Abstract
Objective
Investigate the impact of nursing home information technology sophistication on publically reported health safety deficiency scores documented during standard inspections.
Methods
The sample included 807 NHs from every US state. A total of 2187 health inspections were documented in these facilities. A national IT sophistication survey describing IT capabilities, extent of IT use, and degree of IT integration in resident care, clinical support, and administrative activities in US NHs was used. The relationship between NH health deficiencies and IT sophistication survey scores were examined, using weighted regression.
Results
Controlling for RN hours per resident day, deficiency scores decreased as total IT sophistication increased. Controlling for total IT sophistication score, deficiency scores decreased as RN hours per resident day increased. Ownership status significantly influenced health deficiency scores.
Conclusions
These results highlight the necessity to understand benefits of implementing NH IT and demonstrating its impact on patient safety.
Keywords: quality measurement, patient safety, surveys
INTRODUCTION
Quality of care in nursing home (NH) facilities is regulated by a set of standards at both federal and state levels(1). Compliance with these standards is monitored by state regulatory agencies through yearly standard and compliance-driven inspections. The results of these inspections provide information on health care deficiencies, related to the overall standard of care provided by NHs nationally. A 2015 assessment of long-term care facilities found that the percentage of NHs in a substandard quality of care classification had declined to 3.2% in 2014; however, the percentage of deficiencies graded at actual harm levels that were in a more severe category (G-L) (Table 1) had increased to 10.6%(2). In September 2016, growing awareness of continued substandard care led the Centers for Medicare and Medicaid to implement mandatory remedies and assessment factors to determine seriousness of health deficiencies in NH(3). The three most cited deficiencies included having a program that investigates, controls and keeps infection from spreading, food safety, and that NHs are free from accident hazards and prevent avoidable accidents(2). More sophisticated mechanisms are needed to reduce deficiencies and improve patient safety in NHs to protect the 1.5 million residents nationally, whose average length of stay is just over 2 years, and that reside in 1.7 million beds in over 16,000 US facilities(4).
Table 1.
Health Inspection Score: Weights for Different Type of Deficiencies
| Scope | |||
|---|---|---|---|
| Severity | Isolated | Pattern | Widespread |
| Immediate jeopardy to resident health or safety | J 50 points |
K 100 points |
L 150 points |
| Actual harm that is not immediate jeopardy | G 20 points |
H 35 points |
I 45 points |
| No actual harm with potential for more than minimal harm that is not immediate jeopardy | D 4 points |
E 8 points |
F 16 points |
| No actual harm with potential for minimal harm | A 0 points |
B 0 points |
C 0 points |
Source: Centers for Medicare & Medicaid
Shaded areas denote deficiency scope/severity levels that constitute substandard quality of care
One hope for improving patient safety in NH settings is integration of sophisticated health information technology (IT) systems into clinical care(5). The Institute of Medicine indicates the degree of impact of health IT on patient safety is limited because of the diversity of organizational environments and information systems used(6). Organizational factors in health systems influence administrative decisions about implementation and adoption of health IT, which leads to greater diversity across systems(7). Understanding this limitation is even more pronounced in NHs nationally, because there is insufficient reporting of some organizational variables, such as current IT capabilities, extent of IT use, and IT integration. Furthermore, links between IT adoption and patient safety, such as health deficiencies in NH settings, has not been consistently studied nationally.
BACKGROUND
Conceptual Models in IT Maturity
Information systems in healthcare have made enormous progress the past few years. Technological innovation in the U.S. has been supported politically in recent years by meaningful use, which was legislation instituted to provide much needed incentives for hospitals and providers in ambulatory clinics to promote adoption and use of IT for patient care delivery(8). Similar incentives to stimulate innovation in post-acute care, such has NHs, were not provided. Regardless, innovations in healthcare IT in all healthcare sectors has resulted in the development of IT maturity models which are used to understand how people, organizations, and processes develop and mature over time through various growth stages(9). Staging within an IT maturity model are influenced by a number of factors including IT implementation strategies used by healthcare leadership, centralization or decentralization of IT systems within an organization, staffing including IT personnel, leadership styles incorporated into project management teams, and skills that leaders possess(10).
