Abstract
We report the case of a 66-year-old male patient with massive ossification of the distal portion of the Achilles tendon, as a late consequence of a surgical release for club foot conducted in his childhood. The singularity of the case report derives from its clinical features: the bone mass was of abnormal dimensions, almost substituting the entire tendon; the condition had always been asymptomatic, without deficits in range of motion, in absence of either pain or biomechanical defects with age. In fact, the condition was diagnosed just recently as a consequence of a tear. Despite an ultrasound diagnosis after the injury, only during the surgical treatment, a proper evaluation of the entity of the pathology was possible. Although the ossification of Achilles tendon is a rare clinical condition with a complex multifactorial etiology, in our case report, some of the elements in the patient’s medical history could be useful for the pathogenesis and early diagnosis of the disease. The aim of this case report is to emphasize the importance both of a correct evaluation of clinical history and of an accurate diagnosis, in order to conduct a proper management of this pathology.
Keywords: Achilles tendon, ossification, club foot
Introduction
The Achilles tendon (AT) is one of the longest and strongest tendons in the human body which can withstand loads up to 400 kg.1,2 The tendon is susceptible to several types of injuries as a consequence of both its continuous functional demands during gait and running and because of the poor blood supply. Heavy loads on AT, over time, can lead to cases of chronic inflammation, degeneration and various types of fracture.3 The ossification of the tendon is a very unusual clinical event4 and this is characterized by the presence of an ossified mass within the substance of the tendinous tissue. It is usually a firm, tender mass4 and should be considered for the swelling and the pain in the region of the posterior ankle. Severe ossification involving more than half of the tendon bulk is extremely rare.5,6 The etiology of the ossification of Achilles tendon (OAT) is largely unknown but the evidence in literature suggest a multifactorial etiology.
Case presentation
The case patient treated in our structure is a 66-year-old man who reported a spontaneous AT fracture during running activity. The patient has a height of 180 cm, weight of 90 kg and a body mass index of 27.77 kg/m2. He arrived to our Orthopedic Emergency Department after an acute trauma to the ankle declaring a sudden “pop” in the right region of the ankle while running, followed by a subsequent collapse. Previous medical features included a systemic arterial hypertension treated with β-blockers, a gout of acid uric, a vascular insufficiency at lower limbs and a prostatic hyperplasia; the patient is also a smoker (about 20 cigarettes/day). He was subjected to surgical unilateral correction of club foot (right side) during his childhood, through the simple tendon release technique. No pain complications resulted after the surgery and the ankle had always shown a normal mobility and functionality. Preliminary inspection showed a slight swelling on the right heel, but no skin changes or ecchymosis. The scar of the previous surgery along the back part of the ankle was not clear. Palpation revealed a discontinuity with palpable defect of the AT about 8 cm above the calcaneal tuberosity (in the proximal part of the tendon). Physical examination showed problems in active plantar flexion of the right foot and pain in passive dorsiflexion. The patient reported easily palpable dorsalis pedis and posterior tibial pulses. Sensory testing of the right leg resulted in the normal range. Our suspected diagnosis was “Atraumatic AT Lesion” and we performed an ultrasonography (US) in order to confirm our diagnosis. The US reported a fibers interruption a few centimeters above the proximal junction with gastrocnemius muscle. Furthermore, a partial lesion of the muscle fibers emerged. At the side of the rupture, a fluid area (hematoma) appeared, while the distal part of the tendon showed a great hyperechoic mass (Figure 1).
Figure 1.
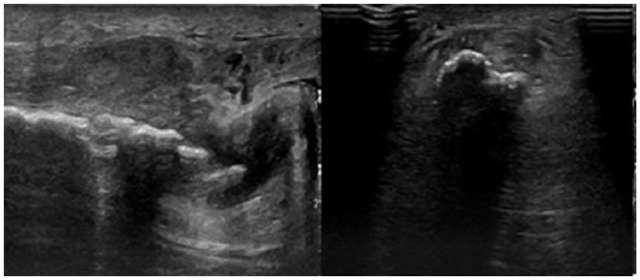
Longitudinal and transversal US view of the hyperechoic mass.
