Abstract
Background
Adjuvant acupuncture for the symptomatic treatment of migraine reduces the frequency of headaches and may be at least similarly effective to treatment with prophylactic drugs.
Methods
This article describes an open-label randomized controlled clinical trial with two groups: the intervention group (n=42) and the waiting-list control group (n=44). This study occurred at the Czech-Chinese Center for Traditional Chinese Medicine at the University Hospital Hradec Kralove between October 2015 and April 2017.
Results
After 12 weeks of acupuncture, the number of migraine days was reduced by 5.5 and 2.0 days in the acupuncture and the waiting-list control groups, respectively, with a statistically significant inter-group difference of 2.0 migraine days (95% CI: −4 to −1). A significantly greater reduction in the number of migraine days per 4 weeks was reached at the end of the 6-month follow-up period in the acupuncture vs. control groups (Δ −4.0; 95% CI: −6 to −2). A statistically significant difference was observed in the number of responders to treatment (response defined as at least a 50% reduction in average monthly migraine day frequency) in the acupuncture vs waiting-list control groups (50% vs 27%; p<0.05) at the end of the intervention. A significantly greater percentage of responders to treatment was noted in the intervention vs control groups at the 6-month follow-up (81% vs 36%; p<0.001).
Conclusion
Acupuncture can reduce symptoms and medication use, both short term and long term, as an adjuvant treatment in migraine prophylaxis in Czech patients.
Keywords: acupuncture, effectiveness, migraine, prophylaxis, Traditional Chinese medicine, treatment
Introduction
According to the systematic review by Natoli et al,1 the prevalence of migraine is 0%–5.1%, with estimates typically in the range of 1.4%–2.2%. Based on the Global Burden of Disease Survey 2010 conducted by the World Health Organization (WHO), migraine was ranked as the seventh highest cause of disability in the world, accounting for 2.9% of all years of life lost to disability.2 In addition to the significant socioeconomic burden that migraine imposes on societies, migraine negatively affects many aspects of patients’ personal lives, including career, social activities, leisure time and family.3,4
Successful migraine management depends on the clinician’s approach, a patient’s compliance and realistic expectations.5 Many patients become nonadherent to therapy because of the perceived ineffectiveness of medication or the occurrence of drug side effects. These reasons were commonly cited among people with headache and migraine who used other forms of complementary and alternative methods (CAMs) and often combined them with standard pharmacological treatments.6–8 CAM users are more likely to suffer from more intense headaches for a longer period of time, have comorbid mental health conditions and experience more negative life impacts from migraine compared to non-CAM users.9 Vitamins, diet, massage, acupuncture, relaxation/meditation, biofeedback, light avoidance and hot/cold therapy belonged to the most popular therapies.9 Although evidence for CAM effectiveness is often controversial, there is some evidence that patients with migraine may benefit from cognitive-behavioral therapies including relaxation and biofeedback, minerals (eg, magnesium), vitamins (eg, pyridoxine), herbal supplements (eg, butterbur, ginkgolide B), other dietary supplements (eg, coenzyme Q10) and traditional healing techniques such as acupuncture.10,11 An updated review on acupuncture for the prevention of episodic migraine included 22 trials with 4,985 participants. The authors concluded that adding acupuncture to the symptomatic treatment of attacks reduces the frequency of headaches and may be at least similarly effective as treatment with prophylactic drugs.11 At the same time, acupuncture showed a lower risk of serious adverse reactions than many orthodox medical treatments.12,13
In the Czech Republic, the prevalence of Traditional Chinese medicine (TCM) use during the last 30 days among the general population was 1.5% in 2011, which is slightly lower compared with other countries.14,15 There has been greater focus on this mode of CAM therapy in recent years, especially after the opening of the first University Center for Traditional Chinese Medicine at the University Hospital Hradec Kralove in 2015 in the Czech Republic.16 Currently, acupuncture is well regulated and practiced by a minimum of 500 physicians certified in acupuncture.17
Currently, no data are available on acupuncture effectiveness among Czech migraine patients. The goal of this study was to evaluate the short- and long-term effectiveness of 14 adjuvant sessions of acupuncture with conventional treatment administered over the course of 3 months compared with standard pharmacological treatment alone in patients with clinically diagnosed migraine. The reduction in migraine day frequency was assessed as the primary outcome. The number of patients with a reduction of migraine days >50%, migraine duration and intensity, reductions in relief medication use and quality of life were monitored and assessed as secondary outcomes. The outcomes were evaluated at baseline and at 3 and 9 months after randomization to determine the short-and long-term benefits of acupuncture.
