Abstract
The purpose of the study was to examine the effects of a school-based cross-training program on body mass index (BMI), attitudes toward physical activity (ATPA), and physical activity (PA) levels of children in the 4th and 5th grades. Children (N = 118) were divided into control (n = 60) and experimental (n = 58) groups based on class availability. While the control group continued academic classes as usual, the experimental group participated in cross-training involving resistance training (RT), calisthenics, and stretching twice a week for 10 weeks. Pre- and post-intervention measures included height, mass, ATPA, and PA. BMI was calculated and ATPA and PA levels were assessed via questionnaire. The groups did not differ significantly (p > .05) for either pre- or post-intervention regarding BMI, ATPA, and PA. However, BMI and PA levels significantly increased over time for both groups (p ≤ .05). Overall, cross-training in a school setting may be a safe and enjoyable option for physical activity participation. BMI and PA increases were likely the result of the natural growth process and seasonal weather pattern changes, respectively. Nevertheless, the cross-training did not detract from PA levels and may have led to an overall increase in PA levels. As subdomain analyses revealed decreased attitude toward health and fitness in the experimental group, shorter programs involving RT with various protocols are recommended.
Keywords: Fitness, pediatric, motivation, resistance exercise, weight lifting
INTRODUCTION
According to National Health and Nutrition Examination Survey (NHANES) data, only 42% of children in the U.S. participate in the recommended daily amount of moderate-to-vigorous physical activity (MVPA) (32,33). This lack of MVPA increases health risks. Children who do not participate in recommended levels of PA are at greater risk for developing cardiovascular disease (CVD) risk factors including increased blood pressure, insulin resistance, and triglycerides (3,15,23,25). Further, in 2011 and 2012, almost one third of children and adolescents in the U.S. from ages 2 to 19 years were overweight or obese (BMI ≥ 85th percentile) (21).
While numerous methods of increasing PA levels in children have been researched with varying degrees of success (14,34,36), the impact of a resistance-based program on total PA levels (e.g., ambulatory PA) is unknown. In the past, resistance training (RT) as a mode of exercise for children was ill-advised due to perceived safety issues (11). However, a better understanding of RT programming and safety issues by several organizations and publications concerned with pediatric well-being now supports the use of RT as a mode of exercise for children (1,7,11,18,31,35).
RT as an exercise mode for children is attractive for several reasons. Aside from the well-evidenced benefit of increased muscular strength (12) and motor unit recruitment (7), RT has been shown to reduce body fat, body mass index (BMI), and waist-to-hip ratio in children (5), as well as improving insulin-sensitivity in overweight boys (28). RT programs employ PA patterns that mimic the more sporadic nature of children (4) who often have shorter attention spans (19,22). Heavier children, especially, may enjoy the more diverse and strength-based nature of RT as they may not be able to participate in constant aerobic activity (30) but are simultaneously stronger than their lighter counterparts. Another benefit of RT for children is novelty, which may produce greater learning and mastery in students as shown in education psychology literature (2). The effects of novelty and similarity to natural PA patterns may have a positive impact on children’s attitudes toward PA (ATPA), an important factor in PA participation (27). Historically, school-based programs have focused on aerobic activities (11). However, including RT in school-based programs allows for cross-training that may intrigue children by adding variety to the typical physical education (PE) class.
PA levels are alarmingly low in children contributing to numerous health problems. As such, methods to increase the PA of children are continually sought. Cross-training exercise programs including RT have produced favorable results, but their impact on total PA is unknown. Because RT simulates natural patterns of PA in children and carries the motivational benefit of novelty, adding RT to an exercise regime for children may improve children’s ATPA and, ultimately, overall PA levels. Therefore, the purpose of the current study is to examine the effect of a cross-training program with an RT emphasis on BMI, ATPA, and PA levels of 4th and 5th grade children.
METHODS
Participants
Children (N = 118) from an elementary school in the southeast U.S. volunteered to participate in the study. The sample included boys (n = 56) and girls (n = 62) in the 4th and 5th grades (age 9.5 ± 0.6 yrs) who were apparently healthy. Participants were divided into a control group (3 classes) and an intervention group (3 classes) based on teacher availability. Approximately 20 students were in each class yielding 58 students in the exercise intervention group and 60 students in the control group. Before participating, all students completed an assent form and their parents all completed a consent form.
