Introduction and a Look Back
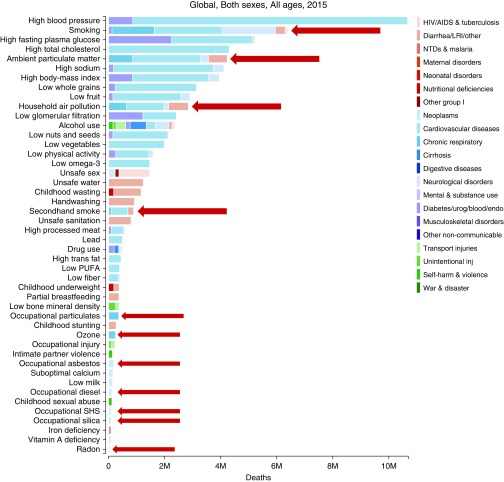
At the 60th annual Thomas L. Petty Aspen Lung Conference, environmental factors remained among the leading causes of premature death and disability worldwide. The 2015 estimates from the Global Burden of Disease project set an informative context for the meeting (Figure 1). Although there have been major gains for some causes of premature death and disability, ambient and household air pollution remain top contributors to disease burden by increasing risk for chronic respiratory diseases and acute respiratory infections, for cardiovascular disease, and for cancer, particularly lung cancer. Substantial gains have been made in high-income countries in controlling ambient air pollution through reduction of emissions from industrial, vehicular, and residential sources and in mitigating indoor air pollution through reducing smoking indoors and other approaches. However, in some low- and middle-income countries (e.g., China and India), ambient air quality has sharply deteriorated and indoor air pollution from combustion of biomass fuels has persisted, receiving little attention until recently. In addition, all nations are facing the threat of climate change and its consequences for human health.
Figure 1.
Global burden of disease 2015: mortality risk factors. AIDS = acquired immunodeficiency syndrome; endo = endocrine; HIV = human immunodeficiency virus; inj = injury; LRI = lower respiratory infection; M = million; NTDs = neglected tropical diseases; Other group I = other group infections; PUFA = polyunsaturated fatty acid; SHS = secondhand smoke; urog = urogenital. Modified from Reference 9 (https://doi.org/10.1016/S0140-6736(17)32366-8) under Creative Commons Attribution License (CC BY) (https://creativecommons.org/licenses/by/4.0/). Arrows were added to the original figure to provide emphasis on specific mortality risk factors.
Thus, for this 60th Aspen Lung Conference, a return to the topic of the environment was timely. Previously, the conference had the environment as the core theme in 1980, 1995, and 2009, summarized by Margaret Becklake, Joe Brain, and David Christiani, respectively (1–3). In her summary, Becklake noted that several prior conferences had covered environmental agents and that all, not surprisingly, had touched on cigarette smoking in one or more presentations. The 1980 conference, my first, took place against the backdrop of the eruption of Mount St. Helens a month before and concerns about the potential health risks of the ash, which had blanketed parts of Oregon and Washington. In a special session, the potential contributions of epidemiology and toxicology were reviewed and the need for complementary strategies was stressed, as was the urgency of assessing risks to inform the public. Looking back, the 1980 conference was held at a point when diverse environmental and occupational agents were established as causes of respiratory disease, and regulations were moving forward. Much of the conference focused on underlying mechanisms and dose–response relationships, critical elements of the evidence foundation for regulation.
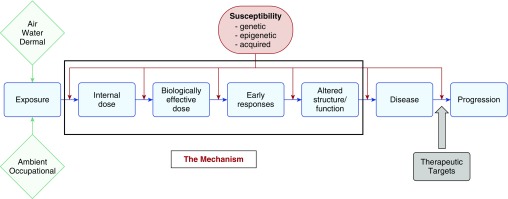
By the time of the 1995 Aspen Lung Conference, the probing of mechanisms had deepened, with many new tools available (2). Emphasis was placed on biomarkers, and the role of molecular epidemiology as a bridging approach from populations to laboratory research was considered. At the time, new epidemiological evidence had retriggered concern about airborne particles and health, and this topic, still a current one, was extensively discussed. The presentations at the 2009 conference, summarized by Christiani (3) within a framework that incorporated environmental agents and genetic determinants of response (Figure 2), reflected the new 21st century tools of genomics and other “omics” and exposure assessment. That framework still remains relevant to the 60th conference, as modified in Figure 2 to capture mechanistic research more fully and research on therapeutic outcomes, addressed in presentations at the 2017 meeting.
