Abstract
Background:
Traumatic brain injury (TBI) is a main health problem among communities. There exists a variety of effective factors on the outcome of patients with TBI. We describe the demographic, clinical, and injury related variables of the patients with severe TBI, and determine the predictors of outcome.
Materials and Methods:
We did this cross-sectional study on all 267 adult patients with severe TBI admitted to three trauma centers of Isfahan University of Medical Sciences (IUMS) from March 20, 2014 to March 19, 2015. Data were extracted from patients' profiles. We considered the patients' outcome as discharged and died. We analyzed the collected data using descriptive (frequency, mean, and standard deviation) and analytical (independent t-test, Mann–Whitney U-test, Kruskal–Wallis test and logistic regression) statistics in Statistical Package for the Social Sciences (SPSS) 16.0. We considered p < 0.05 as the significance level.
Results:
The mean (SD) age of patients was 43.86 (18.40) years. The majority of the population was men (87.27%). Road traffic accidents (RTAs) were the most common mechanism of trauma (79.40%). The mean (SD) of Glasgow coma scale (GCS) was 6.03 (3.11). In 50.19% of the patients, the pupillary reflex was absent. One hundred and twenty-four patients (46.44%) died before discharge. We found age, gender, GCS, pupillary reflex, hypernatremia, and increased intracranial pressure (IICP) as the predictors of death in severe TBI.
Conclusions:
In this study, the mortality rate of patients with severe TBI was high. In addition, some factors were determined as the significant predictors of outcome. The findings can assist in planning to enhance the quality of care and reduce the mortality rate in the patients with severe TBI.
Keywords: Head trauma, Iran, patients, traumatic brain injury
Introduction
Traumatic brain injury (TBI) is a common cause of mortality and disability among communities affecting people of all age groups.[1] The clinical severity of TBI can be categorized into mild injury with the score of 13–15, moderate injury with the score of 9–12, and severe injury with the score of 3–8 based on Glasgow coma scale (GCS) as the most extensive used classification of the severity of TBI.[2] In general, 5-15% of TBI are severe. Despite the fact that severe TBI involves little percentage of overall cases of TBI, it injury is one of the most important health problems worldwide due to the high global burden on societies.[3]
Most mortality and burden following severe TBI occur in non-developed/developing countries.[4] In United States, the annual mortality rate related to severe TBI per 100000 population is 18 persons, and in Europe is 15 persons. However, in Asia this rate per 100000 population is within the range of 20 persons in India to 38 persons in Taiwan.[5] In Iran, trauma is the second cause of death and the most important reason of hospitalization.[6] According to Iranian forensic Medicine Organization, Isfahan province is in the fourth place in mortality rate related to road traffic accidents (RTAs) in 2016 (24697 died and injured were reported in the year which is 7.41% of the whole). Head trauma is the cause of 51.7% of mortalities. In addition, in a study by Zand and Rafiei, TBI following accidents have been stated as the most common cause of death in intensive care units (ICUs) in Iran.[7]
A latest report of the World Health Organization (WHO) has been emphasized on doing more research regarding the epidemiological pattern of accidents in order to detect the expansions of the problem and also to recognize at risk individuals in non-developed and developing countries.[8] Currently, many researchers are interested in predicting the outcome following severe TBI; since to determine the predictors of outcome assists health care providers to make better decisions regarding the clinical situation of the patients.[9] Previous studies have identified some effective factors on the outcome of patients with TBI, such as age, GCS, primary hypoxia and hypotension, pupillary reflex, the cause of injury, secondary injuries, biochemical parameters, and computed tomography (CT) scan findings.[1,10,11,12,13] However, the epidemiologic patterns of these injuries and their outcomes change in different communities as they are dependent on geographic specializations, local health-service features and the sociocultural differences.[9]
Due to lack of a comprehensive trauma registry system in Iran, sufficient data on the epidemiological patterns of trauma and the outcomes are not available.[13] The purpose of this study is to describe the demographic, clinical, and injury-related variables and to determine the predictors of outcome in adult patients with severe TBI in Isfahan, Iran. We compare our findings to the existing literature in the field, and specify the agreements and differences. We also discuss the importance of this health problem in our region, and assess the local parameters that intensify this issue.