Methods
Study design and setting
This was an open-label randomized controlled clinical trial. The study occurred at the Czech-Chinese Center for Traditional Chinese Medicine at the University Hospital Hradec Kralove between October 2015 and April 2017.
Patients
Patients between 18 and 70 years of age with a history of migraine for at least 12 months and a minimum of 4 days of migraine per 4 weeks attending the neurology outpatient clinic at the University Hospital Hradec Kralove were consecutively enrolled in this study. All patients were diagnosed with migraine with or without aura by board-certified neurologists according to the criteria of the International Classification of Headache Disorders.18 The participants were informed about acupuncture benefits and side effects and provided a written informed consent before study entry. This study was approved by the ethics committee of the University Hospital Hradec Kralove. The trial was registered under DRKS00009803.
Patients were excluded if they were pregnant; had malignancy; had experienced acupuncture treatment for the face, hands, legs or front part of the body in the past 6 months; had a history of head or neck injury; had severe arrhythmia or heart failure, brain tumor, epilepsy and hemophilia; had participated in another clinical trial in the past 6 months; were unable to distinguish between migraine and tension-type headache and were using anticoagulants or Chinese herbal medicines.
The patients were allocated to either the acupuncture group or the waiting-list control group that received delayed acupuncture treatment after the end of the 6-month follow-up period.
Intervention
In this study, traditional Chinese-style acupuncture was used and treatments were conducted by a specialized acupuncturist with a master’s degree in acupuncture and >15 years of clinical practice in acupuncture. The acupuncture points were selected according to traditional classic and systematic reviews of ancient and modern literature on acupuncture for migraine.19
During the 12-week treatment period, acupuncture treatment was performed 14 times. Acupuncture occurred twice a week in the first 4 weeks, once a week during weeks 5–8 and once every 14 days during the last month. A semi-standardized acupuncture treatment protocol was used. The locations of the acupuncture points were determined according to the WHO standards of acupuncture nomenclature.20 The protocol was composed of a set of mandatory and optional acupuncture points (Table 1). Optional points were selected based on the diagnosis of TCM syndrome as determined by the acupuncturist, with a limit of 9–12 needles introduced at each acupuncture session in total. Acupuncture needles with a diameter of 0.20 mm and a length of either 25 or 40 mm were used according to the locations of the acupuncture points.21 The depth of acupuncture needle insertion was 10–30 mm according to the location of the acupuncture point. Acupuncture needles were introduced after local skin disinfection. When an acupuncture needle was introduced, a specific sensory perception called the De Qi sensation (a complex feeling including soreness, numbness, heaviness, distention and dull pain at the site of needle placement) was experienced by a patient. Acupuncture needles were left in the acupuncture point for 25 minutes.
Table 1.
Selection of acupuncture points
| Syndromes | Mandatory acupuncture points | Optional acupuncture points (bilateral) by syndrome |
|---|---|---|
| Ascending hyperactivity of liver yang | Fengchi (GB20) Taiyang (EX-HN5) Shuai Gu (GB8) | Baihui (DU20), Xingjian (LR2), Taichong (LR3), Taixi (KI3), Xuanzhong (GB39), and Sanyinjiao (SP6) |
| Deficiency of both Qi and blood | Hegu (LI4) | Baihui (DU20), Shang Xing (DU23), Zusanli (ST36), and Sanyinjiao (SP6) |
| Wind phlegm blocking the meridians | Feng Long (ST40), Zhongwan (CV12), and Yinlingquan (SP9) | |
| Blood stasis | Sanyinjiao (SP6), Xuehai (SP10), and Ashi point |
A full case history was taken by the acupuncturist, together with tongue and pulse examinations, to arrive at an individual diagnosis in accordance with the principles of TCM. Although all patients in the study had migraine, this corresponded to several TCM patterns, making individual diagnosis essential. The same acupuncturist carried out the treatments according to a semi-standardized acupuncture treatment protocol.
The patients were informed about acupuncture as follows: “In this study, traditional Chinese style acupuncture will be used. This type of acupuncture is similar to the acupuncture treatment used in China.” Minimal discussion related to treatment was held between the study participants and the acupuncturist to reduce placebo effects from the patient–therapist interaction.
Standard pharmacological treatment
During this study, the patients in the waiting-list control group used standard pharmacological treatments following the appropriate guidelines (Headache Classification Subcommittee of the International Headache Society, 2004). Additionally, the patients in the intervention group were allowed to take their prophylactic medications and analgesics as needed (eg, beta blockers, tricyclic antidepressants, divalproex, topiramate, or in cases with insufficient effect monoamine oxidase inhibitors, flunarizine or gabapentin).