Protocol
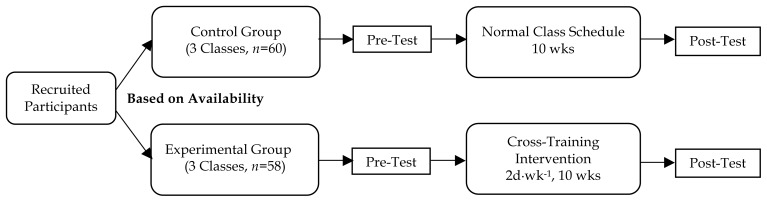
Approval for the study was granted by the Institutional Review Board, principal, and superintendent prior to data collection. Prior to the exercise intervention, each child’s height and mass were measured, from which BMI was calculated. His or her PA and ATPA levels were also assessed via self-report questionnaires. A 2-session accommodation period to RT was provided for the experimental group 1 week prior to the intervention to familiarize the students with proper lifting technique and program goals. Initial resistance for RT machines was also determined for each student so that he or she could lift at least 8 but less than 15 repetitions on any given machine. The classes met at separate times for these sessions and for the intervention. After the 10-week intervention, height, mass, PA, and ATPA were assessed in the same manner as the pre-test (Figure 1).
Figure 1.
General experimental design. Cross-training intervention included resistance training, calisthenics, and stretching. The intervention was in addition to the students’ regular PE class.
Body mass and height: Participants wore typical school clothing for measurements, but were asked to remove their shoes. Body mass was measured to the nearest tenth of a kilogram using a Seca electronic scale (Model #770). Height was measured with students standing as straight as possible with their heels together touching the back of the stadiometer. As they stared straight ahead, the headplate was lowered to the crown of their head. Measurements were taken to the nearest tenth of a centimeter using a Seca stadiometer (Model #222). These measurements were used to calculate BMI (kg·m−2).
PA questionnaire: The validated PA Questionnaire for Older Children (PAQC) (9) was used to measure general PA levels. The questionnaire has demonstrated a weighted mean validity of .39, along with a 1-week test-retest reliability of .79 (26). The PAQC consists of 10 questions employing checklist, Likert, and open-ended questions about primarily athletic activities during PE, lunch, recess, and time outside of school. For example, one question reads, “In the last 7 days, on how many days right after school, did you do sports, dance, or play games in which you were very active?” The composite score can range from 1 to 5 with 1 representing very low PA participation and 5 representing very high PA participation throughout the week. For a detailed understanding of the questionnaire, see Kowalski et al., 2004 (16).
Children’s ATPA Inventory (CATPAI): The Revised CATPAI (27) was developed to measure ATPA in children. The inventory has demonstrated construct validity and a 2-week test-retest reliability of .71 (27). Among the reasons to participate in PA, the Revised CATPAI focuses on seven subdomains, asking the children for their opinions on certain ideas representing each subdomain. For example, to assess the health and fitness subdomain, children are asked how they feel about the following idea: “taking part in physical activities to make your health better and get your body in better condition”. The subdomain is assessed via a 5-point Likert scale with five bipolar adjective word pairs (e.g., “good” versus “bad”). The other subdomains of social continuation, social growth, pursuit of vertigo, aesthetic experience, catharsis, and ascetic experience are evaluated likewise. Participants’ scores range from very poor ATPA (1) to very good ATPA (5) by subdomain and for the entire questionnaire. For a detailed understanding of the inventory, see Schutz et al., 1985 (27).
RT equipment: HOIST® KL machines, which are designed specifically for use with children, were used in a circuit fashion for the RT intervention. Upper body machines included the seated dip, chin-up, mid row, chest press, and shoulder press. Lower body machines included the squat press and seated leg press.
The experimental group met twice a week on Tuesdays and Thursdays for 10 weeks while the control group continued with their normal academic day. The intervention did not take the place of the students’ regular PE class. Exercise sessions began with a brief warm-up including aerobic exercise and ended with an aerobic cool-down as well. Both the warm-up and cool-down lasted 5–10 minutes. Every session allowed for the rotation of the children through 20 stations where they spent 45 seconds exercising and 30 seconds of rest for a total time of approximately 30 minutes. Two staff members monitored and encouraged the children, prompting them to begin and end at each station.