Materials and Methods
We conducted this cross-sectional, retrospective study during one year from March 20, 2014 to March 19, 2015 in three trauma centers of Isfahan University of Medical Sciences (IUMS), Isfahan, Iran. Data were obtained from the patients' profiles (secondary source of data). There were 1,204 profiles of adult patients with TBI, admitted to trauma centers of IUMS during the above-mentioned period. All 267 profiles of patients aged 18 years or older with a GCS of 8 or less (severe TBI) during the first 24 hours after admission [2] were included in our study. Exclusion criteria were lack of access to patient's information and incomplete information recorded in the medical profiles. We collected the data after getting permission from the IUMS and the hospitals' managers. From the patients' profiles, we acquired the data on some demographic and injury related characteristics named as age, gender, cause of injury, date and time of incident, and time of arrival to Emergency Department (ED). Moreover, for the clinical variables, we collected the data on the level of consciousness on admission measured by the GCS, pupillary reflex, hospitalization duration, the duration of ventilator dependent, secondary injuries, the presence of concomitant injuries, and the outcome (discharged and died). The brain CT scan results were extracted in terms of cerebral edema, epidural/subdural/intracerebral hematoma, and intraventricular/subarachnoid hemorrhage. In addition, we assessed the laboratory parameters measured at the time of admission and during the hospitalization. The measured parameters were hemoglobin concentration, platelet count, international normalized ratio (INR), sodium level, and blood sugar level. Data were recorded in a data collection form with a special code for each patient. The instrument is a researcher-made form, which includes demographics, clinical, and injury related characteristics. Some neurosurgery specialists and faculty members of nursing confirmed the face and content validity of the form.
We analyzed the collected data using the Statistical Package for the Social Sciences (SPSS) (version 16, SPSS Inc, Chicago, IL, USA). We demonstrated the continuous variables in terms of mean and standard deviation, and the categorical variables in terms of frequency and percentage. Also, we used independent t-test and, Mann–Whitney U or Kruskal–Wallis tests to compare the continuous and categorical variables, respectively, in dead and discharged patients. Logistic regression analysis was used to determine the predictor variables associated with the outcome. We tested the following variables in logistic regression analysis: age (as a continuous variable), gender, GCS on admission (as a continuous variable), presence of cerebral hematoma, presence of cerebral edema, mechanism of injury, time from accident to ED (as a continuous variable), pupillary reflex on admission, presence of concomitant injuries, mechanical ventilation, and presence of secondary injuries (Increased Intracranial Pressure (IICP), hypoxia, hypernatremia, hyperglycemia, hypotension, seizure, coagulopathy). We also calculated odds ratio and 95% confidence intervals (95% CI). We considered a p < 0.05 (two-tailed) as statistically significant.
Ethical considerations
Ethics committee of IUMS approved this study. It should be noted that all the information gathered from the patients' profiles was considered confidential.
Results
In this study, 267 patients (out of 1,204) with severe TBI were assessed (87.27% were male with the mean (SD) age 43.86 (18.40) years). The most common cause of injury was RTAs (79.40%). The majority of injured patients (52.06%) were between 18–40 years old. Table 1 shows the demographic, clinical, and injury-related variables of patients.
Table 1.
