Abstract
Rotavirus is the leading cause of diarrheal death among children <5 years old worldwide, estimated to have caused ~215,000 deaths in 2013. Prior to rotavirus vaccine implementation, >65% of children had at least one rotavirus diarrhea illness by 5 years of age and rotavirus accounted for >40% of all-cause diarrhea hospitalizations globally. Two live, oral rotavirus vaccines have been implemented nationally in >100 countries since 2006 and their use has substantially reduced the burden of severe diarrheal illness in all settings. Vaccine efficacy and effectiveness estimates suggest there is a gradient in vaccine performance between low-child mortality countries (>90%) and medium- and high-child mortality countries (57–75%). Additionally, an increased risk of intussusception (~1–6 per 100,000 vaccinated infants) following vaccination has been documented in some countries, but this is outweighed by the large benefits of vaccination. Two additional live, oral rotavirus vaccines were recently licensed and these have improved on some programmatic limitations of earlier vaccines, such as heat stability, cost, and cold-chain footprint. Non-replicating rotavirus vaccines that are parenterally administered are in clinical testing, and these have the potential to reduce the performance differential and safety concerns associated with live oral rotavirus vaccines.
1. Introduction
Rotavirus is a significant cause of diarrheal hospitalizations and deaths among children <5 years old worldwide [1, 2]. Symptoms of rotavirus infection include watery diarrhea, vomiting, and fever. Rotavirus is primarily spread through the fecal-oral route [3]. Since their licensure in 2006, rotavirus vaccines have dramatically reduced the disease burden. However, vaccines are not yet routinely available in all countries and there are limitations to the currently licensed vaccines. In this article, we present the current state of rotavirus disease burden and vaccines and discuss post-licensure rotavirus vaccine effectiveness, impact, and safety.
2. Disease burden
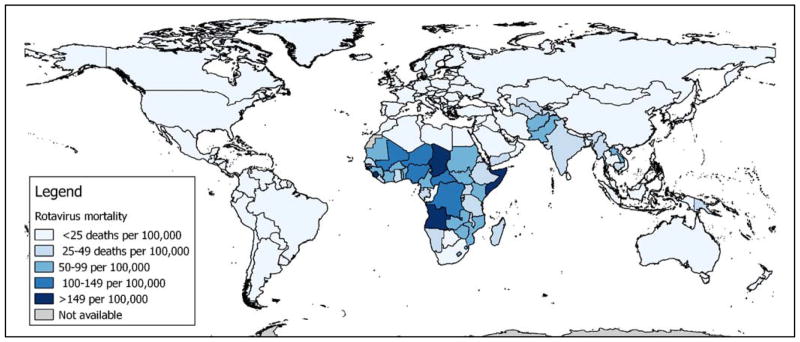
Prior to the availability of rotavirus vaccines, rotavirus infection was a common experience for children <5 years old. Studies of the natural history of rotavirus infections during the pre-vaccine era in Australia, Bangladesh, Canada, Guinea Bissau, India, and Mexico found 64–80% of children had at least one rotavirus infection in infancy and early childhood [4–9]. In 2013, an estimated 215 000 deaths due to rotavirus diarrhea among children <5 years of age occurred worldwide, of which >95% occurred in countries in Africa and Asia [2]. Estimated rotavirus mortality rates by country are visualized in Figure 1. Rotavirus infections also represent a significant proportion of diarrhea hospitalizations in young children [10]. The Global Rotavirus Surveillance Network, a sentinel hospital-based active surveillance system for diarrhea coordinated by the World Health Organization (WHO) has found that rotavirus accounted for over one third of diarrhea hospitalizations before the vaccine was introduced [11].
Figure 1.
Estimated rotavirus mortality rates by country, 2013.
3. Rotavirus biology and immunity
Rotavirus consists of a non-enveloped RNA virus with a segmented genome surrounded by a triple-layered protein capsid [12, 13]. While many species of animals can be infected by rotavirus, human infections are primarily caused by group A; two structural proteins in the outer layer, VP7, the G protein, and VP4, the P protein, determine the genotype [12–14]. In a synthesis of 30 years of pre-vaccine data, more than two thirds of rotavirus infections globally were attributed to G1P[8] and an additional 20% were due to G2P[4], G3P[8], and G4P[8] [14]. There is some variation in circulating genotypes by year and region, for example G1P[8] accounted for just 23% of infections in Africa and 34% in Asia. More recently, G9 and G12 viruses have contributed to a larger proportion of global rotavirus infections [15].
Initial natural rotavirus infections, including asymptomatic neonatal infections, have been shown to reduce the frequency and severity of subsequent rotavirus infections during childhood and beyond [4, 5, 7, 16]. First natural infections were 56–77% efficacious against later rotavirus infections and increased with each subsequent; protection was higher against diarrheal illness caused by rotavirus [5, 7, 16]. Rotavirus infections also offer some protection against other strains of rotavirus causing diarrheal disease [4, 5]. These findings provided the rationale for the development of an infant vaccine against rotavirus. Despite this body of research, no good correlate of protection against diarrheal disease due to rotavirus has been identified.
4. Licensed rotavirus vaccines
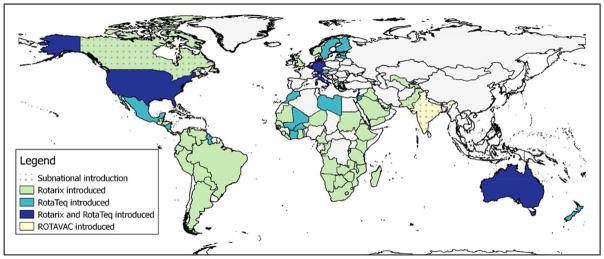
Since 2006, two live, oral rotavirus vaccines have been licensed in >100 countries and pre-qualified by the World Health Organization (WHO). RotaTeq (Merck and Co) is a three-dose, pentavalent bovine-human reassortant rotavirus vaccine that is distributed in a single, 2mL dose vial and Rotarix (GSK Biologics) is a two-dose, monovalent human G1P[8] rotavirus vaccine that is distributed in a single, 1.5mL dose vial (Table 1) [17–19]. As of September 2017, more than 80 countries have introduced rotavirus vaccine into their national, routine infant vaccination programs (Figure 2) [20, 21]. Two newly-licensed live, oral rotavirus vaccines, Rotasiil (Serum Institute of India), a three-dose, pentavalent bovine-human reassortant vaccine, and ROTAVAC (Bharat Biotech), a three-dose, monovalent human-bovine G9P[11] vaccine, are seeking WHO pre-qualification as of 2017 [22–24]. In addition to these four vaccines, domestically licensed live, oral rotavirus vaccines are available in China (LLR, Lanzhou Institute of Biological Produces) and Vietnam (Rotavin, PolyVac) [24].
Table 1.
Licensed rotavirus vaccines.
| Name/Type | Organization/Company | Composition | Doses/course | VVM Type | Price/dose | Licensure |
|---|---|---|---|---|---|---|
| Rotarix | GSK Biologics | Live human-attenuated rotavirus strain, G1P[8] | 2 | 14 | $2.501 | >100 countries globally, WHO pre-qualified |
| RotaTeq | Merck and Co | Live attenuated bovine-human reassortant strains, G1, G2, G3, G4, P1[8] | 3 | None | $3.201 | >100 countries globally, WHO pre-qualified |
| Rotasiil | Serum Institute of India, India and PATH, USA | Bovine-Human Reassortant Rotavirus Vaccine [G1, G2, G3, G4, G9] | 3 | 30 | $2.502 | In India, under consideration for WHO pre-qualification |
| ROTAVAC | Bharat Biotech, India and PATH, USA | Live attenuated neonatal rotavirus strain, G9P[11] (aka 116E) | 3 | 2 | $1.002 | In India, under consideration for WHO pre-qualification |
| Lanzhou Lamb Rotavirus (LLR) | Lanzhou Institute of Biological Products, China | Live attenuated lamb rotavirus strain, G10P[12] | 5 | - | N/A | In China |
| Rotavin-M1 | POLYVAC, Vietnam | Live attenuated human rotavirus strain, G1P[8] | 2 | - | N/A | In Vietnam |
Figure 2.