Rationale for the comparator
False acupuncture was not done. The reason for the decision not to include a control group of patients is the analysis of fake acupuncture studies published in the Cochrane Systematic Review.22 An analysis of 12 clinical trials using false acupuncture showed that acupuncture points used for migraine prophylaxis are not specific. The acupuncture effect in the analysis was the same in the true acupuncture group and in the false acupuncture group. Another conclusion of the analysis was the observation that a large proportion of the patients with migraine included individuals who were susceptible to placebo effects. Fake acupuncture also plays a role because acupuncture points can vary in size. In the case of false acupuncture performed 1–2 cm from the acupuncture point, the acupuncture point can be stimulated (the difference between the effect of true acupuncture vs false penetrating acupuncture was 7%, and the difference in the effect of true acupuncture vs false non-penetrating acupuncture was 15%).23,24
Outcome measures
Primary outcome
The primary outcome was the difference in the number of migraine days during the last 4 weeks before randomization (baseline period) and at weeks 12 and 36 after randomization. A migraine day was defined as a headache lasting for at least 30 minutes to 4 hours (believed by the subject to be a migraine that was relieved by medication) or ≥4 hours and had at least two of the following (unilateral location, pulsating quality, moderate or severe intensity and aggravation by or causing avoidance of routine physical activity). Moderate to severe pain intensity was defined as a cutoff of 30 mm on a 100 mm visual analog scale (VAS).25
Secondary outcomes
The secondary outcome measures included reduction in migraine attacks, headache intensity (mm) and duration (hours), reduction in the use of relief medication (Anatomical Therapeutic Chemical Classification System/defined daily doses [ATC/DDDs]) and the number of patients with a reduced monthly frequency of migraine days by ≥50% over 4-week period.26 Distinct attacks were defined as attacks separated by an entire 24-hour period of freedom from headache as recommended by the guidelines for controlled trials of drugs in migraine.27 Pain intensity was assessed on a 10-point visual analog scale (VAS). All patients completed daily diaries of headaches and medication starting 4 weeks prior to randomization up to the 6-month follow-up. Migraine-specific quality of life was also evaluated using the Migraine Disability Assessment Scale (MIDAS).28 Questionnaires were completed at baseline, 12 weeks after the end of acupuncture treatment and at the 6-month follow-up in the respective study groups.
In addition, adherence to acupuncture treatment was assessed. Adverse reactions to acupuncture were monitored based on Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) guidelines.29
Data on sociodemographic characteristics such as age, sex, education, family income, marital status, religion, self-perceived health, comedication and comorbidites were collected using self-reported questionnaire. Medical data were verified against electronic patient medical records at the University Hospital Hradec Kralove. The STRICTA recommendations and CONSORT guidelines on randomized controlled trial (RCT) reporting were followed.29,30
Statistical analysis
Sample size
The sample size was determined relative to the achievement of a significant alpha result <0.05 with a probability of at least power =1-beta ≥0.8, assuming an effect of an average size of at least f=0.25. When determining the correlation between measures ~0.5, GPower counted the necessary net number of people as n=76 with consideration for possible losses due to insufficient adherence or other reasons for lost observations. Therefore, we accepted 91 patients, including 86 who met the criteria and were submitted to randomization.31
Randomization
Block randomization was used, with 12 participants in each block. The randomization criteria were age, sex and the number of headache days during the past 4 weeks.
Data processing and analysis
An independent researcher prepared the computer-generated randomization. Independent assistants who entered and assessed the data were blinded to the treatment allocation.
Descriptive statistics were computed for the variables of interest. To compare the data within and between the groups, parametric and nonparametric tests were used based on data normality. Calculations were based on the intention-to-treat population. The resulting significance level for a single comparison was 0.05. The statistical analysis was performed using the software SPSS version 18.0.
