meniscal) and extra-articular (medial collateral ligament [MCL]/lateral collateral ligament [LCL]) injuries in patients with an acutely injured ACL after noncontact sports trauma. The hypothesis of our study was that the prevalence of intra- and extra-articular injuries would be significantly associated with an increase in bone bruise involvement from the lateral compartment alone to both the medial and lateral compartments of the knee.
Methods
Participants
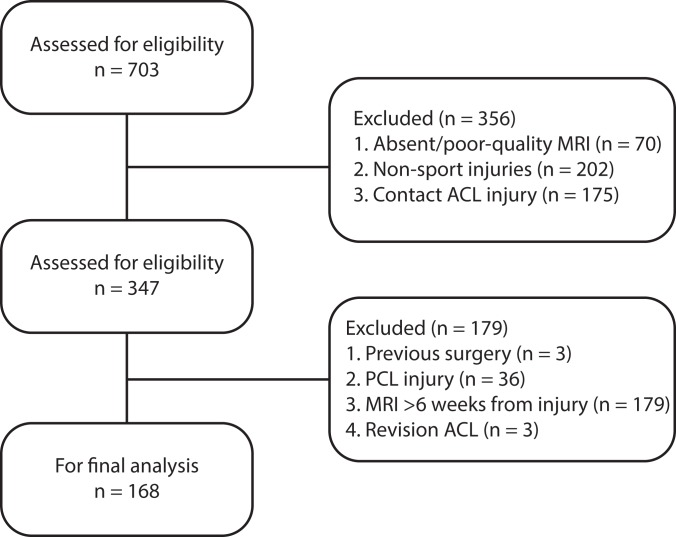
The present study was a retrospective analysis of a prospectively maintained database of patients who underwent arthroscopic ACL reconstruction surgery at our institution from January 2013 to August 2016. A total of 703 ACL reconstruction procedures were performed during this period. Ethical approval for this study was obtained from our institution’s domain-specific review board.
The inclusion criteria comprised (1) MRI performed within 6 weeks of sustaining the injury, (2) injuries sustained during sports activities, and (3) noncontact mechanisms of injury. Our exclusion criteria included (1) prior surgery in the affected knee, (2) posterior cruciate ligament ruptures, (3) poor-quality MRI scans affecting interpretation or absent MRI results, (4) revision ACL reconstruction, and (5) nonsports injuries.
Based on these criteria, 168 (23.9%) of 703 patients were eligible for this study. A flowchart showing the application of the inclusion and exclusion criteria and the derivation of the study group is presented in Figure 1. We collected the following information for all patients who met our inclusion criteria: demographics (age, sex, body mass index [BMI], and race), injury details (date of injury, mechanism of injury, date of first clinic visit, and date of MRI), and MRI findings (bone bruises, lateral and medial meniscal injuries, chondral injuries, and MCL/LCL injuries). We defined a noncontact sports injury as one that occurred with no bodily contact with another player or when the injured knee was in no direct contact with any other object, as reported by the patient.
Figure 1.
Flowchart of patient selection. ACL, anterior cruciate ligament; MRI, magnetic resonance imaging; PCL, posterior cruciate ligament.
MRI Acquisition and Interpretation
As bone bruises show dynamic changes,3,5,11 only patients who underwent MRI within 6 weeks of sustaining the injury were included in this study. All the images were interpreted in a desktop computer using Centricity Universal Viewer software (GE Healthcare). The imaging protocol consisted of coronal and sagittal images obtained in proton density–weighted fat-suppressed, T2-weighted fat-suppressed, and T1-weighted high-resolution sequences. All the MRI scans were read and interpreted by an orthopaedic sports medicine fellow (P.A.).
A bone bruise was defined as increased signal density on the proton density–weighted fat-suppressed and T2-weighted images and decreased signal density on the T1-weighted images.26,29 The specific sites of bone bruises (medial femoral condyle, lateral femoral condyle, medial tibial plateau, lateral tibial plateau) were identified and documented. Bone bruises affecting the lateral compartment were defined as those involving the lateral femoral condyle and/or lateral tibial plateau, while bone bruises affecting the medial compartment were defined as those involving the medial femoral condyle and/or medial tibial plateau.
