Abstract
Background
Acne and facial post-inflammatory hyperpigmentation are relatively common clinical conditions among adolescents and young adults, and inflict psychosocial injuries on sufferers.
Objective
To document the psychosocial and self-esteem implications of acne and facial hyperpigmentation on newly admitted undergraduates.
Materials and methods
A cross-sectional survey was conducted among 200 undergraduates. Demographics and clinical characteristics were obtained and acne was graded using the US Food and Drug Administration 5-category global system of acne classification. Participants completed the Cardiff Acne Disability Index (CADI) and the Rosenberg self-esteem scale (RSES), and data were analyzed using SPSS 20.
Results
Mean age of acne onset was 16.24 ± 3.32 years. There were 168 (84.0%) cases categorized as almost clear, 24 (12.0%) as mild acne, 4 (2.0%) as moderate acne and 4 (2.0%) as severe acne. Acne with facial hyperpigmentation, compared to acne without hyperpigmentation, was associated with significant level of anxiety in 30 participants (26.5% vs 10.3%, p=0.004) and emotional distress in 40 (35.4% vs 10.3%, p<0.001). Acne severity correlated with total CADI score but not with total RSES score. Quality of life (QoL) was significantly reduced among acne patients with facial hyperpigmentation (1.77±1.62, vs 1.07±1.02, p<0.001) compared to those without hyperpigmentation. Acne and facial hyperpigmentation was associated with social life interference, avoidance of public facilities, poor body image and self-esteem and perception of worse disease. There was no association between gender and QoL but acne was related to a reduction of self-worth. Low self-esteem was present in 1.5%, and severe acne was associated with an occasional feeling of uselessness in the male gender.
Conclusion
Acne with facial hyperpigmentation induces poorer QoL and self-esteem is impaired only in severe acne. Beyond the medical treatment of acne, dermatologists should routinely assess the QoL and give attention to treatment of facial post-inflammatory hyperpigmentation among people of color.
Keywords: acne, quality of life, self-esteem, facial hyperpigmentation, undergraduates
Introduction
Acne vulgaris is a global disease of adolescents and young adults and a leading cause of visits to dermatologists. Approximately 80–85% of adolescents are affected at a given time, and the effects can continue into adulthood.1,2 Acne is neither life-threatening nor physically debilitating but has been associated with increased psychosocial burdens; such as increased anxiety, anger, depression, and frustration.3–6 The resulting psychosocial complications, in turn, have implications on vocational and academic performance, quality of life (QoL), and self-esteem.3–6 Until recently, little research attention was given to the psychosocial and emotional impact of acne, despite enormous work done in profiling the science of its pathophysiology, risk factors and treatment.6
Acne impairs QoL,3–11 and the assessment of QoL provides a valuable insight into the debilitating effects.8 Shuster et al9 reported that acne affected the psyche of sufferers in a way comparable to chronic medical conditions like asthma, epilepsy, diabetes, back pain, arthritis, and coronary heart disease. The impairment of QoL in acne patients is irrespective of acne severity, and the sensitivity and specificity of test instruments, and QoL impairment may consequently result in an adolescent’s poor self-image, low self-esteem, as well as social isolation and restriction of activities.3,5 Acne affects the face and upper part of the body, and this makes its contribution to the formation of self-esteem immense. The presence of post-inflammatory hyperpigmentation (PIH) induced by acne is a cause of further distress among acne patients.12 PIH is seen as an amplifier of already impaired psychosocial status, causing poorer QoL, and is associated with the use of cosmetic camouflage due to imperfections.13,14
Self-esteem is defined as favorable or unfavorable attitude toward oneself.15 The assessment of self-esteem is more relevant in today’s society in the context of social media who place a high premium on appearance and body image.4,11 Adolescents and young adults are under intense pressure to ensure their appearance meets acceptable societal standards. Acne and its accompanying blemishes have been related to depressive symptoms, embarrassment, feeling of uselessness, poor self-attitude, and reduced pride, self-worth, and body satisfaction in adolescent late teenage years.6,16
Studies investigating the impact of acne and PIH on QoL and self-esteem are rare in Africa. There is a need to fill the gap in knowledge and demonstrate how much this common skin condition, with demonstrated far-reaching consequences on the emotional and psychosocial life of adolescents, affects the QoL and self-esteem of African young people.