Most maturity models being used to guide management strategies for IT implementation include those for acute care organizations. For example, the Electronic Healthcare Maturity Model by Quintegra incorporates progress made in IT maturity through characteristics, such as timeliness of process, data access, efficiency of effort, cost effectiveness, quality of process, and value to stakeholders(11). Another popular IT maturity model includes the Health Information Management Systems Society’s (HIMSS) eight stage Electronic Medical Record Adoption Model (EMRAM) for hospitals which is a model used by organizational leaders to analyze their current situation, document accomplishments, and compare progress with other healthcare organizations(12). In post-acute care, there have been preliminary IT maturity models proposed including a 7-Stage Electronic Health Record Adoption Model for Long-Term and Post-Acute care being published by LeadingAge’s Center for Aging Services Technologies (CAST) (13). The purpose of this model is to provide a framework for leaders to evaluate IT use and adoption in their organizations.
Gaps remain in our understanding of how existing IT maturity models truly impact quality. For example, there are very few rigorous evaluations incorporating measures of NH IT use as independent variables and long established NH quality measures as dependent variables. Furthermore, existing studies with these types of measures are limited in scope by number of facilities and geographic spread. Larger research studies, incorporating nationally representative samples of NHs with diversity of IT use are needed to determine widespread effects of IT sophistication on quality. The current research surveyed a nationally representative sample to measure NH IT sophistication, which is linked to IT maturity. Total IT sophistication measures were used to examine relationships between deficiencies found during standard NH health inspections. The specific aim and research question for this research was:
Specific Aim: Investigate relationships between total NH IT sophistication and deficiencies found during standard NH health inspections in a national sample.
Research Question: Do relationships exist between total NH IT sophistication and deficiencies found during standard NH health inspections in a national sample?
METHODS
IT Sophistication Measure
The IT sophistication survey, developed by the primary author through a series of rigorous studies, measures 3 IT sophistication dimensions (IT capabilities, extent of IT use, IT integration) in 3 healthcare domains (resident care, clinical support, and administrative activities)(14–17). The IT Sophistication instrument is reliable, with good internal consistency in each healthcare domain including: Resident Care, .87-.88; Clinical Support, .86-.91; and Administrative Activities, .69-.80(17). Additionally, the IT sophistication instrument has been field tested using extensive observations of communication activities about pressure ulcer preventions used by NH staff in facilities with diverse IT sophistication measures(18). Results of these field tests verified that increased NH IT sophistication enhances efficiency in clinical workflow among nursing facility staff in NH with high and low levels of IT sophistication. The change in total and unique interactions among staff resulted in enhanced workflow and efficiencies in facilities with high levels of IT sophistication. Enhanced nursing staff workflow and efficiency leads to better quality(19).
Health Deficiency Measures
NH quality indices, captured in a national public database called NH Compare, contain measures with weighted health inspection scores about health deficiencies discovered during standard state health inspections or investigations following a complaint(20). Health deficiencies are recorded by state surveyors in NH Compare. Surveyors rate the severity of each deficiency within 4 classifications ranging from no actual harm with potential for minimal harm, to immediate jeopardy to resident health or safety. Furthermore, surveyors rate each health deficiency into 3 classes ranging from isolated to widespread incidents. A point system is used to classify deficiencies into one of 12 (4X3) classes (Table 1). More points acquired by a facility during health inspections means that deficiencies have greater severity with wider scope of occurrence. Health deficiencies found during standard inspections were included in this analysis, while those found during complaint investigations were excluded.
Sample
These data are derived from a national study of NH IT adoption, using an IT sophistication survey, conducted January 2014-July 2015 involving 815 NHs from every state in the US(21). Health deficiency scores were computed for 815 NHs participating in the national IT sophistication survey. NHs were excluded if identified as special focus homes (those with pre-existing quality problems); located in Guam, Puerto Rico or Virgin Islands; or if deficiency surveys were 2 or more years before completion of the IT survey. After applying inclusion/exclusion criteria there were 807 NHs with usable IT sophistication survey and health deficiency data included in the analysis.
Analysis
In this study, we analyzed whether the NH total IT sophistication score predicted the health deficiency score of the NH reported during standard safety inspections, controlling for NH staffing, bed-size, location, and ownership. For staffing, NH hours per resident day for registered nurses (RNs), licensed practical nurses (LPNs), and certified nurse aides (CNAs) were obtained from NH Compare. Rural-Urban Commuting Area Codes using ZIP Code information were used to classify the homes into 4 regional locations based on population size including: Metropolitan >50,000; Micropolitan 10,000-49,999; Small town 2,500-9,999; and Rural <2,500. Bed-size was collapsed into three categories including small (<60 beds), medium (60-120), and large (>120). We collapsed the type of ownership into two categories, including for-profit and non-profit NHs (non-profit included NHs with a government classification in NH Compare).
