Abstract
Objectives:
The current study investigated whether personality traits and facets were associated with interleukin-6, C-reactive protein, and fibrinogen, and whether physical activity mediated the relationship between personality and biomarkers of inflammation.
Methods:
Personality was assessed in the Midlife Development in the United States study using the Multi-Dimensional Personality Questionnaire and Midlife Development Inventory personality scale. Data were included from 960 participants (mean age = 57.86 years, standard deviation = 11.46). Personality was assessed from 2004 to 2009. Serum levels of interleukin-6, fibrinogen, and C-reactive protein were assessed in 2005–2009 as part of the Midlife Development in the United States biomarkers subproject.
Results:
Lower neuroticism was associated with elevated interleukin-6, and achievement was associated with lower fibrinogen. Higher physical activity was associated with lower interleukin-6 and C-reactive protein. Mediation models suggested that physical activity mediated the associations between achievement and both interleukin-6 and C-reactive protein.
Discussion:
Physical activity is an important factor in the Health Behavior Model of personality and explains some of the associations between personality and inflammation. These findings contribute to the fields of aging and health by linking individual difference factors to markers of inflammation, and showing that these processes may function partially through specific behaviors, in this case physical activity.
Keywords: Inflammatory markers, personality traits, personality facets, physical activity, Health Behavior Model
Introduction
Chronic inflammation can contribute to poor health outcomes in later life. It can dampen immune function, exacerbate symptoms of chronic conditions, and accelerate the aging process.1,2 There is evidence for possible psychosocial (e.g. personality)3–5 and behavioral (e.g. physical activity)6–9 factors that are associated with markers of inflammation. Identifying these factors is important toward improved understanding of who is at risk for inflammation and the development of interventions to help improve health outcomes. The current study examined both psychosocial and behavioral pathways to inflammation. Moreover, we connected these pathways via mediation analysis in order to examine the mechanisms by which psychosocial characteristics are associated with inflammatory markers.
Basic construct definitions
Biomarkers of inflammation
Serum interleukin-6 (IL-6) is a pro-inflammatory cytokine and a marker of inflammation.10 When infection occurs in the body, cells of the immune system release IL-6 to promote inflammation and notify the body that an inflammatory response is taking place.11 C-reactive protein (CRP) is released from the liver in the presence of IL-6 and goes to the site of inflammation and helps destroy pathogens and return the body to homeostasis.12 Fibrinogen is a glycoprotein that acts as an acute phase reactant in the bloodstream, responding to physiological stress and disease.13 Fibrinogen, IL-6, and CRP are part of a critical response to battling pathogen invasion.10 Individuals who frequently experience these responses over time often develop chronic inflammation, which is associated with a myriad of negative health outcomes such as cardiovascular disease and cancer.14,15
Personality
Personality is a broad construct that refers to individual differences in general patterns of thinking, feeling, and behaving.16 These individual differences are what make a person unique and have been linked to both behavior and health outcomes across the life span.17–20 Many researchers use trait taxonomies to define personality (e.g. the Big Five: neuroticism, extraversion, openness to experience, conscientiousness, and agreeableness).21,22 Facet-level measures of personality represent more narrow-bandwidth characteristics (e.g. motivation, anxiety, need for control) and are often considered to be underlying characteristics defining the traits. In addition, these more narrow facets can be independently linked to consequential outcomes.18,23,24 The combined analysis of broad-trait and narrow-facet levels of personality is essential in deepening our understanding of patterns of associations between personality traits and various outcomes.18,25 Thus, the current study used both trait and facet measures of personality to examine the links to inflammatory markers.
Personality and inflammation
Inflammatory markers have emerged as key factors in understanding health and can be partially understood through associations with personality.10,12–14 Traits such as higher neuroticism, lower conscientiousness, lower extraversion, and lower openness are related to elevated fibrinogen, IL-6, and CRP.3–5,26,27 Furthermore, specific facets of personality such as depressive symptoms, hostility, impulsivity, and excitement seeking are also related to serum IL-6 and serum CRP, white blood cell count, and lymphocyte count.28–30 Others have supported these findings, suggesting that higher conscientiousness and higher levels of self-directedness were associated with lower IL-631 and lower CRP.32 This is further evidence for the importance of examining narrower, facet-level personality on these biomarkers, as it can be the case that associations are not detected at the trait level but only emerge when examining these lower order characteristics. Thus, this gives us more precise findings regarding how personality may be linked to inflammation.