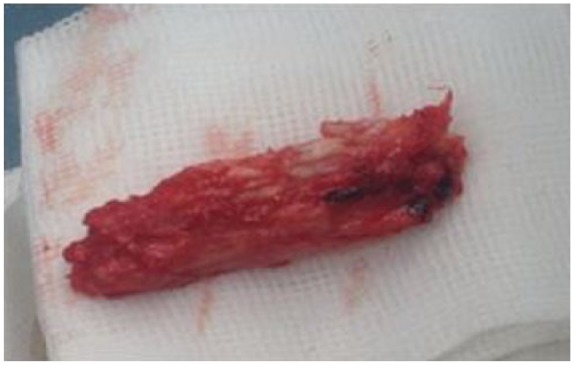
Surgery to repair the AT was performed at day 1 after pre-operative examinations. An incision of 8–10 cm was made over the palpable defect. The tendon tissue was found extremely variable. The rupture appeared as a joint between a normal soft tendinous tissue and an extremely hard one. A real “new” bone, by means of a very large heterotopic ossification, filled the whole thickness of the distal part of the structure. The size of the mass was wide (8.5 cm × 2.5 cm) and the mass itself was covered by fibrous fibers. For these reasons, the ossified part of the tendon was completely removed (Figures 2 and 3).
Figure 2.

The excision of the whole mass.
Figure 3.
“New bone” after complete excision.
As a result, a large gap appeared between the upper proximal part of the tendon above the rupture and the distal one below the ossified tissue that we removed; we therefore proceeded with the reconstruction of the tendon using modified Bosworth technique,7–9 turning down the gastrocnemius aponeurosis and doing a tendon flap plasty. Reconstruction was reinforced with the graft of plantar gracilis, using Lynn technique10 and absorbable suture (Vicryl) with no tension. The paratenon tissue and the subcutaneous tissue were sealed using an absorbable suture. The operation was successfully completed, and a short leg cast was applied to maintain the lower leg in an equine position. Histological analysis confirmed the heterotopic ossification, showing real trabecular bone tissue, osteoblasts and osteocytes along the entire tissue (Figure 4).
Figure 4.
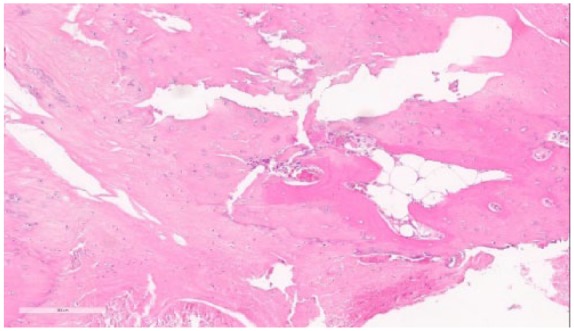
A histological section of the mass: transition from tendinous tissue toward trabecular bone tissue and osteoblasts.
Discussion
Accumulation of calcific deposits in the intra-tendinous tissue is a common pathology that can frequently occur to tendons.11 Nevertheless, the ossification of the tendons cannot be considered as an accumulation of calcific deposits. Indeed, while the process of calcification of tendinous tissue is well known, the origin of the cells involved in the tendon ossification process is still poorly understood.12 Since the first description in 1908, there have been very few cases of OAT reported in literature.4,13–16 Various hypotheses have been proposed in order to explain the uncommon and still not well-known process that leads to ossification within the substance of the tendon. None of the proposed hypotheses has been proved so far. However, the situation certainly develops from conditions of decreased oxygen tension, leading to the conversion of the tendon into a region rich in fibrocartilage where chondrocytes act calcium deposition.13 This physiological process has also been confirmed in several recent publications,17–19 although only a few pieces of evidence link causes and predisposing conditions.18,20 In similar diseases, such as idiopathic skeletal hyperostosis and ossificans myositis, skeletal tissue is thought to be a result of metaplasia of tenocytes into osteogenic cells. Furthermore, other predisposing conditions have been described such as fluorosis, Wilson’s disease, seronegative arthropathies, renal failure, gout and retinoid therapy, diabetes, genetic disorders in ossifications, neoplasm and chronic infection.6,18,21–25 Ghormley,21 in 1938, first observed that over 50% of the OAT cases were associated with previous trauma or surgery. Besides the rare pathology, in 1990, Morris and colleagues classified AT ossifications in three types, according to the different anatomical positions;16,26 in particular, our case of study can be ascribed to the second class (namely, lesion located 1–3 cm from the tendon insertion). Ossification can also be classified as either incomplete or complete;16 our case is included in the second condition because of the almost complete substitution of the distal part of the tendon with the heterotopic bone. As mentioned above, surgical treatments are among the