Abstract
Objectives
Reporting of adverse and near miss events are essential to identify system-level targets to improve patient safety. Resident physicians historically report few events despite their role as front-line patient care providers. We sought to evaluate barriers to adverse event reporting in an effort to improve reporting. Our main outcomes were: resident attitudes about event reporting, and the frequency of event reporting before and after interventions to address reporting barriers.
Methods
We surveyed first year residents regarding barriers to adverse event reporting, and used this input to construct a fishbone diagram listing barriers to reporting. Barriers were addressed and resident event reporting was compared before and after efforts were made to reduce obstacles to reporting.
Results
First year residents (97%) recognized the importance of submitting event reports, however the majority (85%) had not submitted an event report in the first 6 months of residency. Only 7% of residents specified that they had not witnessed an adverse event in 6 months, while one third had witnessed 10 or more events. The main barriers were: lack of knowledge about how to submit events (38%) and lack of time to submit reports (35%). After improving resident education around event reporting and simplifying the reporting process, resident event reporting increased 230% (68 to 154 annual reports, p=0.025).
Conclusions
We were able to significantly increase resident event reporting by educating residents about adverse events and near misses, and addressing the primary barriers to event reporting. Moving forward, we will continue annual resident education about patient safety, focus on improving feedback to residents who submit reports, and empower senior residents to act as role models to junior residents in patient safety initiatives.
Background
As front-line workers who dedicate as many as 80 hours per week to patient care, residents are uniquely positioned to identify adverse events and propose solutions to these patient safety issues. Physicians have historically been infrequent reporters of adverse events due to time constraints, cultural factors, training, and lack of knowledge around event reporting.(1–3) Physician reported events have been shown to make up only 1–2% of all reported events.(1, 2) Based on recommendations by the Institute of Medicine report Resident duty hours: Enhancing sleep, supervision and safety, the Accreditation Council for Graduate Medical Education (ACGME) has made recommendations regarding the development of future physicians.(4, 5) The ACGME emphasizes that residents need to know how to identify and report adverse events.(6) In addition, residents must learn how to implement best practices to identify patient safety events and incorporate knowledge from adverse events/near misses to improve the safety of medical care.(7) With increasing emphasis on resident participation in quality improvement work, and the goal of developing a generation of physicians focused on patient safety,(8, 9) it is imperative that residents contribute to event reporting. Therefore, many organizations are motivated to improve resident event reporting.(10)
Previous studies have examined various methods to improve resident event reporting.(11, 12) The most common approach was resident education. A one-time educational intervention was found to improve reporting from average of 2.5 per month to 19 per month in a group of internal medicine residents, however the increase in reporting was not sustainable over time.(11) On the other hand, the combination of resident education, quarterly discussions about ongoing quality improvement based on event reporting, and immediate feedback to residents who reported events, was found to sustainably improve anesthesia resident reporting from 0 reports quarterly to 28.(12) Another group demonstrated 5 fold improvement in rates of reporting in residents who were rewarded financially for reporting.(13) Interestingly, no improvement in reporting was found in anesthesia or emergency medicine residents. The authors also did not evaluate the long term sustainability of this intervention. Although financial incentives may improve event reporting in the short term, they are unlikely to result in sustained physician reporting.(14) Others have utilized quantitative goals to increase resident reporting. The expectation for a group of internal medicine residents was that they report one event per rotation and only 6% of residents met the goal.(11) Female and second year residents were found to be most likely to report events. Simply telling residents they are expected to report a specific number of events may take the focus away from the patient and the implications of near misses and adverse outcomes. Having residents fill a quota of reported events may thereby lead to poor quantity and quality of reported events.
Many of these previous studies have focused on changing event reporting at a departmental level, and have not implemented hospital wide resident education programs to improve event reporting.(11, 14, 15) Our aims were to assess resident attitudes about event reporting hospital wide, and to identify perceived barriers to reporting. We sought to evaluate changes in resident event reporting after eliminating resident identified barriers to reporting.
Methods
The study was undertaken in three phases: pre-intervention evaluation of barriers to resident event reporting, intervention based on the pre-intervention findings, and post-intervention assessment of resident event reporting. The primary outcome was the number of patient safety events reported before and after implementation of barrier reduction strategies. The study was exempt from IRB approval as it deemed a quality improvement project.
