Abstract
Rising healthcare costs coupled with patient safety considerations and quality of care have become major concerns for healthcare purchasers, providers, and policymakers. Health information technology, particularly the electronic health record (EHR), is posed as a solution to address these concerns by delivering greater efficiencies and improved quality of care. Despite the national movement toward EHR adoption, successful EHR implementation continues to be challenging for many healthcare organizations, both large and small. This article uses sociotechnical systems theory as a framework to discuss 5 best practice guidelines for EHR implementation and outlines what clinical nurse specialists can do to make the process successful.
Keywords: clinical nurse specialist, electronic health record, implementation
Rising healthcare costs have led healthcare professionals and policymakers to consider ways to improve efficiency and cut costs while simultaneously increasing patient safety and quality of care.1 The effective use of technology, specifically electronic health record (EHR) systems, is proposed as one of the primary solutions to the problems facing healthcare today.2 However, implementing and maintaining an EHR system are costly,3 and failure rates remain as high as 50%.4 While the Centers for Medicare & Medicaid Services is offsetting the cost of implementing new EHR systems through the Electronic Health Record Incentive program,5 ensuring successful implementation requires clinical nurse specialists (CNSs) to fully understanding the interrelated social, technical, and environmental factors involved.6
Sociotechnical systems theory is a particularly well-suited tool to identify, analyze, and redesign the complex mixture of technical, social, and environmental components that impact EHR implementation.7 The term sociotechnical system implies that an interrelated and interdependent congruence exists between the social and technical aspects of an organization. In order to optimize the system redesign process, these aspects must not be viewed separately, but instead should be studied in relation to one another. Sittig and Singh6 identified 8 sociotechnical dimensions related specifically to information technology in healthcare including hardware and software, clinical content, the human-computer interface, people (ie, system users), workflow and communication, internal organizational features (including culture and policies), external rules and regulations, and measurement and monitoring. The following 5 best practice guidelines describe how these dimensions relate in the context of leadership and EHR implementation.
FIVE BEST PRACTICE GUIDELINES
Institute a Long-term Plan
The EHR implementation process can be broken down into 3 phases: (1) preimplementation, which includes initial project management and choosing an EHR system; (2) implementation, including workflow redesign, testing, and training; and (3) postimplementation, including ongoing training, quality improvement monitoring, and adaptation.4 It is important to stress that the implementation process is ongoing and requires sustained attention and resources throughout. Even before discussions with EHR vendors can begin, establishing an institutional framework and identifying key stakeholders are crucial.8 This framework is necessary in order to negotiate priorities for system capabilities and development throughout the project’s lifetime.9 The CNS is a key stakeholder to provide input regarding clinical workflow, quality outcomes monitoring, and change management. Establishing change management strategies and communication plans is necessary in order to translate system priorities into deliverables, thereby establishing legitimacy throughout the organization.10
Anticipate Technology and Workflow Evolution
Electronic health record implementation will inevitably change the way an organization functions. Instead of immediately focusing on what needs to change, begin by examining the preimplementation workflow and identifying its strengths as well as its weaknesses as part of a formative assessment.11 Be prepared to incorporate the strengths into the new work-flow while addressing weakness during the design and testing phase. However, keep in mind that workflow and technology issues will continue to be identified well beyond the design and testing phase. Establishing a baseline for expected efficiency, effectiveness, and safety measures during the preimplementation process will help to identify areas that need to be adjusted during the postimplementation phase.12 The CNS is poised to provide leadership concerning the provision of best practice models and thus evaluating workflow to achieve optimal patient outcomes.
Combine Qualitative and Quantitative Evaluation Methods
In order for a CNS to support the adjustment to a new EHR system and a new workflow, both qualitative and quantitative assessment tools should be selected.13 Quantitative methods of analysis are used to analyze the what, why, and how of social phenomenon, whereas quantitative methods capture the size, extent, and duration of a given phenomenon. Combining both qualitative and quantitative methods as part of a process-focused analysis can help to target the areas that need the most attention and give the CNS a way to measure improvement over the course of the project.14
Target Meaningful User Engagement
Electronic health record implementation is highly dependent on system user acceptance and engagement.1 In order to encourage both, recruiting future users to be a part of the design and testing phase is an effective way to get feedback and gain support at the beginning of the implementation process. These users can then become what are known as “superusers” in that they are system experts who are able to help train others and are available for technical support in the early phases of system-wide adoption.15 During system-wide adoption, individuals who are less able and/or willing to adopt the new technology become evident. Super-users can help to individualize training and offer extra support to those who need it.16
Adapt Implementation Strategies as Needed
Appropriate implementation strategies may vary throughout the organization and are dependent on the workflow and function of the users in that area.17 Designating implementation team leaders unique to the unit or site allows the implementation plan to be customized accordingly. This includes designing support materials that relate specifically to the anticipated transitions and changes in workflow and pairing super-users with employees who need additional support. It may also require scheduling additional training after the initial adoption phase to target unforeseen problems in the workflow, or it may mean adjusting the software in order to match the needs of the users.18 In general, promoting flexible and adaptable strategies at the level of the EHR system user increases the likelihood of addressing EHR system implementation problems when and where they start (Figure).15
FIGURE.
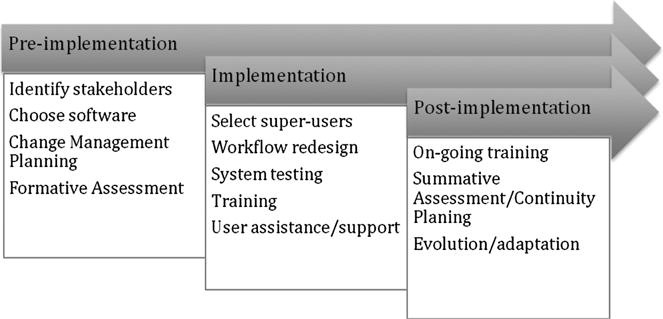
Best practices for electronic health record implementation within a sociotechnical system.