Demographic, clinical, and injury-related characteristics of samples
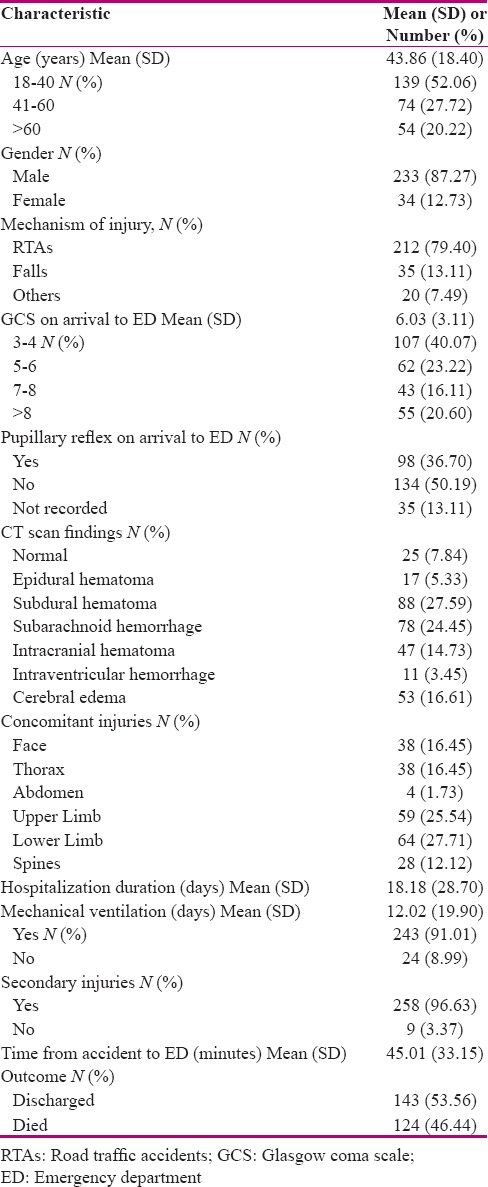
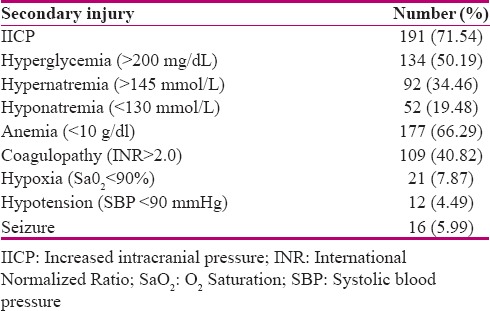
The mean time from accident to ED was 45.01 (33.15) minutes (median = 36). The mean GCS of the patients at the time of admission to ED was 6.03 (3.11). The pupillary reflex at the time of admission was absent in 134 cases (50.19%). The mean duration of the hospitalization was 18.18 (28.70) days. A number of 243 patients (91.01%) were under mechanical ventilation during hospitalization (12.02 (19.90) days). The most common findings of the initial brain CT scans were subdural hematoma (27.59%). Up to 201 patients (75.28%) had concomitant injuries. A total of 258 patients (96.63%) experienced at least one secondary injury [Table 2].
Table 2.
Frequency of secondary injuries in patients with severe TBI
Finally, 124 patients (46.44%) died in the hospitals. Motorcycles were the cause of head injuries in 30.60% of deaths.