The total health deficiency scores were highly skewed; therefore, the analysis was done using the log transformation of the total deficiency score. The correlation estimates were found by taking the square root of the multiple R-square obtained from the weighted regression analysis. Specifically, the SURVEYREG procedure of SAS v9 (SAS Institute Inc., Cary, NC, USA) was used for this analysis. Procedures were approved by the university’s ethics board (IRB #1209004 HS).
RESULTS
Table 2 presents the mean and median IT scores that NH administrators reported in each IT sophistication dimension and healthcare domain. In this sample, the highest median IT sophistication score includes technologies used in administrative activities which are integrated internally and externally with other IT systems (e.g. IT backup systems). The lowest IT sophistication score was in use of clinical support technologies (e.g. laboratory and pharmacy) which are integrated internally and externally with other IT systems. In 6 of the 9 categories measuring IT sophistication, at least one NH administrator reported the maximum possible score achievable on the survey (100). Conversely, at least one nursing facility administrator reported the lowest possible score, which was 0 (meaning no technology was present) in 8 out of the 9 dimensions and domains of IT sophistication.
Table 2.
NH IT Sophistication Scores (n=807 Nursing Homes)
| Mean | Median | Std. Dev | Min | Max | |
|---|---|---|---|---|---|
| Administrative Activities | |||||
| IT capabilities | 40.9 | 42.5 | 23.9 | 0.0 | 100.0 |
| Extent of IT Use | 36.0 | 35.9 | 15.7 | 0.0 | 94.2 |
| IT Integration | 47.9 | 48.1 | 16.1 | 9.0 | 93.7 |
|
| |||||
| Resident Care | |||||
| IT capabilities | 43.5 | 42.8 | 21.5 | 0.0 | 100.0 |
| Extent of IT Use | 29.3 | 29.3 | 17.7 | 0.0 | 98.4 |
| IT Integration | 44.9 | 44.0 | 28.1 | 0.0 | 100.0 |
|
| |||||
| Clinical Support | |||||
| IT capabilities | 23.4 | 17.6 | 24.1 | 0.0 | 100.0 |
| Extent of IT Use | 19.3 | 11.9 | 22.0 | 0.0 | 100.0 |
| IT Integration | 14.7 | 0.0 | 22.9 | 0.0 | 100.0 |
|
| |||||
| Total IT Sophistication | 299.9 | 281.5 | 142.1 | 24.8 | 833.0 |
About half of the homes completed IT Sophistication surveys within 109 days (about 3.5 months) of their health inspection. In the 807 NHs there were 2187 health inspections documented. Only 11 (1.3%) of the homes in the study had no deficiencies reported. The top 10 most frequently cited health deficiency tags for our sample are listed in Table 3. Nursing facilities in the sample completing the IT sophistication survey have similar numbers of health deficiency citations (within 1%) as non- sample facilities that did not participate in the national survey. The most frequent citation in the sample facilities was related to infection control programs. The relative frequency of the scope and severity of the health citation tags in the sample are listed in Table 4. The majority of the deficiency tags are within scope and severity level of D. At this level, deficiencies have isolated occurrences ranging from no actual harm to having potential for more than minimal harm that is not immediate jeopardy (see Table 1). The most frequent tag with a scope and severity level of D relates to qualified persons providing care according to each resident’s written plan of care. However, there are several facilities that have health citations tagged with scope and severity levels of F or higher, which indicates widespread occurrence of deficiencies with no actual harm with potential for more than minimal harm that is not immediate jeopardy. In particular, 4% of the health citations for tag number 323 had a scope and severity of J or higher, which is isolated to wide spread occurrences of deficiencies that have immediate jeopardy to patients. Tag number 323 is issued when a facility has not ensured that nursing home areas are free from accident hazards and are not providing adequate supervision to prevent avoidable accidents.
Table 3.