Physical activity and inflammation
There is a substantial body of literature examining links between physical activity and inflammation.6–8,33,34 One meta-analysis examined studies that linked levels of activity and exercise training to inflammatory markers.7 Results showed that regular training over time produced a long-term anti-inflammatory effect. This decrease in the inflammatory response as a result of physical activity may be a key to explaining links between physical activity and reduced cardiovascular disease risk.
Personality and physical activity
We used the Health Behavior Model (HBM)17,35–37 as our theoretical framework for the current study. This theory posits that certain characteristics are associated with either beneficial or detrimental behaviors that are directly related to health. There is a growing body of literature on various aspects of health in multiple samples supporting this theory,38 and a number of studies have found associations between personality and behaviors such as substance abuse and physical activity.19,37,39–43 These factors may be a pathway through which personality influences health. That is, personality traits have a direct impact on health, but personality traits are also related to other factors (such as health behaviors), which in turn are the stronger influence on health. Ultimately, a more cohesive narrative explaining the personality–health relationship can be reached through the inclusion of these health behaviors.
Physical activity is an important health behavior linked to personality and health, as shown by a growing body of literature connecting it to personality.44 Two recent meta-analyses reviewed the existing literature on personality and physical activity. Rhodes and Smith45 found that higher extraversion and conscientiousness were consistently associated with higher levels of physical activity, while higher neuroticism was associated with lower levels. Others46 have found that extraversion, openness, and conscientiousness were consistently associated with more physical activity (both objective and self-report), and neuroticism was associated with less physical activity. These findings paint a clear picture of personality traits and physical activity. However, relatively few studies have examined personality facets47 to gain a fine-grained glimpse into what drives these associations. There is some evidence48 that personality facets predict exercise behavior. Activity (a facet of extraversion) and self-discipline (a facet of conscientiousness) were direct predictors of exercise behavior, while anxiety (a facet of neuroticism) moderated the association between exercise intention and exercise behavior. Low anxiety, paired with high levels of exercise intention, was associated with the greatest likelihood of engaging in exercise behavior.
The current study sought to bring these areas of inquiry together, using the theoretical framework of the HBM, and the associations between personality (traits and facets) and inflammatory biomarkers, via physical activity. Specifically, it is expected that personality would be associated with physical activity and that physical activity would be associated with IL-6, CRP, and fibrinogen. Three indicators of inflammation were chosen as key to outcomes of health, as they were the key inflammatory markers measured by the Midlife Development in the United States (MIDUS) study team.
Methods
Sample
Data for this study were taken from the MIDUS study,49 a national sample of 7108 participants recruited by random-digit-dialing completed data collection (mail questionnaires and phone interviews) in 1994–1995. A second wave of data collection (MIDUS II) occurred in 2004–2005 and consisted of a total sample of 4963 participants from the original sample (a full analysis of sample attrition can be found in Radler and Ryff50). In addition to the time 2 follow-up, a subset of respondents was recruited for participation in the biomarker study (2004–2009). These participants (N = 1255) were required to travel to one of three General Clinical Research Centers to provide blood, urine, and saliva specimens for an intensive study of hypothalamic–pituitary–adrenal (HPA) axis, autonomic, immune, cardiovascular, musculoskeletal, and metabolic function. Trained medical staff collected these data in addition to vital signs, a physical exam, and a medical history. An attrition analysis of the key variables in the current study indicated that individuals who dropped out before completing the biomarkers project were higher in neuroticism (t(1811.8) = 2.48, p = .013) and lower in openness (t(1878.7) = –4.08, p ≤ .001), as well as less healthy (t(1794.1) = 6.39, p < .001), less educated (t(1654.4) = –7.96, p < .001), and more likely to be Caucasian (χ2(1) = 16.31, p < .001.
Measures
Personality traits
Traits were assessed at Time 2 using the Midlife Development Inventory (MIDI) personality scales.22,51 Participants rated the extent to which 26 adjectives described them on a 1–4 scale (1 = not at all, 4 = a lot). These adjectives were used to measure the Big Five: Neuroticism (moody, worrying, nervous, calm (reverse), α = .74); Extraversion (outgoing, friendly, lively, active, talkative, α = .76); Openness to Experience (creative, imaginative, intelligent, curious, broad-minded, sophisticated, adventurous, α = .77); Conscientiousness (organized, responsible, hardworking, thorough, careless (reverse) α = .68); and Agreeableness (helpful, warm, caring, softhearted, sympathetic, α = .80).