Rotavirus vaccine introduction status by country, 2017
Clinical trials of vaccine efficacy and post-licensure effectiveness evaluations of RotaTeq and Rotarix in high and upper-middle income countries demonstrated that the vaccines were >90% effective in preventing severe rotavirus disease [17, 18, 25–28]. However, clinical trials in countries with higher child mortality found that rotavirus vaccines were less efficacious in these settings, with published efficacy estimates ranging from 50–64% [29–31]. Similar to the results from the clinical trials of RotaTeq and Rotarix, ROTAVAC’s vaccine efficacy against hospitalization for rotavirus diarrhea was 54% in a clinical trial in India and Rotasiil’s was 67% in a clinical trial in Niger and 39% in India [22, 23, 32].
ROTAVAC and Rotasiil promised improvements on certain programmatic aspects of Rotarix and RotaTeq. For example, ROTAVAC is expected to cost USD$1 and Rotasiil is expected to cost USD$2.50 per dose, compared to approximately USD$3.20 for RotaTeq and USD$2.50 for Rotarix through UNICEF’s supply division [22, 23, 33, 34]. Additionally, ROTAVAC’s presentation as a 0.5mL vaccine in a 5-dose vial reduces the required space in the cold chain and associated costs [19, 24]. Rotasiil, a lyophilized vaccine, is heat stable for 6 months at 40°C; the clinical trial for Rotasiil in Niger found the vaccine was efficacious after storage at up to 25°C in the distribution facility and at the ambient temperature once distributed to the vaccination centers [23, 35]. This demonstrated heat stability could reduce the burden on the cold chain, as well as the financial costs and forecasting challenges associated with vaccine wastage due to temperature excursions [36, 37].
5. Vaccine effectiveness
A recent systematic review of post-licensure vaccine effectiveness (VE) evaluations in countries using RotaTeq and Rotarix supported the clinical trial findings that suggested differential vaccine performance between low and high children mortality countries (as ROTAVAC and Rotasiil are recently licensed and not yet introduced on a national scale, they were not included in the literature review). Jonesteller et al reported median Rotarix VE of 84% in low child mortality countries, 75% in medium child mortality countries, and 57% in high child mortality countries (Table 2) [38]. Comparably, median RotaTeq VE was 90% in low child mortality countries and 45% in high child mortality countries [38].
Table 2.
Post-licensure vaccine effectiveness
| Rotarix | RotaTeq | ||||||
|---|---|---|---|---|---|---|---|
| Low | Medium | High | Low | Medium | High | ||
| Full series VE, median (range) | 84 (19, 97) | 75 (−2, 94) | 57 (18, 69) | 90 (63, 100) | - | 45 (43, 92) | |
| Median difference in VE | |||||||
| Partial series | full series VE v. 1 dose VE | −3 | 10 | 19 | 16 | - | 6 |
| full series VE v. 2 doses VE | - | - | - | 7 | - | −4 | |
| By age group | <12 months VE v. ≥12 months VE | −5 | 31 | −1 | 4 | - | 23 |
| By severity | hospitalizations VE v. ED VE | 5 | - | - | 9 | - | - |
| Vesikari 15 VE v. Vesikari 11 VE | - | −25 | 17 | - | - | 15 | |
Because many of the post-licensure evaluations have not been sufficiently powered to detect differences between subpopulations, the systematic review also aimed to clarify questions of VE with a partially completed vaccination series and against a range of disease severities through summary statistics. For Rotarix in low child mortality countries, VE was nearly the same for children who received the full number of the manufacturer recommended doses and children who only were partially vaccinated; the median reported difference was 3 percentage points. In medium and high child mortality countries, VE was higher in children who received the full-series compared to children who received a single dose, with a median difference of 10 and 19 percentage points, respectively. For RotaTeq in low child mortality countries, VE was higher among fully vaccinated children compared to children who received only one or two doses, with a median difference of 16 percentage points. A single evaluation from a high child mortality country using RotaTeq showed that VE was 65 higher among fully vaccinated children compared with partially vaccinated children [38].
The review found articles defined severity in two ways: by hospitalization status (i.e. emergency department or inpatient) and by Vesikari score. Vesikari score is a grading of seven clinical signs and symptoms; higher numeric values on the 20-point scale indicate more severe and dehydrating diarrheal illness [39]. In low child mortality countries, the median difference in VE was slightly higher among hospitalized children compared to those treated in the emergency department for both vaccines, with a median difference of 5 percentage points for Rotarix and 9 percentage points for RotaTeq [38]. While there is some variation, overall these results indicate higher effectiveness against more severe rotavirus disease in a variety of settings. In medium child mortality countries, Rotarix VE was a median 25% lower among children with high Vesikari scores compared to lower scores. In high child mortality countries, the median difference in VE was 17 and 16 percentage points higher among children with high Vesikari scores compared to those with low scores using Rotarix and RotaTeq, respectively [38].
6. Explaining and improving performance of oral rotavirus vaccines in developing countries
The exact reasons for the gradient in VE between low, medium, and high child mortality countries are unknown, however several factors are known to reduce the effectiveness of these vaccines. Other oral vaccines, such as cholera and polio, have also demonstrated lower effectiveness in low income settings. Co-infections with other enteric pathogens at the time of vaccination inhibits immune response to rotavirus vaccine, as well as oral polio vaccine [40, 41]. Transplacental maternal rotavirus antibodies have been shown to reduce vaccine-induced immunity in young infants [42–44]. Some improvement to VE may occur naturally as the global polio program transitions from live oral polio vaccine to injectable formulations. Polio and rotavirus vaccines are typically recommended for concomitant administration and oral polio vaccine has been found to interfere with rotavirus vaccine in the gut and immunogenicity of rotavirus vaccine [45–47].
Researchers are exploring several additional hypotheses that might explain differential vaccine performance. Matched case-control studies that included Ghanaian, Pakistani, and Dutch infants suggested compelling correlations between gut microbiota composition and rotavirus seroconversion following vaccination. However, the sample sizes in these initial studies were quite small and a corresponding intervention would need to be proposed and tested [48, 49].
There had been some initial concern that immunity induced by RotaTeq and Rotarix vaccines may not protect against non-vaccine strains, which was particularly relevant in Africa and Asia, since the distribution of rotavirus strains varied compared to countries where rotavirus vaccines were initially developed, tested and introduced [14]. However, a meta-analysis of studies from Australia, Belgium, Brazil, Bolivia, El Salvador, Mexico, Nicaragua, and the United States showed that RotaTeq and Rotarix provide protection against homotypic and heterotypic rotavirus strains [50]. Rotavirus recognizes human histo-blood group antigens (HBGA) and individuals with Lewis-negative secretor-positive HBGA phenotypes have an increased susceptibility to P[8] rotavirus strains, compared to non-secretors [51, 52]. As this phenotype is more common in African populations than US or European populations, researchers have hypothesized that Lewis-negative secretor-positive children may be unable to develop protection using the current rotavirus vaccines, as a reason for poorer performance of Rotarix and RotaTeq in sub-Saharan Africa. However, ROTAVAC uses a G9P[11] strain and its efficacy in India was comparable to Rotarix and RotaTeq in medium and high child mortality settings, indicating HBGA status is not the only reason for the effectiveness gradient. Further research is needed to determine what role HBGAs may play in vaccine-induced immunity against rotavirus and how this might guide future vaccine development.
