Abstract
Background:
Despite the increased survival of premature infants, many infants are discharged from the hospital while they still require care and follow-up. The present study aimed to determine the effect of empowerment program on maternal discharge preparation and infants' length of hospital stay.
Materials and Methods:
In this pretest-posttest clinical trial, 60 premature infants along with their mothers were selected from the neonatal intensive care unit (NICU) of a teaching hospital in Kermanshah in 2016 via convenience sampling and were allocated to experimental and control groups. Mothers in the control group performed routine care and those in experimental group, in addition to the routine care, performed an intervention program, training sessions including touching and massage, bathing, infection prevention, warning signs, and neonatal resuscitation. Data were collected by a maternal and neonatal demographic questionnaire and a discharge preparation checklist, performed twice (at admission and before discharge), by the researcher. The collected data were analyzed by independent and paired t-test.
Results:
The mean (standard deviation) of the total score of maternal discharge preparation in intervention group 44.65 (3.90) was significantly higher than that of the control group 33.00 (8.28) (t = -6.58, p <0.001). The mean length of neonatal hospitalization in the intervention group (14.79 days) was significantly shorter than that of the control group (20.43 days) (p = 0.020).
Conclusions:
The increasing maternal discharge readiness and reducing the length of neonatal hospital stay would decrease the medical costs and supply more beds for admission of other infants.
Keywords: Discharge planning, Iran, length of stay, premature infant
Introduction
Statistics show that 10% of infants are born premature,[1,2,3] need long hospitalization in neonatal intensive care unit (NICU) and face many problems.[4] With development in science and technology and increasing survival of infants in intensive care units (NICU), many infants are discharged from hospital while they need more care and accurate follow-up, thereby remaining vulnerable.[5] Transfer from hospital to home is a critical period for parents because they are responsible for all cares at home, and if they are not able to handle these responsibilities, complications will occur for the infants. Therefore, it is necessary to design appropriate programs and healthcare interventions before transferring the infant to home.[6] Since maternal care for premature infants affects the length of neonatal hospital stay, hospital infection, and neonatal rehospitalization, it seems necessary to design interventions to empower mothers in taking care of their premature infant.[7] A leading cause of neonatal mortality in the first year of birth is the prematurity involving complications, and many infants that survive will face disabilities, learning disorders, and audio and visual problems.[8,9] To prevent these complications, mothers are required to have sufficient knowledge during neonatal hospital stay in the ward.[10]
The discharge training plan, which has been accurately structured, is initiated at admission and after passing neonatal critical conditions, is designed until neonatal discharge and even after discharge and mother, as an active and principal member of this plan, is trained on how to safely transfer the infant to home.[11] On the other hand, limited number of hospital beds available to NICU and long neonatal hospital stay have restricted the possibility of admitting more infants.[12] Thus, the possibility of neonatal admission is provided by early discharge of inpatient infants.[13] One of the reasons for improper relationship of parents with their infants is delay in postpartum emotional attachment between the mother and newborn. Therefore, increasing the length of neonatal hospital stay in intensive care units, in addition to disturbing mother-infant interaction and nutrition, increases the possible risk of hospital infections and treatment costs.[14] However, the main concern is that short hospitalization and neonatal discharge before physiologic stabilization may increase the risk of neonatal complications [15] and possible rehospitalization [16] and may question the adequacy and quality of the presented cares and neonatal discharge readiness.[17]
The most important measures to be taken for nurses to reduce the maternal problems in NICU are implementation of maternal empowerment program and provision of favorable conditions for cooperation in neonatal care in new situations.[18] In fact, maternal empowerment in NICU is a family-oriented nursing intervention that takes into account the needs of both mothers and infants and tries to achieve favorable results and prevent unfavorable consequences.[19] Intensive care units for the newborn obviously need to be family-centered care to be able to eliminate the stress with positive impact on the relationship between mother and child.[20] The empowerment program caused a significant reduction in the length of hospital stay.[21] Hence, in a comprehensive discharge plan, safe transfer of infant from hospital to home is planned by maternal empowerment and early neonatal discharge from intensive care units.[10] The current study was an attempt to evaluate the effect of empowerment program on maternal discharge readiness and neonatal length of hospital stay.