Personality facets
Facets were assessed at Time 2 using the Multi-Dimensional Personality Questionnaire (MPQ),52,53 based on the Tellegen three-factor model (positive emotionality, negative emotionality, behavioral constraint) assessing 10 sub-facets of personality (well-being (α = .73), social potency (α = .71), achievement (α = .67), social closeness (α = .69), stress reactivity (α = .74), aggression (α = .66), alienation (α = .61), behavioral control (α = .61), traditionalism (α = .59), and harm avoidance (α = .57). Participants rated the extent to which certain statements described them (1 = true, 2 = somewhat true, 3 = somewhat false, 4 = false) (e.g. “I usually find ways to liven up my day” and “when I get angry, I am often ready to hit someone”). In constructing the measurement for harm avoidance, two statements were used in addition to a set of two scenarios where participants were asked to choose the scenario they would dislike more (“riding a long stretch of rapids in a canoe,” or “waiting for someone who’s late,”). This was done to measure this facet as a self-report behavioral measure of harm avoidance, rather than an indicator of characteristic anxiety.
Physical activity
Physical activity was assessed at time 2 via 12 items that asked about the frequency of moderate and vigorous physical activity that the respondent engaged in (0 = never to 5 = several times a week). Frequency of moderate/vigorous activity was asked about separately by domain (leisure, work, or home) and by season (winter or summer). Items were combined per Cotter and Lachman’s19 scoring procedure (α = .92). Seasonal scores (winter vs summer) were first averaged within each domain for moderate and vigorous activity, then the domain with the highest score (leisure, work, or home) was used as the moderate or vigorous activity score. Finally, moderate and vigorous activity scores were averaged together, resulting in the final total physical activity score.
Inflammatory markers
While other studies have typically used a single biomarker (most commonly IL-6), we used multiple indicators of inflammation that were available in the MIDUS biomarker subproject. IL-6, CRP, and fibrinogen each represent a distinct part of the immune process. For predictive validity of personality traits, we tested multiple outcomes to determine whether parallel effects would be found. Inflammatory markers were assessed between 2005 and 2009 as part of the MIDUS Biomarker Subproject (project 4), whose primary aim was to identify biological pathways associated with health outcomes. Investigators randomly selected individuals from the MIDUS II sample to participate. Consenting participants then traveled to one of three data collection sites (University of California, Los Angeles (UCLA); University of Wisconsin; and Georgetown University). The testing protocol included blood samples, morphology, functional capacities, bone densitometry, medication use, and a physical exam, all conducted by clinicians or trained staff. For full details on the project 4 data collection, see Ryff et al.54 As biomarkers also tend to be affected by a series of medications, all models controlled for the use of blood thinners, statins, steroids, chronic condition comorbidity, and time between the measurement of personality and the biomarker measurement.5
Data analysis
Preliminary analyses were conducted using linear regression models to estimate the effects of personality and physical activity on inflammatory markers. We tested personality traits and facets separately, and tested each of the three inflammatory markers separately as well (IL-6, CRP, and fibrinogen). Due to positively skewed distributions, IL-6 and CRP were natural log-transformed for analysis. The distribution for fibrinogen was normal and is in gram per deciliter units. We kept the models for the MPQ and Big Five scales separate, as personality dimensions tend to be correlated and could over-saturate the models if combined.55 All models included physical activity and also controlled for age, gender, education, race, self-rated health, depression, body composition, medications, comorbidities, and time (from personality measurement to biomarkers assessment).