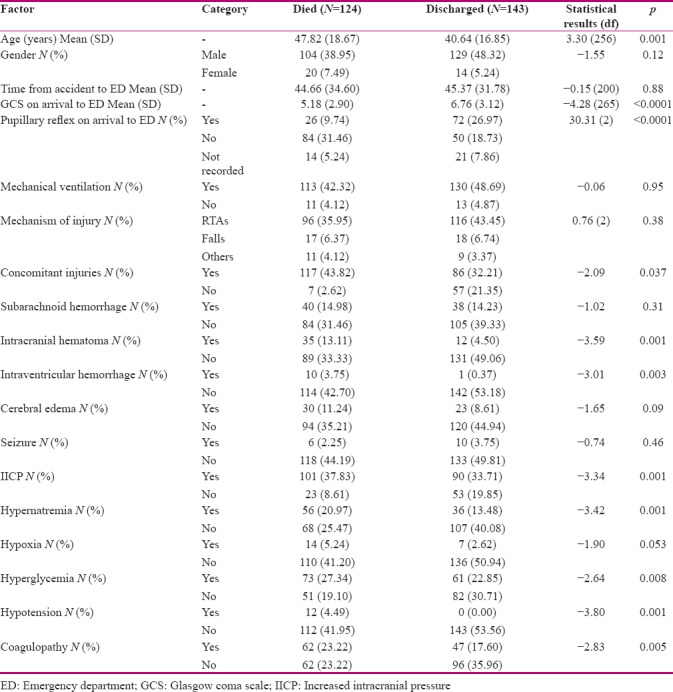
The mean age (47.82 (18.67) years vs. 40.64 (16.85) years), lack of pupillary reflex (31.46% vs. 18.73%), concomitant injuries (43.82% vs. 32.21%), intracranial hematoma (13.11% vs. 4.50%), intraventricular hemorrhage (3.75% vs. 0.37%), IICP (37.83% vs. 33.71%), hypernatremia (20.97% vs. 13.48%), hyperglycemia (27.34% vs. 22.85%), hypotension (4.49% vs. 0.00%), and coagulopathy (23.22% vs. 17.60%), all had higher rates in dead patients. Also, the mean of GCS on arrival to ED (5.18 (2.90) vs. 6.76 (3.12)) in dead patients were less than discharged patients [Table 3].
Table 3.
Factors associated with outcome in samples (univariate analysis)
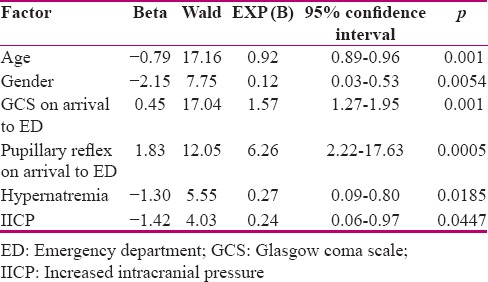
According to the logistic regression analysis, six variables (out of 17) were selected as significant independent predictors of death with regard to the significant level of 5%, and the values of B and Beta. Age (Wald = 17.16, p<0.001), GCS on arrival to ED (Wald = 17.04, p<0.001), and pupillary reflex on arrival to ED (Wald = 12.05, p = 0.0005) were the stronger predictors in the presence of other variables. Table 4 shows the predictors of death according to logistic regression analysis.
Table 4.
Predictor factors of outcome in samples
Discussion
We found that younger men have higher rates of severe TBI due to ARTs. This can be due to varieties in their lifestyle, work, and activities; e.g., their high-risk jobs and more usage of motor vehicles.[14] This result is in accordance with several previous studies.[2,10,11,12] However, in a variety of studies a shift toward a greater incidence of injury in older people has been observed, particularly in developed countries.[14] Also, in two systematic review studies on the epidemiologic pattern of TBI in Europe, an evident shift from RTAs to falls during the time is observed as the cause of TBI, whereas in the studies that were focusing solely on severe TBI, RTAs were still kept as the most common cause of TBI.[15,16] This fact is in accordance with our results. In Iran as a developing country, the average age is less compared to the developed countries. In effect, it can lead into a difference in the mean age of patients with TBI. Also, the higher frequency of severe TBI related to RTAs especially motorcycles in Isfahan (79.40%) than some other studies in New Zealand (71%),[17] India (48.91%),[11] Brazil (60.3%),[18] and Tanzania (70.8%)[19] can be due to the fact that in Isfahan (1) there is much traffic in the external highways as it is connecting many cities, (2) the majority of motor vehicles are not safe,[20] and (3) many people are not following traffic rules as well as in Iran. Despite the fact that wearing helmets is mandatory, the executers are not harsh to this matter, so that in a study by Modaghegh et al. only 7.4% of the motorcyclists had used helmets.[21] Therefore, the absence of adequate protection and a quick reversal of the motorcycles at the time of accident put the riders at a high risk of head trauma. It is worth mentioning that compared to some other studies conducted in Iran in the last 10-12 years, this study shows no significant change in the frequency of TBI caused by RTAs.[22,23] This fact is calling for more attention in this subject.