Several programmatic strategies have also been evaluated to boost rotavirus VE, including improving nutrition status, recommending alternative ages of administration, timing of breastfeeding, and supplementation with zinc [53–63]. Findings from studies that considered alternate ages of administration have been mixed, with one study demonstrating improved immunogenicity with older administration of Rotarix and two others showing no impact [29, 56, 64, 65]. There was concern that lower VE may be because rotavirus vaccine is neutralized by high maternal antibody in breastmilk in settings with high rotavirus burden. However, studies evaluating withholding breastfeeding at the time of vaccination and rotavirus vaccine response have not found any relationship [57, 58, 60, 62]. A recent randomized control trial in India found a modest improvement in immunogenicity following rotavirus vaccination with zinc and probiotic supplementation together; no effect was found when rotavirus vaccine was administered with zinc or the probiotic alone, however the authors report the dosage of zinc may have been too low [63].
While clinical trials in low child mortality countries did not identify a difference in vaccine efficacy between children <12 months of age and children ≥12 months of age, there was some evidence suggesting waning vaccine efficacy after first year of life in medium and high child mortality countries [65–67]. Similar to the clinical trial findings, in low child mortality countries differences between age groups were not found by the systematic review of post-licensure VE studies with either vaccine. However, Rotarix VE was almost a third higher among children <12 month of age in medium child mortality countries compared to children ≥12 months of age; there was no difference in the summary differences in high child mortality countries. RotaTeq VE was nearly 25% higher among children <12 month of age in high child mortality countries compared to children ≥12 months of age [38]. The age-group specific sample sizes in these evaluations were generally too small to detect a difference; never the less, the potential waning has important implications for vaccination programs. A clinical trial in Bangladesh demonstrated a booster dose at 9 months of age improved IgG antibodies against rotavirus; a similarly designed analysis from a clinical trial in Mali is forthcoming [68, 69]. These findings have led to optimism that modifying recommendations to include a booster dose of rotavirus vaccine may address the observed waning immunity with the currently available vaccines. However further research is needed as the published analysis did not include a clinical endpoint to assess vaccine efficacy following a rotavirus booster dose [68].
7. Vaccine impact
Despite differential VE, rotavirus vaccines have had a sizeable impact on diarrhea morbidity and mortality in low, medium, and high child mortality countries. Following rotavirus vaccine introduction, rotavirus mortality decreased by 22% in Brazil and 41% in Mexico among children <1 years old [70, 71]. Countries have experienced a reduction in rotavirus diarrhea hospitalizations by a median of 67% after including rotavirus vaccine in their national immunization programs [72]. In absolute numbers, this translates to thousands of hospitalizations prevented each year. For instance, in the first 7 years of rotavirus vaccine implementation in the United States, vaccination prevented an estimated 382,000 hospitalizations and saved over USD$1 billion in direct medical costs [73]. In the 29 African countries that had introduced rotavirus vaccine by the end of 2014, nearly 135,000 rotavirus hospitalizations and 21,000 rotavirus deaths were estimated to have been prevented in 2016 [74].
Universal adoption of routine rotavirus vaccination would also reduce the global burden of rotavirus disease. As an example, in all African countries that had not introduced rotavirus vaccine, including Nigeria and the Democratic Republic of Congo, an additional 119,000 hospitalizations and 22,000 deaths were projected to be prevented with national, routine use of rotavirus vaccines at coverage levels comparable to diphtheria-tetanus-pertussis (DTP) vaccines.
8. Safety
An earlier rotavirus vaccine, RotaShield (Wyeth), a rhesus quadravalent rotavirus vaccine licensed in the US in 1998, was removed from the market in 1999 after post-licensure safety assessments identified a 10-fold (aOR: 10.6, 95%CI:5.7–19.6) elevated risk of intussusception, a rare bowel obstruction caused by telescoping of the small intestine, following rotavirus vaccination, or approximately 1 excess intussusception case per 10,000 children vaccinated [75–78].
Large clinical trials of RotaTeq and Rotarix did not detect an increased incidence of intussusception following vaccination [17, 18, 79]. Since the licensure of Rotarix and RotaTeq in 2006, a slightly increased risk of intussusception has been observed in post-licensure safety monitoring, especially in the first seven days post-vaccination [80–85]. A 2015 meta-analysis of intussusception risk following real-world rotavirus vaccination in Australia, Brazil, England Mexico, Singapore, and the United States found an elevated risk of intussusception in the first 21 days following the first dose of Rotarix (OR: 2.4, 95%CI: 1.5, 3.8) and the second dose (OR: 1.8, 95%CI: 1.3, 2.4), or roughly 1.9 and 1.5 excess cases of intussusception per 100,000 children vaccinated, respectively [86]. In an analysis of the risk of intussusception following RotaTeq vaccination in Australia and the US, also found a similar level of risk for the first and second doses [87]. No association between intussusception and rotavirus vaccination was found in a retrospective evaluation in South Korea, although the number of children included in the analysis was smaller than other post-licensure studies [88]. As more countries with medium and high child mortality introduce rotavirus vaccine, it will be important to evaluate the risk of intussusception specifically in those settings.
Over the decade since licensure of Rotarix and RotaTeq, the benefits of rotavirus vaccination in decreased hospitalizations and deaths have far outweighed the risks. Initially, WHO recommended upper age limits for vaccination to minimize excess cases of intussusception; evidence from RotaShield suggested the highest incidence of intussusception was among older infants, when the natural incidence of intussusception also increases [75–77]. These recommendations were changed in 2009 after models demonstrated 44 rotavirus diarrhea deaths would be prevented for every one potential intussusception death if children were eligible to receive rotavirus vaccination up to 1 year of age [75, 89]. WHO recommends administering rotavirus vaccine to children up to 24 months of age concomitantly with DTP vaccine [75].
Newer rotavirus vaccines have evaluated safety in their clinical trials, however the sample size was insufficient to detect a small increase in risk, like that observed with Rotarix and RotaTeq. The Phase III clinical trials for both ROTAVAC and Rotasiil reported 0 cases of intussusception in the first month following any dose of vaccine or placebo [22, 23, 32]. Post-licensure safety monitoring will also continue to be important as new vaccines are adopted more widely.
9. Vaccines in development
Although the existing rotavirus vaccines have dramatically reduced rotavirus diarrhea worldwide, the licensure of additional rotavirus vaccines may address some of the limitations of the current vaccines as well as reinforce the market. Several additional live oral vaccines are being developed. Lanzhou Institute has completed a Phase III trial for a trivalent lamb reassortant rotavirus vaccine (Table 3) [24, 90]. Butantan Instutite completed Phase I clinical trials for a pentavalent human-bovine vaccine [91]. A hexavalent bovine-human rotavirus vaccine by Wuhan Institute of Biological Products (China) is in the process of completing Phase I trials [24]. Additionally, Bharat Biotech is developing a liquid stable formulation of ROTAVAC.
Table 3.