Materials and methods
This cross-sectional study was conducted at the General Outpatient Department (GOPD) of the Ladoke Akintola University of Technology Teaching Hospital (LAUTECH), Ogbomoso, Oyo State, Nigeria. The study aimed to document some clinical characteristics of acne, psychological feelings about acne and to determine the impact of acne and facial PIH on the QoL and self-esteem of newly admitted undergraduates. Two hundred newly admitted undergraduates with acne who fulfilled the inclusion criteria were recruited into the study. The GOPD of the hospital has the responsibility of conducting a compulsory medical examination for fitness, which undergraduates must pass before they can formally enroll into academic activities. The inclusion criteria include a recent admission to the Ladoke Akintola University of Technology as an undergraduate, age 18 years or above, willingness to participate in the study, and written informed consent. Undergraduates who were below 18 years, those being treated for acne, those who showed no interest in the study and those who were not willing to sign informed consent were excluded. Similarly, we excluded participants with other co-existing diseases: skin diseases such as atopic dermatitis, seborrheic eczema, and hair loss. Students with known medical ailments including known sickle cell anemia, epilepsy, human immunodeficiency virus infection (HIV), diabetes mellitus, and chronic renal disease was also excluded.
Clinical assessment
The study participants completed a semi-structured questionnaire to obtain their history, including their present age, age at acne onset, history of facial itch, pus discharging acne eruptions, painful acne eruptions, and the presence of acne-related PIH. The participants were asked about their feelings about the presence of acne and its complications, including whether or not they felt stigmatized, socially unacceptable, judged, depressed, ashamed, anxious or emotionally upset by their acne. Two college certified dermatologists examined the participants, made a clinical diagnosis, documented presence of PIH, assessed the severity of acne and documented the distribution of acne lesions. Each participant also graded their acne on a scale of mild, moderate and severe, based on how they felt.
Assessment of acne severity
Acne was graded (grade 1–5) using the simple US Food and Drug Administration (US-FDA) 5-category global system of acne classification according to the predominant lesions including:
Clear: indicating no inflammatory or non-inflammatory lesions.
Almost clear: rare non-inflammatory lesions with no more than 1 papule/pustule.
Mild: some non-inflammatory lesions, no more than a few papules/pustules but no nodules.
Moderate: up to many non-inflammatory lesions, may have some inflammatory lesions, but no more than 1 small nodule.
Severe: up to many non-inflammatory and inflammatory lesions, but no more than a few nodules.17
Assessment of QoL
The QoL was assessed using the Cardiff Acne Disability Index (CADI).18 The CADI is a 5-item questionnaire with scores ranging from 0 to 3 for a total maximum score of 15 and a minimum score of 0. The percentage impairment was calculated from the grouped scores of the participants over total scores and expressed in percentages. Score 0 = no impairment, scores 1–3 = 7–20% impairment, scores 4–9 = 27–60% impairment, and 10–15 = 67–100% impairment.19
Assessment of self-esteem
Self-esteem was assessed using the Rosenberg self-esteem scale (RSES).15 The RSES instrument uses a 5-point scale that ranges from strongly agree to disagree to rate a series of 10 statements. The total score ranges from 0 to 30. Scores less than 15 suggest low self-esteem, while scores of 15 and higher indicate normal self-esteem. Permission was sought from the rights owners of the instruments for their use in the study. The institutional ethical review committee of LAUTECH Teaching Hospital Ogbomoso approved the study.
Data analysis
The analysis of data was done using the Statistical Package for Social Sciences (SPSS) software, version 18 (SPSS Inc., Chicago, IL, USA). All categorical variables were analyzed using chi-square (χ2) statistics and are presented in tables as fractions and percentages, and as pie charts. Fischer’s exact statistics were utilized as indicated. The continuous and non-skewed continuous variables were analyzed using Student’s t-test and the non-parametric Mann–Whitney test was utilized for skewed data. Effect size was manually calculated using the , where r is the effect size, Z is the Z score generated from SPSS, and N = number of participants. Effect size was interpreted using the Cohen’s effect size estimate.20 The mean rank of the scores of the instruments was compared across gender and presence or absence of acne related PIH. The level of significance was set at p<0.05.
Results
The present study enrolled 200 participants, 96 (48.0%) males, and 104 (52.0%) females. The overall mean age ± SD of all the participants was 23.90 ± 3.34 years. There was no difference in the mean age in terms of gender and the presence or absence of acne with PIH. Acne patients with facial PIH had statistically significant painful eruptions (49.6% vs 14.9%, p<0.001), pus-containing eruptions (33.6 % vs 8.0%, p<0.001), facial scars (53.1% vs 11.5%, p<0.001) and a family history of acne (59.3% vs 31.0%, p<0.001) compared to those without PIH.