Figure 2.
Relationship between exposure, outcome, and susceptibility. Modified from Figure 1 in Reference 3.
The 60th Anniversary Aspen Lung Conference of 2017 reflected the continued and rapid evolution of the approaches used to investigate the environment and the lung. Advances in omics methodologies continue, and permit the probing of pathways by which environmental agents cause injury; the new tools of exposure sciences support estimation of exposures for large populations and deeper characterization for individuals, using the holistic “exposomics” methods. In the United States and globally, such research is increasingly the foundation for regulation and other strategies for risk assessment and risk management that are intended to achieve acceptable levels of risk.
What Environmental Agents Pose a Risk to Human Health?
Plenary presentations provided overviews of some of the environmental agents that threaten health—some focused on agents to which populations are widely exposed (ambient and household air pollution, tobacco products, and the general consequences of climate change), and other presentations provided case studies of specific agents, such as dust from the World Trade Center tragedy, arsenic in drinking water, and exposures sustained by troops deployed to the Gulf region. Ana Navas-Acien provided a global picture of the use of tobacco products, covering evidence-driven gains that have been made in reducing second-hand smoke exposure and the benefits of these reductions. This good news is balanced by the bad news of emerging tobacco products (e.g., hookah and electronic cigarettes) that are being embraced by youth and young adults, and that expose them to toxic agents, including metals. Roger Glass offered a global perspective on environmental agents and health from the perspective of the work of the Fogarty International Center of the National Institutes of Health, which supports teams of U.S. and international investigators. The research focuses on some of the most salient exposures, air pollution and occupational agents, and blends approaches that include exposure assessment, epidemiology, interventions, and implementation. In a focused case study of the Fogarty International Center–supported work, David Warburton described the extraordinarily high levels of air pollution during the wintertime in Ulaanbaatar, Mongolia, and the diverse adverse consequences for the population, including not only respiratory but also reproductive consequences. With his Mongolian colleagues, he has successfully engaged decision-makers in seeking solutions.
John Balmes addressed the most general environmental threat—climate change. His wide-ranging presentation covered how climate change can harm (or benefit) population health, and covered some of the plausible scenarios of increasing climate impact from human activities. Penny Nymark touched on another emerging concern, nanotechnology, and the potential risks of engineered nanomaterials for human health.
Drivers of Susceptibility to Environmental Agents
In his plenary presentation, Joel Kaufman gave a broad perspective on susceptibility, noting that its drivers include not only the specifics of individuals, but broader population-level characteristics (e.g., the sociodemographics of neighborhoods where people live). He commented on the interplay across the range of adverse health effects of environmental agents with the broad suite of determinants of susceptibility, which complicates investigation of susceptibility. He focused on the potential to gain insights by investigating very high-risk groups (e.g., people with cystic fibrosis or after lung transplant) by carrying out intervention studies, such as those in progress in China to reduce personal air pollution exposures.
Rachel Miller illustrated the complexity of investigating susceptibility with the example of childhood asthma, for which there may be key windows of exposure across the life course, including before and after birth. She posed a mechanistic framework that included epigenetic changes from early-life exposures, environmental exposures, and also their interactions with the child’s genes. Supporting evidence for this framework can be found in population studies of children growing up in farming environments who have differing patterns of exposure across the life course. Not surprisingly, other presentations also examined genetic determinants of susceptibility: asbestos (Raphael Bueno) and beryllium (Andrew Fontenot). The work on asbestos focused on the genomes of tumors and the potential for finding therapeutic targets, and only tangentially on risk for developing mesothelioma; for beryllium, there is far more focused understanding of disease risk related to a specific human leukocyte antigen haplotype (4, 5).