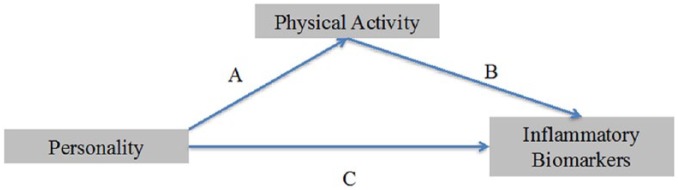
Linear regression models also tested the associations between personality and physical activity, in order to decipher the factors that were candidates for mediation. The personality–biomarker models and personality–physical activity models were then combined into a series of mediation models, using the R package “mediation.”56,57 These models test the effect of personality on inflammatory markers through physical activity.58,59 We used the default simulation type, which was a quasi-Bayesian Monte Carlo method based on normal approximation.56,57 Traditionally, mediation is established when the effect of an independent variable on a dependent variable is reduced (partial mediation) or eliminated (full mediation) by a mediating variable.58 However, current methodological models of mediation55 hold that mediation can be present when there is no direct pathway between predictor and outcome. This suggests that the predictor is indeed related to the outcome but only through a mediator. See Figure 1 for a theoretical model. Table 4 contains the results of the final mediation models and includes the indirect effect (mediation), direct effect (the part of the effect not mediated), and total effects (the sum of the indirect and direct effects). The similarity among the three outcomes is acknowledged, and while these were not any formal adjustments for multiple comparisons, alpha criteria were set to .01, and interpretation reflects interpreted only those effects that are significant at p < .01. Some discussion is mentioned for those trends that were significant at alpha values between .01 and .05; however, we emphasize the need for replication of all effects reported in this study. The full analytic script for this study can be found at https://osf.io/h6jnm/.
Figure 1.
Theoretical mediation model.
Table 4.
Mediating effects of personality traits/facets on inflammatory markers through physical activity.
| IL-6 |
CRP |
|||||
|---|---|---|---|---|---|---|
| Estimate | 95% CI | p | Estimate | 95% CI | p | |
| Extraversion | ||||||
| Mediation effect | −.01 | −0.03 to 0.00 | .016 | −.02 | −0.04 to 0.00 | .024 |
| Direct effect | .02 | −0.04 to 0.08 | .570 | .05 | −0.04 to 0.14 | .280 |
| Total effect | .002 | −0.05 to 0.06 | .950 | .04 | −0.06 to 0.12 | .434 |
| Achievement | ||||||
| Mediation effect | −.01 | −0.03 to 0.00 | .010 | −.02 | −0.04 to 0.00 | .010 |
| Direct effect | −.03 | −0.08 to 0.03 | .360 | −.09 | −0.18 to 0.00 | .056 |
| Total effect | −.04 | −0.10 to 0.02 | .160 | −.10 | −0.19 to −0.01 | .030 |
| Harm avoidance | ||||||
| Mediation effect | .01 | 0.001 to 0.02 | .028 | .01 | 0.0002 to 0.03 | .048 |
| Direct effect | .05 | −0.003 to 0.09 | .070 | .06 | −0.01 to 0.14 | .092 |
| Total effect | .06 | 0.01 to 0.10 | .018 | .08 | 0.001 to 0.15 | .050 |
IL-6: interleukin-6; CRP: C-reactive protein; CI: confidence interval.
Results
Direct effects
Personality facets and inflammatory markers
The models showed that very few facet-level predictors were directly associated with inflammatory markers after adjusting for covariates. However one facet, achievement, was associated with lower fibrinogen (p = .004). This effect was robust and held up when controlling for the other personality facets as well as physical activity. In addition, a few facets were weakly related with p values between .01 and .05. Specifically, higher reactivity was related to lower IL-6 (p = .031), and higher social potency (p = .019) and control (p = .035) were related to higher fibrinogen. See Table 1 for a complete summary of the facet models.
Table 1.
Effects of personality facets on biomarkers.