Concerning the subjective psychological feelings of all participants about acne, 49 (24.5%) were emotionally upset, 39 (19.2%) were anxious, 29 (14.5%) were depressed, 25 (12.5%) felt judged by others, and 17 (8.5%) felt socially unacceptable. Also, 15 (7.5%) felt stigmatized, and 12 (6.0%) had reduced self-esteem because of their acne. Although there was no gender difference in psychological feelings, acne participants with PIH expressed a significant level of subjective anxiety (26.5% vs 10.3%, p=0.004) and emotional distress (35.4% vs 10.3%, p<0.001) compared to those without PIH (Table 1).
Table 1.
Clinical characteristics of the study participants in terms of gender and facial post-inflammatory hyperpigmentation
| Variables | Total (%) N=200 | Gender
|
Facial PIH
|
||||
|---|---|---|---|---|---|---|---|
| Male (%) | Female (%) | p-value | Acne with facial PIH | Acne without facial PIH | p-value | ||
| Acne presentation | |||||||
| Mean age ± SD (years) | 23.90±3.34 | 24.35±3.49 | 23.48±3.17 | 0.065 | 24.14±2.97 | 23.59±3.26 | 0.245 |
| Mean age of onset ± SD (years) | 16.24±3.32 | 16.15±3.04 | 16.32±3.58 | 0.771 | 16.40±3.26 | 15.76±3.51 | 0.335 |
| Facial pruritus | 47 (23.5) | 15 (15.6) | 32 (30.8) | 0.012 | 31 (27.4) | 16 (18.4) | 0.135 |
| Painful eruptions | 69 (34.5) | 31 (32.3) | 38 (36.5) | 0.528 | 56 (49.6) | 13 (14.9) | <0.001 |
| Purulent eruptions | 45 (22.5) | 19 (19.8) | 26 (25.0) | 0.378 | 38 (33.6) | 7 (8.0) | <0.001 |
| Facial scars | 70 (35.0) | 27 (28.1) | 43 (41.3) | 0.050 | 60 (53.1) | 10 (11.5) | <0.001 |
| Family history of acne | 94 (47.0) | 50 (52.1) | 44 (42.3) | 0.166 | 67 (59.3) | 27 (31.0) | <0.001 |
| Psychological feelings | |||||||
| Stigmatized | 15 (7.5) | 10 (10.4) | 5 (4.8) | 0.670 | 7 (6.2) | 8 (9.2) | 0.424 |
| Socially unacceptable | 17 (8.5) | 9 (9.4) | 8 (7.7) | 0.517 | 12 (10.6) | 5 (5.7) | 0.221 |
| Being judged | 25 (12.5) | 13 (13.5) | 12 (11.5) | 0.669 | 15 (13.3) | 10 (11.5) | 0.706 |
| Loss of self-esteem | 12 (6.0) | 8 (8.3) | 4 (3.8) | 0.182 | 10 (8.8) | 2 (2.3) | 0.071 |
| Depression | 29 (14.5) | 15 (15.6) | 14 (13.5) | 0.664 | 17 (15.0) | 12 (13.8) | 0.803 |
| Feelings of shame | 21 (10.5) | 11 (11.5) | 10 (9.6) | 0.671 | 11 (9.7) | 10 (11.5) | 0.687 |
| Anxiety | 39 (19.2) | 18 (18.8) | 21 (20.2) | 0.874 | 30 (26.5) | 9 (10.3) | 0.004 |
| Emotionally upset | 49 (24.5) | 24 (25.0) | 25 (24.0) | 0.241 | 40 (35.4) | 9 (10.3) | <0.001 |
Abbreviation: PIH, post-inflammatory hyperpigmentation.
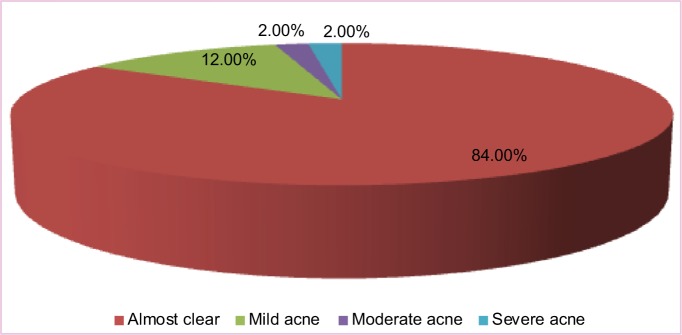
According to the US-FDA 5-category global system of acne severity classification, 168 (84.0%) cases were classified as almost clear, 24 (12.0%) as mild acne, 4 (2.0%) as moderate acne, and 4 (2.0%) as severe acne (Figure 1).