The setup of the fitness room included the HOIST® KL Circuit RT equipment interspersed with 13 other callisthenic and stretching stations for the 20 stations to ensure full class participation. The calisthenics included marching, lateral hops, step ups, jumping jacks, supine back extensions, Dance Dance Revolution® (two stations), abdominal crunches, biking, and treadmill stations. The stretching stations included stretches for the hamstrings, quadriceps, and hip adductors.
The training protocol was developed using age-appropriate guidelines (5, 8). On RT equipment, children completed 8 to 15 repetitions with proper form. When a child was able to complete more than 15 repetitions in a controlled manner, he or she increased the resistance on the machine. For calisthenics, children were encouraged to do as many repetitions as possible in the allotted 45 seconds or a higher intensity on the treadmill and bike to continually provide sufficient overload.
Children in the exercise intervention tracked their progress in a training log including the date, selected resistance, and number of repetitions completed. For stations that did not include resistance machines, the children checked off stretching exercises and noted bike/treadmill speed or number of repetitions of calisthenics completed. Staff members checked the children’s logs daily to ensure children were properly documenting and progressing in their exercises.
Statistical Analysis
Descriptive statistics were calculated for all study variables. Two-way RMANOVAs, with group (i.e., experimental and control) as a between-subjects factor and time (i.e., pre-test and post-test) as a within-subjects factor, were conducted for BMI, composite PAQC scores, and both composite and subdomain CATPAI scores to assess statistical significance. An alpha level of .05 was set a priori. Data analyses were conducted using SPSS® Version 16 (SPSS, Inc., Chicago, IL).
RESULTS
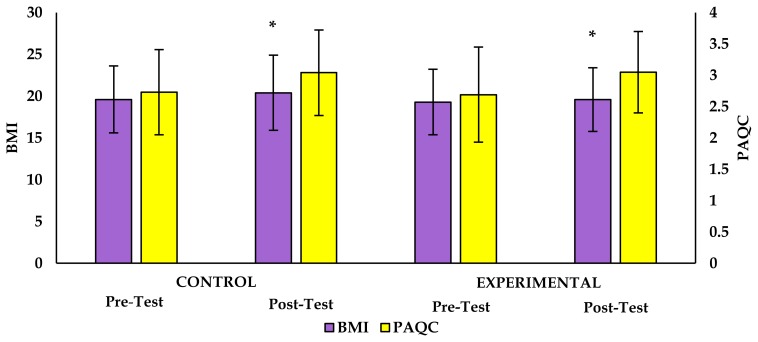
A total of 118 children, with an average age of 9.5 ± 0.6 years, volunteered to participate in this study. Complete data for all variables were available for only 109 participants due to student absences on pre- and post-testing days. Table 1 provides descriptive statistics for height and body mass. Figure 2 provides a comparison between pre-test and post-test scores for BMI and PAQC measures and Table 2 provides descriptive statistics for CATPAI scores.
Table 1.
Descriptive statistics for height and body mass.
| Height (cm) | Mass (kg) | ||||
|---|---|---|---|---|---|
| Group | Pre | Post | Pre | Post | |
| Control | M | 145.4 | 146.9 | 42.0 | 44.4 |
| SD | 6.3 | 6.5 | 10.4 | 12.1 | |
| n | 56 | 58 | 56 | 58 | |
| Experimental | M | 141.4 | 142.7 | 39.0 | 40.3 |
| SD | 7.8 | 7.9 | 10.8 | 11.1 | |
| n | 56 | 58 | 56 | 58 | |
Note. Unequal sample sizes are due to student absences for the pre- and post- test.
Figure 2.
A comparision of the control and experimental groups on body mass index (BMI) and reported physical activity (PAQC) over the intervention. Bars represent means ± SDs. * Denotes a significant increase from pre-test, p≤.05.
Table 2.