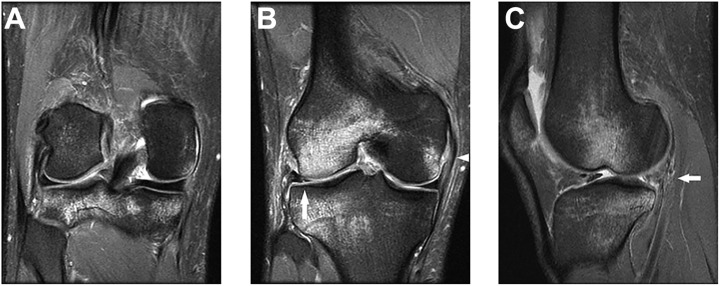
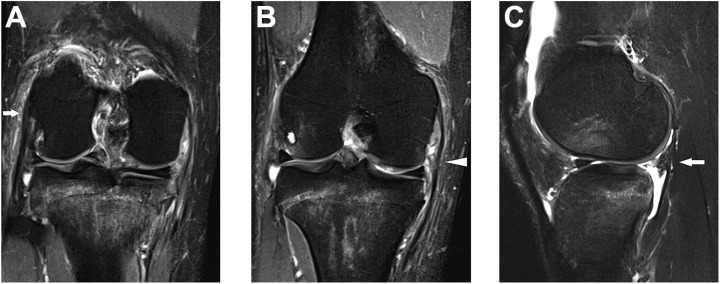
Associated intra-articular injuries involving the meniscus, cartilage, and collateral ligaments were identified on MRI. Meniscal injuries and chondral injuries were graded as either present or absent in T2-weighted and proton density–weighted fat-suppressed images. Meniscal injuries were identified as increased signal intensity along with disruption in substance or communication with the articular surface. Chondral injuries were defined as abnormal signal intensity between the articular cartilage and subchondral bone. MCL and LCL injuries were classified on MRI according to the system described by Rasenberg et al,24 and injuries of any grade were counted (Figures 2 and 3).
Figure 2.
(A, B) Coronal proton density–weighted fat-saturated images and (C) fat-suppressed T2-weighted image illustrating bone bruising in both the medial and lateral compartments with a grade 2 injury of the medial collateral ligament (white triangle) with a lateral meniscal tear (solid arrow) in the posterior horn and body.
Figure 3.
(A, B) Coronal proton density–weighted fat-saturated images showing bone bruising in both the medial and lateral compartments with periligamentous high-signal intensity in the medial collateral ligament (white triangle) and lateral collateral ligament (right-facing arrow), suggestive of a grade 2 injury. (C) Fat-suppressed T2-weighted image illustrating bone bruising on the lateral femoral condyle and tibial plateau with a full-thickness lateral meniscal tear (left-facing arrow) in the posterior horn.
Statistical Analysis
The 168 patients were first classified according to the presence or absence of bone bruises. Demographic and background variables (age, sex, race, BMI) and the presence of associated injuries (medial meniscal, lateral meniscal, chondral, MCL, LCL) identified on MRI were compared between these 2 groups of patients with the use of the chi-square test for categorical variables. Patients were then further classified based on the absence or presence of bone bruises in the medial or lateral compartment. Specifically, bone bruises were classified as absent, present in the lateral compartment only, present in the medial compartment only, or present in both the medial and lateral compartments. A similar classification was used in previous studies.17,35 The presence of associated injuries (medial and lateral meniscal, chondral, MCL, and LCL) was compared among the patients in these categories.
Finally, patients were classified according to the extent of their bone bruises. A diffuse bone bruise was defined as involvement of >2 of 4 sites (medial femoral condyle, lateral femoral condyle, medial tibial plateau, lateral tibial plateau), while a localized bone bruise was defined as involvement of ≤2 sites. The presence of associated injuries (medial and lateral meniscal, chondral, MCL, and LCL) was compared among the patients in the 2 categories.
The aim of the primary exploratory analysis was to investigate the presence or absence of bone bruises with respect to demographic factors such as age, sex, and BMI as well as concomitant injuries such as MCL, LCL, chondral, and meniscal injuries. The aim of the secondary exploratory analysis was to investigate the compartmental distribution and extent of bone bruises with respect to associated ligamentous, meniscal, and chondral injuries.
Statistical software SPSS version 22 (IBM) was used for analysis. Univariate and multivariate analyses were performed for variables in relation to bone contusions. A univariate logistic regression model was used to generate the odds ratio (OR) for the variables. For the variables that showed statistical significance in the univariate logistic regression analysis, we then proceeded with a multiple logistic regression analysis to ascertain if the significant variables were independent of each other or confounded. The chi-square test was used for univariate analyses, and the Fisher exact test was used for analyses with ≤5 variables. Statistical significance was deemed as P < .05.
Results
Demographics and Characteristics
The mean age at the time of injury was 25.2 ± 7.0 years (range, 15-52 years), and mean BMI was 23.9 ± 3.8 kg/m2 (range, 16.9-34.7 kg/m2). The majority of the patients were aged ≤25 years, male, and of Chinese race and had a BMI of ≤25.0 kg/m2. Knee injuries were sustained during soccer (n = 76 patients), basketball (n = 20), netball (n = 10), Frisbee (n = 9), rugby (n = 8), trampoline (n = 7), badminton (n = 5), volleyball (n = 4), floorball (n = 4), and other (n = 25) (Table 1).
TABLE 1.