Results
Patients’ characteristics
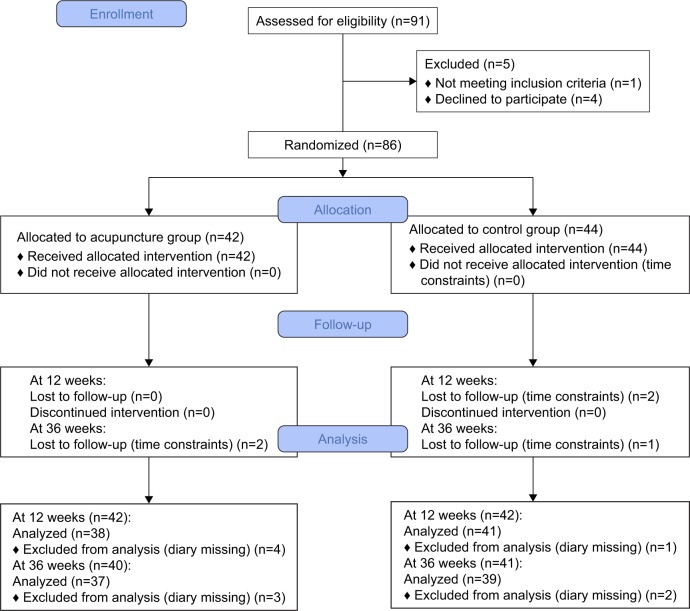
Baseline patients’ characteristics are shown in Table 2. No differences were found between the intervention and control groups at baseline. A total of 91 patients were enrolled in this study. Eighty-six patients were ultimately entered into the intention-to-treat analysis. The flow diagram is presented in Figure 1.
Table 2.
Baseline sociodemographic characteristics
| Characteristics | Acupuncture group (n=42) | Control group (n=44) |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 45.6 (12.8) | 46.5 (10.3) |
| Median | 47 | 47.5 |
| Female, n (%) | 37 (88) | 39 (89) |
| Positive family history of migraine, n (%) | 24 (57) | 29 (66) |
| Duration of migraine (years) | ||
| Mean (SD) | 26.9 (12.9) | 23.0 (14.1) |
| Median | 27.5 | 20.0 |
| Syndrome, n (%) | ||
| Deficiency of both Qi and blood | 9 (21.4) | 10 (22.7) |
| Blood stasis | 7 (16.7) | 7 (15.9) |
| Ascending hyperactivity of liver yang | 13 (31.0) | 11 (25.0) |
| Wind phlegm blocking the meridians | 13 (31.0) | 16 (36.4) |
| Comorbidity, n (%) | 23 (54.8) | 23 (52.3) |
| Smokers, n (%) | 9 (21) | 5 (11) |
| Migraine days | ||
| Frequency (n per month) | 11.97 (6.6) | 12.1 (9.2) |
| Duration (hours) | 12.2 (15.3) | 10 (11.4) |
| Intensity, VAS (mm) | 5.2 (1.3) | 5.4 (1.8) |
| Drug consumption, (ATC/DDD) | 14.8 (14.3) | 11.5 (11.8) |
| Migraine attack (n per month) | 6.4 (2.4) | 6.0 (2.7) |
| MIDAS score | 48.9 (38.1) | 52.9 (31.9) |
| MIDAS severity, n (%) | ||
| Little | 1.0 (2.4) | 0.0 (0.0) |
| Mild | 1.0 (2.4) | 0.0 (0.0) |
| Moderate | 5.0 (11.9) | 4.0 (9.1) |
| Severe | 24.0 (57.1) | 28.0 (63.6) |
Note: Data shown as mean (SD) unless indicated otherwise.
Abbreviations: ATC/DDD, Anatomical Therapeutic Chemical Classification System/defined daily doses; MIDAS, Migraine Disability Assessment Scale; VAS, visual analog scale.
Figure 1.
Flow diagram.
Adherence to acupuncture
In all, 67% of the acupuncture patients completed all acupuncture sessions (mean, 13.5; median, 14 [interquartile range 13–14]). The number of needle insertions per subject per session was 16.3 (range: 14–20).
Effectiveness after the 12-week intervention and the 6-month follow-up
Migraine days
After 12 weeks of acupuncture, the number of migraine days was reduced by 5.5 vs 2.0 days in the acupuncture and waiting-list control groups, respectively, with a statistically significant inter-group difference of 2.0 migraine days (95% CI: −4 to −1).
A significantly greater reduction in the number of migraine days per 4 weeks was achieved at the end of the 6-month follow-up period in the acupuncture vs control groups (Δ −4.0; 95% CI: −6 to −2).
A statistically significant difference in the number of responders to treatment was observed (response defined as at least a 50% reduction in average monthly migraine day frequency) in the acupuncture vs waiting-list control groups (50% vs 27%; p<0.05) at the end of the intervention. A significantly greater percentage of responders to treatment was noted in the intervention vs control groups at the 6-month follow-up (81% vs 36%; p<0.001).
No significant differences in pain intensity and duration were noticed within or between the groups (Table 3).
Table 3.