The in-hospital mortality rate of patients with severe TBI was 46.44%. In Iran, the mortality rate was reported 42.3% in Arak (in central Iran) for severe TBI, and 60.9% in Kashan (in central Iran) for TBI.[22,23] In the meta-analysis study of Georgoff et al. the mortality rate of severe TBI in developing countries was reported from 29.1% to 62.3%.[24] Difference in some factors such as habits, lifestyle, and health services in different societies are known as the reasons for the variety in mortality prevalence.[14] It should be noted that in this study, only patients with severe TBI were studied, while in some other studies such as study of Kasmaei et al. patients with any severity of TBI formed the samples, and it could result in lower mortality rates compared to our study.[13] Also, the findings of our study show a high rate of secondary injuries in the samples, which can affect the mortality rate. In Isfahan trauma centers, the healthcare team tried to avoid secondary brain injuries in patients with severe TBI. However, the lack of some facilities such as the IICP monitoring device can cause troubles in managing the injuries. Moreover, the existence of concomitant injuries in most cases can cause the secondary brain injuries. Nonetheless, identifying the causes of high rates of secondary injuries in this region needs further investigations.
The results of this study showed that age, gender, GCS on admission, hypernatremia, IICP, and papillary reflex on admission are the predictors of mortality. Researchers reported different associated factors with death in their studies. In several studies age, GCS, and papillary reflex were reported more frequently as the predictor factors in relation to mortality and morbidity of TBI [10,11,19,25,26] that are in accordance with the results of our study. Also, in a review study by Kulesza et al. age, GCS, and pupil response were recognized as the most important prognostic factors of outcome.[27] In the study by Perel, the level of consciousness had a linear relationship with mortality.[4] Saini et al. confirmed that the death of patients was associated with the ages more than 40, the level of consciousness, abnormal pupillary reaction, and hypoxia.[11] Kasmaei et al. described ages more than 60, trauma mechanism (motorcycle and falling), existence of intracranial and subdural hemorrhage, and GCS < 9 as independent predictors of adverse outcome.[13] Also, Iba et al. demonstrated that age, papillary reflex, ICP, and subarachnoid haemorrhage were related to the unfavourable outcome.[26] While Fabbri et al. did not recognize any relation between age and outcome.[25] In the study by Leong et al. the mortality rate increased significantly in patients with serious extracranial injuries.[28] However, Baum et al. stated that serious extracranial injuries were not associated with the outcome.[12] These differences can be due to the sample sizes, study population, variables under study and the method. Hence, further investigations are needed in this topic. For instance, in this study only 16 patients had a seizure, and since this sample size is too small further information is needed to confirm the effect of seizure on the outcome.
In order to specify a limitation for this study, we point out that it is a retrospective study. A study based on the patients' profiles can lead to the loss of information due to non-registered information or inaccuracy in the registration. However, as in this study, most of the information recorded in patients' profiles were complete, and all patients with severe TBI were admitted only in the aforementioned centers in Isfahan, the acquired results should be reliable. In this study, we did not analyze the probable complications that can occur during hospitalization; if the death occurred due to the fatal complications and were not directly caused by TBI, this could have reduced the generalizability of the results with regard to the outcome of mortality in patients with severe TBI. Despite the limitations, this study provides some worthwhile information to establish effective safety principles according to the context.
Conclusion
Assessing the prognosis after TBI is important and difficult. Several different factors are associated with outcome of TBI that can assist the healthcare team.[9] The results of this study showed that severe TBI mostly happen in younger males and motorcycle riders. Also, the frequency of secondary injuries and in-hospital mortality rate are high in our region. Based on the findings, the outcome of severe TBI can be affected by various factors. Therefore, it is crucial to design and use local clinical guidelines for improving the trauma outcome. Moreover, having a comprehensive trauma registry system in Iran will make the researchers and authorities able to identify the effective factors on trauma. This would facilitate fast and appropriate proceedings to prevent injuries and disabilities/mortalities following them.