Descriptive statistics for CATPAI scores.
| Group | Pre-test | Post-test | |
|---|---|---|---|
| Control (n = 55) | M | 4.02 | 4.09 |
| SD | 0.56 | 0.5 | |
| Experimental (n = 54) | M | 3.88 | 3.88 |
| SD | 0.53 | 0.52 |
The main effect of time was significant for BMI and PAQC scores (BMI: H-F p = .03, η2 = .04, obs. power = .58; PAQC: H-F p < .001, η2 = .29, obs. power = 1.00), but not for CATPAI scores (H-F p = .46, η2 = .01, obs. power = .12), with only the BMI and PAQC scores increasing from pre-test to post-test. The main effect of group was not significant for any measures (BMI: p = .45, η2 = .01, obs. power = .12; PAQC: p = .94, η2 = .00, obs. power = .05; CATPAI: p = .05, η2 = .04, obs. power = .50). Similarly, interaction effects were not significant for any of the dependent variables (BMI: H-F p= .26, η2 = .01, obs. power = .20; PAQC: H-F p = .65, η2 = .00, obs. power = .07; CATPAI: H-F p = .46, η2 = .01, obs. power = .11). However, CATPAI subdomain analyses revealed a significantly lower score in the health and fitness subdomain for the experimental group compared to the control group over time (p= .007, η2 = .07, obs. power = .78). All other subdomain interactions were not significant (p>.05).
DISCUSSION
As RT has increased in popularity as an exercise mode for children, understanding the effects of a resistance-based training regimen on various health outcomes and behaviors is important. The current study showed that BMI and PA increased for children in both the control and cross-training intervention groups, but ATPA did not change. To our knowledge, these are the first published data on the effects of a resistance-based cross-training intervention on ATPA and PA levels of elementary school children.
Participants in both the control group and experimental group increased in height and body mass (Table 1). Increases in BMI in 10 year old children are common. Treuth et al. studied the effect RT had on intra-abdominal fat in obese, pre-pubescent girls and found no significant impact (32). However, similar to the current study, both groups significantly increased in height and mass, leading to an increase in BMI (see Figure 2). Even though the Treuth et al. study only included girls, as opposed to the current study which included both boys and girls, and assuming the children in both studies were of pre-pubertal age, the growth process was likely unaltered by the sex difference in the samples. While cross-training may play a role in the fitness of children, its ability to reduce weight status and diseases thereof based on BMI in children is still in question.
Children’s ATPA did not differ by time (p = .56) or group (p = .50) in this study (see Table 2). This finding was unexpected given the evidence that McGuigan et al. provided showing that RT was positively viewed by children (19). Other studies have also found an increase in children’s ATPA and PA levels after exposure to PA-promoting media (14,34). Although the experimental group did have a favorable ATPA pre- (3.88) and post-intervention (3.88), the intervention was hypothesized to impact and improve that level.
The current study, however, is the first known to have assessed the impact of a cross-training RT intervention on children’s ATPA. Although the cross-training program did not affect overall attitude, further RMANOVAs were conducted on each ATPA subdomain. Interaction tests (of group and time) were not significant (p > .05) for any domain except the health and fitness subdomain (p = .007). The children’s average score for the health and fitness subdomain increased in the control group (4.63 to 4.69), but decreased in the experimental group (4.64 to 4.40), indicating a less positive view towards health and fitness.
One possible explanation for this phenomenon is that children may become bored with the repetitive nature of RT. Although the staff that worked with the children encouraged them throughout their training, the children were noticeably less excited towards the end of the program. Work by Cowan et al. involving children’s ATPA found similar results (8). Fifth through eighth graders (N = 149) completed an 8-week RT program, yet their ATPA decreased in both the experimental and control groups. This decrease in children’s ATPA led Cowan et al. to conclude that redundancy, lack of student choice, and, ultimately, boredom were due to the repetitive nature of RT. Although boredom may be a possible explanation for a decrease in the subdomain, the subdomain still remained high in the experimental group (4.40 out of 5).