Rotavirus vaccine in development
| Stage of development | Name/Type | Composition | Route of administration | Organization/Company |
|---|---|---|---|---|
| Phase III | LLR reassortants | Live attenuated lamb-human reassortant rotavirus strains, G2, G3, G4 | Oral | Lanzhou Institute of Biological Products, China |
| Phase III | RotaShield | Live attenuated rhesus-human reassortant rotavirus strains, tetravalent | Oral | International Medica Foundation and PATH, USA |
| Phase III | UK reassortants | BRV Tetravalent (G1–G4) | Oral | Shantha Biotech, India |
| Phase IIb | RV3 | Live attenuated neonatal rotavirus strain, G3P[6] | Oral | Murdoch Children’s Research Institute, Australia and Biofarma, Indonesia |
| Phase II | Subunit | Truncated VP8 of P4, P6, P8 | Intramuscular | National Institutes of Health and PATH, USA |
| Phase I | UK reassortants | Bovine UK Human G1,G2,G3,G4,G9 reassortants 5V | Oral | Instituto Butantan, Brazil |
| Phase I | UK reassortants | Live attenuated bovine-human reassortant strains, tetravalent to hexavalent | Oral | Wuhan Institute of Biological Products, China and PATH, USA |
| Pre-clinical | IRV | Inactivated G1P[8], G2P[4] | Intramuscular or intradermal | US CDC |
| Pre-clinical | Subunit | Virus-like particles: VP 2/6/7 and VP 2/4/6/7 | To be determined | Baylor College of Medicine, USA |
| Pre-clinical | Subunit | Truncated VP8 in norovirus P particles | To be determined | Cincinnati Children’s Hospital Medical Center, USA |
| Research | Subunit | VP6 combined with norovirus G1 and GII VLPs | To be determined | University of Tampere School of Medicine, Finland |
Two alternative types of rotavirus vaccines are in development that may eliminate the VE differential between child mortality settings and the small risk of vaccine-associated intussusception. Murdoch Children’s Research Institute (Australia) and PT Biofarma (Indonesia) are developing a live oral human rotavirus vaccine from a G3P[6] strain found to cause asymptomatic infections in neonates [24]. This strain was selected because it is able to replicate in the newborn gut, even in the presence of maternal antibodies, and the strain may also offer protection to individuals with a Lewis-negative and secretor-positive phenotype. A Phase IIa clinical trial demonstrated this vaccine was immunogenic with both infant (6 week, 10 week, 14 week) and newborn (birth, 6 week, 10 week) administration schedules [92]. Administration of a rotavirus vaccine to newborns offers other benefits. A birth dose could offer protection from diarrheal disease and deaths before any children are exposed to wild rotavirus, potentially preventing additional infections that occur between birth and the current recommended age administration of the first dose, usually 6 weeks or 2 months of age [2, 93]. Other vaccines that have a recommended birth dose, such as polio, Hepatitis B, and bacilli Calmette-Guerin (BCG) vaccines, have high vaccination coverage of children <1 year old; birth dose administration of rotavirus vaccine could improve coverage compared to the current infant schedule. Additionally, natural intussusception is rare before three months of age [94]; a birth dose may eliminate the vaccine-associated risk of intussusception. This vaccine is undergoing in Phase IIb clinical trial [24]. RotaShield has also been considered for a neonatal administration schedule; a clinical trial showed 61% efficacy in Ghanaian infants vaccinated during the first and second months of life [95].
Non-replicating vaccines with a parenteral delivery strategy have been proposed as a way to eliminate the risk of intussusception, since immune response would not be dependent on vaccine viruses replicating in the gut. Additionally, these vaccines may not be susceptible to the hypothesized reasons for lower VE in medium and high child mortality settings such as co-infections, microbiota composition, or interference by oral polio vaccine [24, 96]. Intramuscular administration has additionally benefits; for example, it could be included in a combination vaccine with other routine infant vaccinations like DTP and pneumococcal vaccines (PCV). A subunit vaccine developed by PATH showed safety and immunogenicity in a recently completed a Phase I/II descending dose study; an additional Phase I/II study is currently underway [97]. To date, none of the clinical trials of these vaccines have included a clinical endpoint. Intradermal administration of a whole, inactivated particle vaccine, using a microneedle patch of an inactivated vaccine, is also being developed by CDC. Microneedle patches have several programmatic advantages, including thermal stability, reduced packaging, elimination of sharp biohazardous waste, and ease of administration [98, 99]. Additionally, immune response to intradermal administration may allow for a fractional dose to be administered, which could improve the supply chain and reduce costs [24, 100].
10. Conclusions
Over the last 11 years, rotavirus vaccines have been safely and effectively implemented in more than 80 countries worldwide. Large reductions in rotavirus diarrhea deaths and hospitalizations during these period have been sweeping; however, the live, oral rotavirus vaccines have been shown to be less effective in medium and high child mortality settings than countries with low child mortality. New vaccines in development are promising to further reduce the burden of rotavirus diarrhea morbidity and mortality among children <5 years old.
Key Points.
Since 2006, two live, oral rotavirus vaccines have reduced the substantial burden of rotavirus disease in countries that have introduced the vaccines into their national, routine immunization program.
The effectiveness of rotavirus vaccines is lower in high child mortality settings, compared to low child mortality settings; while there are several hypotheses, including differences in co-infections with other enteropathogens at the time of vaccination, gut microbiota composition, and prevalence of Lewis-negative secretor-positive histo-blood group antigens, the exact causes for lower vaccine performance are unknown.
Other rotavirus vaccines are currently under development that make use of alternate rotavirus strains and delivery strategies to ameliorate specific programmatic challenges with the currently available vaccines.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention (CDC).
Compliance with Ethical Standards
The authors declare that they have no conflict of interest. There was no funding for this review.