Materials and Methods
This pretest-posttest clinical trial was registered in Iranian Clinical Site (IRCT 201604084613N19) in 2016 and carried out at NICU of a teaching hospital in Kermanshah, Iran. Based on the mean hospitalizations days in intervention and control groups in the study of Khajeh et al.[19] respectively, which were 23.27 and 19.23 days, we considered α = 0.05 as error level and β = 0.80 as the statistical power. The sample size was 25 infants for each group that we considered 30 for probable loss of patients during the study. The randomization was performed by using RAND List software.
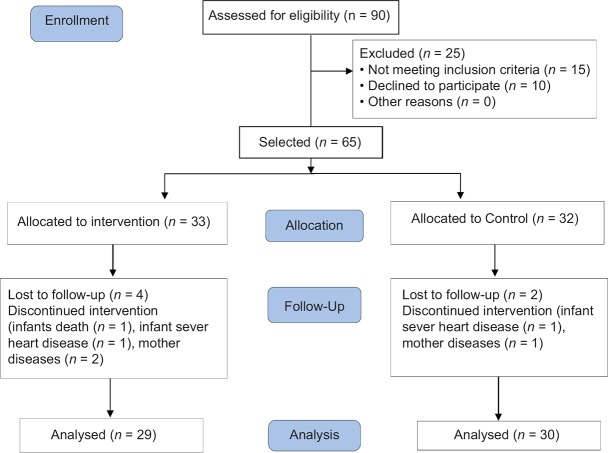
Despite the suitability of parallel random sampling, the participants were chosen from among the mothers of hospitalized neonates in intensive care unit by convenience sampling due to probable exchange of empowerment trainings between two groups. The inclusion criteria for mothers comprised of age ≥18 years, junior high school education and above, no history of former infants' hospitalization in NICU and absence of maternal preeclampsia. The inclusion criteria for infants consisted of the weight 1000–2500 g, gestational age 28–34 weeks, lack of congenital anomalies and major physical diseases and absence of neurological deficits. The exclusion criteria were neonatal death, neonatal dispatch to other centers for treatment, maternal withdrawal from participation in the study, and lack of mothers' participation in training sessions [Figure 1].
Figure 1.
Flow chart of participants in the steps of the study.
The research instruments were neonatal demographic questionnaire, which was completed by the researcher using medical files and, if required, by asking mothers, and 28-item discharge preparation checklist, including 12 items on physical or general health status of infants during discharge, and 16 items on the adequacy of trainings presented to mothers; scoring of the items was based upon 3-point Likert scale ranging from NO (1) Unfavorable (2) and Favorable (3). This scale was prepared by Dashti et al.[22] with content validity index (CVI) of 0.99 and interclass correlation coefficient (ICC) of 0.88. The reliability of this scale in the present study was calculated by Cronbach's alpha to be 0.95.
Due to probable exchange of empowerment trainings between two groups, the intervention and control groups were not selected simultaneously; they were chosen at separate times and after the discharge of the first group. Mothers in control group were taught usual cares (kangaroo mother care and breastfeeding) by the nurses of the ward. Mothers in intervention groups, in addition to usual cares, received an empowerment program, including frequency of hand washing with disinfectant, milk preparation and maintenance, sucking practice with pacifier or finger and then with mother breast, medication, sleeping, touching and massaging, bathing, changing, vaccination, developmental tasks, infection prevention, warning signs and resuscitation, teaching mothers in the department was usually done in group and on the bedside of the infant during the hospitalization period and according to the clinical condition of the newborn and according to the order of the physician in consecutive days and gradually until discharge presented by the researcher. In this program, in addition to face-to-face training, mothers were provided with educational materials in a written manual and a video CD.