Overall PA levels increased for both groups (Figure 2). The higher full sample post-test PA levels may be accounted for by the seasonal changes throughout the intervention with the administration of the pre-test in January (36°F avg) and of the post-test in April (57°F avg) for the current study. Hagger et al. studied seasonal variations in PA levels of elementary school children and documented that the average time children spent performing MVPA in summer months (90 min) was significantly higher than in winter months (68 min) (13). Similarly, Loucaides et al. documented that boys and girls accumulate more steps on average during the summer months (15,471 ± 5,116) than in the winter months (13,429 ± 4,340) (17). Both author groups attributed the difference in PA levels to longer periods of daylight and ideal weather in the summer, but not in the winter.
The interaction of time and group was not significant (p = .65) in this study. Children who participated in the cross-training did not increase their PA levels more than children who did not participate in cross-training. Because the PAQC is not specific regarding flexibility and RT exercises, there is the potential that the children did not consider a significant portion of the intervention when completing the questionnaire, meaning the questionnaire mainly measured their PA outside of the intervention. As this study was the first to include the impact of a cross-training program on overall PA levels, no comparisons to other studies including RT are available. However, Watson et al. found in their meta-analysis that classroom-based exercise interventions did not affect children’s PA levels (37). Similarly, Shephard et al. found that the amount of PE time in school did not significantly impact children’s PA outside of school (29). Nevertheless, students who participated in more PE accrued more total PA than those students who participated in less PE. Similarly, a study by Morgan et al. demonstrated an increased step count for the least, moderate, and most active children (1,700, 1,100, and 2,500 respectively) on days when PE was offered in school than days when no PE was offered (20). Furthermore, the children did not participate in compensatory PA on days when PE was not offered. Accelerometry data collected by Dale et al. also demonstrated that children did not compensate for their low activity by increasing their PA after an inactive school day, but they had significantly higher PA levels after active school days than after the inactive school days (10).
In light of the studies on compensatory PA, the finding that the cross-training intervention did not increase PA should not necessarily be viewed negatively. By the end of the program, children in the experimental group had similar average reported PAQC scores (3.05) to the control group (3.03). However, the questionnaire likely did not account for the RT component of the cross-training in which the experimental group participated because there were no RT-specific questions on the PAQC. As such, experimental group participants possibly accrued more total PA than the children in the control group because the intervention did not displace other PA. This is important for children in this generation who tend to receive stimulation through phones, televisions, computers, and similar electronics instead of PA after school (6,24). Therefore, any additional cross-training included in a school day, in PE or elsewhere, can help increase overall PA levels of children.
Including a variety of RT modes (i.e. bands, dumbells, etc.), as opposed to solely employing resistance machines would likely prevent children’s stagnating interest in a cross-training program. Future studies in this area may benefit from additional supervisors (better student to supervisor ratio) to ensure proper use of equipment and completion of each exercise. Unlike the current study, supervisors should be unknown by the children so as to eliminate any bias that may result from previous experience. Also, asking the supervisors, rather than the children, to track progress would improve the accuracy of reported exercise. Regarding BMI, measuring body composition with tools such as bioelectrical impedance analysis devices or skin-fold calipers may clarify the source of observed weight gain in both the intervention and control groups. When measuring PA, objective measures such as pedometers or accelerometers would improve the accuracy of this assessment. A final limitation of the study was the lack of true random assignment. Future studies would benefit from dividing the groups on an individual basis instead of by class.
Overall, the cross-training was completed without injury and was a safe mode of exercise for the children. Thus, cross-training in a school setting can be an option for physical activity participation. Though BMI differences between groups did not change significantly over the course of the study, significant increases for both groups may be due to the growth common for children. Children’s total ATPA was unaffected by the protocol used in the current study although the experimental group decreased in the health and fitness subdomain, likely due to boredom. As such, implementing a short RT-based, cross-training section in a PE or health-related class could peak children’s interest in this mode of training without inducing boredom. Increases in PA levels most likely resulted from a change to more clement weather by the end of the study. The experimental group, though, may have accrued additional PA time because the intervention PA was not accounted for in the questionnaire. Future studies should include greater variation in training modalities and program structure to enhance participant interest as well as more precise, objective measures of PA.
ACKNOWLEDGEMENTS
The authors would like to thank the Center for Physical Activity and Health in Youth for their financial support of this project.