Resident Attitudes and Barriers to Reporting
We first sought to identify barriers to resident event reporting. We surveyed first year residents at a single academic teaching institution regarding resident reporting of patient safety events. We targeted all 94 first year residents at our institution. The survey was developed by an interdisciplinary team of quality and safety experts and was not validated or piloted. Surveys were distributed at the beginning of the First Annual Patient Safety Orientation, which was a mandatory event (January 2015) for all first year residents regardless of specialty. The surveys were anonymous and did not include identifiable information. The survey sought to identify resident attitudes about event reporting, reasons for not submitting events, and the number of events residents had witnessed in the first six months of training.
Our institution has a robust Resident Quality and Safety Council (RQSC). The council is comprised of residents from every specialty at our institution and focuses on improving quality and safety within and across departments, educating residents and medical students about quality and safety, and acting as conduit of information between residents and hospital administration and other institutional quality and safety councils. Members participate in the Event Evaluation Team, Safety Committee, Quality Council, EPIC Superuser Group, RCA Committee, and the Interdisciplinary Model of Care Committee to name a few. This group of residents worked together to identify barriers to resident event reporting.
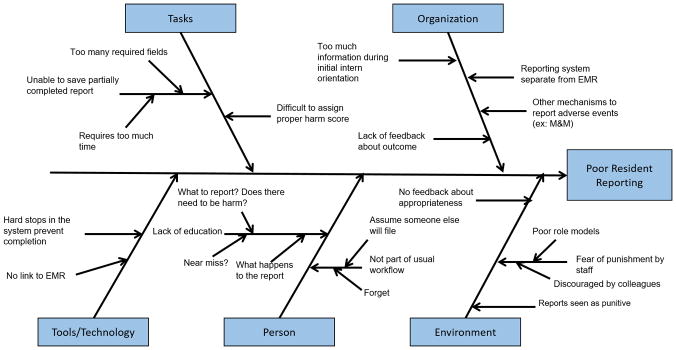
The RQSC utilized a fishbone diagram, which is a straightforward tool used to identify all contributing root causes for a specific problem. Causes for poor event reporting were categorized under the following headings: tasks, organization, tools/technology, person, and environment. None of the RQSC members were first year residents who completed the survey at the Patient Safety Orientation and data from that survey was not available when the fishbone diagram was constructed.
Improvement Work and Resident Reporting
We utilized the results of the resident surveys and the RQSC fishbone diagram to address specific barriers to event reporting. Specifically, we held the First Annual Patient Safety Orientation for first year residents. The event was planned by a multi-disciplinary team of physicians (faculty and residents) from diverse specialties as well as experts in quality improvement and patient safety including the Vice President of Quality and Safety and the Medical Director of Patient Safety. The four-hour event consisted of large group discussions about event reporting and small group sessions where residents worked with a facilitator to complete a root cause analysis. The event reporting discussion included a description of Just Culture, definitions of adverse events and near misses, the importance of reporting, instructions about how to submit events, and a summary of how reports are processed and how institutional processes are changed based on reports. While first year residents were surveyed at the beginning of this event, this information was not used to tailor the event, but rather to identify first year resident perceptions on event reporting.
We also revised the patient safety event reporting system by simplifying the data entry process and linking event reporting to the electronic medical record. The entry form was shortened dramatically to only include necessary information. Additionally, the reporting system was previously only accessible from the hospital intranet website. We linked the reporting system to the electronic medical record so that it can be accessed while reviewing a patient chart. We published an article on event reporting in the RQSC quarterly newsletter to further educate residents on the topic. These changes and education were all implemented simultaneously. Annual resident event reporting was analyzed in the three years prior to the Patient Safety Orientation and the year following the intervention.
Outcome Measures
The primary outcome of interest was the number of patient safety events reported before and after implementation of barrier reduction strategies. Annual resident event reporting was analyzed in the three years prior to the Patient Safety Orientation and the year following the intervention.
Statistical Analysis
Demographic data including specialty and gender was collected for residents attending the Patient Safety Orientation. Survey results were tallied in the following categories: resident attitudes, barriers to event reporting, and number of witnessed patient safety events. The number of patient safety events reported in the three years prior to the intervention and in the one year after the intervention were evaluated with a one sided t test. P values <0.05 were considered significant.
Results
A group of first year trainees (n=94) at a single academic institution were surveyed regarding their personal history with adverse event reporting and their attitudes regarding event reporting. Trainees from general medicine (17%), pediatrics (14%), emergency medicine (12%), general surgery (11%), and anesthesia (10%) comprised the majority of invited residents. The majority of residents were male (62%).