Top 10 Health Deficiency Tags in Non-sample and Sample Nursing Facilities
| Deficiency Description [tag ID number] | Non-sample facilities | Sample facilities | Total | ||
|---|---|---|---|---|---|
| Frequency | Percenta | Frequency | Percenta | ||
| Have a program that investigates, controls, and keeps infection from spreading. [0441] | 16,496 | 6.53 | 897 | 6.71 | 17,393 |
| Store, cook, and serve food in a safe and clean way. [0371] | 15,654 | 6.20 | 821 | 6.14 | 16,475 |
| Ensure that a nursing home area is free from accident hazards and provide adequate supervision to prevent avoidable accidents. [0323] | 12,851 | 5.09 | 716 | 5.35 | 13,567 |
| Provide necessary care and services to maintain or improve the highest well-being of each resident. [0309] | 10,785 | 4.27 | 585 | 4.37 | 11,370 |
| Ensure that each resident’s 1) entire drug/medication regimen is free from unnecessary drugs; and 2) is managed and monitored to achieve highest level of well-being. [0329] | 9,922 | 3.93 | 550 | 4.11 | 10,472 |
| Maintain drug records and properly mark/label drugs and other similar products according to accepted professional standards. [0431] | 9,174 | 3.63 | 489 | 3.66 | 9,663 |
| Develop a complete care plan that meets all the resident’s needs, with timetables and actions that can be measured. [0279] | 8,821 | 3.49 | 483 | 3.61 | 9,304 |
| Provide care for residents in a way that maintains or improves their dignity and respect in full recognition of their individuality. [0241] | 6,841 | 2.71 | 357 | 2.67 | 7,198 |
| Keep accurate, complete and organized clinical records on each resident that meet professional standards. [0514] | 6,575 | 2.60 | 349 | 2.61 | 6,924 |
| Provide care by qualified persons according to each resident’s written plan of care. [0282] | 5,947 | 2.36 | 318 | 2.38 | 6,265 |
Frequency of occurrence of a given tag relative to the total number of tags within Non-sample facilities or within Sample facilities.
Table 4.
Relative frequencya and scope of the top 10 deficiencies for the nursing facilities participating in this study
| Deficiency Tagb | Scope of Severity
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B | C | D | E | F | G | H | I | J | K | L | |
| 0441 | 0.33 | 0.45 | 44.04 | 42.14 | 12.71 | 0 | 0 | 0 | 0.11 | 0.11 | 0.11 |
| 0371 | 0.24 | 0.73 | 12.55 | 32.64 | 53.47 | 0 | 0 | 0 | 0.37 | 0 | 0 |
| 0323 | 0.14 | 0.14 | 48.74 | 36.45 | 0.14 | 10.2 | 0.14 | 0 | 2.93 | 0.84 | 0.28 |
| 0309 | 0.17 | 0 | 70.26 | 20 | 0 | 8.03 | 0.17 | 0 | 1.2 | 0.17 | 0 |
| 0329 | 0 | 0 | 69.82 | 29.45 | 0 | 0.55 | 0 | 0 | 0 | 0.18 | 0 |
| 0431 | 1.02 | 1.02 | 51.74 | 41.51 | 4.7 | 0 | 0 | 0 | 0 | 0 | 0 |
| 0279 | 0.62 | 0 | 76.4 | 20.08 | 2.69 | 0 | 0 | 0 | 0 | 0.21 | 0 |
| 0241 | 1.12 | 0.28 | 62.75 | 34.17 | 0.28 | 1.12 | 0.28 | 0 | 0 | 0 | 0 |
| 0514 | 5.44 | 0.86 | 65.04 | 24.36 | 3.72 | 0 | 0 | 0 | 0.29 | 0 | 0.29 |
| 0282 | 0.31 | 0 | 74.53 | 17.92 | 2.2 | 3.46 | 0 | 0 | 1.26 | 0 | 0.31 |
The frequency of occurrence of a given scope level relative to the total number of deficiencies with that tag among Sample homes
For descriptions of deficiency tags see Table 3
The mean deficiency score for our sample was 42.9(22). Study nursing homes had a mean of 6.2 total deficiencies. Non-study homes across the U.S. were comparable, but had slightly worse health deficiencies, reporting a mean total deficiency score of 43.9 and an average count of 6.4 deficiencies.
To get a visual picture of the relationship between total IT sophistication and deficiency variables, box plots of total health deficiency scores were diagramed with deciles of increasing IT sophistication (Figure 1). For the first decile, with the lowest total IT sophistication scores ranging from 0 to 129 the median total deficiency score was 32. Nursing homes reporting the highest total IT sophistication, greater than 487 and in the 10th decile, had a median health deficiency score of 24. Figure 1 includes a line connecting estimated mean values for total deficiency scores based on regression on the total IT sophistication score. The median deficiency count for all homes ranged from 4-6, across all deciles, indicating there was not much difference in the total deficiency counts documented, but they appeared to be less severe and more isolated as total IT sophistication increased.
Figure 1.