| Interleukin-6 |
C-reactive protein |
Fibrinogen |
||||
|---|---|---|---|---|---|---|
| B (95% CI) | p | B (95% CI) | p | B (95% CI) | p | |
| Intercept | 0.49 (0.28 to 0.69) | <.001 | 0.47 (0.14 to 0.80) | .005 | 0.35 (0.33 to 0.38) | <.001 |
| Age | 0.10 (0.04 to 0.16) | <.001 | −0.06 (−0.15 to 0.04) | .244 | 0.01 (0.01 to 0.02) | <.001 |
| Education | −0.01 (−0.05 to 0.04) | .837 | −0.06 (−0.14 to 0.02) | .114 | −0.01 (−0.01 to −0.00) | .011 |
| Sex | 0.02 (−0.08 to 0.11) | .707 | −0.19 (−0.35 to −0.04) | .016 | −0.02 (−0.04 to −0.01) | <.001 |
| Self-rated health | 0.09 (0.03 to 0.14) | .002 | 0.15 (0.06 to 0.23) | .001 | 0.01 (−0.00 to 0.01) | .098 |
| Race | 0.06 (−0.13 to 0.25) | .511 | 0.12 (−0.19 to 0.43) | .450 | −0.03 (−0.05 to −0.01) | .014 |
| Blood | 0.08 (0.03 to 0.13) | .003 | 0.05 (−0.03 to 0.14) | .232 | −0.00 (−0.01 to 0.00) | .493 |
| Statin | 0.02 (−0.03 to 0.06) | .526 | −0.09 (−0.17 to −0.02) | .018 | 0.00 (−0.00 to 0.01) | .705 |
| Steroid | −0.01 (−0.05 to 0.03) | .650 | 0.07 (−0.00 to 0.14) | .051 | −0.01 (−0.01 to −0.00) | <.001 |
| Time | 0.08 (0.04 to 0.11) | <.001 | −0.03 (−0.08 to 0.03) | .309 | 0.01 (0.01 to 0.01) | <.001 |
| CountCom | 0.04 (−0.02 to 0.10) | .179 | 0.13 (0.03 to 0.23) | .012 | 0.01 (−0.00 to 0.01) | .124 |
| Depression | 0.08 (0.03 to 0.12) | <.001 | 0.09 (0.02 to 0.16) | .009 | 0.00 (−0.00 to 0.01) | .067 |
| Waist–hip ratio | −0.00 (−0.00 to 0.00) | .374 | 0.00 (−0.00 to 0.00) | .783 | 0.00 (−0.00 to 0.00) | .242 |
| Physical activity | −0.09 (−0.14 to −0.05) | <.001 | −0.11 (−0.19 to −0.03) | .005 | −0.00 (−0.01 to 0.00) | .172 |
| Well-being | 0.04 (−0.01 to 0.10) | .141 | 0.06 (−0.03 to 0.16) | .178 | 0.00 (−0.01 to 0.01) | .686 |
| Social potency | −0.02 (−0.07 to 0.04) | .518 | 0.08 (−0.01 to 0.17) | .067 | 0.01 (0.00 to 0.01) | .019 |
| Achievement | −0.03 (−0.08 to 0.03) | .374 | −0.09 (−0.18 to 0.00) | .062 | −0.01 (−0.02 to −0.00) | .004 |
| Social closeness | −0.00 (−0.05 to 0.04) | .853 | 0.02 (−0.06 to 0.09) | .621 | −0.00 (−0.01 to 0.00) | .712 |
| Reactivity | −0.06 (−0.11 to −0.01) | .031 | −0.09 (−0.18 to 0.00) | .060 | −0.01 (−0.01 to 0.00) | .072 |
| Aggression | 0.04 (−0.01 to 0.10) | .112 | 0.04 (−0.05 to 0.13) | .405 | 0.00 (−0.00 to 0.01) | .506 |
| Alienation | 0.03 (−0.02 to 0.08) | .234 | 0.06 (−0.03 to 0.14) | .186 | 0.00 (−0.00 to 0.01) | .195 |
| Control | 0.01 (−0.04 to 0.05) | .759 | 0.04 (−0.03 to 0.11) | .293 | 0.01 (0.00 to 0.01) | .035 |
| Traditional | 0.03 (−0.02 to 0.07) | .223 | −0.03 (−0.10 to 0.04) | .445 | −0.00 (−0.01 to 0.00) | .670 |
| Harm avoidance | 0.05 (−0.00 to 0.09) | .063 | 0.06 (−0.02 to 0.14) | .124 | −0.00 (−0.01 to 0.01) | .937 |
| Observations | 958 | 958 | 958 | |||
| R2/adjusted R2 | .176/.155 | .114/.093 | .123/.101 | |||
CI: confidence interval.
Personality traits and inflammatory markers
The models testing associations between personality traits and inflammatory markers yield few significant results (see Table 2). Specifically, the fully adjusted models showed that lower neuroticism (p = .004) predicted higher serum IL-6. This effect was robust and was independent of other traits as well as physical activity.
Table 2.