CONCLUSION
Although EHR systems have been identified as a way to raise healthcare quality and safety while reducing costs, EHR implementation is costly and complex. Increasing the likelihood of success involves understanding how the various sociotechnical dimensions are related. It requires commitment to a long-term plan, including a formative assessment process comprising both quantitative and qualitative components. Information gained from this assessment should inform workflow redesign. Planning for and supporting the evolution and adoption of the system workflow beyond the redesign process include targeting meaningful user engagement and providing training and support materials that directly address the concerns of the user. Electronic health record system implementation is an ongoing process consisting of many phases and elements. The CNS practice spheres for EHR implementation are at the organization and nursing practice levels. Developing a strategic plan for system implementation is part of the organization sphere, whereas workload redesign and evaluation lie within the nursing practice sphere. Ensuring successes requires the CNS to be engaged throughout the process.19
Footnotes
The authors report no conflicts of interest.
Contributor Information
Taya Irizarry, Graduate Student, College of Nursing, University of Colorado, Boulder.
Amy J. Barton, Professor and Associate Dean for Clinical and Community Affairs, College of Nursing, University of Colorado, Centennial.
References
- 1.Al-Azmi SF, Al-Enezi N, Chowdhury RI. Users’ attitudes to an electronic medical record system and its correlates: a multivariate analysis. HIM J. 2009;38(2):33–40. doi: 10.1177/183335830903800205. [DOI] [PubMed] [Google Scholar]
- 2.Jha AK, DesRoches CM, Kralovec PD, Joshi MS. A progress report on electronic health records in U.S hospitals. Health Aff (Project Hope) 2010;29(10) doi: 10.1377/hlthaff.2010.0502. [DOI] [PubMed] [Google Scholar]
- 3.Congressional Budget Office. Technological change and the growth of health care spending. 2008 http://www.cbo.gov/ftpdocs/89xx/doc8947/01-31-TechHealth.pdf. Accessed July 8, 2013.
- 4.Keshavjee K, Bosomworth J, Copen J, et al. Best practices in EMR implementation: a systematic review. AMIA Annu Symp Proc. 2006;2006:982. [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Medicare and Medicaid. An Overview of EHR Incentive Programs. 2011 http://www.cms.gov/EHRIncentivePrograms. Accessed July 8, 2013.
- 6.Sittig DF, Singh H. A new sociotechnical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Health Care. 2010;19(Suppl 3) doi: 10.1136/qshc.2010.042085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chisholm RF. A review of applications of the sociotechnical systems approach to health care organizations. J Appl Behav Sci. 1986;22(3) doi: 10.1177/002188638602200310. [DOI] [PubMed] [Google Scholar]
- 8.Adler Kenneth G. How to successfully navigate your EHR implementation. Fam Pract Manage. 2007;14(2):33–39. [PubMed] [Google Scholar]
- 9.Laurie LL, Novak Cindy SG, Nancy ML. The science behind health information technology implementation: understanding failures and building on successes. AMIA Annu Symp Proc. 2012;2012:14. [Google Scholar]
- 10.Mooney Brenda L, Annette MB. 10 Steps to successful EHR implementation. Med Econ. 2011;88(9):S4–S6. S8–S11. [PubMed] [Google Scholar]
- 11.Baron Richard J, Elizabeth LF, Melissa S, Erica W. Electronic health records: just around the corner? Or over the cliff? Ann Intern Med. 2005;143(3):222–226. doi: 10.7326/0003-4819-143-3-200508020-00008. [DOI] [PubMed] [Google Scholar]
- 12.Carr DM. A team approach to EHR implementation and maintenance. Nurs Manage. 2004;35(Suppl 5):15–16. 24. [PubMed] [Google Scholar]
- 13.Eason KD, Dent M, Waterson P, Tutt D, Thornett A. Bottom-up and middle-out approaches to electronic patient information systems: a focus on healthcare pathways. Inform Prim Care. 2012;20(1):51–56. doi: 10.14236/jhi.v20i1.47. [DOI] [PubMed] [Google Scholar]
- 14.McGowan Julie J, Caitlin MC, Eric GP. Formative evaluation: a critical component in EHR implementation. J Am Med Inform Assoc. 2008;15(3) doi: 10.1197/jamia.M2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shachak JJJ, Aviv JJJ, Jan B, Karen T, Alejandro RJ, Louise LC. Understanding end-user support for health information technology: a theoretical framework. Inform Prim Care. 2011;19(3):169–172. doi: 10.14236/jhi.v19i3.810. [DOI] [PubMed] [Google Scholar]
- 16.Krisik KM. Lessons learned. how to smooth your EHR implementation. Health Manage Technol. 2013;34(3):8. [PubMed] [Google Scholar]
- 17.Cresswell K, Morrison Z, Crowe S, Robertson A, Sheikh A. Anything but engaged: user involvement in the context of a national electronic health record implementation. Inform Prim Care. 2011;19(4):191–206. doi: 10.14236/jhi.v19i4.814. [DOI] [PubMed] [Google Scholar]
- 18.Verdon DR. Survey identifies keys to EHR implementation success: hiring outside help, purchasing quality hardware, and getting staff buy-in all important in this phase of adding technology. Med Econ. 2012;89(14):44–46. [PubMed] [Google Scholar]
- 19.National Association of Clinical Nurse Specialists. Statement on Clinical Nurse Specialist Education and Practice. Harrisburg, PA: National Association of Clinical Nurse Specialists; 2004. [Google Scholar]