References
- 1.Causes of child mortality, by country, 2000–2010. 2017 Aug 29; ]; Available from: http://www.who.int/gho/child_health/mortality/mortality_causes_text/en/
- 2.Tate JE, Burton AH, Boschi-Pinto C, Parashar UD World Health Organization-Coordinated Global Rotavirus Surveillance N. Global, Regional, and National Estimates of Rotavirus Mortality in Children <5 Years of Age, 2000–2013. Clin Infect Dis. 2016 May 1;62(Suppl 2):S96–S105. doi: 10.1093/cid/civ1013. [DOI] [PubMed] [Google Scholar]
- 3.Ansari SA, Springthorpe VS, Sattar SA. Survival and vehicular spread of human rotaviruses: possible relation to seasonality of outbreaks. Rev Infect Dis. 1991 May-Jun;13(3):448–61. doi: 10.1093/clinids/13.3.448. [DOI] [PubMed] [Google Scholar]
- 4.Bishop RF, Barnes GL, Cipriani E, Lund JS. Clinical immunity after neonatal rotavirus infection. A prospective longitudinal study in young children. N Engl J Med. 1983 Jul 14;309(2):72–6. doi: 10.1056/NEJM198307143090203. [DOI] [PubMed] [Google Scholar]
- 5.Fischer TK, Valentiner-Branth P, Steinsland H, Perch M, Santos G, Aaby P, et al. Protective immunity after natural rotavirus infection: a community cohort study of newborn children in Guinea-Bissau, west Africa. J Infect Dis. 2002 Sep 1;186(5):593–7. doi: 10.1086/342294. [DOI] [PubMed] [Google Scholar]
- 6.Gladstone BP, Ramani S, Mukhopadhya I, Muliyil J, Sarkar R, Rehman AM, et al. Protective effect of natural rotavirus infection in an Indian birth cohort. N Engl J Med. 2011 Jul 28;365(4):337–46. doi: 10.1056/NEJMoa1006261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Velazquez FR, Matson DO, Calva JJ, Guerrero L, Morrow AL, Carter-Campbell S, et al. Rotavirus infection in infants as protection against subsequent infections. N Engl J Med. 1996 Oct 3;335(14):1022–8. doi: 10.1056/NEJM199610033351404. [DOI] [PubMed] [Google Scholar]
- 8.Gurwith M, Wenman W, Hinde D, Feltham S, Greenberg H. A prospective study of rotavirus infection in infants and young children. J Infect Dis. 1981 Sep;144(3):218–24. doi: 10.1093/infdis/144.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Black RE, Greenberg HB, Kapikian AZ, Brown KH, Becker S. Acquisition of serum antibody to Norwalk Virus and rotavirus and relation to diarrhea in a longitudinal study of young children in rural Bangladesh. J Infect Dis. 1982 Apr;145(4):483–9. doi: 10.1093/infdis/145.4.483. [DOI] [PubMed] [Google Scholar]
- 10.Parashar UD, Hummelman EG, Bresee JS, Miller MA, Glass RI. Global illness and deaths caused by rotavirus disease in children. Emerg Infect Dis. 2003 May;9(5):565–72. doi: 10.3201/eid0905.020562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease C, Prevention. Rotavirus surveillance --- worldwide, 2009. MMWR Morb Mortal Wkly Rep. 2011 Apr 29;60(16):514–6. [PubMed] [Google Scholar]
- 12.Estes MK, Cohen J. Rotavirus gene structure and function. Microbiol Rev. 1989 Dec;53(4):410–49. doi: 10.1128/mr.53.4.410-449.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greenberg HB, Estes MK. Rotaviruses: from pathogenesis to vaccination. Gastroenterology. 2009 May;136(6):1939–51. doi: 10.1053/j.gastro.2009.02.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santos N, Hoshino Y. Global distribution of rotavirus serotypes/genotypes and its implication for the development and implementation of an effective rotavirus vaccine. Rev Med Virol. 2005 Jan-Feb;15(1):29–56. doi: 10.1002/rmv.448. [DOI] [PubMed] [Google Scholar]
- 15.Matthijnssens J, Bilcke J, Ciarlet M, Martella V, Banyai K, Rahman M, et al. Rotavirus disease and vaccination: impact on genotype diversity. Future Microbiol. 2009 Dec;4(10):1303–16. doi: 10.2217/fmb.09.96. [DOI] [PubMed] [Google Scholar]
- 16.Bhan MK, Lew JF, Sazawal S, Das BK, Gentsch JR, Glass RI. Protection conferred by neonatal rotavirus infection against subsequent rotavirus diarrhea. J Infect Dis. 1993 Aug;168(2):282–7. doi: 10.1093/infdis/168.2.282. [DOI] [PubMed] [Google Scholar]
- 17.Ruiz-Palacios GM, Perez-Schael I, Velazquez FR, Abate H, Breuer T, Clemens SC, et al. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med. 2006 Jan 5;354(1):11–22. doi: 10.1056/NEJMoa052434. [DOI] [PubMed] [Google Scholar]
- 18.Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, et al. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med. 2006 Jan 5;354(1):23–33. doi: 10.1056/NEJMoa052664. [DOI] [PubMed] [Google Scholar]
- 19.Introduction of Rotavirus Vaccines: information for policy makers, programme managers, and health workers. World Health Organization; 2013. http://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/sentinel/rotavirus_intro_guidance_who_july31_2013.pdf. [Google Scholar]
- 20.Loharikar A, Dumolard L, Chu S, Hyde T, Goodman T, Mantel C. Status of New Vaccine Introduction - Worldwide, September 2016. MMWR Morb Mortal Wkly Rep. 2016 Oct 21;65(41):1136–40. doi: 10.15585/mmwr.mm6541a3. [DOI] [PubMed] [Google Scholar]
- 21.Vaccine in national immunization programme update 2007. 2017 Aug 29; ]; Available from: http://www.who.int/immunization/monitoring_surveillance/data/en/
- 22.Bhandari N, Rongsen-Chandola T, Bavdekar A, John J, Antony K, Taneja S, et al. Efficacy of a monovalent human-bovine (116E) rotavirus vaccine in Indian infants: a randomised, double-blind, placebo-controlled trial. Lancet. 2014 Jun 21;383(9935):2136–43. doi: 10.1016/S0140-6736(13)62630-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Isanaka S, Guindo O, Langendorf C, Matar Seck A, Plikaytis BD, Sayinzoga-Makombe N, et al. Efficacy of a Low-Cost, Heat-Stable Oral Rotavirus Vaccine in Niger. N Engl J Med. 2017 Mar 23;376(12):1121–30. doi: 10.1056/NEJMoa1609462. [DOI] [PubMed] [Google Scholar]
- 24.Kirkwood CD, Ma LF, Carey ME, Steele AD. The rotavirus vaccine development pipeline. Vaccine. 2017 Apr 7; doi: 10.1016/j.vaccine.2017.03.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vesikari T, Uhari M, Renko M, Hemming M, Salminen M, Torcel-Pagnon L, et al. Impact and effectiveness of RotaTeq(R) vaccine based on 3 years of surveillance following introduction of a rotavirus immunization program in Finland. Pediatr Infect Dis J. 2013 Dec;32(12):1365–73. doi: 10.1097/INF.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 26.Yen C, Figueroa JR, Uribe ES, Carmen-Hernandez LD, Tate JE, Parashar UD, et al. Monovalent rotavirus vaccine provides protection against an emerging fully heterotypic G9P[4] rotavirus strain in Mexico. J Infect Dis. 2011 Sep 1;204(5):783–6. doi: 10.1093/infdis/jir390. [DOI] [PubMed] [Google Scholar]
- 27.Cortese MM, Immergluck LC, Held M, Jain S, Chan T, Grizas AP, et al. Effectiveness of monovalent and pentavalent rotavirus vaccine. Pediatrics. 2013 Jul;132(1):e25–33. doi: 10.1542/peds.2012-3804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang FT, Mast TC, Glass RJ, Loughlin J, Seeger JD. Effectiveness of the pentavalent rotavirus vaccine in preventing gastroenteritis in the United States. Pediatrics. 2010 Feb;125(2):e208–13. doi: 10.1542/peds.2009-1246. [DOI] [PubMed] [Google Scholar]