Resident Attitudes and Barriers to Reporting
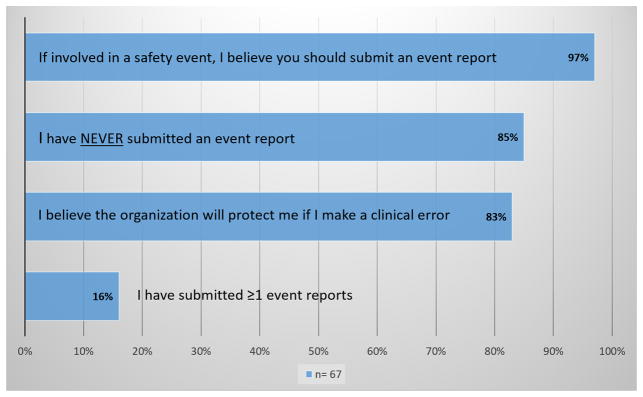
Of the 94 invited residents, 67 (71%) both attended the event and completed the survey. Figure 1 summarizes resident attitudes about event reporting. Almost all surveyed residents (97%) believed it was important to submit an event report if involved in a patient safety event. However, 85% reported they had not submitted an event report in the first 6 months of their training. Most residents (83%) did not fear punishment from the organization for clinical error on their part, therefore this does not appear to be a primary driver of poor reporting.
Figure 1.
Resident Attitudes About Event Reporting
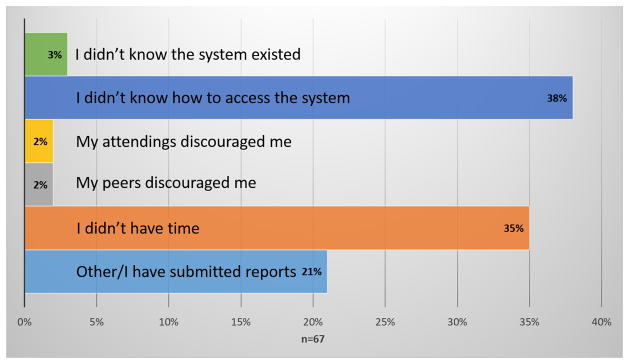
We also queried residents regarding reasons they were not submitting patient safety events. As demonstrated in Figure 2, the two major barriers to event reporting were lack of knowledge about how to submit events (38%) and lack of time (35%). Almost all residents (97%) were aware there was a system for event reporting. Discouragement or fear of retribution from peers or faculty was uncommonly cited as a barrier to event reporting (4%).
Figure 2.
Main reason I have not submitted an event report
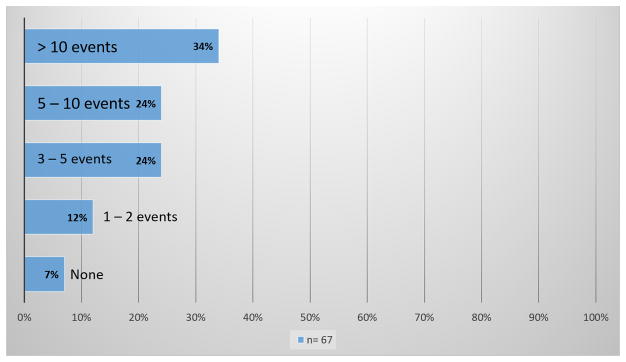
To gain a better understanding regarding residents’ ability to identify adverse events, residents were asked how many events they had witnessed in the first 6 months of their training that they considered reportable. One third of residents reported they had witnessed >10 events and 58% of residents witnessed >5 events over 6 months (Figure 3). Almost one tenth of residents (7%) reported that they had not witnessed any adverse events.
Figure 3.
How many events have you witnessed that could have been reported?
The fishbone diagram constructed by our Resident Quality and Safety Council is demonstrated in Figure 4. The RQSC found that the electronic reporting system was both difficult to access, time consuming, and contained questions that residents did not know how to answer (i.e. assigning harm scores). Furthermore, residents reported a lack of education about event reporting including how to report, what to report, and what happens with submitted reports. Residents cited a lack of time, assumption that others (nursing and other staff) would report, and lack of positive role models in their field as additional barriers to event reporting.
Figure 4.
Fishbone diagram - Barriers to submitting adverse event reports
Improvement Work and Resident Reporting
After implementing our improvement work, we noted an increase in the number of resident reported events. Over the 3 years prior to the changes an average of 68 events per year were reported by residents (61 in 2012, 68 in 2013, 76 in 2014). Following the interventions, there were 154 resident reported events in 2015. This change was significant with p value 0.025. A summary of the 2015 resident reported events is listed in Table 1. The most commonly reported events were related to medications (25%) or care coordination (24%). Thirty seven percent of reported events were near misses, which was a major focus of teaching during the Patient Safety Orientation.