Figure 1.
The severity of acne vulgaris among LAUTECH undergraduates according to the US Food and Drug Administration 5-category global system of acne classification.
Note: The pie chart was created using US Food and Drug Administration classification system.17
The overall mean scores of all participants on CADI was 1.47±1.42. The participants with acne and PIH had significantly higher mean score of CADI (1.77±1.60 vs 1.07±1.02) compared to those without PIH. There was no gender difference in the mean CADI score. Seventy-two participants had no QoL impairment, 114 (57.0%) had 7–20% QoL impairment while 14 (7.0%) had 27–60% QoL impairment. Participants with acne and facial PIH were more likely to have higher scores on CADI compared to those without PIH (p=0.006). Similarly, the overall mean score of RSES was 24.90±3.67, and there was no difference in RSES scores in terms of gender and the presence or absence of PIH distribution among acne patients. Self-esteem was low only in 3 (1.5%) participants (all male), and normal in 98.5% of participants (Table 2).
Table 2.
The pattern of Cardiff Acne Disability Index and Rosenberg self-esteem scale scores among study participants in relation to gender and facial post-inflammatory hyperpigmentation
| Variables | Total (%) N=200 | Gender
|
Facial PIH
|
|||||
|---|---|---|---|---|---|---|---|---|
| Male (% | Female (%) | p-value | Acne with facial PIH | Acne without facial PIH | p-value | |||
| Mean total CADI ± SD | 1.47±1.42 | 1.41±1.35 | 1.52±1.49 | 0.576 | 1.77±1.60 | 1.07±1.02 | <0.001 | |
| CADI group [impairment] | ||||||||
| 0 | [0] | 72 (36.0) | 35 (36.5) | 37 (35.6) | 0.922 | 34 (30.1) | 38 (43.7) | 0.006 |
| 1–3 | [7–20%] | 114 (57.0) | 55 (57.3) | 59 (56.7) | 66 (58.4) | 48 (55.2) | ||
| 4–9 | [27–60%] | 14 (7.0) | 6 (6.2) | 8 (7.7) | 13 (11.5) | 1 (1.1) | ||
| 10–15 | [67–100%] | – | – | – | ||||
| Mean total RSES ± SD | 24.90±3.67 | 24.96±3.70 | 24.85±3.66 | 0.830 | 24.90±3.73 | 25.90±3.62 | 0.991 | |
| RSES group [esteem level] | ||||||||
| 10–15 | [normal SE] | 197 (98.5) | 93 (96.9) | 104 (100.0) | 0.109 | 111 (98.2) | 86 (98.9) | 0.720 |
| >15 | [low SE] | 3 (1.5) | 3 (3.1) | 0 (0.0) | 2 (1.8) | 1 (1.1) | ||
Abbreviations: PIH, post-inflammatory hyperpigmentation; RSES, Rosenberg self-esteem scale; SE, self-esteem; CADI, Cardiff Acne Disability Index.
The correlations between patients’ and physicians’ assessments of acne severity (US-FDA), CADI, and RSES scores were examined using Spearman rank correlation. Total CADI correlated both with the physicians’ assessed severity classification (r=0.152, p=0.030) and patients’ assessed severity of acne (r=0.273, p<0.001). Patients’ severity assessment of acne showed positive correlation most of the CADI axes: aggressive, frustrated or embarrassed (r=0.251, p<0.001), interference with social life (r=0.2, p=0.004), avoidance of public facilities (r=0.158, p=0.002), but not feeling about skin appearance (r=0.119, p<0.090). Meanwhile, physicians’ assessed severity of acne showed a positive correlation with the appearance of skin axis alone (r=0.202, p=0.004).
There was no correlation between total self-esteem scores and both physicians’ and patients’ assessment of acne severity. There was an inverse correlation (r=−0.171, p=0.015 and r=–0.194, p=0.005) between RSES axes of “do not feel that I am a person of worth” and both the patients’ and physicians’ assessed acne severity, respectively. Also, the axes “I certainly feel useless at times” of RSES showed an inverse correlation with patients’ assessed severity (r=−0.177, p=0.012) and positive association (r=0.265, p<0.001) with the physicians’ severity assessment, Table 3.
Table 3.