- 29.Armah GE, Sow SO, Breiman RF, Dallas MJ, Tapia MD, Feikin DR, et al. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in sub-Saharan Africa: a randomised, double-blind, placebo-controlled trial. Lancet. 2010 Aug 21;376(9741):606–14. doi: 10.1016/S0140-6736(10)60889-6. [DOI] [PubMed] [Google Scholar]
- 30.Madhi SA, Cunliffe NA, Steele D, Witte D, Kirsten M, Louw C, et al. Effect of human rotavirus vaccine on severe diarrhea in African infants. N Engl J Med. 2010 Jan 28;362(4):289–98. doi: 10.1056/NEJMoa0904797. [DOI] [PubMed] [Google Scholar]
- 31.Zaman K, Dang DA, Victor JC, Shin S, Yunus M, Dallas MJ, et al. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in Asia: a randomised, double-blind, placebo-controlled trial. Lancet. 2010 Aug 21;376(9741):615–23. doi: 10.1016/S0140-6736(10)60755-6. [DOI] [PubMed] [Google Scholar]
- 32.Kulkarni PS, Desai S, Tewari T, Kawade A, Goyal N, Garg BS, et al. A randomized Phase III clinical trial to assess the efficacy of a bovine-human reassortant pentavalent rotavirus vaccine in Indian infants. Vaccine. 2017 Oct 27;35(45):6228–37. doi: 10.1016/j.vaccine.2017.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Division S, editor. UNICEF. Supply Catalogue- Rotavirus. UNICEF; 2017. [Google Scholar]
- 34.Detailed Product Profiles- Rotavirus. 2017 Nov 7; ]; Available from: http://www.gavi.org/library/gavi-documents/supply-procurement/detailed-product-profiles/
- 35.Zade JK, Kulkarni PS, Desai SA, Sabale RN, Naik SP, Dhere RM. Bovine rotavirus pentavalent vaccine development in India. Vaccine. 2014 Aug 11;32(Suppl 1):A124–8. doi: 10.1016/j.vaccine.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 36.Immunization V, and Biologicals. World Health Organization; 2005. Monitoring vaccine wastage at country level: Guidelines for program managers. [Google Scholar]
- 37.Wallace AS, Willis F, Nwaze E, Dieng B, Sipilanyambe N, Daniels D, et al. Vaccine wastage in Nigeria: An assessment of wastage rates and related vaccinator knowledge, attitudes and practices. Vaccine. 2017 Dec 4;35(48 Pt B):6751–8. doi: 10.1016/j.vaccine.2017.09.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jonesteller CL, Burnett E, Yen C, Tate JE, Parashar UD. Effectiveness of Rotavirus Vaccination: A Systematic Review of the First Decade of Global Postlicensure Data, 2006–2016. Clin Infect Dis. 2017 Sep 1;65(5):840–50. doi: 10.1093/cid/cix369. [DOI] [PubMed] [Google Scholar]
- 39.Ruuska T, Vesikari T. Rotavirus disease in Finnish children: use of numerical scores for clinical severity of diarrhoeal episodes. Scand J Infect Dis. 1990;22(3):259–67. doi: 10.3109/00365549009027046. [DOI] [PubMed] [Google Scholar]
- 40.Wang H, Moon S, Wang Y, Jiang B. Multiple virus infection alters rotavirus replication and expression of cytokines and Toll-like receptors in intestinal epithelial cells. Virus Res. 2012 Jul;167(1):48–55. doi: 10.1016/j.virusres.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 41.Taniuchi M, Platts-Mills JA, Begum S, Uddin MJ, Sobuz SU, Liu J, et al. Impact of enterovirus and other enteric pathogens on oral polio and rotavirus vaccine performance in Bangladeshi infants. Vaccine. 2016 Jun 8;34(27):3068–75. doi: 10.1016/j.vaccine.2016.04.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Patel M, Shane AL, Parashar UD, Jiang B, Gentsch JR, Glass RI. Oral rotavirus vaccines: how well will they work where they are needed most? J Infect Dis. 2009 Nov 1;200(Suppl 1):S39–48. doi: 10.1086/605035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Appaiahgari MB, Glass R, Singh S, Taneja S, Rongsen-Chandola T, Bhandari N, et al. Transplacental rotavirus IgG interferes with immune response to live oral rotavirus vaccine ORV-116E in Indian infants. Vaccine. 2014 Feb 3;32(6):651–6. doi: 10.1016/j.vaccine.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 44.Jiang B, Gentsch JR, Glass RI. The role of serum antibodies in the protection against rotavirus disease: an overview. Clin Infect Dis. 2002 May 15;34(10):1351–61. doi: 10.1086/340103. [DOI] [PubMed] [Google Scholar]
- 45.Patel M, Steele AD, Parashar UD. Influence of oral polio vaccines on performance of the monovalent and pentavalent rotavirus vaccines. Vaccine. 2012 Apr 27;30(Suppl 1):A30–5. doi: 10.1016/j.vaccine.2011.11.093. [DOI] [PubMed] [Google Scholar]
- 46.Emperador DM, Velasquez DE, Estivariz CF, Lopman B, Jiang B, Parashar U, et al. Interference of Monovalent, Bivalent, and Trivalent Oral Poliovirus Vaccines on Monovalent Rotavirus Vaccine Immunogenicity in Rural Bangladesh. Clin Infect Dis. 2016 Jan 15;62(2):150–6. doi: 10.1093/cid/civ807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ramani S, Mamani N, Villena R, Bandyopadhyay AS, Gast C, Sato A, et al. Rotavirus Serum IgA Immune Response in Children Receiving Rotarix Coadministered With bOPV or IPV. Pediatr Infect Dis J. 2016 Oct;35(10):1137–9. doi: 10.1097/INF.0000000000001253. [DOI] [PubMed] [Google Scholar]
- 48.Harris V, Ali A, Fuentes S, Korpela K, Kazi M, Tate J, et al. Rotavirus vaccine response correlates with the infant gut microbiota composition in Pakistan. Gut Microbes. 2017 Sep;11:1–9. doi: 10.1080/19490976.2017.1376162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harris VC, Armah G, Fuentes S, Korpela KE, Parashar U, Victor JC, et al. Significant Correlation Between the Infant Gut Microbiome and Rotavirus Vaccine Response in Rural Ghana. J Infect Dis. 2017 Jan 1;215(1):34–41. doi: 10.1093/infdis/jiw518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leshem E, Lopman B, Glass R, Gentsch J, Banyai K, Parashar U, et al. Distribution of rotavirus strains and strain-specific effectiveness of the rotavirus vaccine after its introduction: a systematic review and meta-analysis. Lancet Infect Dis. 2014 Sep;14(9):847–56. doi: 10.1016/S1473-3099(14)70832-1. [DOI] [PubMed] [Google Scholar]
- 51.Nordgren J, Sharma S, Bucardo F, Nasir W, Gunaydin G, Ouermi D, et al. Both Lewis and secretor status mediate susceptibility to rotavirus infections in a rotavirus genotype-dependent manner. Clin Infect Dis. 2014 Dec 1;59(11):1567–73. doi: 10.1093/cid/ciu633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kambhampati A, Payne DC, Costantini V, Lopman BA. Host Genetic Susceptibility to Enteric Viruses: A Systematic Review and Metaanalysis. Clin Infect Dis. 2016 Jan 1;62(1):11–8. doi: 10.1093/cid/civ873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gastanaduy PA, Steenhoff AP, Mokomane M, Esona MD, Bowen MD, Jibril H, et al. Effectiveness of Monovalent Rotavirus Vaccine After Programmatic Implementation in Botswana: A Multisite Prospective Case-Control Study. Clin Infect Dis. 2016 May 1;62(Suppl 2):S161–7. doi: 10.1093/cid/civ1207. [DOI] [PubMed] [Google Scholar]