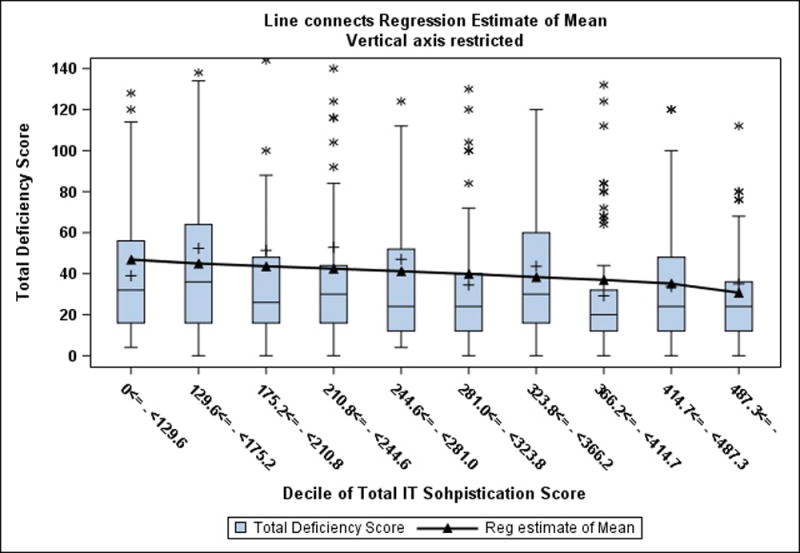
Boxplot of Nursing Home Total Deficiency Score versus Decile of Total IT Sophistication Score
In other analyses, the correlation of the deficiency score with total IT sophistication score is −0.07 which is weak, but approaching significance (p=.06). Additional analysis included correlations between deficiency scores and RN, LPN, and CNA adjusted staffing hour’s per/resident/day. The estimated correlations for CNA and LPN hours/resident/day were small and not statistically significant (p> 0.60). For RN adjusted hours, the estimated correlation was −0.11(p= .007). Consequently, in subsequent analysis we used only RN adjusted hours. For bed-size, the p-value was .07, which was not quite significant; however, there was some evidence that small homes have better scores than medium or large homes. There was no evidence of differences based on location in this sample (p=.25). There is evidence that non-profit homes do better than for-profit (p=.0005). The mean health deficiency scores were 31 and 46, while the medians were 20 and 25 for non-profit and for-profit homes respectively.
To examine the joint effect of the independent variables, a model was fit with total IT sophistication, RN adjusted hours, and ownership status included as predictor variables and the log of the deficiency score as the dependent variable. In this model, all p-values were less than .10 with for-profit status being highly significant (p=.007). Although the coefficients for RN adjusted hours and total IT sophistication were not significant at the 0.05 level, we examined this model further to get estimates of the effect on the deficiency score for each of these variables. Since RN adjusted hours and total IT sophistication are continuous, the effect of each one was examined while holding the other fixed at its median value, .5 RN hours/resident/day and total IT sophistication score of 290, respectively. Based on the least squares means estimates for the effect of ownership, the estimated deficiency scores are exp(3.33)=28.1 for for-profit ownership and exp(3.12)=22.7 for non-profit. The graphs and values in Figures 2 and 3 give some idea as to the effect of RN for other variables fixed as well as total IT sophistication for other variables fixed. The range of values on the horizontal axis was chosen to include about 90% of the observed values. In terms of the amount of variation explained by IT as opposed to other predictors, the multiple R-square with RN and For-Profit (but no IT) is 0.02. When IT is added there is a small increase to 0.03. Using only IT the R-Square is 0.01.
Figure 2.
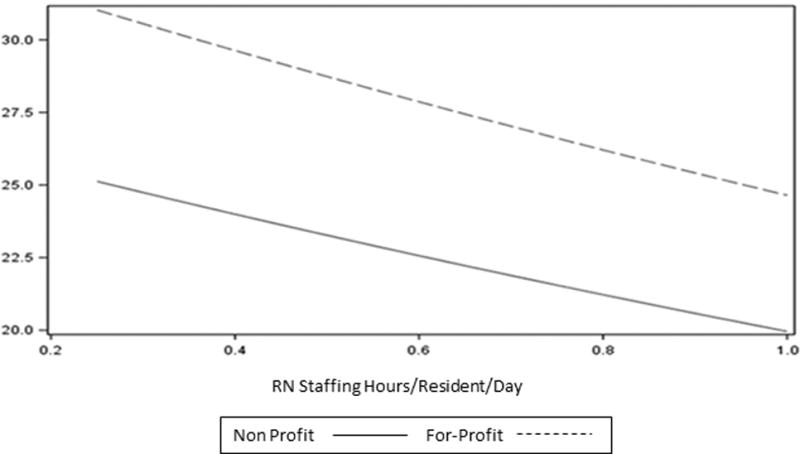
Estimated deficiency score as a function of RN staffing hours/resident/day for median total IT sophistication score =290
Figure 3.