Since the intervention was of an educational type, it was not possible to blind the researcher; therefore, to reduce the bias, the pretest and posttest questionnaires were completed 1–2 days after the infant's admission and 1–2 days before the infant's discharge from hospital, respectively by blinded co-researcher in two groups. Data were analyzed by The Statistical Package for the Social Sciences (SPSS software version 20; SPSS Inc., Chicago, IL, USA) using descriptive statistics [mean (standard deviation = SD)] and inferential statistics (independent t-test, paired t-test, Chi-square, and the log-rank test). The mean scores of maternal discharge preparation between intervention and control groups before and after intervention were compared by independent and paired t-test, and demographic characteristics of the two groups were compared by Chi-square. Also, 95% confidence interval was considered for all above tests. In statistics, the log-rank test is a hypothesis test to compare the survival distributions of two samples. It is a nonparametric test and appropriate to use when the data are right skewed and censored (technically, the censoring must be noninformative).[23]
Ethical considerations
This article was taken from a research project (no: 5/d/58066- August 29, 2016) approved by the ethics committee of Tabriz University of Medical Sciences. At the beginning of study, informed consent forms for participation in the study was completed by the mothers.
Results
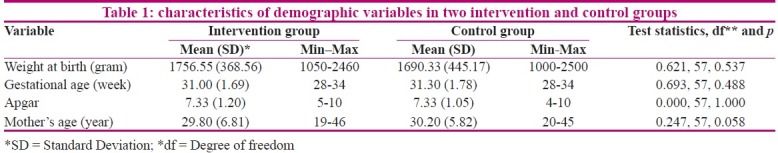
In this study, most of the infants were male (69%) in intervention group and female (53.3%) in control group. In both groups, most of the infants had a gestational age of 30 weeks at birth and Apgar score of 6-8. Most of the mothers in both groups had secondary education and were homemaker. Of them, 62.2% in intervention group and 96.7% in control group had cesarean delivery and did not have another living children. The results of Chi-square showed a significant difference between groups only in delivery method (p = 0.001), anddistribution of other variables was similar in both groups [Table 1].
Table 1.
characteristics of demographic variables in two intervention and control groups
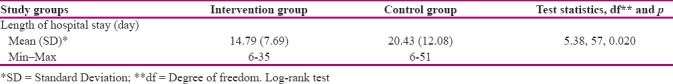
Maternal discharge preparation in intervention group was significantly higher than that of control group (t = -6.58, df = 57, p <0.001). Therefore, maternal discharge preparation in terms of abilities and trainings presented to mothers was significantly higher in intervention group than in control group (t = -7.29, df = 57, p <0.001). Moreover, the mean maternal discharge preparation with regard to physical or general health of the infant was significantly higher in intervention group than in control group (t = -3.48, p <0.001) [Table 2]. The log-rank test showed neonatal length of hospital stay was significantly shorter in intervention group than in control group (p = 0.020) [Table 3].
Table 2.
Comparison of mean score changes of maternal preparation for neonatal discharge in two intervention and control groups
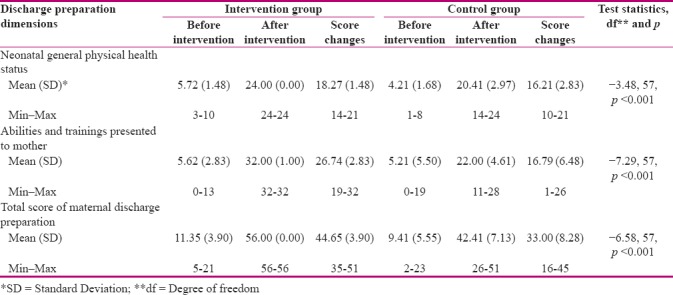
Table 3.