Table 1.
Summary of resident reported events January – September 2015
| Resident Reported Events | N =154 n (%) |
|---|---|
| Event Type | |
| Medication | 39 (25) |
| Care coordination/Communication | 37 (24) |
| Error in assessment, diagnosis, monitoring | 15 (10) |
| Laboratory | 15 (10) |
| Imaging | 10 (6) |
| Non-surgical complications | 7 (5) |
| Surgical/Procedural complications | 7 (5) |
| Medical records/Patient identification | 6 (4) |
| Equipment/Devices | 4 (3) |
| Fall | 3 (2) |
| Other* | 11 (7) |
|
| |
| Harm Score | |
| Unsafe condition | 34 (22) |
| Near miss | 57 (37) |
| No harm evident | 17 (11) |
| Emotional distress or inconvenience | 13 (8) |
| Additional treatment required | 18 (12) |
| Temporary harm | 14 (9) |
| Permanent harm | 1 (1) |
| Death | 0 (0) |
Other: Exposures, Nutrition, Maternal, Behavioral Transfusions
Discussion
In summary, we found that residents understand the importance of reporting adverse events and near misses. However, first year residents cited lack of knowledge about how to report and lack of time as barriers to submitting event reports. After improving resident education and simplifying the reporting process, we found a significant increase in event reporting. Also, over one third of reports were near misses indicating that residents understand the importance of identifying areas for improvement even when harm does not reach the patient.
We found that 85% of first year residents had not reported an adverse event in the first 6 months of training. Those same residents reported having witnessed multiple adverse events during that time period with 58% having witnessed >5 events. If all of the 600 residents at our institution witness 5 events every 6 months, it would suggest that residents are witnessing thousands of events annually at our hospital alone. We are currently only capturing a small proportion of those events with our reporting system.
By improving resident education, we modestly improved resident reporting by 2-fold. We anticipate that going forward we will continue to see an increase in reporting over the next 3–5 years. We will continue to hold annual patient safety education events and as residents progress through their training they will pass their knowledge of event reporting to junior residents. Others have found an increase in event reporting after a single educational intervention, but the increase was not sustainable over time.(11) Therefore, we believe that ongoing training in patient safety is necessary to create a culture of patient safety and ensure ongoing reporting of near misses and adverse events.
We found that residents cited lack of time (35%) and lack of knowledge about how to submit events (38%) as the most common barriers to event reporting. Another study surveyed a group of anesthesia residents about event reporting, and half were found to lack knowledge about what events should be reported.(12) Interestingly, almost a quarter of the anesthesia residents felt colleagues would not be supportive and 18% were concerned about litigation. This is in contrast to our study where <5% of residents feared retribution from faculty or fellow residents.
Moving forward we plan to continue the Patient Safety Orientation annually to educate residents about event reporting. We will also continue to query residents about potential barriers to event reporting and will use the RQSC to provide reminders and feedback about reported events. We would also like to empower senior residents to be role models to junior residents and medical students when it comes to addressing patient safety and reporting adverse events.
This study had several limitations. First, the study was conducted at a single academic teaching hospital and therefore the results may not be generalizable. While first year residents were required to attend the Patient Safety Orientation, only 70% of residents both attended and completed the survey. Lack of 100% response rate, as well as utilization of surveys to assess resident reporting and perspectives on reporting lends itself to response biases. To address this concern, we also utilized objective reporting data from hospital sources, and the RQSC constructed a fish bone diagram for barriers to event reporting, which identified barriers not included in the survey.
We implemented multiple changes to the reporting system and resident education simultaneously, this could be viewed negatively as it would be difficult to discern which change had the largest effect. However, we felt that residents raised many issues with event reporting at our institution and therefore multiple changes were necessary to make the system more resident friendly. In addition, this study is unique in that we focused on application of changes hospital wide including all residents at the institution. The hospital leadership has committed to continuing education efforts annually and RQSC will continue to continue to educate residents and examine additional areas for improvement.
The results of this study have important implications for patient safety. We outlined resident perceived barriers to adverse event reporting. We demonstrated that by educating residents about adverse events, near misses, and event reporting, in addition to eliminating barriers to event reporting, we can dramatically increase resident event reporting. Residents are on the front lines of patient care in all hospital settings and can have a profound impact on the quality of care patients receive. Educating and empowering residents to report adverse events and near misses will allow hospitals to more readily identify systems issues and areas for improvement in patient safety, and through continued engagement and emphasis of resident participation in patient safety initiatives, we hope patient safety will be an integral part of the future practice of these residents.