main predisposing conditions for AT ossification. Furthermore, club foot surgical release can be considered as an extremely rare cause of OAT. The incidence of isolated club foot is of about 0.6–6.8 per 1000 newborns.27,28 Different approaches exist for the treatment of foot wrong position.28–30 The area of the operative treatment is always related to the severity of the deformity and in accordance with the clinical and standard radiographic results.31,32 In the past decades, various surgical procedures have been recommended to correct the irreducible equinus deformity between the third and the sixth months of life,33–36 but no universally accepted criteria are currently available in relation to the various surgical techniques.37 Our patient was subjected to surgical AT lengthening, in childhood, and little evidence is available in literature concerning complications for this type of treatment. The identification of the long-term complications and the late adverse effects of the surgical release of the tendon is very difficult because of the missing results in long-term follow-up.38,39 Recent accurate reviews are also lacking of long-term results, especially concerning adverse complications. As an example, the latest review from Cochrane failed in reviewing long-term complications.40 However, although the process of calcification of some of the portions of the tendon tissue has been described in relation to the surgery of our case report, massive ossifications have been noticed more rarely, never after simple tendon release for club foot.21–25 The recent case report published by Majeed et al.41 describes how multiple discrete deposits of ossification appeared after surgery for club foot, but without massive ossifications. Therefore, the diagnosis of AT ossification is based on clinical features such as discomfort, restriction of motion and disability in daily activities.42 Heel pain together with mass and swelling is the most common sign.43 Also, in the study from Majeed et al.,41 pain was shown as the predominant symptom. For these reasons, plain film radiography can be useful in order to reveal a calcified mass with free bone fragments or ossifications within the body of the tendon.4,21 Unfortunately, in our case, neither symptoms nor signs were reported by the patient and the condition has been silent for a long time (about 60 years), up to the unexpected tendon tear. Although tendon ossification remains a rare condition, historical elements should be properly evaluated in order to avoid wrong diagnosis. In our case, there have been two elements that could have been considered as possible causes of the pathology: past surgery for club foot and the gout.21–25 Probably, these two conditions together have predisposed to ossification, perhaps in a favorable hereditary pattern. Considering the pathogenesis of bone transition of soft tissues, chronic reduction in oxygen should be considered as a possible cause; along this view, in our patient, the vascular insufficiency of lower limbs and smoking might have been involved in the causality of OAT.13,17–20 The absence of a proper identification of the pathology can lead to a wrong diagnostic process. As a result, an incomplete diagnosis might lead to wrong treatments, especially when surgery is performed. Pre-operative planning cannot be correct. In fact, when a large gap remains after the removal of the ossification, a direct repair is almost impossible.14
Conclusion
Tendon ossification is a rare condition with multifactorial etiology. The history of any previous insult or surgery should be considered as a medical historical element predisposing OAT. Even if the surgical release of the tendon for club foot has been rarely associated with this kind of late effects, it should not be neglected as possible previous predisposing conditions. In rare cases, ossification could be partially asymptomatic, but this condition is unlikely in case of more severe conditions. Our evidence emphasizes the importance of a correct evaluation of the clinical history and an accurate diagnosis, in order to conduct a proper management of the disease. Without a proper diagnosis, planning for treatment, especially surgery, might be difficult or insufficient.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Francesco Manfreda  https://orcid.org/0000-0002-0807-3955