Mechanisms of Injury by Environmental Agents
As with previous Aspen Lung Conferences, many presentations explored the mechanisms by which inhaled agents cause injury to the lung and other organs. Looking back to 1980, animal bioassays and simplistic in vitro systems have been supplanted by omics approaches that generate rich and sometimes high-density data sets. We can now explore multiple indicators of response using omics approaches and attempt to construct the activation of pathways that lead to adverse outcomes using surrogates for the apical responses directly relevant to human health. The adverse-outcomes pathway approach, discussed by Nymark in regard to nanomaterials, has been advanced over the last decade for that purpose, after the emergence of pathway-based methods for assessing chemical toxicity (6). She proposed high-throughput testing as one way to prospectively anticipate the toxicity of nanomaterials.
Other presentations addressed specific mechanistic pathways, all illustrating the richness of the data that can now be generated. Karl Kelsey proposed a new term, “immunomethylomics,” to address the multiplicity of immune phenotypes and the role of DNA methylation in generating diverse profiles, possibly in response to environmental agents. Rik Derynck reviewed several roles of transforming growth factor β in disease pathogenesis, covering its broad role and the many potentially related genes. For asthma, Max Seibold gave an overview of the environment and interleukin-13, using asthma as the example. Exploring the expression of thousands of genes, he used clustering methodology to describe patterns of regulation linked to various endophenotypes.
Reducing the Burden of Environmental Lung Disease
Many of the presentations provided evidence with implications for primary prevention, whereas several addressed treatment of pulmonary diseases with environmental etiology: lung cancer, idiopathic pulmonary fibrosis, and chronic beryllium diseases. For lung cancer, there is a search for molecular targets for therapeutic agents, although such targets have not yet been linked to specific etiological agents. For chronic beryllium disease, caused by a single agent through a well characterized mechanism, 5-aminosalicyclic acid is being tested for therapeutic potential.
As indicated by the estimates provided in Figure 1, the substantial disease burden from environmental agents can be greatly reduced through mitigation and elimination of sources, but obstacles are abundant. In the case of cigarettes and other tobacco products, efforts have been underway since the mid-20th century, after the documentation of the strong and causal association of cigarette smoking with lung cancer and other diseases. Progress has been made in many countries, particularly high-income countries, but smoking remains highly prevalent in some countries, and low-prevalence countries are threatened by the multinational tobacco industry.
Climate change and chronic beryllium disease illustrate the challenges of moving from evidence to preventive action. As elegantly presented by Fontenot, the mechanism by which beryllium causes immune sensitization is well worked out, and a revision of the beryllium standard, leading to a substantial reduction in allowable exposure, has been approved by both labor and industry. However, the Occupational Safety and Health Administration under the new presidential administration has delayed implementation of this evidence-based revision. Addressing climate change has proved equally challenging, as described by Balmes. With the replacement of the Obama Administration by the Trump Administration, the United States is backing away from measures intended to reduce greenhouse gas emissions, and will no longer be a party to the Paris Agreement on climate change. In the face of these national actions, Balmes described how the State of California is taking meaningful steps to control emissions of greenhouse gases.