Changes in the clinical outcomes from baseline to 3 and 9 months after randomization
| Clinical outcome | Acupuncture group (n=42)
|
Control group (n=44)
|
DI (Δ) | 95% CI | ||
|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |||
| Baseline – post-intervention (3 months) | ||||||
| Migraine days | ||||||
| Frequency (n per month)a | 38 | −5.5d (−8, −2) | 41 | −2d (−5, 0.5) | −2.00e | (−4 to −1) |
| Duration (hours)a | 38 | −0.46 (−4.5, 1.3) | 40 | −0.07 (−2.7, 1.3) | −0.53 | (−2.5–1.2) |
| Intensity, VAS (mm)a | 38 | −0.18 (1.3) | 41 | 0.3 (0.76) | −0.48 | (−0.96 to −0.001) |
| Drug consumption (N02, M01, R06), (ATC/DDD)a. | 38 | −3.2c (−10, −1) | 41 | −1.2c (−4.7, 1.0) | −2.70e | (−5.2 to −0.7) |
| Responder rate, n (%) | 38 | 19 (50) | 41 | 11 (27) | 8e | |
| Migraine attack | ||||||
| Frequency (n per month)b | 38 | −2.2c (2.6) | 41 | −0.7d (1.9) | −1.47f | (−2.5 to −0.45) |
| MIDAS scoreb | 26 | −18.15c (23.3) | 27 | −10.7c (30.3) | −7.5 | (−22.4–7.5) |
| Baseline – post-intervention (9 months) | ||||||
| Migraine days | ||||||
| Frequency (n per month)a | 37 | −7c (−10, −4) | 39 | −4c (−7, −1) | −4f | (−6 to −2) |
| Duration (hours)a | 33 | −0.89 (−3, 2) | 36 | −0.48 (−2.8, 2.2) | 0.121 | (−2.1–2.3) |
| Intensity, VAS (mm)b | 32 | 0.18 (1.5) | 37 | 0.13 (0.97) | 0.05 | (−0.55–0.65) |
| Drug consumption (N02, M01, R06), (ATC/DDD)a | 33 | −5.7c (−11, −3) | 38 | −2.7c (−7, 0.02) | −3e | (−5.8 to −0.7) |
| Responder rate, n (%) | 37 | 30 (81.1) | 39 | 14 (35.9) | 16f | |
| Migraine attack | ||||||
| Frequency (n per month)b | 37 | −3.4c (2.2) | 39 | −2.1c (2.4) | −1.36e | (−2.4 to −0.31) |
| MIDAS scoreb | 29 | −15.8c (25.6) | 29 | −6.2 (32.6) | −9.55 | (−25–5.9) |
Notes:
Data are presented as median (25 quartile, 75 quartile).
Data are presented as mean (SD).
Level of significance 0.01 (within group comparison, paired t-test, Wilcoxon signed-rank test).
Level of significance 0.05 (within group comparison, paired t-test, Wilcoxon signed-rank test).
Level of significance 0.05 (between-group comparison, unpaired t-test, Mann–Whitney test, Fisher’s exact test).
Level of significance 0.01 (between-group comparison, unpaired t-test, Mann–Whitney test, Fisher’s exact test). DI is the difference between the acupuncture and the control groups.
Abbreviations: ATC/DDD, Anatomical Therapeutic Chemical Classification System/defined daily doses; MIDAS, Migraine Disability Assessment Scale; VAS, visual analog scale.
Symptomatic medication intake
The acupuncture group showed a larger reduction in symptomatic medication intake compared to the waiting-list control group after the end of acupuncture (Δ −2.7; 95% CI: −5.2 to −0.7) and at the 6-month follow-up (Δ −3.0; 95% CI: −5.8 to −0.7; Table 3).
Migraine Disability Assessment Scale (MIDAS)
The mean scores on the migraine-specific quality of life questionnaire as measured by the MIDAS significantly decreased in both groups, and no inter-group difference was detected (−18.2 vs −10.7; p>0.05) at the end of the intervention (Table 3).
At the end of the 6-month follow-up period, a significant reduction in the MIDAS score was noted only in the acupuncture group with no significant inter-group difference (−15.8 vs −6.2; p>0.05).
Nevertheless, a statistically significant difference was observed between the number of patients with mild (grades I and II; mean score 0–10) vs moderate and severe disability (grades III and VI; mean score >10) before and after the intervention and at the follow-up in favor of the acupuncture group (mild vs moderate/severe disability; week 0 – acupuncture: 6.4%/93.5% vs control: 0%/100%; week 12 – acupuncture: 38%/62% vs control: 16%/84%, week 36: 40%/60% vs control: 13%/87%; p<0.05).
Adverse events
One mild and common adverse event was reported during the 3-month course of acupuncture. Facial hematoma resolved within 2 days without medication or medical help.