Patient Demographics (N = 168)
| n (%) | |
|---|---|
| Age at the time of injury, y | |
| ≤25 y | 113 (67.3) |
| >25 | 55 (32.7) |
| Sex | |
| Male | 126 (75.0) |
| Female | 42 (25.0) |
| Race | |
| Chinese | 91 (54.2) |
| Malay | 38 (22.6) |
| Indian | 20 (11.9) |
| Other | 19 (11.3) |
| Body mass index, kg/m2 | |
| ≤25.0 | 99 (58.9) |
| >25.0 | 50 (29.8) |
| Missing | 19 (11.3) |
Bone bruises were observed in 92.3% of the patients and were most often present on the lateral tibial plateau (83.9%), followed by the lateral femoral condyle (78.6%). A bone bruise was less frequently identified on the medial tibial plateau (56.5%) and least on the medial femoral condyle (29.8%). The detailed prevalence and distribution of bone bruises are shown in Table 2. The detailed prevalence of concomitant meniscal, chondral, and collateral ligament injuries is shown in Table 3.
TABLE 2.
Bone Bruise Characteristics
| n (%) | |
|---|---|
| Presence | |
| Present | 155 (92.3) |
| Absent | 13 (7.7) |
| Site | |
| Lateral femoral condyle | 132 (78.6) |
| Lateral tibial plateau | 141 (83.9) |
| Medial femoral condyle | 50 (29.8) |
| Medial tibial plateau | 95 (56.5) |
| Compartment | |
| Absent | 13 (7.7) |
| Isolated medial | 4 (2.4) |
| Isolated lateral | 41 (24.4) |
| Medial and lateral | 110 (65.5) |
| Extent | |
| Localized (≤2 of 4 sites) | 74 (44.0) |
| Diffuse (>2 of 4 sites) | 94 (56.0) |
TABLE 3.
Associated Injuries
| n (%) | |
|---|---|
| Meniscal | |
| Medial | 66 (39.3) |
| Lateral | 63 (37.5) |
| Chondral | 18 (10.7) |
| Collateral ligament | |
| Medial | 83 (49.4) |
| Grade 1 | 28 (16.7) |
| Grade 2 | 40 (23.8) |
| Grade 3 | 15 (8.9) |
| Lateral | 66 (39.3) |
| Grade 1 | 36 (21.4) |
| Grade 2 | 22 (13.1) |
| Grade 3 | 8 (4.8) |
Presence of Bone Bruises
Table 4 illustrates the multiple logistic regression models for the presence or absence of bone bruises. The subpopulations in the 2 groups were comparable in terms of age, sex, race, and BMI. Demographic factors (age, sex, race, BMI) were not significantly associated with the presence or absence of bone bruises. The presence of bone bruises was significantly associated with lateral meniscal injuries in both univariate (OR, 8.00 [95% CI, 1.01-63.09]; P = .02) and multivariate analyses (OR, 7.73 [95% CI, 0.97-61.34]; P = .05). The presence of bone bruises was not found to be significantly associated with medial meniscal, MCL, LCL, or chondral injuries.
TABLE 4.
Logistic Regression Analysesa
| Bone Bruises Absent (n = 13) | Bone Bruises Present (n = 155) | Univariate | Multivariate | |||
|---|---|---|---|---|---|---|
| P Value | OR (95% CI) | P Value | OR (95% CI) | |||
| Sex | ||||||
| Male | 9 (69.2) | 117 (75.5) | 1.00 | |||
| Female | 4 (30.8) | 38 (24.5) | .62 | 0.73 (0.21-2.51) | ||
| Age, y | 25.5 ± 6.8 | 25.2 ± 7.1 | ||||
| ≤25 | 10 (76.9) | 103 (66.5) | 1.00 | |||
| >25 | 3 (23.1) | 52 (33.5) | .44 | 1.68 (0.44-6.38) | ||
| Race | ||||||
| Chinese | 7 (53.8) | 84 (54.2) | 1.00 | |||
| Malay | 2 (15.4) | 36 (23.2) | .62 | 1.50 (0.30-7.57) | ||
| Indian | 1 (7.7) | 19 (12.3) | .67 | 1.58 (0.18-13.64) | ||
| Other | 3 (23.1) | 16 (10.3) | .27 | 0.44 (0.10-1.90) | ||
| BMI, kg/m2 | ||||||
| ≤25.0 | 8 (61.5) | 91 (58.7) | 1.00 | |||
| >25.0 | 4 (30.8) | 46 (29.7) | .99 | 1.01 (0.29-3.53) | ||
| MCL injury | ||||||
| No | 9 (69.2) | 76 (49.0) | 1.00 | |||
| Yes | 4 (30.8) | 79 (51.0) | .16 | 2.34 (0.69-7.92) | ||
| LCL injury | ||||||
| No | 11 (84.6) | 91 (58.7) | 1.00 | |||
| Yes | 2 (15.4) | 64 (41.3) | .07 | 3.87 (0.83-18.05) | .10 | 3.70 (0.78-17.52) |
| Chondral injury | ||||||
| No | 13 (100.0) | 137 (88.4) | 1.00 | |||
| Yes | 0 (0.0) | 18 (11.6) | .19 | NA | ||
| Medial meniscal injury | ||||||
| No | 8 (61.5) | 94 (60.6) | 1.00 | |||
| Yes | 5 (38.5) | 61 (39.4) | .95 | 1.04 (0.33-3.32) | ||
| Lateral meniscal injury | ||||||
| No | 12 (92.3) | 93 (60.0) | 1.00 | |||
| Yes | 1 (7.7) | 62 (40.0) | .02 | 8.00 (1.01-63.09) | .05 | 7.73 (0.97-61.34) |
aData are presented as n (%) or mean ± SD unless otherwise specified. BMI, body mass index; LCL, lateral collateral ligament; MCL, medial collateral ligament; NA, not applicable; OR, odds ratio.