https://orcid.org/0000-0002-0807-3955
References
- 1. DeMaio M, Paine R, Drez D. Achilles tendonitis. Sports Med Rehabil Series 1995; 18: 195–204. [DOI] [PubMed] [Google Scholar]
- 2. Lemm M, Blake R, Colson J, et al. Achilles peritendinitis: a literature review with case report. J Am Podiatr Med Assoc 1992; 82: 482–490. [DOI] [PubMed] [Google Scholar]
- 3. Lesic A, Bumbasirevic M. Disorders of the Achilles tendon. Current Orthopaed 2004; 18(1): 63–75. [Google Scholar]
- 4. Yu JS, Witte D, Resnick D, et al. Ossification of the Achilles tendon: imaging abnormalities in 12 patients. Skeletal Radiol 1994; 23(2): 127–131. [DOI] [PubMed] [Google Scholar]
- 5. Doherty MJ, Ashton BA, Walsh S, et al. Vascular pericytes express osteogenic potential in vitro and in vivo. J Bone Miner Res 1998; 13(5): 828–838. [DOI] [PubMed] [Google Scholar]
- 6. Sobel E, Giorgini R, Hilfer J, et al. Ossification of a ruptured Achilles tendon: a case report in a diabetic patient. J Foot Ankle Surg 2002; 41(5): 330–334. [DOI] [PubMed] [Google Scholar]
- 7. Khiami F, Di Schino M, Sariali E, et al. Treatment of chronic Achilles tendon rupture by shortening suture and free sural triceps aponeurosis graft. Orthop Traumatol Surg Res 2013; 99(5): 585–591. [DOI] [PubMed] [Google Scholar]
- 8. Lee YS, Lin CC, Chen CN, et al. Reconstruction for neglected Achilles tendon rupture: the modified Bosworth technique. Orthopedics 2005; 28(7): 647–650. [DOI] [PubMed] [Google Scholar]
- 9. Chang Q, Huang X, Guan C. Treatment of chronic Achilles tendon rupture by use of allogeneic tendon. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2004; 18(4): 336–337. [PubMed] [Google Scholar]
- 10. Lynn TA. Repair of the torn Achilles tendon, using the plantaris tendon as a reinforcing membrane. J Bone Joint Surg Am 1966; 48(2): 268–272. [PubMed] [Google Scholar]
- 11. Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon: a controlled study of 891 patients. J Bone Joint Surg Am 1991; 73(10): 1507–1525. [PubMed] [Google Scholar]
- 12. Fenwick S, Harrall R, Hackney R, et al. Endochondral ossification in Achilles and patella tendinopathy. Rheumatology 2002; 41(4): 474–476. [DOI] [PubMed] [Google Scholar]
- 13. Uber HF. Tendinitis ossificans traumatica. Munchen Med Wochen 1908; 55: 674–675. [Google Scholar]
- 14. Ross KA, Smyth NA, Hannon CP, et al. An atraumatic case of extensive Achilles tendon ossification. Foot Ankle Surg 2014; 20(4): e59–64. [DOI] [PubMed] [Google Scholar]
- 15. Hatori M, Matsuda M, Kokubun S. Ossification of Achilles tendon–report of three cases. Arch Orthop Traum Surg 2002; 122(7): 414–417. [DOI] [PubMed] [Google Scholar]
- 16. Arora AJ, Arora R. Ossification of the bilateral Achilles tendon: a rare entity. Acta Radiol Open. Epub ahead of print 8 September 2015. DOI: 10.1177/2058460115599184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Uhthoff HK, Sarkar K, Maynard JA. Calcifying tendinitis: a new concept of its pathogenesis. Clin Orthop Relat R 1976; 118: 164–168. [PubMed] [Google Scholar]
- 18. Richards PJ, Braid JC, Carmont MR, et al. Achilles tendon ossification: pathology, imaging and aetiology. Disabil Rehabil 2008; 30: 1651–1665. [DOI] [PubMed] [Google Scholar]
- 19. Joshi N, Diaz E, Massons J. Achilles tendon ossification. Acta Orthop Belg 1994; 60: 432–433. [PubMed] [Google Scholar]
- 20. Cortbaoui C, Matta J, Elkattah R. Could ossification of the Achilles tendon have a hereditary component? Case Rep Orthop. Epub ahead of print 12 February 2013. DOI: 10.1155/2013/539740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ghormley JW. Ossification of the tendon Achilles. J Bone Joint Surg 1938; 20: 153–156. [Google Scholar]