Discussion
This was a randomized clinical trial investigating short-and long-term effectiveness of acupuncture for migraine prophylaxis. Currently, prophylactic treatment is indicated in specific cases with the goals of reducing the frequency of migraine attacks, decreasing the consumption of acute medications, improving the quality of life of the patient, reducing the cost of treatment and reducing the risk of migraine transformation into a chronic condition. Acupuncture is one of alternative prophylactic methods with the advantage of absent interactions with chronic medications.
The effectiveness of an individual prophylactic drug is difficult to assess accurately; however, it is estimated in 50% of patients on average.32,33 Amongst the most common prophylactic drugs are beta blockers, tricyclic antidepressants and divalproex sodium (DVPX), the latter being a topiramate.
In this regard, beta blockers are widely used in the prophylactic treatment of migraine, resulting in an estimated >50% reduction in attack frequency.34 On the other hand, Silberstein et al reported that topiramate-treated patients (50 mg/day, 35.9% [p=0.04]; 100 mg/day, 54.0% [p<0.001]; and 200 mg/day, 52.3% [p<0.001]) exhibited a ≥50% reduction in monthly migraine frequency when compared against placebo-treated patients (22.6%).35
A total of 176 patients were randomized (44 placebo, 132 DVPX); of them, 171 provided efficacy data and 137 completed the study. The mean reduction in migraine frequency (per 4 weeks) as a result of DVPX treatment was of 1.7 (500 mg), 2.0 (1,000 mg) and 1.7 (1,500 mg), whereas only a mean reduction of 0.5 migraine attacks was observed in the placebo group (p≤0.05 vs placebo). Concerning DVPX-treated patients, 44%–45% achieved a ≥50% reduction in migraine attack frequency (p≤0.05 vs placebo), as opposed to only 21% of placebo patients. Based on these observations, the recommended initial DVPX dose in migraine prophylaxis is 500 mg/day, although some patients could benefit from higher doses.36
On the other hand, amitriptyline is the only antidepressant able to prevent migraines, as observed in placebo-controlled trials (effect size, 0.62; 95% CI: 0.15–1.1).37
Obtained data from the Cochrane Database of Systematic Reviews showed an association between acupuncture and a moderate reduction in headache frequency in comparison with control patients (four trials, 2,199 participants; standardized mean difference [SMD] =0.56; 95% CI: −0.65 to −0.48); However, these findings were statistically heterogeneous (I2=57%; moderate quality evidence).11 In our study, half of the patients undertaking acupuncture showed at least a 50% reduction in average monthly migraine day frequency and the improvement persisted over 6 months. Compared to other work, Linde et al showed that the number of days with headaches of moderate or severe intensity decreased by a mean (SD) of 2.2 days (2.7 days) in an acupuncture group between baseline and weeks 9–12, which is similar to our results.38 The goal of prophylactic treatment is not only to reduce the frequency of migraine attacks but also to reduce the consumption of acute medications. The acupuncture group showed a greater reduction in symptomatic drug intake compared to the waiting-list control group after the end of the intervention (Δ −2.7; 95% CI: −5.2 to −0.7) and at the 6-month follow-up (Δ −3.0; 95% CI: −5.8 to −0.7). The acupuncture effect of reduced symptomatic medication consumption was also demonstrated in other works.19,38 The MIDAS questionnaire is a standardized questionnaire that assesses the ability to work and conduct daily life activities on five dimensions. Acupuncture treatment at the end of the 6-month follow-up revealed significantly reduced MIDAS scores. The findings of the current study are supported by the study by Facco et al.39
The advantages of our study are assessment of both a short-and a long-term effect of acupuncture as well as its safety, following guidelines 1) for controlled trials on migraine and 2) reporting interventions in controlled trials of acupuncture and low dropout rates. Our study has several limitations. Patients entering the study were not blinded and may have had strong treatment preferences for acupuncture, which may have introduced adjuvant treatment effect. On the other hand, nonspecific effects most likely affected both the intervention as well as the waiting-list control group evenly since both groups showed improvement in the number of migraine days and symptomatic medication use after 12 and 36 weeks of randomization. Occurrence of spontaneous improvement could not also be ruled out. Nevertheless, we monitored selected non-specific factors in the study and the results will be presented separately. Among patients with migraine, acupuncture was associated with a short- and a long-term reduction in the number of migraine days and symptomatic medication intake during the last 4 weeks. Acupuncture is an alternative treatment modality for patients suffering from frequent migraine attacks, especially those who do not consume regular oral medications due to fear of possible side effects. It is also an alternative therapy for patients who do not show an adequate response to standard prophylactic treatment.