Compartmental Distribution of Bone Bruises
Bone bruises were categorized as absent in 13 (7.7%), present in the medial compartment only in 4 (2.4%), present in the lateral compartment only in 41 (24.4%), and present in both the medial and lateral compartments in 110 patients (65.5%). There were no significant differences in terms of demographic factors, including age, sex, race, and BMI. Given the small sample size, the 4 patients who had an isolated medial compartment injury were not included in the following analysis.
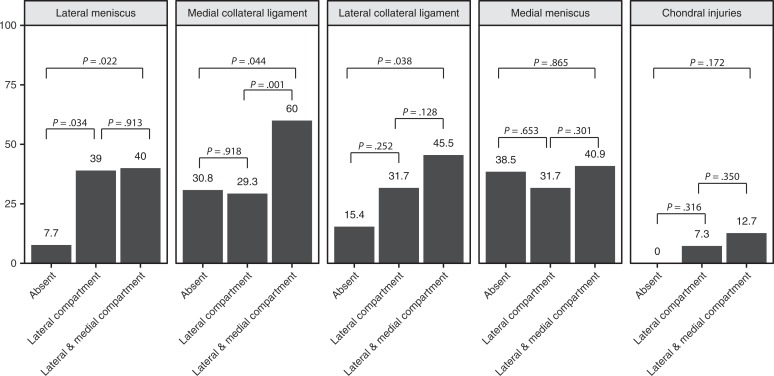
The prevalence of medial meniscal, lateral meniscal, chondral, MCL, and LCL injuries was compared among the 3 groups of patients: namely, those with no bone bruises, those with isolated lateral compartment bone bruises, and those with bone bruises involving both compartments.
The prevalence of lateral meniscal injuries was 7.7% (1/13) among patients with no bone bruises, 39.0% (16/41) among patients with isolated lateral compartment bone bruises, and 40.0% (44/110) among patients with bone bruises involving both compartments. Patients with isolated lateral compartment bone bruises had a significantly increased prevalence of lateral meniscal injuries compared with those with no bone bruises (P = .034) and similarly for those with both lateral and medial compartment bone bruises when compared with those with no bone bruises (P = .022). However, there was no significant difference in the prevalence of lateral meniscal injuries between those with isolated lateral compartment bone bruises and those with both lateral and medial compartment bone bruises (Figure 4).
Figure 4.
Bar graphs showing the prevalence of lateral meniscal, medial and lateral collateral ligament, medial meniscal, and chondral injuries according to the involved compartment.
The prevalence of MCL injuries was 30.8% (4/13) among patients with no bone bruises, 29.3% (12/41) among patients with isolated lateral compartment bone bruises, and 60.0% (66/110) among patients with bone bruises involving both compartments. Patients with bone bruises involving both the lateral and medial compartments had a significantly increased prevalence of MCL injuries compared with patients with no bone bruises (P = .044) and those with isolated lateral compartment bone bruises (P = .001). There was no significant difference in terms of the prevalence of MCL injuries between patients with no bone bruises and those with isolated lateral compartment injuries (Figure 4).
The prevalence of LCL injuries was 15.4% (2/13) among patients with no bone bruises, 31.7% (13/41) among patients with isolated lateral compartment bone bruises, and 45.5% (50/110) among patients with bone bruises involving both compartments. Patients with bone bruises involving both the lateral and medial compartments had a significantly increased prevalence of LCL injuries compared with patients with no bone bruises (P = .038). There was no significant difference in terms of the prevalence of LCL injuries between patients with no bone bruises and patients with isolated lateral compartment injuries or those with isolated lateral compartment injuries versus both lateral and medial compartment injuries (Figure 4).
The prevalence of medial meniscal injuries was 38.5% (5/13) among patients with no bone bruises, 31.7% (13/41) among patients with isolated lateral compartment bone bruises, and 40.9% (45/110) among patients with bone bruises involving both compartments. The prevalence of chondral injuries was 0.0% (0/13) among patients with no bone bruises, 7.3% (3/41) among patients with isolated lateral compartment bone bruises, and 12.7% (14/110) among patients with bone bruises involving both compartments. There was no significant association between sidedness of bone bruises and medial meniscal injuries or chondral injuries (Figure 4).