The correlation of patients’ and physicians’ assessed severity of acne, and the Cardiff Acne Disability Index and Rosenberg self-esteem scale
| Variables CADI |
Patients’ assessed severity of acne
|
Physicians’ assessed (US-FDA) severity of acne
|
||
|---|---|---|---|---|
| Correlation (r) | p-value | Correlation (r) | p-value | |
| Aggressive, frustrated or embarrassed | 0.251** | <0.001 | 0.137 | 0.051 |
| Interfered with social life | 0.201** | 0.004 | 0.125 | 0.075 |
| Avoidance of public facilities | 0.158* | 0.002 | 0.083 | 0.237 |
| Feelings about appearance of skin | 0.286** | <0.001 | 0.202 | 0.004 |
| How bad is your acne now? | 0.119 | 0.090 | 0.044 | 0.530 |
| Total CADI | 0.273* | <0.001 | 0.152* | 0.030 |
| RSES | ||||
| Do not feel that I am a person of worth | −0.171* | 0.015 | −0.194** | 0.005 |
| Do not feel that I have good qualities* | −0.084 | 0.233 | −0.111 | 0.115 |
| Inclined to feel that I am a failure | −0.113 | 0.109 | −0.051 | 0.473 |
| Unable to do things like other people | 0.000 | 0.991 | 0.020 | 0.778 |
| Do not have much to be proud of* | −0.002 | 0.982 | 0.039 | 0.579 |
| No positive attitude towards myself* | −0.124 | 0.078 | −0.120 | 0.088 |
| I am not satisfied with myself | −0.099 | 0.107 | 0.066 | 0.350 |
| Wish for more respect for myself * | 0.107 | 0.128 | 0.117 | 0.095 |
| I certainly feel useless at times* | −0.177* | 0.012 | 0.265** | <0.001 |
| At times I think I am no good at all | 0.024 | 0.733 | −0.037 | 0.600 |
| Total self-esteem | −0.042 | 0.549 | −0.040 | 0.574 |
Notes:
Correlation significant at 0.01 (2 tailed);
Correlation significant at 0.05 (2 tailed)
Abbreviations: CADI, Cardiff Acne Disability Index; RSES, Rosenberg self-esteem scale; US-FDA, US Food and Drug Administration; r = Spearman’s rho.
The scores of acne patients on individual axes of CADI and RSES were examined according to gender classification and the presence or absence of PIH classifications in the Mann–Whitney U-test for non-parametric data with the aim of identifying the differences in the mean rank of scores and the size effect of score differences estimated using Cohen’s effect. There was no difference in the mean rank of CADI and RSES scores across gender classifications, although the female gender had a significantly lower mean rank score in the “do not have much to be proud of” subscale (U=4.28, Z=−2.21, p=0.027, r=0.2). The presence of acne PIH spots was associated with significant higher mean scores across all the subscales of CADI: “aggressive, frustrated, and embarrassed” subscale [U=4.12 (Z=−3.92), p<0.001, r=−0.3], “interfered with social life” subscale [U=4.71 (Z=−2.52), p=0.012, r=−0.2], “avoidance of public facilities” subscale [U=4.77 (Z=−2.00), p=0.046, r=−0.1],“negative feeling about appearance of skin” subscale [U=4.18 (Z=−2.38), p=0.018, r=−0.2], “how bad is your acne now” subscale [U=4.30 (Z=−2.10), p=0.038, r=−0.1] and total CADI [U=3752 (Z=−3.38), p<0.001, r=−0.2] (Table 4).
Table 4.