Acknowledgments
The authors would like to thank Professor George Lewith for his contribution to the conception and design of the study and Mgr Jiri Haviger, PhD, and Mgr Ales Kubena, PhD for providing statistical supervision for the study. This study was supported by MH CZ-DRO (UHHK, 00179906).
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Natoli JL, Manack A, Dean B, et al. Global prevalence of chronic migraine: a systematic review. Cephalalgia. 2010;30(5):599–609. doi: 10.1111/j.1468-2982.2009.01941.x. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2016 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/S0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buse DC, Lipton RB. Global perspectives on the burden of episodic and chronic migraine. Cephalalgia. 2013;33:885–890. doi: 10.1177/0333102413477736. [DOI] [PubMed] [Google Scholar]
- 4.Lipton RB, Silberstein SD, Saper JR, Bigal ME, Goadsby PJ. Why headache treatment fails. Neurology. 2003;60(7):1064–1070. doi: 10.1212/01.wnl.0000052687.03646.74. [DOI] [PubMed] [Google Scholar]
- 5.Wells RE, Bertisch SM, Buettner C, Phillips RS, McCarthy EP. Complementary and alternative medicine use among adults with migraines/severe headaches. Headache. 2011;51(7):1087–1097. doi: 10.1111/j.1526-4610.2011.01917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adams J, Barbery G, Lui CW. Complementary and alternative medicine use for headache and migraine: a critical review of the literature. Headache. 2013;53(3):459–473. doi: 10.1111/j.1526-4610.2012.02271.x. [DOI] [PubMed] [Google Scholar]
- 7.Rhee TG, Harris IM. Gender differences in the use of complementary and alternative medicine and their association with moderate mental distress in U.S. adults with migraines/severe headaches. Headache. 2017;57(1):97–108. doi: 10.1111/head.12986. [DOI] [PubMed] [Google Scholar]
- 8.Lee J, Bhowmick A, Wachholtz A. Does complementary and alternative medicine (CAM) use reduce negative life impact of headaches for chronic migraineurs? A national survey. Springerplus. 2016;5:1006. doi: 10.1186/s40064-016-2362-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schiapparelli P, Allais G, Castagnoli Gabellari I, Rolando S, Terzi MG, Benedetto C. Non-pharmacological approach to migraine prophylaxis: part II. Neurol Sci. 2010;31:S137–S139. doi: 10.1007/s10072-010-0307-4. [DOI] [PubMed] [Google Scholar]
- 10.Mauskop A. Nonmedication, alternative, and complementary treatments for migraine. Continuum (Minneap Minn) 2012;18(4):796–806. doi: 10.1212/01.CON.0000418643.24408.40. [DOI] [PubMed] [Google Scholar]
- 11.Linde K, Allais G, Brinkhaus B, et al. Acupuncture for the prevention of episodic migraine. Cochrane Database Syst Rev. 2016;6:CD001218. doi: 10.1002/14651858.CD001218.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med. 2004;22:122–133. doi: 10.1136/aim.22.3.122. [DOI] [PubMed] [Google Scholar]
- 13.Witt CM, Pach D, Brinkhaus B, et al. Safety of acupuncture: results of a prospective observational study with 229,230 patients and introduction of a medical information and consent form. Forsch Komplementmed. 2009;16:91–97. doi: 10.1159/000209315. [DOI] [PubMed] [Google Scholar]
- 14.Frass M, Strassl RP, Friehs H, Müllner M, Kundi M, Kaye AD. Use and acceptance of complementary and alternative medicine among the general population and medical personnel: a systematic review. Ochsner J. 2012;12:45–56. [PMC free article] [PubMed] [Google Scholar]
- 15.Pokladnikova J, Selke-Krulichova I. Prevalence of complementary and alternative medicine use in the general population in the Czech Republic. Forsch Komplementmed. 2016;23(1):22–28. doi: 10.1159/000443712. [DOI] [PubMed] [Google Scholar]
- 16.University Hospital Hradec Kralove [webpage on the Internet] Czech-Chinese Centre of Traditional Chinese Medicine. 2017. [Accessed February 5, 2017]. Available from: https://www.fnhk.cz/tcm.
- 17.Czech Medical Acupuncture Society of the Czech Medical Association of J. E. Purkyně [webpage on the Internet] Akupunktura a přidružené techniky. 2017. [Accessed February 5, 2017]. Available from: http://www.akupunktura.cz/cs/akupunktura-a-pridruzene-techniky.