REFERENCES
- 1.American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. Ninth Edition. Philadelphia: LWW; 2014. [DOI] [PubMed] [Google Scholar]
- 2.Ames C. Classrooms: Goals, structures, and student motivation. J Educ Psychol. 1992;84(3):261–271. [Google Scholar]
- 3.Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, et al. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study) Lancet. 2006;368(9532):299–304. doi: 10.1016/S0140-6736(06)69075-2. [DOI] [PubMed] [Google Scholar]
- 4.Bailey RC, Olson J, Pepper SL, Porszasz J, Barstow TJ, Cooper DM. The level and tempo of children’s physical activities: an observational study. Med Sci Sports Exerc. 1995;27(7):1033–1041. doi: 10.1249/00005768-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Benson AC, Torode ME, Fiatarone Singh MA. The effect of high-intensity progressive resistance training on adiposity in children: a randomized controlled trial. Int J Obes. 2008;32(6):1016–1027. doi: 10.1038/ijo.2008.5. [DOI] [PubMed] [Google Scholar]
- 6.Committee on Public Education. Children, adolescents, and television. Pediatrics. 2001;107(2):423–426. doi: 10.1542/peds.107.2.423. [DOI] [PubMed] [Google Scholar]
- 7.Council on Sports Medicine and Fitness. Strength training by children and adolescents. Pediatrics. 2008;121(4):835–840. doi: 10.1542/peds.2007-3790. [DOI] [PubMed] [Google Scholar]
- 8.Cowan W, Chandler P, Bolen Y, Phillips D. Attitude toward physical activity as influenced by motivational climate [Internet] [Google Scholar]
- 9.Crocker PR, Bailey DA, Faulkner RA, Kowalski KC, McGrath R. Measuring general levels of physical activity: preliminary evidence for the Physical Activity Questionnaire for Older Children. Med Sci Sports Exerc. 1997;29(10):1344–1349. doi: 10.1097/00005768-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Dale D, Corbin CB, Dale KS. Restricting opportunities to be active during school time: do children compensate by increasing physical activity levels after school? Res Q Exerc Sport. 2000;71(3):240–248. doi: 10.1080/02701367.2000.10608904. [DOI] [PubMed] [Google Scholar]
- 11.Faigenbaum AD, Kraemer WJ, Blimkie CJR, Jeffreys I, Micheli LJ, Nitka M, et al. Youth resistance training: updated position statement paper from the national strength and conditioning association. J Strength Cond Res. 2009;23(5 Suppl):S60–S79. doi: 10.1519/JSC.0b013e31819df407. [DOI] [PubMed] [Google Scholar]
- 12.Falk B, Tenenbaum G. The effectiveness of resistance training in children. A meta-analysis. Sports Med Auckl NZ. 1996;22(3):176–186. doi: 10.2165/00007256-199622030-00004. [DOI] [PubMed] [Google Scholar]
- 13.Hagger M, Cale L, Almond L, Krüger A. Children’s physical activity levels and attitudes towards physical activity. Eur Phys Educ Rev. 1997;3(2):144–164. [Google Scholar]
- 14.Huhman ME, Potter LD, Duke JC, Judkins DR, Heitzler CD, Wong FL. Evaluation of a national physical activity intervention for children. Am J Prev Med. 2007;32(1):38–43. doi: 10.1016/j.amepre.2006.08.030. [DOI] [PubMed] [Google Scholar]
- 15.Kavey R-EW. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107(11):1562–1566. doi: 10.1161/01.cir.0000061521.15730.6e. [DOI] [PubMed] [Google Scholar]
- 16.Kowalski KC, Crocker P, Donen RM, Honours B. The physical activity questionnaire for older children (PAQC) and adolescents (PAQ-A) manual. 2004 [Google Scholar]
- 17.Loucaides CA, Chedzoy SM, Bennett N. Pedometer-assessed physical (ambulatory) activity in cypriot children. Eur Phys Educ Rev. 2003;9(1):43–55. [Google Scholar]
- 18.Malina RM. Weight training in youth-growth, maturation, and safety: an evidence-based review. Clin J Sport Med. 2006;16(6):478–487. doi: 10.1097/01.jsm.0000248843.31874.be. [DOI] [PubMed] [Google Scholar]
- 19.McGuigan MR, Tatasciore M, Newton RU, Pettigrew S. Eight weeks of resistance training can significantly alter body composition in children who are overweight or obese. J Strength Cond Res. 2009;23(1):80–85. doi: 10.1519/jsc.0b013e3181876a56. [DOI] [PubMed] [Google Scholar]