The relationship between the mean ranks of Cardiff Acne Disability Index (CADI) and Rosenberg self-esteem scale (RSES) scores in relation to gender and acne with and without facial post-inflammatory hyperpigmentation
| Variables CADI |
Mean rank of scores
|
p-value | Mean rank of scores
|
p-value | ||
|---|---|---|---|---|---|---|
| Male | Female | Acne with facial PIH | Acne without facial PIH | |||
| Aggressive, frustrated or embarrassed? | 103.56 | 100.54 | 0.528 | 110.19 | 91.30 | <0.001 |
| Interfered with social life | 102.10 | 101.90 | 0.943 | 105.06 | 98.00 | 0.012 |
| Avoidance of public facilities | 102.70 | 101.35 | 0.646 | 104.57 | 98.65 | 0.046 |
| Feelings about appearance of skin | 100.19 | 103.69 | 0.638 | 109.70 | 91.94 | 0.018 |
| How bad is your acne now? | 103.19 | 100.89 | 0.751 | 108.61 | 93.36 | 0.038 |
| Total CADI | 101.90 | 102.10 | 0.980 | 113.19 | 87.38 | <0.001 |
| RSES | ||||||
| Do not feel that I am a person of worth | 102.10 | 101.91 | 0.967 | 100.42 | 104.06 | 0.426 |
| Do not feel that I have good qualities | 102.76 | 101.30 | 0.719 | 99.50 | 105.26 | 0.160 |
| Inclined to feel that I am a failure | 101.98 | 102.01 | 0.996 | 98.69 | 106.32 | 0.189 |
| Unable to do things like other people | 106.45 | 97.84 | 0.130 | 105.27 | 97.73 | 0.189 |
| Do not have much to be proud of | 110.83 | 93.76 | 0.027 | 98.36 | 106.76 | 0.280 |
| No positive attitude towards myself | 102.50 | 101.53 | 0.865 | 100.88 | 103.47 | 0.652 |
| I am not satisfied with myself | 100.14 | 103.73 | 0.585 | 97.76 | 107.55 | 0.140 |
| Wish for more respect for myself | 94.79 | 108.73 | 0.071 | 110.19 | 91.30 | 0.165 |
| I certainly feel useless at times | 98.87 | 104.92 | 0.376 | 99.91 | 104.73 | 0.484 |
| At times I think I am no good at all | 101.64 | 102.34 | 0.917 | 102.75 | 101.02 | 0.797 |
| Total self-esteem | 103.47 | 100.62 | 0.728 | 101.54 | 102.60 | 0.899 |
Abbreviations: PIH, post-inflammatory hyperpigmentation; RSES, Rosenberg self-esteem scale; CADI, Cardiff Acne Disability Index.
Discussion
PIH is a common condition characterized by increased skin pigmentation following inflammation. Although the etiology of PIH is diverse, it is known to be more common in dark skinned people with acne.21 In the present study, in addition to mild to moderate acne, about 56.0% of the participants presenting with acne had some degree of facial PIH. The present study shows acne negatively affects QoL, and the presence of facial PIH in participants with acne compounded these problems and accounted for poorer psychosocial consequences of acne. Although the severity of PIH was not examined, we found acne severity to be correlated with impaired QoL, while acne alone or with facial PIH had little effect on the self-esteem of the participants. Only 3 cases of severe acne which occurred in males were associated with a reduction of self-esteem in our study.
The mean CADI score (1.77±1.60) for participants with acne and PIH is significantly higher than the 1.07±1.02 observed for cases of acne without PIH, and lower than but comparable to the score of 1.9 (CI: 0–1) from Walker and Lewis-Jones.19 The low CADI score might be related to the predominance of mild cases of acne (84.0%) in our study. The high prevalence of mild to moderate forms of acne as seen in this study is similar to findings documented in some previous studies.5,6,11,22,23 Acne studies based in dermatology clinics are more likely to have a higher proportion of moderate–severe acne compared to surveys done outside of the clinic among predominantly asymptomatic adolescents not seeking treatment. Studies have shown that increasing severity of acne correlated with impairment of QoL.5,19,24 Patients’ assessed severity showed correlation with all axes of CADI except 1 (axis 5), compared to the acne severity assessed using US-FDA scales that only correlated with total CADI score and “feeling about skin appearance” axis. This shows certain patient-related traits might be strong factors contributing to QoL impairment. Studies have shown that the association between QoL and severity of acne varies with QoL instruments, the acne grading system used, participants and the sample size of the survey.3–11,19,22–25
The presence of acne related PIH was significantly associated with a feeling of aggression, frustration, and embarrassment among young acne sufferers. Patients with acne and facial PIH also had social avoidance and negative feelings about their appearance. A recent study showed PIH was most common on the face and sufferers felt embarrassed and concealed imperfections and stains that resulted from acne with makeup.14 Davis and Callender showed acne related facial PIH was more common among individuals of color than others.26 PIH in acne is a cause of further psychological distress in addition to acne itself.26 Darji et al reported that irrespective of the graded severity of PIH associated with acne, PIH induced psychosocial consequences such as self-consciousness and feeling like an outcast, and their participants with PIH had trouble with friends due to higher levels of anxiety and embarrassment in social settings compared to those without acne.13 It has become important to give attention to the treatment of PIH in acne patients, as without this the QoL might not improve, because PIH contributes significantly to its impairment.