Effects of personality traits on biomarkers.
| Interleukin-6 |
C-reactive protein |
Fibrinogen |
||||
|---|---|---|---|---|---|---|
| B (95% CI) | p | B (95% CI) | p | B (95% CI) | p | |
| Intercept | 0.56 (0.36 to 0.76) | <.001 | 0.56 (0.23 to 0.88) | <.001 | 0.36 (0.34 to 0.38) | <.001 |
| Age | 0.11 (0.05 to 0.16) | <.001 | −0.06 (−0.15 to 0.03) | .216 | 0.01 (0.01 to 0.02) | <.001 |
| Education | −0.03 (−0.07 to 0.02) | .280 | −0.05 (−0.13 to 0.02) | .157 | −0.01 (−0.01 to −0.00) | .011 |
| Sex | −0.01 (−0.11 to 0.08) | .785 | −0.17 (−0.33 to −0.02) | .028 | −0.02 (−0.04 to −0.01) | <.001 |
| Self-rated health | 0.09 (0.04 to 0.14) | .001 | 0.15 (0.06 to 0.24) | .001 | 0.01 (−0.00 to 0.01) | .110 |
| Race | −0.00 (−0.19 to 0.18) | .970 | 0.00 (−0.30 to 0.31) | .981 | −0.04 (−0.06 to −0.01) | .002 |
| Blood | 0.09 (0.03 to 0.14) | .002 | 0.06 (−0.03 to 0.14) | .200 | −0.00 (−0.01 to 0.00) | .443 |
| Statin | 0.01 (−0.03 to 0.06) | .555 | −0.09 (−0.17 to −0.01) | .027 | 0.00 (−0.00 to 0.01) | .480 |
| Steroid | −0.01 (−0.06 to 0.03) | .577 | 0.07 (0.00 to 0.15) | .039 | −0.01 (−0.01 to −0.00) | <.001 |
| Time | 0.08 (0.04 to 0.11) | <.001 | −0.03 (−0.08 to 0.03) | .351 | 0.01 (0.01 to 0.01) | <.001 |
| CountCom | 0.04 (−0.02 to 0.10) | .227 | 0.13 (0.03 to 0.23) | .011 | 0.01 (−0.00 to 0.01) | .130 |
| Depression | 0.08 (0.04 to 0.12) | <.001 | 0.09 (0.02 to 0.16) | .009 | 0.01 (0.00 to 0.01) | .036 |
| Waist–hip ratio | −0.00 (−0.00 to 0.00) | .220 | 0.00 (−0.00 to 0.00) | .996 | 0.00 (−0.00 to 0.00) | .295 |
| Physical activity | −0.09 (−0.14 to −0.04) | <.001 | −0.11 (−0.19 to –.03) | .006 | −0.00 (−0.01 to 0.00) | .136 |
| Neuroticism | −0.07 (−0.12 to −0.02) | .004 | −0.06 (−0.14 to 0.01) | .104 | −0.01 (−0.01 to −0.00) | .044 |
| Extraversion | 0.02 (−0.04 to 0.07) | .586 | 0.05 (−0.04 to 0.14) | .247 | 0.00 (−0.01 to 0.01) | .708 |
| Openness | −0.03 (−0.08 to 0.02) | .278 | −0.05 (−0.14 to 0.04) | .293 | −0.00 (−0.01 to 0.00) | .378 |
| Conscientiousness | −0.04 (−0.09 to 0.01) | .084 | −0.05 (−0.13 to 0.03) | .236 | −0.00 (−0.01 to 0.00) | .561 |
| Agreeableness | 0.00 (−0.05 to 0.06) | .873 | 0.07 (−0.02 to 0.15) | .110 | −0.00 (−0.01 to 0.00) | .379 |
| Observations | 960 | 960 | 960 | |||
| R2/adjusted R2 | .173/.157 | .109/.092 | .113/.096 | |||
CI: confidence interval.
Physical activity on inflammatory markers
Physical activity was included in the above reported models estimating the effects of personality traits and facets on inflammatory markers, and showed in both sets of models that higher physical activity predicted lower levels of both IL-6 (p < .001) and CRP (p < .01), reflecting the expected pattern that individuals who reported higher amounts of physical activity had lower levels of inflammatory markers (see Tables 1 and 2).
Personality traits/facets on physical activity
Models showed small effects on physical activity. For facets, higher achievement (p = .011) and lower harm avoidance (p = .041) were associated with greater physical activity. For the broader personality traits, higher extraversion (p = .015) was associated with greater physical activity (see Table 3).