Comparison of mean length of hospitalization in intervention and control groups
Discussion
The results of present study showed a low level of maternal discharge preparation for premature infant care at admission, and maternal readiness was gradually increased as mothers attended their infants' bedside, creating a remarkable difference between maternal and neonatal readiness before discharge and at admission, and making mothers more prepared to take care of their preterm infants owing to their active and direct clinical participation in empowerment program. In line with the present study, Saki et al. (2012) carried out a study to investigate the appropriateness of conditions and rehospitalization rate through family-oriented care. Making judgment on rehospitalization rate, which was 1% after discharge over 1 month and 9.5% over 1 year, they reported the usefulness of family-oriented care program in increasing parental readiness and early discharge of preterm infant.[13] Further, Dashti et al. (2014) evaluated the correlation of discharge preparation and rehospitalization among hospitalized infants and infants without rehospitalization. They reported a decreased possibility of rehospitalization with a rise in neonatal and parental discharge preparation.[22]
In the current study, by implementing maternal empowerment program and maternal discharge preparation, the length of neonatal hospital stay was reduced by almost 6 days. In line with the present research, Armanian et al. (2001) conducted a study to determine rehospitalization rate and length of hospital stay among 495 preterm infants with a weight less than 2500 g. Their results revealed that given the frequent requests for admission of new premature infants as well as very low possibility of admission, infants who were able to maintain their body temperature in room conditions, had oral feeding and did not have apnea and bradycardia. Regardless of their gestational age and body weight, they were discharged earlier.[24] In another study, Dashti et al. (2013) assessed the association of neonatal factors with rehospitalization. Unlike the results of this research about early neonatal discharge, the findings showed 39.6% of preterm infants were hospitalized again 1 month after discharge from hospital, and most of them were returned to hospital in less than 10 days.[25]
Similar to the findings of present study, Gonya et al. (2014), performed an experimental study on the effect of parental empowerment on neonatal outcomes, including length of hospital stay and rehospitalization. Their results indicated that active involvement of parents in their infants' care before discharge resulted in a shorter length of hospital stay and rehospitalization.[26] Furthermore, Melnyk et al. (2006) conducted a quasi-experimental study to examine parental empowerment and promotion of parents' beliefs to promote neonatal outcomes. The findings showed the length of hospitalization was 3.8 days shorter in intervention group than in control group. Also, family-oriented trainings and parental empowerment promoted the parental mental health, reinforced parent-child interaction, and reduced the length of hospital stay.[27] In addition, Ingram et al. (2015) carried out a quasi-experimental study to evaluate the impact of family-oriented training. Unlike the present study, a significant difference was not found for the length of hospital stay. The findings showed the frequency of rehospitalization was reduced with an increase in maternal self-efficacy score, which was followed by reduction of treatment costs.[28] Data collection and sampling methods were limitation of the present study. Due to possible exchange of information between the mothers in both groups, it was not possible to perform random and parallel sampling for both groups; hence, nonrandom convenience sampling was carried out, which might have affected the results. Therefore, by providing favorable grounds in clinical environments, it seems necessary for the concerned authorities to implement this strategy as an effective intervention.
Conclusion
Implementing maternal empowerment program for premature infants, ensuring neonatal and maternal discharge readiness by improving the presented cares, planning for discharge, training mothers during hospitalization, and providing family support after discharge are the most important nursing interventions to prevent postdischarge complications and early neonatal discharge from hospital and to reduce the length of hospital stay, which consequently decrease the treatment costs and provide other preterm infants with empty beds. Moreover, considering the severe shortage of nursing staff, active maternal participation in neonatal care, as a significant element of family-oriented care, makes a great contribution to neonatal treatment and care.
Financial support and sponsorship
Tabriz University of Medical Sciences.
Conflicts of interest
Nothing to declare.