- 20.Morgan CF, Beighle A, Pangrazi RP. What are the contributory and compensatory relationships between physical education and physical activity in children? Res Q Exerc Sport. 2007;78:407–412. doi: 10.1080/02701367.2007.10599440. [DOI] [PubMed] [Google Scholar]
- 21.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ozmun JC, Mikesky AE, Surburg PR. Neuromuscular adaptations following prepubescent strength training. Med Sci Sports Exerc. 1994;26(4):510–514. [PubMed] [Google Scholar]
- 23.Raitakan OT, Porkka KVK, Taimela S, Telama R, Räsänen L, Vllkari JS. Effects of persistent physical activity and inactivity on coronary risk factors in children and young adults the cardiovascular risk in young Finns study. Am J Epidemiol. 1994;140(3):195–205. doi: 10.1093/oxfordjournals.aje.a117239. [DOI] [PubMed] [Google Scholar]
- 24.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282(16):1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 25.Sallis JF, Patterson TL, Buono MJ, Nader PR. Relation of cardiovascular fitness and physical activity to cardiovascular disease risk factors in children and adults. Am J Epidemiol. 1988;127(5):933–941. doi: 10.1093/oxfordjournals.aje.a114896. [DOI] [PubMed] [Google Scholar]
- 26.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71(sup2):1–14. doi: 10.1080/02701367.2000.11082780. [DOI] [PubMed] [Google Scholar]
- 27.Schutz RW, Smoll FL, Carre F, Mosher R. Inventories and norms for children’s attitudes toward physical activity. Res Q Exerc Sport. 1985;56(3):256–265. [Google Scholar]
- 28.Shaibi GQ, Cruz ML, Ball GDC, Weigensberg MJ, Salem GJ, Crespo NC, et al. Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Med Sci Sports Exerc. 2006;38(7):1208–1215. doi: 10.1249/01.mss.0000227304.88406.0f. [DOI] [PubMed] [Google Scholar]
- 29.Shephard RJ, Jéquier JC, Lavallée H, La Barre R, Rajic M. Habitual physical activity: effects of sex, milieu, season and required activity. J Sports Med Phys Fitness. 1980;20(1):55–66. [PubMed] [Google Scholar]
- 30.Sothern MS, Loftin JM, Udall JN, Suskind RM, Ewing TL, Tang SC, et al. Inclusion of resistance exercise in a multidisciplinary outpatient treatment program for preadolescent obese children. South Med J. 1999;92(6):585–592. doi: 10.1097/00007611-199906000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Sothern MS, Loftin JM, Udall JN, Suskind RM, Ewing TL, Tang SC, et al. Safety, feasibility, and efficacy of a resistance training program in preadolescent obese children. Am J Med Sci. 2000;319(6):370–375. doi: 10.1097/00000441-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Treuth MS, Hunter GR, Figueroa-Colon R, Goran MI. Effects of strength training on intra-abdominal adipose tissue in obese prepubertal girls. Med Sci Sports Exerc. 1998;30(12):1738–1743. doi: 10.1097/00005768-199812000-00013. [DOI] [PubMed] [Google Scholar]
- 33.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 34.Tsorbatzoudis H. Evaluation of a school-based intervention programme to promote physical activity: an application of the theory of planned behavior. Percept Mot Skills. 2005;101(3):787–802. doi: 10.2466/pms.101.3.787-802. [DOI] [PubMed] [Google Scholar]
- 35.U.S. Department of Health and Human Services. 2008 physical activity guidelines for Americans. 2008. [Google Scholar]
- 36.Van Sluijs EMF, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007;335(7622):703. doi: 10.1136/bmj.39320.843947.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Watson A, Timperio A, Brown H, Best K, Hesketh KD. Effect of classroom-based physical activity interventions on academic and physical activity outcomes: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2017;14 doi: 10.1186/s12966-017-0569-9. [DOI] [PMC free article] [PubMed] [Google Scholar]