Table 3.
Effects of personality traits and facets on physical activity.
| Physical activity |
Physical activity |
|||
|---|---|---|---|---|
| B (95% CI) | p | B (95% CI) | p | |
| Intercept | 2.78 (2.35 to 3.21) | <.001 | 2.72 (2.29 to 3.14) | <.001 |
| Age | −0.35 (−0.47 to −0.23) | <.001 | −0.35 (−0.46 to −0.23) | <.001 |
| Education | 0.12 (0.02 to 0.22) | .021 | 0.14 (0.04 to 0.24) | .005 |
| Sex | 0.22 (0.02 to 0.43) | .034 | 0.27 (0.07 to 0.48) | .009 |
| Self-rated health | −0.26 (−0.37 to −0.14) | <.001 | −0.28 (−0.40 to −0.16) | <.001 |
| Race | 0.31 (−0.09 to 0.72) | .129 | 0.40 (−0.00 to 0.80) | .052 |
| Blood | 0.07 (−0.05 to 0.18) | .257 | 0.07 (−0.05 to 0.18) | .247 |
| Statin | 0.07 (−0.03 to 0.18) | .154 | 0.07 (−0.03 to 0.17) | .172 |
| Steroid | 0.09 (−0.01 to 0.18) | .073 | 0.08 (−0.02 to 0.17) | .100 |
| Time | −0.01 (−0.08 to 0.06) | .838 | −0.02 (−0.09 to 0.05) | .638 |
| CountCom | −0.10 (−0.23 to 0.03) | .128 | −0.11 (−0.24 to 0.02) | .110 |
| Depression | 0.02 (−0.07 to 0.11) | .639 | 0.01 (−0.08 to 0.10) | .806 |
| Waist–hip ratio | −0.00 (−0.00 to 0.00) | .452 | −0.00 (−0.00 to 0.00) | .665 |
| Well-being | 0.07 (−0.05 to 0.19) | .233 | ||
| Social potency | −0.06 (−0.18 to 0.05) | .271 | ||
| Achievement | 0.15 (0.03 to 0.27) | .011 | ||
| Social closeness | 0.05 (−0.05 to 0.14) | .351 | ||
| Reactivity | −0.02 (−0.14 to 0.09) | .688 | ||
| Aggression | 0.06 (−0.06 to 0.17) | .328 | ||
| Alienation | −0.03 (−0.14 to 0.08) | .623 | ||
| Control | 0.05 (−0.05 to 0.14) | .359 | ||
| Traditional | −0.07 (−0.16 to 0.03) | .169 | ||
| Harm avoidance | −0.11 (−0.21 to −0.00) | .041 | ||
| Neuroticism | 0.07 (−0.03 to 0.17) | .185 | ||
| Extraversion | 0.15 (0.03 to 0.26) | .015 | ||
| Openness | 0.07 (−0.05 to 0.18) | .255 | ||
| Conscientiousness | 0.01 (−0.09 to 0.11) | .816 | ||
| Agreeableness | −0.11 (−0.22 to 0.01) | .062 | ||
| Observations | 958 | 960 | ||
| R2/adjusted R2 | .137/.117 | .125/.110 | ||
CI: confidence interval.
Mediation effects
The mediation models adjusted for the same covariates as the preliminary analyses. These models suggested that the personality–inflammation associations were mediated by physical activity (see Table 4). Specifically, mediation was found for the facet achievement on both IL-6 (p = .01) and CRP (p = .01). The direction of the estimates indicates that the individuals higher on achievement had lower levels of both IL-6 and CRP, and this association is operated at least partially through engagement in more physical activity. In addition, a few mediation models showed weak effects with p values between .01 and .05. Specifically, there was an effect for harm avoidance on both IL-6 (p = .028) and CRP (p = .048), and for extraversion on both IL-6 (p = .016) and CRP (p = .024).