- 54.Colgate ER, Haque R, Dickson DM, Carmolli MP, Mychaleckyj JC, Nayak U, et al. Delayed Dosing of Oral Rotavirus Vaccine Demonstrates Decreased Risk of Rotavirus Gastroenteritis Associated With Serum Zinc: A Randomized Controlled Trial. Clin Infect Dis. 2016 Sep 1;63(5):634–41. doi: 10.1093/cid/ciw346. [DOI] [PubMed] [Google Scholar]
- 55.Armah G, Pringle K, Enweronu-Laryea CC, Ansong D, Mwenda JM, Diamenu SK, et al. Impact and Effectiveness of Monovalent Rotavirus Vaccine Against Severe Rotavirus Diarrhea in Ghana. Clin Infect Dis. 2016 May 1;62(Suppl 2):S200–7. doi: 10.1093/cid/ciw014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ali SA, Kazi AM, Cortese MM, Fleming JA, Parashar UD, Jiang B, et al. Impact of different dosing schedules on the immunogenicity of the human rotavirus vaccine in infants in Pakistan: a randomized trial. J Infect Dis. 2014 Dec 1;210(11):1772–9. doi: 10.1093/infdis/jiu335. [DOI] [PubMed] [Google Scholar]
- 57.Ali A, Kazi AM, Cortese MM, Fleming JA, Moon S, Parashar UD, et al. Impact of withholding breastfeeding at the time of vaccination on the immunogenicity of oral rotavirus vaccine--a randomized trial. PLoS One. 2015;10(6):e0127622. doi: 10.1371/journal.pone.0127622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Groome MJ, Moon SS, Velasquez D, Jones S, Koen A, van Niekerk N, et al. Effect of breastfeeding on immunogenicity of oral live-attenuated human rotavirus vaccine: a randomized trial in HIV-uninfected infants in Soweto, South Africa. Bull World Health Organ. 2014 Apr 1;92(4):238–45. doi: 10.2471/BLT.13.128066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moon SS, Wang Y, Shane AL, Nguyen T, Ray P, Dennehy P, et al. Inhibitory effect of breast milk on infectivity of live oral rotavirus vaccines. Pediatr Infect Dis J. 2010 Oct;29(10):919–23. doi: 10.1097/INF.0b013e3181e232ea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rongsen-Chandola T, Winje BA, Goyal N, Rathore SS, Mahesh M, Ranjan R, et al. Compliance of mothers following recommendations to breastfeed or withhold breast milk during rotavirus vaccination in North India: a randomized clinical trial. Trials. 2014 Jun 28;15:256. doi: 10.1186/1745-6215-15-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Burnett E, Yen C, Tate JE, Parashar UD. Rotavirus vaccines: current global impact and future perspectives. Future Virol. 2016 Oct;11(10):699–708. doi: 10.2217/fvl-2016-0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Becker-Dreps S, Choi WS, Stamper L, Vilchez S, Velasquez DE, Moon SS, et al. Innate Immune Factors in Mothers’ Breast Milk and Their Lack of Association With Rotavirus Vaccine Immunogenicity in Nicaraguan Infants. J Pediatric Infect Dis Soc. 2017 Mar 1;6(1):87–90. doi: 10.1093/jpids/piv076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lazarus RP, John J, Shanmugasundaram E, Rajan AK, Thiagarajan S, Giri S, et al. The effect of probiotics and zinc supplementation on the immune response to oral rotavirus vaccine: A randomized, factorial design, placebo-controlled study among Indian infants. Vaccine. 2018 Jan 4;36(2):273–9. doi: 10.1016/j.vaccine.2017.07.116. [DOI] [PubMed] [Google Scholar]
- 64.Groome MJ, Zell ER, Solomon F, Nzenze S, Parashar UD, Izu A, et al. Temporal Association of Rotavirus Vaccine Introduction and Reduction in All-Cause Childhood Diarrheal Hospitalizations in South Africa. Clin Infect Dis. 2016 May 1;62(Suppl 2):S188–95. doi: 10.1093/cid/civ1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Madhi SA, Kirsten M, Louw C, Bos P, Aspinall S, Bouckenooghe A, et al. Efficacy and immunogenicity of two or three dose rotavirus-vaccine regimen in South African children over two consecutive rotavirus-seasons: a randomized, double-blind, placebo-controlled trial. Vaccine. 2012 Apr 27;30(Suppl 1):A44–51. doi: 10.1016/j.vaccine.2011.08.080. [DOI] [PubMed] [Google Scholar]
- 66.Vesikari T, Karvonen A, Ferrante SA, Ciarlet M. Efficacy of the pentavalent rotavirus vaccine, RotaTeq(R), in Finnish infants up to 3 years of age: the Finnish Extension Study. Eur J Pediatr. 2010 Nov;169(11):1379–86. doi: 10.1007/s00431-010-1242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cunliffe NA, Witte D, Ngwira BM, Todd S, Bostock NJ, Turner AM, et al. Efficacy of human rotavirus vaccine against severe gastroenteritis in Malawian children in the first two years of life: a randomized, double-blind, placebo controlled trial. Vaccine. 2012 Apr 27;30(Suppl 1):A36–43. doi: 10.1016/j.vaccine.2011.09.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zaman K, Fleming JA, Victor JC, Yunus M, Bari TI, Azim T, et al. Noninterference of Rotavirus Vaccine With Measles-Rubella Vaccine at 9 Months of Age and Improvements in Antirotavirus Immunity: A Randomized Trial. J Infect Dis. 2016 Jun 1;213(11):1686–93. doi: 10.1093/infdis/jiw024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.PATH. Immune Response to Rotavirus Vaccine After a Supplemental Dose Given at 9 Months of Age With Local EPI Vaccines in Mali 18 August 2015 ed. ClinicalTrials.gov. 2015 https://clinicaltrials.gov/ct2/show/NCT02286895.
- 70.Richardson V, Hernandez-Pichardo J, Quintanar-Solares M, Esparza-Aguilar M, Johnson B, Gomez-Altamirano CM, et al. Effect of rotavirus vaccination on death from childhood diarrhea in Mexico. N Engl J Med. 2010 Jan 28;362(4):299–305. doi: 10.1056/NEJMoa0905211. [DOI] [PubMed] [Google Scholar]
- 71.do Carmo GM, Yen C, Cortes J, Siqueira AA, de Oliveira WK, Cortez-Escalante JJ, et al. Decline in diarrhea mortality and admissions after routine childhood rotavirus immunization in Brazil: a time-series analysis. PLoS Med. 2011 Apr;8(4):e1001024. doi: 10.1371/journal.pmed.1001024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Burnett E, Jonesteller CL, Tate JE, Yen C, Parashar UD. Global Impact of Rotavirus Vaccination on Childhood Hospitalizations and Mortality From Diarrhea. J Infect Dis. 2017 Jun 1;215(11):1666–72. doi: 10.1093/infdis/jix186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Leshem E, Tate JE, Steiner CA, Curns AT, Lopman BA, Parashar UD. National Estimates of Reductions in Acute Gastroenteritis-Related Hospitalizations and Associated Costs in US Children After Implementation of Rotavirus Vaccines. J Pediatric Infect Dis Soc. 2017 Aug 10; doi: 10.1093/jpids/pix057. pix057. [DOI] [PubMed] [Google Scholar]
- 74.Shah MP, Tate JE, Mwenda JM, Steele AD, Parashar UD. Estimated reductions in hospitalizations and deaths from childhood diarrhea following implementation of rotavirus vaccination in Africa. Expert Rev Vaccines. 2017 Oct;16(10):987–95. doi: 10.1080/14760584.2017.1371595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rotavirus vaccines. WHO position paper - January 2013. Wkly Epidemiol Rec. 2013 Feb 1;88(5):49–64. [PubMed] [Google Scholar]
- 76.Peter G, Myers MG National Vaccine Advisory C, National Vaccine Program O. Intussusception, rotavirus, and oral vaccines: summary of a workshop. Pediatrics. 2002 Dec;110(6):e67. doi: 10.1542/peds.110.6.e67. [DOI] [PubMed] [Google Scholar]