Skin disorders associated with the face or other areas of the skin not coverable by clothing can be a source of significant anxiety to patients. Students with acne and PIH expressed significant levels of anxiety and emotional distress. This emotional status has consequences on their psychological life, as acne with PIH significantly interfered with students’ social life and induced more avoidance of public facilities, poor body image and self-esteem, and worse self-assessment of their diseases, than those without PIH. The study by Jowett and Ryan12 supports the present findings of concern about social interactions and socializing, and reduced interaction with the opposite gender among patients with acne. Similarly, in a previous review acne was found to be associated with poor self-image, self-consciousness, and embarrassment, which is further exacerbated by taunting stigmatization, perceptions of scrutiny and being judged, leading to avoidance of interaction and social situations as expressed by our patients.4 There was no gender difference in the QoL, as also found by for example, Darji et al.13
We did not find an association between cumulative self-esteem and acne in the present study, unlike the findings of previous studies,4,24 but acne was associated with a reduction of self-worth and the occasional feeling of uselessness. Studies have shown that self-esteem was proportional and in direct correlation with the severity of acne and participants with severe acne were more likely to be neurotic and liable to lower self-esteem.4,27,28 The prevalence of reduced self-esteem (1.5%) is low compared to 46.8% reported by Tasuola et al5 and Nguyen et al.27 This is probably because of the high prevalence of almost clear to mild acne in our study or because of the cultural interpretation of acne as “a must-have thing” while growing up in the adolescent years. A sub-analysis of our participants shows reduced self-esteem was present in 100% of the cases of severe acne in our study, which is close to 89.3% reported by Tasuola et al,5 and which implies self-esteem might be compromised only in severe acne. Although there was no difference in the self-esteem of participants with acne and hyperpigmentation and those without it, male self-esteem was significantly affected, as they wish for more self-respect because of their acne. Dalgard et al similarly found the presence of acne was associated with poor self-attitude and self-worth in girls alone, independent of body mass index and depression.16
The present study is limited as it is hospital-based and might not be representative of the general population from which sampling was drawn. The small to moderate effect size of the non-parametric inferential testing also limits the strength of its application.
Conclusion
Acne with PIH is associated with poorer QoL in patients. Mild to moderate acne was not associated with a reduction of self-esteem. Acne patients with PIH had a feeling of aggression, frustration, and embarrassment, social life interference, poor self-worth, and reduced self-respect. Beyond the treatment of acne, PIH should be treated in people of color to improve their QoL. Appropriate referral to a psychologist is necessitated when QoL and self-esteem are impaired.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Dreno B, Poli F. Epidemiology of acne. Dermatology. 2003;206(1):7–10. doi: 10.1159/000067817. [DOI] [PubMed] [Google Scholar]
- 2.White GM. Recent findings in the epidemiologic evidence, classification, and subtypes of acne vulgaris. J Am Acad Dermatol. 1998;39:S34–S37. doi: 10.1016/s0190-9622(98)70442-6. [DOI] [PubMed] [Google Scholar]
- 3.Do JE, Cho SM, In SI, Lim KY, Lee S, Lee ES. Psychosocial aspects of acne vulgaris: a community-based study with Korean adolescents. Ann Dermatol. 2009;21:125–129. doi: 10.5021/ad.2009.21.2.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunn LK, O’Neill JL, Feldman SR. Acne in adolescents: quality of life, self-esteem, mood, and psychological disorders. Dermatol Online J. 2011;17:1. [PubMed] [Google Scholar]
- 5.Tasoula E, Gregoriou S, Chalikias J, et al. The impact of acne vul-garis on quality of life and psychic health in young adolescents in Greece. Results of a population survey. An Bras Dermatol. 2012;87:862–869. doi: 10.1590/S0365-05962012000600007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.França K, Keri J. Psychosocial impact of acne and post inflammatory hyperpigmentation. An Bras Dermatol. 2017;92(4):505–509. doi: 10.1590/abd1806-4841.20175645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sulzberger MB, Zaidens SH. Psychogenic factors in dermatological disorders. Med Clin North Am. 1948;32:669–685. doi: 10.1016/s0025-7125(16)35686-3. [DOI] [PubMed] [Google Scholar]