Financial support and sponsorship
Isfahan University of Medical Sciences.
Conflicts of interest
Nothing to declare.
Acknowledgement
This study was derived from a doctoral thesis of Marzieh Ziaeirad with project number 394447. The authors acknowledge the funding of the Vice Chancellery for Research at MUI. The authors also appreciate the staff of MUI trauma centers who kindly helped during this research.
References
- 1.Imen RB, Olfa C, Kamilia C, Meriam B, Hichem K, Adel C, et al. Factors predicting early outcome in patients admitted at emergency department with severe head trauma. J Acute Dis. 2015;4:68–72. [Google Scholar]
- 2.Atci IB, Yilmaz H, Kara D, Yilmaz N, Bitlisli H, Ayden O, et al. Retrospective analysis of 3524 head trauma patients admitted to the emergency department as epidemiological approach to head traumas in our region. Acta Med Mediterranea. 2015;31:825–8. [Google Scholar]
- 3.Haller CS, Walder B. Severe neurotrauma in Switzerland: Have short-term outcomes improved? Swiss Med Wkly. 2015;145:w14177. doi: 10.4414/smw.2015.14177. [DOI] [PubMed] [Google Scholar]
- 4.Collaborators MC. Perel P, Arango M, Clayton T, Edwards P, Komolafe E, et al. Predicting outcome after traumatic brain injury: Practical prognostic models based on large cohort of international patients. BMJ. 2008;336:425–9. doi: 10.1136/bmj.39461.643438.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Damkliang J, Considine J, Kent B. Thai emergency nurses management of patients with severe traumatic brain injury: Comparison of knowledge and clinical management with best available evidence. Australas Emerg Nurs J. 2013;16:127–35. doi: 10.1016/j.aenj.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 6.Hejini ES, Hadavi M. Assessment of epidemiology of traumatic brain injuries and its consequences in Rafsanjan: A descriptive study. Community Health J. 2015;9:37–46. [Google Scholar]
- 7.Zand S, Rafiei M. Causes and duration of hospitalization and mortality rate in intensive care units in central province. J Crit Care Nurs. 2010;3:7–8. [Google Scholar]
- 8.Hijar M, Perez-Nunez R, Inclan-Valadez C, Silveira-Rodrigues EM. Road safety legislation in the Americas. Rev Panam Salud Publica. 2012;32:70–6. doi: 10.1590/s1020-49892012000700011. [DOI] [PubMed] [Google Scholar]
- 9.Whyte J, Gosseries O, Chervoneva I, DiPasquale M, Giacino J, Kalmar K, et al. Predictors of short-term outcome in brain-injured patients with disorders of consciousness. Prog Brain Res. 2009;177:63–72. doi: 10.1016/S0079-6123(09)17706-3. [DOI] [PubMed] [Google Scholar]
- 10.Grigorakos L, Alexopoulou A, Tzortzopoulou K, Stratouli S, Chroni D, Papadaki E, et al. Predictors of outcome in patients with severe traumatic brain injury. J Neurosci Clin Res. 2016;1:1. [Google Scholar]
- 11.Saini NS, Rampal V, Dewan Y, Grewal SS. Factors predicting outcome in patients with severe head injury: Multivariate analysis. Indian J Neurotrauma. 2012;9:45–8. [Google Scholar]
- 12.Baum J, Entezami P, Shah K, Medhkour A. Predictors of outcomes in traumatic brain injury. World Neurosurg. 2016;90:525–9. doi: 10.1016/j.wneu.2015.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Kasmaei VM, Asadi P, Zohrevandi B, Raouf MT. An epidemiologic study of traumatic brain injuries in emergency department. Emerg (Tehran) 2015;3:141–5. [PMC free article] [PubMed] [Google Scholar]