- 18.Headache Classification Subcommittee of the International Headache Society (HIS) The international classification of headache disorders 3rd edition. Cephalalgia. 2013;33(9):629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Xue CC, Helme R, et al. Acupuncture for frequent migraine: a randomized, patient/assessor blinded, controlled trial with one-year follow-up. Evid Based Complement Alternat Med. 2015;2015:14. doi: 10.1155/2015/920353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization . Standard Acupuncture Nomenclature. Manila, Philippines: World Health Organization; 1993. [Google Scholar]
- 21.Wuxi Jiajian Medical Instrument Co. Ltd [webpage on the Internet] Acupuncture Rational (22–24) 2017. [Accessed February 14, 2017]. Available from: http://jiaji-anchina.en.made-in-china.com/
- 22.Linde K, Allais G, Brinkhaus B, et al. Acupuncture for migraine prophylaxis. Cochrane Database Syst Rev. 2009;1:CD001218. doi: 10.1002/14651858.CD001218.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vincent C, Lewith G. Placebo controls for acupuncture studies. J R Soc Med. 1995;88:199–202. [PMC free article] [PubMed] [Google Scholar]
- 24.Langevin HM, Wayne PM, MacPherson H, et al. Paradoxes in acupuncture research: strategies for moving forward. Evid Based Complement Alternat Med. 2011;2011:180805. doi: 10.1155/2011/180805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72(1–2):95–97. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 26.WHO Collaborating Centre for Drug Statistics Methodology [webpage on the Internet] ATC/DDD Index 2017. 2017. [Accessed February 7, 2017]. Available from: https://www.whocc.no/atc_ddd_index/
- 27.Tfelt-Hansen P, Block G, Dahlöf C, et al. Guidelines for controlled trials of drugs in migraine: second edition. Cephalalgia. 2000;20(9):765–786. doi: 10.1046/j.1468-2982.2000.00117.x. [DOI] [PubMed] [Google Scholar]
- 28.Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56(6 suppl 1):S20–S28. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
- 29.MacPherson H, Altman DG, Hammerschlag R, et al. Revised Standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. PLoS Med. 2010;7:E1000261. doi: 10.1371/journal.pmed.1000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Consort [webpage on the Internet] Transparent Reporting of Trials. 2017. [Accessed June 15, 2017]. Available from: http://www.consort-statement.org/
- 31.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 32.Diener HC, Matias-Guiu J, Hartung E, et al. Efficacy and tolerability in migraine prophylaxis of flunarizine in reduced doses: a comparison with propranolol 160 mg daily. Cephalalgia. 2002;22:209–221. doi: 10.1046/j.1468-2982.2002.t01-1-00309.x. [DOI] [PubMed] [Google Scholar]
- 33.Brandes JL, Saper JR, Diamond M, et al. Topiramate for migraine prevention: a randomized controlled trial. JAMA. 2004;291:965–973. doi: 10.1001/jama.291.8.965. [DOI] [PubMed] [Google Scholar]
- 34.Silberstein SD. Preventive migraine treatment. Continuum (Minneap Minn). Review. Headache. 2015;21(4 Headache):973–989. doi: 10.1212/CON.0000000000000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Silberstein SD, Neto W, Schmitt J, Jacobs D, MIGR-001 Study Group Topiramate in migraine prevention: results of a large controlled trial. Arch Neurol. 2004;61(4):490–495. doi: 10.1001/archneur.61.4.490. [DOI] [PubMed] [Google Scholar]
- 36.Klapper J. Divalproex sodium in migraine prophylaxis: a dose- controlled study. Cephalalgia. 1997;17(2):103–108. doi: 10.1046/j.1468-2982.1997.1702103.x. [DOI] [PubMed] [Google Scholar]
- 37.Gray RN, Goslin RE, McCrory DC, Eberlein K, Tulsky J, Hasselblad V. Drug Treatments for the Prevention of Migraine Headache. Agency for Health Care Policy and Research; Rockville, MD: 1999. (Technical Reviews No 2.3). [PubMed] [Google Scholar]
- 38.Linde K, Streng A, Jürgens S, et al. Acupuncture for patients with migraine: a randomized controlled trial. JAMA. 2005;293(17):2118–2125. doi: 10.1001/jama.293.17.2118. [DOI] [PubMed] [Google Scholar]
- 39.Facco E, Liguori A, Petti F, et al. Traditional acupuncture in migraine: a controlled, randomized study. Headache. 2008;48(3):398–407. doi: 10.1111/j.1526-4610.2007.00916.x. [DOI] [PubMed] [Google Scholar]