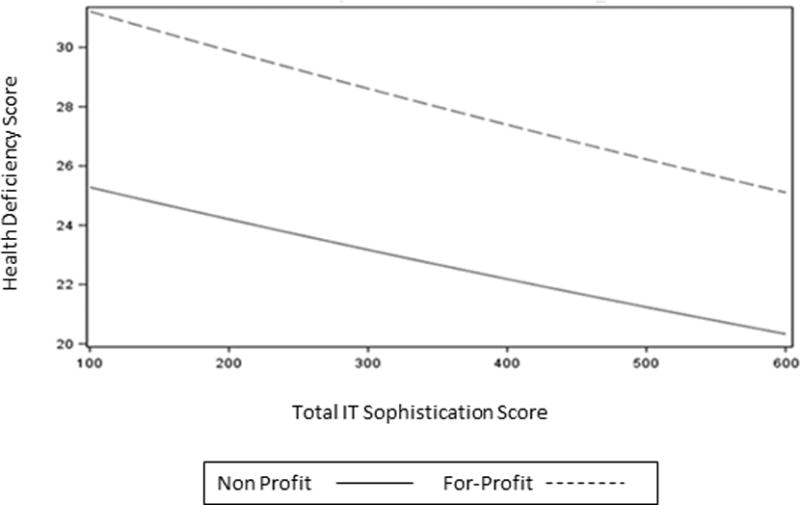
Estimated deficiency score as a function of total IT sophistication for median RN staffing hours = 0.5 hours per resident day
DISCUSSION
Current assessments of NH quality nationally continue to identify inadequacies and substandard care delivery(23). Although recent NH data compendiums show improvements over the past 10 years(2). One hope for better NH quality is health IT. Millions of dollars have been spent incentivizing IT implementation since 2009(8). The benefits of infusing financial resources for health IT are being realized in acute and ambulatory healthcare markets, but not as much in NHs, which has been ineligible for the same incentives. However, according to prior studies about NH IT use, especially in resident care, even without incentives, IT use in these settings is becoming more common(21;24). Our findings have been confirmed in other studies. For example, nursing facilities with higher Medicare populations, which have wider profit margins, also tend to have greater IT adoption rates than facilities with higher Medicaid patients, which have lower profit margins(25). Nevertheless, current models tracking health IT adoption nationally, called Maturity Models, are insufficient because they only capture information from acute care organizations, resulting in only partial estimates of the real impact of regulated incentives(9;26). Furthermore, these models have not been linked with quality measures, which is the ultimate desired outcome.
This research examined the hypothesis that increased IT sophistication would result in lower overall health deficiency scores in a national sample of NHs. The subtle shift in health deficiency scores with a downward trend as IT sophistication increases in Figure 1 seems to support the hypothesis. To corroborate this evidence, more rigorous models were tested. Ownership status appears to have the most significant effect on reducing health deficiency scores, with not for-profit homes having lower deficiency scores. When RN hours/resident/day is held constant, the model predicts that homes will have lower deficiency scores as total IT sophistication increases. Similarly, as total IT sophistication is held constant, when RN hours/resident/day is increased deficiency scores are predicted to be lower.
These results suggest that the IT Sophistication survey instrument may be capable of identifying areas of technology innovation which impact quality, as evidenced by changes in health deficiency scores. The identification of specific dimensions and domains of IT sophistication can provide a more targeted approach to isolating the impacts of increasing technological maturity, which can be linked to improved quality of care more directly. As Accountable Care Organizations flourish, where more stakeholders assume the responsibility for the quality, costs, and care of long term care residents, improvements in quality and decreased health deficiency scores and technology use will become a more valuable characteristic to trend(27).
PRACTICE IMPLICATIONS
Providing safer environments for residents in nursing homes has been a significant issue for many years. Although, gains in safety have been achieved nationally in nursing homes, there continues to be serious concerns, especially related to the occurrence of widespread and severe safety incidents resulting in immediate jeopardy to residents. IT is a tool that health administrators and managers can choose to implement to reduce safety concerns and improve quality of care. However, there are few studies reporting how health IT impacts safety in nursing homes that can be used by leaders to help make decisions about adoption. Generalizable studies are needed in the literature to inform leaders about the effect growing IT maturity may have on safety and quality.