Lessons Learned
Presentations and discussions at the 60th annual Thomas L. Petty Aspen Lung Conference reflected the powerful new tools available to investigate the pathogenesis of environmental lung disease, the increasing multidisciplinarity of environmental lung disease research, the need for approaches for data integration, and the challenges of evidence translation. In summarizing, I highlighted the following:
-
•
Reductionistic versus holistic approaches
-
•
The challenge of defining what a mechanism is, and what is a “causal mechanism”
-
•
Learning something from too much data
-
•
Bridging from laboratory to population to person
-
•
The path from evidence to action is treacherous
Paraphrasing, “Who knew that the environment and the lung could be so complicated?” We need integrative frameworks that can bridge from the increasingly data-intensive approaches of contemporary laboratory methodologies to risks in humans at the individual and population levels. Nymark offered an approach for predictive toxicology for nanomaterials that builds from high-throughput testing. I recently chaired a National Academies of Science, Engineering, and Medicine committee that touched on this topic (the committee on Using 21st Century Science to Improve Risk-Related Evaluations [7]). This committee considered how to use data from the emerging omics technologies to anticipate risks of chemical agents. The “meet-in-the-middle” framework (i.e., using biomarkers to bridge from the laboratory to people) has a central role. This committee explored the complexities of integrating data streams from multiple lines of data generation and the need for methods for this purpose that identify pathways of injury with sufficient certainty.
Undeniably, the 60th annual Aspen Lung Conference took place at the start of a presidential administration that has given little attention to science and that has begun to dismantle the Environmental Protection Agency and regulations intended to protect environmental quality (8). Participants at the meeting could not avoid commenting on the political context and its implications for the impact of their work. The staying of the Occupational Safety and Health Administration beryllium rule exemplified the displacement of reasoned, evidence-based action by nonscientific considerations. Hopefully, the high-quality evidence presented at the annual Aspen Lung Conferences will remain a compelling basis for public health protection.
Supplementary Material
Footnotes
This article was supported with funding by the Fogarty International Center, U.S. National Institutes of Health grant 5U2RTW010125-03. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Becklake MR. The 23d Aspen Lung Conference: the environment and the lung. Conference summary. Chest. 1981;80(1 suppl):89–95. doi: 10.1378/chest.80.1_supplement.89s. [DOI] [PubMed] [Google Scholar]
- 2.Brain JD. Environmental lung disease: exposures and mechanisms. Chest. 1996;109(3 suppl):74S–78S. doi: 10.1378/chest.109.3_supplement.74s. [DOI] [PubMed] [Google Scholar]
- 3.Christiani DC. The environment and the lung: detection, prevention, and mechanism of disease. Proc Am Thorac Soc. 2010;7:146–148. doi: 10.1513/pats.201002-021RM. [DOI] [PubMed] [Google Scholar]
- 4.Balmes JR, Abraham JL, Dweik RA, Fireman E, Fontenot AP, Maier LA, et al. ATS Ad Hoc Committee on Beryllium Sensitivity and Chronic Beryllium Disease. An official American Thoracic Society statement: diagnosis and management of beryllium sensitivity and chronic beryllium disease. Am J Respir Crit Care Med. 2014;190:e34–e59. doi: 10.1164/rccm.201409-1722ST. [DOI] [PubMed] [Google Scholar]
- 5.Fontenot AP, Falta MT, Kappler JW, Dai S, McKee AS. Beryllium-induced hypersensitivity: genetic susceptibility and neoantigen generation. J Immunol. 2016;196:22–27. doi: 10.4049/jimmunol.1502011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Research Council, Committee on Toxicity Testing and Assessment of Environmental Agents, Board on Environmental Studies and Toxicology, Institute for Laboratory Animal Research, Division on Earth and Life Studies. Toxicity testing in the 21st century: a vision and a strategy. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 7. National Academies of Sciences, Engineering, and Medicine; Division on Earth and Life Studies; Board on Environmental Studies and Toxicology; Committee on Incorporating 21st Century Science into Risk-Based Evaluations. Using 21st Century Science to Improve Risk-Related Evaluations. Washington, DC: National Academies Press; 2017 [2017 Jan 5; accessed 2017 Jul 20]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424983/.
- 8.Samet JM, Burke TA, Goldstein BD. The Trump Administration and the environment: heed the science. N Engl J Med. 2017;376:1182–1188. doi: 10.1056/NEJMms1615242. [DOI] [PubMed] [Google Scholar]
- 9.GBD 2016 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioral, environmental and occupational, and metabolic risks or clusters of risk, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390:1345–1422. doi: 10.1016/S0140-6736(17)32366-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.