Acknowledgements
This article was taken from a research project (no: 5/d/58066) Tabriz University of Medical Sciences. The authors appreciate all mothers who participated in this research as well as authorities and nursing staff of intensive care unit of the teaching hospital for their cooperation in this study. The authors also thank the social security organization of Kermanshah and personnel of Hazrat-e-Masoumeh hospital who provided the conditions for the researcher to collect the data.
References
- 1.Akbarbeglou M, L Valizadeh, ELAHI MALIHEH ASAD. “Mothers and nurses viewpoint about importance and rate of nursing supports for parents with hospitalized premature newborn in natal intensive care unit”. Journal of Critical Care Nursing. 2009;2:71–4. [In Persian]. [Google Scholar]
- 2.Howson, Christopher P, et al. Born too soon: preterm birth matters. Reproductive Health. 2013;10(Suppl 1):S1. doi: 10.1186/1742-4755-10-S1-S1. https://doi.org/10.1186/1742-4755-10-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Golestan M, Akhavan Karbasi S, Fallah R. Prevalence and risk factors for low birth weight in Yazd, Iran. Singapore Med J. 2011;52:730–3. [PubMed] [Google Scholar]
- 4.Altman M, Vanpée M, Cnattingius S, Norman M. Moderately preterm infants and determinants of length of hospital stay. Arch Dis Child Fetal Neonatal Ed. 2009;94(6):F414–F8. doi: 10.1136/adc.2008.153668. [DOI] [PubMed] [Google Scholar]
- 5.Aliabadi T, Bastani F, Haghani H. Effect of mothers' participation in preterm infants' care in NICU on readmission rates. Journal of hayat. 2011;17:71–7. [In Persian]. [Google Scholar]
- 6.Boykova M, Kenner C. Transition from hospital to home for parents of preterm infants. J Perinat Neonatal Nurs. 2012;26:81–7. doi: 10.1097/JPN.0b013e318243e948. [DOI] [PubMed] [Google Scholar]
- 7.Bhutta ZA, Khan I, Salat S, Raza F, Ara H. Reducing length of stay in hospital for very low birthweight infants by involving mothers in a stepdown unit: An experience from Karachi (Pakistan) BMJ. 2004;329:1151–5. doi: 10.1136/bmj.329.7475.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo J, et al. Incidencia mundial de parto prematuro: Revisión sistemática de la morbilidad y mortalidad maternas. Boletín de la Organización Mundial de la Salud. 2010;88:1–80. [Google Scholar]
- 9.Hollier LM. Preventing preterm birth: What works, what doesn't. Obstet Gynecol Surv. 2005;60:124–31. doi: 10.1097/01.ogx.0000153640.44509.65. [DOI] [PubMed] [Google Scholar]
- 10.De Rouck S, Leys M. Information needs of parents of children admitted to a neonatal intensive care unit: A review of the literature (1990–2008) Patient Educ Couns. 2009;76:159–73. doi: 10.1016/j.pec.2009.01.014. [DOI] [PubMed] [Google Scholar]
- 11.Verklan MT, Walden M. Core Curriculum for Neonatal Intensive Care Nursing-E-Book. Elsevier Health Sciences; 2014. [Google Scholar]
- 12.Ji H, Abushomar H, Chen X, Qian C, Gerson D. All-cause readmission to acute care for cancer patients. Healthc Q. 2012;15:14–6. doi: 10.12927/hcq.2013.23044. [DOI] [PubMed] [Google Scholar]
- 13.Seki K, Iwasaki S, An H, Horiguchi H, Mori M, Nishimaki S, et al. Early discharge from a neonatal intensive care unit and rates of readmission. Pediatr Int. 2011;53:7–12. doi: 10.1111/j.1442-200X.2010.03179.x. [DOI] [PubMed] [Google Scholar]