In this study, which has national representation of nursing homes from each state, health deficiency scores appear to be trending in a positive, downward direction as health IT matures across settings. Historically, most technologies in these settings have been implemented in administrative billing and procurement activities; however, in this sample health IT seems to have a significant presence in resident care activities too. Maturing IT systems in resident care activities have an impact on care planning activities and communication between staff. For example, IT systems in resident care that optimize communication between caregivers may increase awareness of necessary care planning activities, such as turning and repositioning, which may be time critical to avoid pressure ulcer formation (tag 279). In this sample, 76% of health deficiencies for tag 279 were isolated events with no harm, which may have been influenced by IT maturity in resident care. However, there is room for improvement. The health deficiency tag with the highest percentage of occurrence in this sample was related to infection control. It is interesting that clinical support technologies, which includes laboratory results reporting in the IT sophistication survey used for this study, was found to have the lowest levels of capability, use, and integration across all facilities. An assumption could be made that clinical support technologies with laboratory capabilities that are used and integrated into clinical activities might enable leaders to optimize tracking mechanisms for residents susceptible to infections, allow them investigate the occurrence of infections, and implement controls to prevent infection rates, thereby making the environment safer and of higher quality for residents.
LIMITATIONS
We recognize that a failure to account for biases in our study can have important consequences that could lead to faulty conclusions about theoretical propositions we have made about the influence of IT sophistication on quality measures(28). For example, NHs that participated in the IT sophistication survey may have a vested interest by being early IT adopters. Inclusion of NHs at all stages of adoption is necessary to be able to determine true relationships between increasing IT sophistication and quality of care. To encourage participation our research team provided assistance as needed by scheduling additional follow-up with NH respondents that had questions about some survey items, until the respondents were satisfied with their level of comprehension of survey questions. Our methods also included important exclusion criteria in order to have similar homes in the sample based on current quality improvement initiatives. For example, we excluded all the NHs that were special focus homes Approximately 1.2% of the NHs nationally were considered Special Focus Facilities in Jan 2013(29).
CONCLUSION
National assessments of NH IT are beneficial because they facilitate discoveries that would not otherwise be known. In this research, we have seen evidence in a national study that health deficiency scores may be lower as NH total IT sophistication and RN staffing hours/resident/day increase. This is especially true in non-profit NHs. These results further highlight the necessity of creating tools to better understand the benefits and costs of implementing health IT and demonstrating its impact on patient safety in NHs.
Acknowledgments
The authors would like to thank Mrs. Keely Wise for her excellent organizational skills and leadership on this project.
Funding: This project was supported by grant number R01HS022497 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
Conflict of Interest: None to declare
Contributor Information
Gregory L. Alexander, Professor, University of Missouri, S415 Sinclair School of Nursing, Columbia, MO, USA 65211.
Richard W. Madsen, Medical Research Office, University of Missouri, Columbia, MO, USA.
Reference List
- 1.Centers for Medicare and Medicaid. Centers for Medicare and Medicaid Survey and Certification. https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/nhs.html Accessed 2016 May 19.
- 2.Centers for Medicare & Medicaid Nursing Home Data Compendium. 2015 Edition. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/Downloads/nursinghomedatacompendium_508-2015.pdf Accessed 2017 February 8.
- 3.Centers for Medicare and Medicaid. Mandatory Immediate Imposition of Federal Remedies and Assessment Factors Used to Determine the Seriousness of Deficiencies for Nursing Homes. https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/Survey-and-Cert-Letter-16-31.pdf Accessed 2016 July 29.
- 4.National Center for Health Statistics. Centers for Disease Control and Prevention FastStats Homepage. https://www.cdc.gov/nchs/fastats/nursing-home-care.htm Accessed 2017 February 8.
- 5.Long Term Post Acute Care HIT Collaborative. A Roadmap for Health IT in Long Term and Post Acute Care. Washington DC: American Health Information Management Association; 2015. [Google Scholar]
- 6.Institute of Medicine Health IT and Patient Safety. Building Safer Systems for Better Care. Washington DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 7.Cresswell K, Sheikh A. Organizational issues in the implementation and adoption of health information technology innovations: An interpretative review. International Journal of Medical Informatics. 2013;82(5):e73–e86. doi: 10.1016/j.ijmedinf.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Department of Health and Human Services. Health IT Regulations and Legislation. Office of the National Coordinator; 2016. Available from: URL: https://www.healthit.gov/policy-researchers-implementers/health-it-legislation. Accessed 2017 February 8. [Google Scholar]
- 9.Rocha A. Evolution of information systems and technologies maturity in healthcare. International Journal of Healthcare Information Systems and Informatics. 2011;6(2):28–36. [Google Scholar]
- 10.Galliers RD, Sutherland AR. Information systems management and strategy formulation: the ‘stages of growth’ model revisited. Journal of Information Systems. 1991;1(2):89–114. [Google Scholar]
- 11.Sharma B. Electronic Healthcare Maturity Model (eHMM) http://www.quintegrasolutions.com/eHMM%20White%20Paper.pdf. Accessed 2017 February 8.