- 8.Gorelick J, Daniels SR, Kawata AK, et al. Acne-related quality of life among female adults of different races/ethnicities. J Dermatol Nurses Assoc. 2015;7(3):154–162. doi: 10.1097/JDN.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shuster S, Fisher GH, Harris E, Binnell D. The effect of skin disease on self image [proceedings] Br J Dermatol. 1978;99(16):18–19. [PubMed] [Google Scholar]
- 10.Cresce ND, Davis SA, Huang WW, Feldman SR. The quality of life impact of acne and rosacea compared to other major medical conditions. J Drugs Dermatol. 2014;13(6):692–697. [PubMed] [Google Scholar]
- 11.Ogedegbe EE, Henshaw EB. Severity and impact of acne vulgaris on the quality of life of adolescents in Nigeria. Clin Cosmet Investig Dermatol. 2014;7:329–334. doi: 10.2147/CCID.S73302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jowett S, Ryan T. Skin disease and handicap: an analysis of the impact of skin conditions. Soc Sci Med. 1985;20:425–429. doi: 10.1016/0277-9536(85)90021-8. [DOI] [PubMed] [Google Scholar]
- 13.Darji K, Varade R, West D, Armbrecht ES, Guo MA. Psychosocial impact of postinflammatory hyperpigmentation in patients with acne vulgaris. J Clin Aesthet Dermatol. 2017;10(5):18–23. [PMC free article] [PubMed] [Google Scholar]
- 14.Kayama, Fujii H, Tanioka M, Miyachi Y. Camouflage therapy for post-inflammatory hyperpigmentation on the face caused by fixed drug eruption. Journal of Cosmetics, Dermatological Sciences and Applications. 2013;3(3):8–10. [Google Scholar]
- 15.Rosenberg M. Society and the Adolescent Self-Image. Rev ed. Middle-town, CT: Wesleyan University Press; 1989. [Google Scholar]
- 16.Dalgard F, Gieler U, Holm JØ, Bjertness E, Hauser S. Self-esteem and body satisfaction among late adolescents with acne: results from a population survey. J Am Acad Dermatol. 2008;59(5):746–751. doi: 10.1016/j.jaad.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services. Food and Drug Administration. Center for Drug Evaluation and Research (CDER) Guidance for Industry; Acne Vulgaris: Developing Drugs for Treatment. 2005. [Google Scholar]
- 18.Cardiff Acne Disability Index (CADI) [webpage on the Internet] [Accessed August 8, 2016]. Available from: sites.cardiff.ac.uk/dermatology/...of.../Cardiff-acne-disability-index-cadi/
- 19.Walker N, Lewis-Jones MS. Quality of life and acne in Scottish adolescent schoolchildren: use of the Children’s Dermatology Life Quality Index (CDLQI) and the Cardiff Acne Disability Index (CADI) J Eur Acad Dermatol Venereol. 2006;20(1):45–50. doi: 10.1111/j.1468-3083.2005.01344.x. [DOI] [PubMed] [Google Scholar]
- 20.Sawilowsky S. New effect size rules of thumb. J Mod Appl Stat Method. 2009;8(2):467–474. [Google Scholar]
- 21.Callender VD, Surin-Lord S, Davis EC, Maclin M. Postinflammatory hyperpigmentation: etiologic and therapeutic considerations. Am J Clin Dermatol. 2011;12:87–99. doi: 10.2165/11536930-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 22.Adityan B, Thappa DM. Profile of acne vulgaris—a hospital-based study from South India. Indian J Dermatol Venereol Leprol. 2009;75:272–278. doi: 10.4103/0378-6323.51244. [DOI] [PubMed] [Google Scholar]
- 23.Muthupalaniappen L, Tan HC, Puah JW, Apipi M, Sohaimi AE, Mahat NF, Rafee NM. Acne prevalence, severity and risk factors among medical students in Malaysia. Clin Ter. 2014;165(4):187–192. doi: 10.7417/CT.2014.1731. [DOI] [PubMed] [Google Scholar]
- 24.Hosthota A, Bondade S, Basavaraja V. Impact of acne vulgaris on quality of life and self-esteem. Cutis. 2016;98:121–124. [PubMed] [Google Scholar]
- 25.Abdel-Hafez K, Mahran AM, Hofny ER, Mohammed KA, Darweesh AM, Aal AA. The impact of acne vulgaris on the quality of life and psychologic status in patients from upper Egypt. Int J Dermatol. 2009;48:280–285. doi: 10.1111/j.1365-4632.2009.03838.x. [DOI] [PubMed] [Google Scholar]
- 26.Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in the skin of colour. J Clin Aesthet Dermatol. 2010;3(7):20–31. [PMC free article] [PubMed] [Google Scholar]
- 27.Nguyen CM, BS, Koo John, Cordoro Kelly M. Psychodermatologic effects of atopic dermatitis and acne: a review on self-esteem and identity. Pediatr Dermatol. 2016;33(2):129–135. doi: 10.1111/pde.12802. [DOI] [PubMed] [Google Scholar]
- 28.van der Meeren HL, van der Schaar WW, van den Hurk CM. The psychological impact of severe acne. Cutis. 1985;36:84–86. [PubMed] [Google Scholar]