- 22. Tamam C, Yildirim D, Tamam M, et al. Bilateral Achilles tendon ossification: diagnosis with ultrasonography and single photon emission computed tomography/computed tomography: case report. Med Ultrason 2011; 13(4): 320–322. [PubMed] [Google Scholar]
- 23. Wuenschel M, Trobisch P. Achilles tendon ossification after treatment with acitretin. J Dermatol Treat 2010; 21: 111–113. [DOI] [PubMed] [Google Scholar]
- 24. Rooney P. Intratendinous ossification. In: Hall BK. (ed.) Mechanisms of development and growth. Boca Raton, FL: CRC Press, pp. 47–84, 1994. [Google Scholar]
- 25. Battaglia T, Chandler J. Ossific tendonitis of the Achilles with tendon fracture. Orthopedics 2006; 29(5): 453–455. [DOI] [PubMed] [Google Scholar]
- 26. Morris KL, Giacopelli JA, Granoff D. Classifications of radiopaque lesions of the tendo Achilles. J Foot Surg 1990; 29: 533–542. [PubMed] [Google Scholar]
- 27. Pavone V, Bianca S, Grosso G, et al. Congenital talipes equinovarus: an epidemiological study in Sicily. Acta Orthop 2012; 83(3): 294–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhao DH, Rao WW, Zhao L, et al. Are incidence and severity of clubfoot related to the season of birth? World J Pediatr 2016; 12(3): 360–363. [DOI] [PubMed] [Google Scholar]
- 29. Dobbs MB, Gurnett CA. Update on clubfoot: etiology and treatment. Clin Orthop Relat R 2009; 467: 1146–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Morcuende JA. Congenital idiopathic clubfoot: prevention of late deformity and disability by conservative treatment with the Ponseti technique. Pediatr Ann 2006; 35: 128–130, 132–136. [DOI] [PubMed] [Google Scholar]
- 31. Ponseti IV. Treatment of congenital club foot. J Bone Joint Surg Am 1992; 74(3): 448–454. [PubMed] [Google Scholar]
- 32. Radler C. The Ponseti method for the treatment of congenital club foot: review of the current literature and treatment recommendations. Int Orthop 2013; 37: 1747–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Imhäuser G. Follow-up examinations: 30 Years of Imhäuser clubfoot treatment. Arch Orthop Trauma Surg 1980; 96: 259–704. [DOI] [PubMed] [Google Scholar]
- 34. Simons GW. Complete subtalar release in club feet: part I—a preliminary report. J Bone Joint Surg Am 1985; 67: 1044–1556. [PubMed] [Google Scholar]
- 35. Klaue K, Damsin JP. Heutige operative Therapie des angeborenen Klumpfußes. Ther Umsch 1991; 48: 784–789. [PubMed] [Google Scholar]
- 36. Reichel H, Lebek S, Milikic L, et al. Posteroplantar release for congenital clubfoot in children younger than 1 year. Clin Orthop Relat Res 2001; 387: 183–190. [DOI] [PubMed] [Google Scholar]
- 37. Fujak A, Forst R, Forst J. Outcome after Achilles tendon lengthening with a posterior capsulolysis according to Imhäuser in idiopathic congenital clubfoot. Ortop Traumatol Rehabil 2008; 10(4): 367–376. [PubMed] [Google Scholar]
- 38. Segev E, Keret D, Lokiec F, et al. Early experience with the Ponseti method for the treatment of congenital idiopathic clubfoot. Isr Med Assoc J 2005; 7: 307–310. [PubMed] [Google Scholar]
- 39. Eberhardt O, Schelling K, Parsch K, et al. Treatment of congenital clubfoot with the Ponseti method. Z Orthop 2006; 144: 497–501, 31. [DOI] [PubMed] [Google Scholar]
- 40. Gray K, Pacey V, Gibbons P, et al. Interventions for congenital talipes equinovarus (clubfoot). Cochrane Db Syst Rev 2012; 18(4): CD008602. [DOI] [PubMed] [Google Scholar]
- 41. Majeed H, Deall C, Mann A, et al. Multiple intratendinous ossified deposits of the Achilles tendon: case report of an unusual pattern of ossification. Foot Ankle Surg 2015; 21(2): e33–15. [DOI] [PubMed] [Google Scholar]
- 42. Sasaki D, Hatori M, Kotajima S, et al. Ossification of the Achilles tendon—a case report. Scott Med J 2005; 50(4): 174–175. [DOI] [PubMed] [Google Scholar]
- 43. Proctor MA, Epps CH. Post traumatic ossification of the Achilles tendon. J Natl Med Assoc 1976; 68(5): 368–390. [PMC free article] [PubMed] [Google Scholar]