Extent of Bone Bruises
The distribution of bone bruises among the 4 sites (medial femoral condyle, medial tibial plateau, lateral femoral condyle, lateral tibial plateau) was categorized as either diffuse (involving >2 sites) or localized (involving ≤2 sites). A diffuse bone bruise pattern was found in 94 patients (56.0%), while a localized pattern was found in 74 patients (44.0%). There were no significant differences between the 2 groups with regard to age, sex, race, or BMI.
The prevalence of medial meniscal, lateral meniscal, chondral, MCL, and LCL injuries was compared between patients with diffuse versus localized bone bruise patterns. Having a diffuse pattern was significantly associated with MCL injuries in both the univariate (OR, 2.84 [95% CI, 1.51-5.35]; P = .001) and multivariate analyses (OR, 2.58 [95% CI, 1.34-4.98]; P = .005) (Table 5). We also noted a trend toward statistical significance for diffuse versus localized bone bruise patterns being associated with LCL injuries in the univariate analysis (OR, 8.00 [95% CI, 1.01-63.09]; P = .053). No significant associations were found involving medial meniscal, lateral meniscal, and chondral injuries between the 2 groups of patients.
TABLE 5.
Logistic Regression Analyses on Extent of Bone Bruisesa
| Localized Bone Bruises (n = 74) | Diffuse Bone Bruises (n = 94) | Univariate | Multivariate | |||
|---|---|---|---|---|---|---|
| P Value | OR (95% CI) | P Value | OR (95% CI) | |||
| MCL injury | ||||||
| No | 48 (69.2) | 37 (70.7) | 1.0 | 1.0 | ||
| Yes | 26 (30.8) | 57 (29.3) | .001 | 2.84 (1.51-5.35) | .005 | 2.58 (1.34-4.98) |
| LCL injury | ||||||
| No | 51 (84.6) | 51 (68.3) | 1.0 | 1.0 | ||
| Yes | 23 (15.4) | 43 (31.7) | .053 | 1.87 (0.99-3.54) | .307 | 1.42 (0.72-2.81) |
| Chondral injury | ||||||
| No | 67 (100.0) | 83 (92.7) | 1.0 | |||
| Yes | 7 (0.0) | 11 (7.3) | .641 | NA | ||
| Medial meniscal injury | ||||||
| No | 49 (61.5) | 56 (68.3) | 1.0 | |||
| Yes | 25 (38.5) | 38 (31.7) | .982 | 1.01 (0.54-1.88) | ||
| Lateral meniscal injury | ||||||
| No | 45 (92.3) | 57 (61.0) | 1.0 | |||
| Yes | 29 (7.7) | 37 (39.0) | .377 | 1.33 (0.71-2.51) | ||
aData are presented as n (%) unless otherwise specified. LCL, lateral collateral ligament; MCL, medial collateral ligament; NA, not applicable.
Discussion
The most important findings of our study were that there was a high prevalence of bone bruises involving both the medial and lateral compartments (65.5%) and that bicompartmental bone bruise involvement was associated with a higher prevalence of collateral ligament injuries as well as lateral meniscal injuries. Posttraumatic bone bruises in the knee are commonly found in patients with acute ACL tears. They are thought to be responsible for a patient’s pain symptoms and protracted clinical recovery.13,14,30,32 Bone bruises after an ACL rupture are most commonly distributed over the lateral compartment and are attributed to a pivot-shift valgus injury of the knee.1,16,22,33 Various mechanisms for bone bruises in the medial compartment have been proposed, but their presence is predominantly attributed to anterior translation of the tibia during the primary pivot-shift injury33 and the contrecoup varus malalignment force as the knee reduces after the primary pivot-shift injury.14 A significantly higher level of energy is thought to be involved in these situations. The varus-valgus forces that cause this coup-contrecoup injury pattern may also lead to concomitant collateral ligament injuries.
Viskontas et al33 noted that a noncontact mechanism of injury imparts greater amounts of energy compared with a contact mechanism, and medial compartment bone bruises were more commonly seen in the noncontact group. In our present study, which only included patients with noncontact sports injuries, the overall prevalence of bone bruises was observed to be 92.3%, which was consistent with previous studies.2,12,28,33–35 The most common site of bone bruises was the lateral tibial plateau (83.9%), followed by the lateral femoral condyle (78.6%), medial tibial plateau (56.5%), and medial femoral condyle (29.8%).
Song et al28 evaluated bone bruises in patients with an acute ACL injury after a noncontact mechanism. The anatomic distribution of bone bruises was similar to our study, with the lateral tibial plateau (73.1%) being most commonly involved, followed by the lateral femoral condyle (60.6%). However, bone bruises involving the medial compartment, at the medial tibial plateau (21.2%) and medial femoral condyle (6.2%), were considerably lower.