Acknowledgments
The authors have no conflicts of interest or sources of funding to report.
Footnotes
Conflicts of Interest and Source of Funding: The authors have no conflicts of interest to disclose.
References
- 1.Tuttle D, Holloway R, Baird T, Sheehan B, Skelton WK. Electronic reporting to improve patient safety. Qual Saf Health Care. 2004;13(4):281–6. doi: 10.1136/qshc.2003.009100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Milch CE, Salem DN, Pauker SG, Lundquist TG, Kumar S, Chen J. Voluntary electronic reporting of medical errors and adverse events. An analysis of 92,547 reports from 26 acute care hospitals. J Gen Intern Med. 2006;21(2):165–70. doi: 10.1111/j.1525-1497.2006.00322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rowin EJ, Lucier D, Pauker SG, Kumar S, Chen J, Salem DN. Does error and adverse event reporting by physicians and nurses differ? Jt Comm J Qual Patient Saf. 2008;34(9):537–45. doi: 10.1016/s1553-7250(08)34068-9. [DOI] [PubMed] [Google Scholar]
- 4.Blum AB, Shea S, Czeisler CA, Landrigan CP, Leape L. Implementing the 2009 Institute of Medicine recommendations on resident physician work hours, supervision, and safety. Nature and science of sleep. 2011;3:47–85. doi: 10.2147/NSS.S19649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weiss KB, Bagian JP, Wagner R, Nasca TJ. Introducing the CLER Pathways to Excellence: A New Way of Viewing Clinical Learning Environments. Journal of graduate medical education. 2014;6(3):608–9. doi: 10.4300/JGME-D-14-00347.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Varkey P, Karlapudi S, Rose S, Swensen S. A patient safety curriculum for graduate medical education: results from a needs assessment of educators and patient safety experts. Am J Med Qual. 2009;24(3):214–21. doi: 10.1177/1062860609332905. [DOI] [PubMed] [Google Scholar]
- 7.Albrecht RM. Patient safety: the what, how, and when. Am J Surg. 2015;210(6):978–82. doi: 10.1016/j.amjsurg.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Patow CA, Karpovich K, Riesenberg LA, Jaeger J, Rosenfeld JC, Wittenbreer M, et al. Residents’ engagement in quality improvement: a systematic review of the literature. Acad Med. 2009;84(12):1757–64. doi: 10.1097/ACM.0b013e3181bf53ab. [DOI] [PubMed] [Google Scholar]
- 9.Longo DR, Hewett JE, Ge B, Schubert S. The long road to patient safety: a status report on patient safety systems. JAMA. 2005;294(22):2858–65. doi: 10.1001/jama.294.22.2858. [DOI] [PubMed] [Google Scholar]
- 10.Wachter RM. Patient safety at ten: unmistakable progress, troubling gaps. Health Aff (Millwood) 2010;29(1):165–73. doi: 10.1377/hlthaff.2009.0785. [DOI] [PubMed] [Google Scholar]
- 11.Boike JR, Bortman JS, Radosta JM, Turner CL, Anderson-Shaw L, Centomani NM, et al. Patient safety event reporting expectation: does it influence residents’ attitudes and reporting behaviors? J Patient Saf. 2013;9(2):59–67. doi: 10.1097/PTS.0b013e3182676e53. [DOI] [PubMed] [Google Scholar]
- 12.Jericho BG, Tassone RF, Centomani NM, Clary J, Turner C, Sikora M, et al. An assessment of an educational intervention on resident physician attitudes, knowledge, and skills related to adverse event reporting. Journal of graduate medical education. 2010;2(2):188–94. doi: 10.4300/JGME-D-10-00036.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scott DR, Weimer M, English C, Shaker L, Ward W, Choi D, et al. A novel approach to increase residents’ involvement in reporting adverse events. Acad Med. 2011;86(6):742–6. doi: 10.1097/ACM.0b013e318217e12a. [DOI] [PubMed] [Google Scholar]
- 14.Flodgren G, Eccles MP, Shepperd S, Scott A, Parmelli E, Beyer FR. An overview of reviews evaluating the effectiveness of financial incentives in changing healthcare professional behaviours and patient outcomes. Cochrane Database Syst Rev. 2011;(7):CD009255. doi: 10.1002/14651858.CD009255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beasley JW, Escoto KH, Karsh BT. Design elements for a primary care medical error reporting system. WMJ. 2004;103(1):56–9. [PubMed] [Google Scholar]