- 14.Tooten A, Hoffenkamp HN, Hall RA, Winkel FW, Eliëns M, Vingerhoets AJ, et al. The effectiveness of video interaction guidance in parents of premature infants: A multicenter randomised controlled trial. BMC Pediatr. 2012;12:76. doi: 10.1186/1471-2431-12-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122(5):1119–26. doi: 10.1542/peds.2008-2174. [DOI] [PubMed] [Google Scholar]
- 16.Canadian Institute for Health Information (CIHI) All-cause readmission to acute care and return to the emergency department. Ottawa: CIHI; 2012. [Last accessed on 2016 Jul 15]. Available from: https://secure.cihi.ca/free_products/Readmission_to_acutecare_en.pdf . [Google Scholar]
- 17.Salas R, Sanhueza L, Maggi L. Factores de riesgo y seguimiento clínico en prematuros menores de 1 000 gramos. Revista chilena de pediatría. 2006;77(6):577–88. [Google Scholar]
- 18.Lindberg B, Ohrling K. Experiences of having a prematurely born infant from the perspective of mothers in northern Sweden. Int J Circumpolar Health. 2008;67:461–71. doi: 10.3402/ijch.v67i5.18353. [DOI] [PubMed] [Google Scholar]
- 19.Khajeh M, Karimi R, Sadat Hosseini AS. The effect of parents empowerment program on their beliefs about parental role, behaviors and characteristics of their premature infants in nicu. Journal of Urmia Nursing And Midwifery Faculty. 2013;11:419–27. [In Persian] [Google Scholar]
- 20.Sikorova L, Kucova J. The needs of mothers to newborns hospitalised in intensive care units. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2012;156:330–6. doi: 10.5507/bp.2011.046. [DOI] [PubMed] [Google Scholar]
- 21.Beheshtipoor N, Shaker Z, Edraki M, Razavi M, Zare N. The Effect of family-based empowerment program on the weight and length of hospital stay of preterm infants in the neonatal intensive care unit. Galen Medical Journal. 2013;2:114–9. [Google Scholar]
- 22.Dashti E, Rassouli M, Khanali Mojen L, Puorhoseingholi A, Shirinabady Farahani A. Correlation between discharge preparation and rehospitalization of premature newborns. Journal of Health Promotion Managemen. 2014;3:37–45. [In Persian]. [Google Scholar]
- 23.Kleinbaum DG KM. Survival analysis. Springer; 2010. [Google Scholar]
- 24.Armanian AM, Mohammadzadeh M, Soleimani R, Salehimehr N, Hasanzadeh A. The Duration of Hospitalization and Readmission Rate of Low Birth Weight Infants in a Tertiary Referral Hospital in Isfahan, Iran. Iranian Journal of Neonatology IJN. 2015;6:17–21. [Google Scholar]
- 25.Dashti E, Rassouli M, Khanali Mojen L, Puorhoseingholi A, Shirinabady Farahani A, Sarvi F. Neonatal factors associated with preterm infants' readmissions to the neonatal intensive care units. Journal of hayat. 2015;21(3):29–40. [In Persian]. [Google Scholar]
- 26.Gonya J, Martin E, McClead R, Nelin L, Shepherd E. Empowerment programme for parents of extremely premature infants significantly reduced length of stay and readmission rates. Acta Paediatrica. 2014;103:727–31. doi: 10.1111/apa.12669. [DOI] [PubMed] [Google Scholar]
- 27.Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants' length of stay and improving parents' mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: A randomized, controlled trial. Pediatrics. 2006;118(5):e1414–27. doi: 10.1542/peds.2005-2580. [DOI] [PubMed] [Google Scholar]
- 28.Ingram JC, Powell JE, Blair PS, Pontin D, Redshaw M, Manns S, et al. Does family-centred neonatal discharge planning reduce healthcare usage? A before and after study in South West England. BMJ Open. 2016;6:e010752. doi: 10.1136/bmjopen-2015-010752. [DOI] [PMC free article] [PubMed] [Google Scholar]