Other studies have demonstrated similar patterns of bone bruises after an ACL injury, with the lateral compartment being more commonly involved than the medial compartment.2,12,28,34,35 Regarding the distribution of bone bruises, previous studies have suggested that the energy level involved in the injury progressively increased when comparing patients in whom bone bruises were absent, to those with bone bruises in the lateral compartment alone, and finally to those with bone bruises present in both compartments.2,35 Compared with previous studies, it was notable that the prevalence of patients with bone bruises involving the medial compartment, and thereby both compartments, was significantly higher in our study (65.5%), while the prevalence of bone bruises involving only the lateral compartment was lower (24.4%). This can be attributed to the greater amount of energy associated with the noncontact injury mechanism in sports trauma. It was rare for patients to have bone bruises involving only the medial compartment (2.4%), which was a similar finding in previous studies.35
ACL injuries are often associated with concomitant intra- and extra-articular structural injuries.31 Understanding these associations allows us to be alert to them on MRI and during arthroscopic surgery.6,13,15,29,33,34 The prevalence of lateral and medial meniscal injuries after an ACL injury in the acute phase has been reported to be 15% to 73% and 10% to 55%, respectively.4,6,10,15,19,20,30 In the present study, 37.5% of our patients had lateral meniscal injuries and 39.3% had medial meniscal injuries, which are comparable with previous studies.27,28,30,35 Chondral injuries, present in up to 15% of patients as described in a previous study,2 were less commonly identified in the present study (10.7%).
The results of our study showed that the presence of bone bruises is significantly associated with lateral meniscal injuries, which is a similar finding to previous studies.2,35 In fact, the typical lateral compartmental bone bruise pattern suggests that the lateral meniscus is compressed between the femur and tibia and that this probably leads to the development of lateral meniscal injuries.
The present study identified markedly more extra-articular injuries compared with previous studies. The prevalence of MCL injuries was 49.4% in our present study compared with 22% to 41% as previously described.6,20,35 LCL injuries in patients with an ACL rupture have not been well studied previously, and little data could be found regarding their prevalence (0%-16%),4,19 but they were present in 39.3% of patients in the present study. This may be explained by 3 potential reasons. First, the overall increased prevalence of bone bruises involving both compartments may reflect the higher energy mechanism associated with noncontact sports injuries in our cohort of patients. Second, as MRI was performed in the acute setting, that is, less than 6 weeks from the injury, this may have resulted in a higher likelihood of detecting signal changes pertaining to collateral ligament injuries. Third, injuries of all grades, ranging from a spectrum of sprains to complete tears, were included.
Yoon et al35 demonstrated that the prevalence of injuries to intra-articular structures including the medial and lateral menisci increased significantly as bone bruise distribution progressed from absent to the lateral compartment alone to involvement of both the lateral and medial compartments. The authors also found a trend toward significance regarding the prevalence of MCL injuries as bone contusion distribution progressed.
The present study demonstrated that the prevalence of lateral meniscal injuries significantly increased as bone bruises progressed from absent to involving the lateral compartment to present in both compartments in patients with ACL injuries. Also, as bone bruises progressed from involving only the lateral compartment to involving both compartments, extra-articular injuries including MCL and LCL injuries increased in prevalence significantly. This leads us to the recognition that the presence of bone bruises involving the lateral compartment is significantly associated with lateral meniscal injuries, while the presence of bone bruises involving both compartments is significantly associated with extra-articular injuries including MCL and LCL injuries as well as lateral meniscal injuries.
We also included an analysis regarding the extent of bone bruise distribution and its association with concomitant injuries. Previous studies have assessed the severity of bone bruises according to their size and depth.2,12,28 However, this is more difficult to interpret in the clinic. As we aimed to arrive at a simpler grading system that clinically correlates with associated injuries, we defined bone bruises as diffuse when >2 of 4 sites (medial tibial plateau, medial femoral condyle, lateral tibial plateau, lateral femoral condyle) were involved and localized when ≤2 sites were involved. We found that a diffuse bone bruise pattern was associated with a significantly increased prevalence of MCL injuries as well as a trend toward significance for LCL injuries when compared with a localized pattern.
The findings of our study indicate that the pattern of distribution of bone bruises is significantly associated with the presence of specific concomitant injuries. The identification of such patterns on MRI in patients with acute ACL injuries should prompt clinicians to look out for these associated injuries on both clinical examination and MRI. The accurate determination of associated injuries is important, as these injuries influence treatment plans as well as outcomes in patients with ACL tears.
The strengths of our study include, first, a large study population of 168 patients compared with previous studies. Second, we only included patients with MRI performed within 6 weeks of the injury, which allowed us to establish better accuracy regarding the prevalence of bone bruises and associated injuries after the ACL injury. Third, our study population was more homogenous, as we only included patients with ACL injuries secondary to noncontact sports injuries. Finally, this study adds to the previous literature analyzing LCL injuries and their relation to bone bruises in patients with ACL injuries.