- 14.Roozenbeek B, Maas AI, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol. 2013;9:231–6. doi: 10.1038/nrneurol.2013.22. [DOI] [PubMed] [Google Scholar]
- 15.Brazinova A, Rehorcikova V, Taylor MS, Buckova V, Majdan M, Psota M, et al. Epidemiology of traumatic brain injury in Europe: A living systematic review. J Neurotrauma. 2016 doi: 10.1089/neu.2015.4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peeters W, van den Brande R, Polinder S, Brazinova A, Steyerberg E, Lingsma H, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir. 2015;157:1683–96. doi: 10.1007/s00701-015-2512-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guerrier G, Morisse E, Barguil Y, Gervolino S, Lhote E. Severe traumatic brain injuries from motor vehicle-related events in New Caledonia: Epidemiology, outcome and public health consequences. Aust N Z J Public Health. 2015;39:188–91. doi: 10.1111/1753-6405.12362. [DOI] [PubMed] [Google Scholar]
- 18.Settervall CH, Sousa RM, Silva SC. In-hospital mortality and the Glasgow Coma Scale in the first 72 hours after traumatic brain injury. Rev Lat Am Enfermagem. 2011;19:1337–43. doi: 10.1590/s0104-11692011000600009. [DOI] [PubMed] [Google Scholar]
- 19.Chalya PL, Gilyoma JM, Dass RM, Mchembe MD, Matasha M, Mabula JB, et al. Trauma admissions to the intensive care unit at a reference hospital in Northwestern Tanzania. Scand J Trauma Resusc Emerg Med. 2011;19:1–7. doi: 10.1186/1757-7241-19-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haji Maghsoudi M, Akhlaghi SM, Nikouyeh M, Dehghani MH, Ahmadi SV, Hosseini SM. The role of safety equipment in reduction of head and face injuries in motorcycle and car accidents. J Safety Promot Injury Prev. 2016;4:33–8. [Google Scholar]
- 21.Modaghegh MHS, Saremi E, Mohamadian M, Jafarzadeh R. Characteristics of trauma in North East Iran and the prevention strategies. Arch Iran Med. 2013;16:576–9. [PubMed] [Google Scholar]
- 22.Ebrahimi FH. The outcome of patients hospitalized with severe head injury in Vali-asr hospital according to Glasgow Coma Scale in 2005-06. Arak Med Univ J. 2010;12:1–9. [Google Scholar]
- 23.Fazel M, Fakharian E, Tabesh H, Forghani Z, Yegane Moghadam A, Musavi G. Frequency and ethiology of traumatic brain injuries in Kashan hospitals. Feyz J Kashan Univ Med Sci. 2007;12:21–6. [Google Scholar]
- 24.Georgoff P, Meghan S, Mirza K, Stein SC. Geographic variation in outcomes from severe traumatic brain injury. World Neurosurg. 2010;74:331–45. doi: 10.1016/j.wneu.2010.03.025. [DOI] [PubMed] [Google Scholar]
- 25.Fabbri A, Servadei F, Marchesini G, Stein S, Vandelli A. Early predictors of unfavorable outcome in subjects with moderate head injury in the emergency department. J Neurol Neurosurg Psychiatry. 2008;79:567–73. doi: 10.1136/jnnp.2007.120162. [DOI] [PubMed] [Google Scholar]
- 26.Iba J, Tasaki O, Hirao T, Mohri T, Yoshiya K, Hayakawa K, et al. Outcome prediction model for severe traumatic brain injury. Acute Med Surg. 2014;1:31–6. doi: 10.1002/ams2.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kulesza B, Nogalski A, Kulesza T, Prystupa A. Prognostic factors in traumatic brain injury and their association with outcome. J Pre-Clinical Clin Res. 2015;9:163–6. [Google Scholar]
- 28.Leong BK, Mazlan M, Abd Rahim RB, Ganesan D. Concomitant injuries and its influence on functional outcome after traumatic brain injury. Disability Rehabil. 2013;35:1546–51. doi: 10.3109/09638288.2012.748832. [DOI] [PubMed] [Google Scholar]