- 12.HIMSS. Analytics HIMSS. 2009 Available from: URL: http://www.himssanalytics.org/
- 13.LeadingAge CAST. Electronic Health Records (EHRs) for Long-Term and Post-Acute Care A Primer on Planning and Vendor Selection. http://www.leadingage.org/sites/default/files/EHR_For_LTPAC_A_Primer_on_Planning_and_Vendor_Selection_0.pdf. Accessed 2017 February 8.
- 14.Alexander GL, Wakefield DS. IT sophistication in nursing homes. Journal of the American Medical Directors Association. 2009;10(6):398–407. doi: 10.1016/j.jamda.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alexander GL. A state profile of IT sophistication in nursing homes. Washington DC: American Medical Informatics Association; 2008. pp. 1–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Alexander GL, Madsen R, Wakefield DS. A Regional Assessment of Information Technology Sophistication in Missouri Nursing Homes. Policy, Politics & Nursing Practice. 2010;11(3):214–25. doi: 10.1177/1527154410386616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alexander GL, Steege L, Pasupathy K, Strecker EB. Case Studies of IT Sophistication in Nursing Homes: A Mixed Method Approach to Examine Communication Strategies about Pressure Ulcer Prevention Practices. International Journal of Industrial Engineering. 2015;49:156–66. [Google Scholar]
- 18.Alexander GL, Pasupathy KS, Steege LM, Strecker EB, Carley KM. Multidisciplinary communication networks for skin risk assessment in nursing homes with high IT sophistication. International Journal of Medical Informatics. 2014;83(8):581–91. doi: 10.1016/j.ijmedinf.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cain C, Haque S. Organizational Workflow and its Impact on Quality. In: Hughes Ronda G., editor. Patient Safety and Quality: A Evidence Based Handbook for Nurses. Rockville MD: Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- 20.Antonova E, Zimmerman D. Scope and severity index: a metric for quantifying nursing home survey deficiency number, scope, and severity adjusted for the state-related measurement bias. Journal of the American Medical Directors Association. 2012;13(2):188.e7–188.e12. doi: 10.1016/j.jamda.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Alexander GL, Madsen RW, Miller EL, Schaumber MK, Holm AE, Alexander RL, Wise K, Dougherty M, Gugerty B. A national report of nursing home information technology: Year 1 results. Journal of the American Medical Informatics Association. 2016;24(1):67–73. doi: 10.1093/jamia/ocw051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Medicare & Medicaid Services. Design for Nursing Home Compare five-star quality rating system: Technical users guide. https://www.cms.gov/medicare/provider-enrollment-and-certification/certificationandcomplianc/downloads/usersguide.pdf. Accessed 2017 February 8.
- 23.Ronald LA, McGregor MJ, Harrington C, Pollock A, Lexchin J. Observational evidence of for-profit delivery and inferior nursing home care: When is there enough evidence for policy change? Plos Medicine. 2016;13(4):1–12. doi: 10.1371/journal.pmed.1001995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cherry B, Carter M, Owen D, Lockhart C. Factors affecting electronic health record adoption in long-term care facilities. Journal of Healthcare Quality. 2008;30(2):37–47. doi: 10.1111/j.1945-1474.2008.tb01133.x. [DOI] [PubMed] [Google Scholar]
- 25.Zhang N, Lu S, Xu B, Wu B, Rodriquez-Montquio R, Gurwitz J. Health Information Technologies: Which Nursing Homes Adopted Them? Journal of the American Medical Directors Association. 2016;17(5):441–7. doi: 10.1016/j.jamda.2016.02.028. [DOI] [PubMed] [Google Scholar]
- 26.Vidal Carvalho J, Rocha A, Abreu A. Maturity models of healthcare information systems and technologies: A literature review. Journal of Medical Systems. 2016;40(131) doi: 10.1007/s10916-016-0486-5. [DOI] [PubMed] [Google Scholar]
- 27.Stefanacci RG, Brown G, Reich S. Behind the scenes at nursing facilities. In: Fenstemacher Pamela A, Winn Peter., editors. Post-Acute and Long-Term Medicine. 2nd. Switzerland: Humana Press; 2016. pp. 51–72. [Google Scholar]
- 28.Hamilton BH, Nickerson JA. Correcting for endogeneity in strategic management research. Strategic Organization. 2003;1(1):51–78. [Google Scholar]
- 29.Centers for Medicare & Medicaid Services. Special Focus Facility Initiative. https://www.cms.gov/CertificationandComplianc/Downloads/SFFList.pdf. Accessed 2017 February 8.