Our study has several limitations. First, the study was MRI based, and a comparison with clinical examination and arthroscopic intra-articular findings was not made. However, a meta-analysis conducted by Oei et al21 indicates that MRI shows high sensitivity and specificity in the diagnosis of meniscal tears: 79% sensitivity and 96% specificity for lateral meniscal tears and 93% and 88%, respectively, for medial meniscal tears. In addition, Friemert et al8 suggested MRI as a suitable investigation tool in view of its high specificity (97%-99%) and high negative predictive value (97%-98%) for diagnosing chondral lesions of the knee. MRI grading of collateral ligament injuries has also been shown to correlate closely with clinical and instrumented assessments of these injuries.24
A second limitation is that our study included all grades of collateral ligament injuries, including sprains. This may have led to a higher than expected prevalence of concomitant collateral ligament injuries. Although this may not be of concern in terms of surgical treatment, it does offer an improved understanding of the mechanisms of injury involved in noncontact sports trauma. Third, no intraobserver or interobserver comparisons were made for the diagnosis of chondral, meniscal, and collateral ligament injuries, as the MRI scans were read by a single reader.
Conclusion
The compartmental distribution of bone bruises is associated with concomitant intra- and extra-articular injuries. Bone bruises involving the lateral compartment of the knee are more frequently associated with lateral meniscal injuries, while bone bruises involving both the lateral and medial compartments of the knee are associated with MCL and LCL injuries in addition to lateral meniscal injuries. Knowledge of the compartmental distribution of bone bruises and its association with concomitant injuries adds to our understanding of the pathomechanics of ACL tears.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the National Healthcare Group (NHG DSRB ref: 2016/01003).
References
- 1. Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players, part 1: mechanisms of injury and underlying risk factors. Knee Surg Sports Traumatol Arthrosc. 2009;17(7):705–729. [DOI] [PubMed] [Google Scholar]
- 2. Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med. 2013;41(8):1801–1807. [DOI] [PubMed] [Google Scholar]
- 3. Bretlau T, Tuxøe J, Larsen L, Jørgensen U, Thomsen HS, Lausten G. Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc. 2002;10(2):96–101. [DOI] [PubMed] [Google Scholar]
- 4. Cerabona F, Sherman MF, Bonamo JR, Sklar J. Patterns of meniscal injury with acute anterior cruciate ligament tears. Am J Sports Med. 1988;16(6):603–609. [DOI] [PubMed] [Google Scholar]
- 5. Davies N, Niall D, King L, Lavelle J, Healy J. Magnetic resonance imaging of bone bruising in the acutely injured knee: short-term outcome. Clin Radiol. 2004;59(5):439–445. [DOI] [PubMed] [Google Scholar]
- 6. Duncan JB, Hunter R, Purnell M, Freeman J. Meniscal injuries associated with acute anterior cruciate ligament tears in alpine skiers. Am J Sports Med. 1995;23(2):170–172. [DOI] [PubMed] [Google Scholar]
- 7. Dunn WR, Spindler KP, Amendola A, et al. Which preoperative factors, including bone bruise, are associated with knee pain/symptoms at index anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(9):1778–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Friemert B, Oberländer Y, Schwarz W, et al. Diagnosis of chondral lesions of the knee joint: can MRI replace arthroscopy? A prospective study. Knee Surg Sports Traumatol Arthrosc. 2004;12(1):58–64. [DOI] [PubMed] [Google Scholar]
- 9. Gönç U, Kayaalp A, Irgit K. [Bone bruises of the knee]. Acta Orthop Traumatol Turc. 2007;41(suppl 2):98–104. [PubMed] [Google Scholar]
- 10. Hagino T, Ochiai S, Senga S, et al. Meniscal tears associated with anterior cruciate ligament injury. Arch Orthop Trauma Surg. 2015;135(12):1701–1706. [DOI] [PubMed] [Google Scholar]
- 11. Hanypsiak BT, Spindler KP, Rothrock CR, et al. Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med. 2008;36(4):671–677. [DOI] [PubMed] [Google Scholar]
- 12. Illingworth KD, Hensler D, Casagranda B, Borrero C, van Eck CF, Fu FH. Relationship between bone bruise volume and the presence of meniscal tears in acute anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2181–2186. [DOI] [PubMed] [Google Scholar]
- 13. Johnson DL, Urban WP, Caborn DN, Vanarthos WJ, Carlson CS. Articular cartilage changes seen with magnetic resonance imaging–detected bone bruises associated with acute anterior cruciate ligament rupture. Am J Sports Med. 1998;26(3):409–414. [DOI] [PubMed] [Google Scholar]