- 77.Parashar UD, Alexander JP, Glass RI Advisory Committee on Immunization Practices CfDC, Prevention. Prevention of rotavirus gastroenteritis among infants and children. Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2006 Aug 11;55(RR-12):1–13. [PubMed] [Google Scholar]
- 78.Murphy TV, Gargiullo PM, Massoudi MS, Nelson DB, Jumaan AO, Okoro CA, et al. Intussusception among infants given an oral rotavirus vaccine. N Engl J Med. 2001 Feb 22;344(8):564–72. doi: 10.1056/NEJM200102223440804. [DOI] [PubMed] [Google Scholar]
- 79.Patel MM, Haber P, Baggs J, Zuber P, Bines JE, Parashar UD. Intussusception and rotavirus vaccination: a review of the available evidence. Expert Rev Vaccines. 2009 Nov;8(11):1555–64. doi: 10.1586/erv.09.106. [DOI] [PubMed] [Google Scholar]
- 80.Belongia EA, Irving SA, Shui IM, Kulldorff M, Lewis E, Yin R, et al. Real-time surveillance to assess risk of intussusception and other adverse events after pentavalent, bovine-derived rotavirus vaccine. Pediatr Infect Dis J. 2010 Jan;29(1):1–5. doi: 10.1097/INF.0b013e3181af8605. [DOI] [PubMed] [Google Scholar]
- 81.Shui IM, Baggs J, Patel M, Parashar UD, Rett M, Belongia EA, et al. Risk of intussusception following administration of a pentavalent rotavirus vaccine in US infants. JAMA. 2012 Feb 8;307(6):598–604. doi: 10.1001/jama.2012.97. [DOI] [PubMed] [Google Scholar]
- 82.Weintraub ES, Baggs J, Duffy J, Vellozzi C, Belongia EA, Irving S, et al. Risk of intussusception after monovalent rotavirus vaccination. N Engl J Med. 2014 Feb 6;370(6):513–9. doi: 10.1056/NEJMoa1311738. [DOI] [PubMed] [Google Scholar]
- 83.Carlin JB, Macartney KK, Lee KJ, Quinn HE, Buttery J, Lopert R, et al. Intussusception risk and disease prevention associated with rotavirus vaccines in Australia’s National Immunization Program. Clin Infect Dis. 2013 Nov;57(10):1427–34. doi: 10.1093/cid/cit520. [DOI] [PubMed] [Google Scholar]
- 84.Patel MM, Lopez-Collada VR, Bulhoes MM, De Oliveira LH, Bautista Marquez A, Flannery B, et al. Intussusception risk and health benefits of rotavirus vaccination in Mexico and Brazil. N Engl J Med. 2011 Jun 16;364(24):2283–92. doi: 10.1056/NEJMoa1012952. [DOI] [PubMed] [Google Scholar]
- 85.Yih WK, Lieu TA, Kulldorff M, Martin D, McMahill-Walraven CN, Platt R, et al. Intussusception risk after rotavirus vaccination in U.S. infants. N Engl J Med. 2014 Feb 6;370(6):503–12. doi: 10.1056/NEJMoa1303164. [DOI] [PubMed] [Google Scholar]
- 86.Stowe J, Andrews N, Ladhani S, Miller E. The risk of intussusception following monovalent rotavirus vaccination in England: A self-controlled case-series evaluation. Vaccine. 2016 Jul 12;34(32):3684–9. doi: 10.1016/j.vaccine.2016.04.050. [DOI] [PubMed] [Google Scholar]
- 87.Rosillon D, Buyse H, Friedland LR, Ng SP, Velazquez FR, Breuer T. Risk of Intussusception After Rotavirus Vaccination: Meta-analysis of Postlicensure Studies. Pediatr Infect Dis J. 2015 Jul;34(7):763–8. doi: 10.1097/INF.0000000000000715. [DOI] [PubMed] [Google Scholar]
- 88.Kim KY, Kim DS. Relationship between Pentavalent Rotavirus Vaccine and Intussusception: A Retrospective Study at a Single Center in Korea. Yonsei Med J. 2017 May;58(3):631–6. doi: 10.3349/ymj.2017.58.3.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Patel MM, Clark AD, Glass RI, Greenberg H, Tate J, Santosham M, et al. Broadening the age restriction for initiating rotavirus vaccination in regions with high rotavirus mortality: benefits of mortality reduction versus risk of fatal intussusception. Vaccine. 2009 May 14;27(22):2916–22. doi: 10.1016/j.vaccine.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 90.Wu D, Yen C, Yin ZD, Li YX, Liu N, Liu YM, et al. The Public Health Burden of Rotavirus Disease in Children Younger Than Five Years and Considerations for Rotavirus Vaccine Introduction in China. Pediatr Infect Dis J. 2016 Dec;35(12):e392–e8. doi: 10.1097/INF.0000000000001327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Luna EJ, Frazatti-Gallina NM, Timenetsky MC, Cardoso MR, Veras MA, Miraglia JL, et al. A phase I clinical trial of a new 5-valent rotavirus vaccine. Vaccine. 2013 Feb 4;31(7):1100–5. doi: 10.1016/j.vaccine.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 92.Bines JE, Danchin M, Jackson P, Handley A, Watts E, Lee KJ, et al. Safety and immunogenicity of RV3-BB human neonatal rotavirus vaccine administered at birth or in infancy: a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2015 Dec;15(12):1389–97. doi: 10.1016/S1473-3099(15)00227-3. [DOI] [PubMed] [Google Scholar]
- 93.Steele AD, Madhi SA, Cunliffe NA, Vesikari T, Phua KB, Lim FS, et al. Incidence of rotavirus gastroenteritis by age in African, Asian and European children: Relevance for timing of rotavirus vaccination. Hum Vaccin Immunother. 2016 Sep;12(9):2406–12. doi: 10.1080/21645515.2016.1179412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Parashar UD, Holman RC, Cummings KC, Staggs NW, Curns AT, Zimmerman CM, et al. Trends in intussusception-associated hospitalizations and deaths among US infants. Pediatrics. 2000 Dec;106(6):1413–21. doi: 10.1542/peds.106.6.1413. [DOI] [PubMed] [Google Scholar]
- 95.Armah GE, Kapikian AZ, Vesikari T, Cunliffe N, Jacobson RM, Burlington DB, et al. Efficacy, immunogenicity, and safety of two doses of a tetravalent rotavirus vaccine RRV-TV in Ghana with the first dose administered during the neonatal period. J Infect Dis. 2013 Aug 1;208(3):423–31. doi: 10.1093/infdis/jit174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yen C, Tate JE, Hyde TB, Cortese MM, Lopman BA, Jiang B, et al. Rotavirus vaccines: current status and future considerations. Hum Vaccin Immunother. 2014;10(6):1436–48. doi: 10.4161/hv.28857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Groome MJ, Koen A, Fix A, Page N, Jose L, Madhi SA, et al. Safety and immunogenicity of a parenteral P2-VP8-P[8] subunit rotavirus vaccine in toddlers and infants in South Africa: a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2017 Aug;17(8):843–53. doi: 10.1016/S1473-3099(17)30242-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sullivan SP, Koutsonanos DG, Del Pilar Martin M, Lee JW, Zarnitsyn V, Choi SO, et al. Dissolving polymer microneedle patches for influenza vaccination. Nat Med. 2010 Aug;16(8):915–20. doi: 10.1038/nm.2182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Edens C, Collins ML, Ayers J, Rota PA, Prausnitz MR. Measles vaccination using a microneedle patch. Vaccine. 2013 Jul 25;31(34):3403–9. doi: 10.1016/j.vaccine.2012.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Moon S, Wang Y, Edens C, Gentsch JR, Prausnitz MR, Jiang B. Dose sparing and enhanced immunogenicity of inactivated rotavirus vaccine administered by skin vaccination using a microneedle patch. Vaccine. 2013 Jul 25;31(34):3396–402. doi: 10.1016/j.vaccine.2012.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]