- 14. Kaplan PA, Gehl RH, Dussault RG, Anderson MW, Diduch DR. Bone contusions of the posterior lip of the medial tibial plateau (contrecoup injury) and associated internal derangements of the knee at MR imaging. Radiology. 1999;211(3):747–753. [DOI] [PubMed] [Google Scholar]
- 15. Keene GC, Bickerstaff D, Rae PJ, Paterson RS. The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med. 1993;21(5):672–679. [DOI] [PubMed] [Google Scholar]
- 16. Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359–367. [DOI] [PubMed] [Google Scholar]
- 17. Mair SD, Schlegel TF, Gill TJ, Hawkins RJ, Steadman JR. Incidence and location of bone bruises after acute posterior cruciate ligament injury. Am J Sports Med. 2004;32(7):1681–1687. [DOI] [PubMed] [Google Scholar]
- 18. Mandalia V, Fogg AJB, Chari R, Murray J, Beale A, Henson JHL. Bone bruising of the knee. Clin Radiol. 2005;60(6):627–636. [DOI] [PubMed] [Google Scholar]
- 19. Murphy BJ, Smith RL, Uribe JW, Janecki CJ, Hechtman KS, Mangasarian RA. Bone signal abnormalities in the posterolateral tibia and lateral femoral condyle in complete tears of the anterior cruciate ligament: a specific sign? Radiology. 1992;182(1):221–224. [DOI] [PubMed] [Google Scholar]
- 20. Nikolić DK. Lateral meniscal tears and their evolution in acute injuries of the anterior cruciate ligament of the knee arthroscopic analysis. Knee Surg Sports Traumatol Arthrosc. 1998;6(1):26–30. [DOI] [PubMed] [Google Scholar]
- 21. Oei EHG, Nikken JJ, Verstijnen ACM, Ginai AZ, Myriam Hunink MG. MR imaging of the menisci and cruciate ligaments: a systematic review. Radiology. 2003;226(3):837–848. [DOI] [PubMed] [Google Scholar]
- 22. Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med. 2014;44(2):281–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pezeshki S, Vogl TJ, Pezeshki MZ, Daghighi MH, Pourisa M. Association of the type of trauma, occurrence of bone bruise, fracture and joint effusion with the injury to the menisci and ligaments in MRI of knee trauma. Muscles Ligaments Tendons J. 2016;6(1):161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rasenberg EI, Lemmens JAM, van Kampen A, et al. Grading medial collateral ligament injury: comparison of MR imaging and instrumented valgus-varus laxity test-device: a prospective double-blind patient study. Eur J Radiol. 1995;21(1):18–24. [DOI] [PubMed] [Google Scholar]
- 25. Rosen MA, Jackson DW, Berger PE. Occult osseous lesions documented by magnetic resonance imaging associated with anterior cruciate ligament ruptures. Arthroscopy. 1991;7(1):45–51. [DOI] [PubMed] [Google Scholar]
- 26. Sanders TG, Medynski MA, Feller JF, Lawhorn KW. Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics. 2000;20(suppl 1):S135–S151. [DOI] [PubMed] [Google Scholar]
- 27. Shelbourne KD, Porter DA. Anterior cruciate ligament–medial collateral ligament injury: nonoperative management of medial collateral ligament tears with anterior cruciate ligament reconstruction. A preliminary report. Am J Sports Med. 1992;20(3):283–286. [DOI] [PubMed] [Google Scholar]
- 28. Song G, Zhang H, Wang Q, Zhang J, Li Y, Feng H. Bone contusions after acute noncontact anterior cruciate ligament injury are associated with knee joint laxity, concomitant meniscal lesions, and anterolateral ligament abnormality. Arthroscopy. 2016;32(11):2331–2341. [DOI] [PubMed] [Google Scholar]
- 29. Speer KP, Spritzer CE, Bassett FH III, Feagin JA, Jr, Garrett WE., Jr Osseous injury associated with acute tears of the anterior cruciate ligament. Am J Sports Med. 1992;20(4):382–389. [DOI] [PubMed] [Google Scholar]
- 30. Spindler KP, Schils JP, Bergfeld JA, et al. Prospective study of osseous, articular, and meniscal lesions in recent anterior cruciate ligament tears by magnetic resonance imaging and arthroscopy. Am J Sports Med. 1993;21(4):551–557. [DOI] [PubMed] [Google Scholar]
- 31. Tandogan RN, Taşer Ö, Kayaalp A, et al. Analysis of meniscal and chondral lesions accompanying anterior cruciate ligament tears: relationship with age, time from injury, and level of sport. Knee Surg Sports Traumatol Arthrosc. 2004;12(4):262–270. [DOI] [PubMed] [Google Scholar]
- 32. Thompson RC, Oegema TR, Lewis JL, Wallace L. Osteoarthritic changes after acute transarticular load: an animal model. J Bone Joint Surg Am. 1991;73(7):990–1001. [PubMed] [Google Scholar]
- 33. Viskontas DG, Giuffre BM, Duggal N, Graham D, Parker D, Coolican M. Bone bruises associated with ACL rupture: correlation with injury mechanism. Am J Sports Med. 2008;36(5):927–933. [DOI] [PubMed] [Google Scholar]
- 34. Wittstein J, Vinson E, Garrett W. Comparison between sexes of bone contusions and meniscal tear patterns in noncontact anterior cruciate ligament injuries. Am J Sports Med. 2014;42(6):1401–1407. [DOI] [PubMed] [Google Scholar]
- 35. Yoon KH, Yoo JH, Kim K-I. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93:1510–1518. [DOI] [PubMed] [Google Scholar]