Discussion
The current study found evidence for the relationship between personality and key inflammatory markers. From the trait-level taxonomy of personality, higher neuroticism was associated with lower levels of IL-6; however, there was no evidence for associations between traits and physical activity. At the facet level, we found a few associations between facets and inflammation, but at the more conservative alpha criteria (p < .01), the only effect was for the association between achievement and fibrinogen. Achievement was associated with higher levels of physical activity and also with markers of inflammation, specifically IL-6 and CRP. Mediation models revealed that indeed physical activity mediated the associations between achievement and inflammation (IL-6 and CRP). This suggests that the associations between achievement and inflammation may operate through physical activity59,60 and is consistent with our expectations. Overall, these effects are consistent with our theoretical framework of the HBM, suggesting that the effects that personality have on inflammation are operating through the specific health behavior of physical activity. At the trait level, past work had indicated that extraversion and conscientiousness are associated with health and behavior outcomes.32,48 Achievement, a facet that is closely aligned with those traits, indicated a similar relationship to health outcomes of inflammation through physical activity. These findings suggest that the fine-grained facet-level analyses may be a more robust approach to understanding individual differences in behavior and health and may provide a more comprehensive understanding in the personality–health relationship.
The small effect sizes of the current study are still considered to be of importance, as the nature of personality research shows small coefficients with impactful implications, especially when considered over long periods of time. When predicting objective, medical outcomes, these effects are non-trivial and should not be ignored.61 These effects can be interpreted in standard deviation units, so the estimates are for individuals at 1 standard deviation beyond the mean. When extrapolated out to the individuals who are 2 or even 3 standard deviations above or below the mean of personality, these effects are much greater. In this case, effects were found even after controlling many potential confounders and can still mean something important for how personality psychology is utilized in understanding health-related outcomes in a medical setting.
The current study has shown support for HBM36 as a means of explaining the associations between personality and inflammation. Other potential pathways not accounted for with the HBM exist and require further attention. For example, social support, major life events, and social roles may be more important than health behaviors in contributing to serum levels of inflammatory markers,62 particularly when mediating pathways from some personality traits/facets. These additional pathways between personality and inflammatory markers may be why we only found associations between personality and physical activity for some traits/facets and not all. However, the current research may suggest that physical activity is particularly important for health regulation for those individuals high in achievement. Future studies should explore additional pathways that could explain the associations of other aspects of personality to health outcomes.
Personality gets “outside the skin” via several potential processes, such as reactive process (moderation) or self-regulative process (mediation).63 In this study, we tested the self-regulative process of personality on health, specifically inflammation, via mediation. Additional work with more long-term longitudinal data will give us further insight into the effects on objective long-term health outcomes, such as disease onset and mortality.
Among the limitations to the current study were the relatively low reliabilities (between .6 and .7) of the personality scales used in MIDUS. The results need to be interpreted with caution, and future studies need to extend these findings using different measures. While we did measure personality prior to the measurements of inflammatory markers, another limitation to this study is that we did not have baseline levels of serum inflammatory markers to control for, as they were not available at the time 1 wave of the MIDUS data collection. As such, we do not know whether personality is related to subsequent change in inflammation, and future studies with additional follow-up data of these inflammatory markers are needed. In addition, the temporal structure for testing mediation was not ideal, as physical activity and personality were assessed in the same measurement occasion. That said, further research should clarify whether physical activity acts as a true mediator of the personality–inflammatory marker associations, rather than a confound. Future work will need to continue this line of inquiry and attempt to replicate these findings with optimal data, both using MIDUS as new waves of data collection are added, and with other data sets.
Conclusion
These findings contribute to the broader fields of aging and health by providing evidence that individual difference factors, specifically personality traits and facets, are linked to key markers of inflammation. In addition, the current study describes a complex process underlying direct relationships. Specific behaviors, in this case physical activity, may be an important factor toward understanding the role that individual differences have on health outcomes. As the medical field continues to examine how chronic inflammation contributes to health outcomes in old age, the psychological sciences will do their part in identifying how individual differences may begin to influence those processes earlier in life. If the field continues to find robust evidence that both personality and physical fitness may help reduce inflammation and improve health, this will aid in the development of more tailored interventions in younger individuals who may be at greater risk. This has already begun to be examined for trait conscientious in identifying that an individual who is low in conscientiousness and less likely to engage in healthy behaviors may be more susceptible to inflammation and disease and require some kind of personality informed intervention to mitigate negative outcomes. Personality-based precision medicine can help identify such individuals and tailor preventive care in light of their unique psychological risk factors. The HBM is a theoretical framework that describes why personality characteristics influence health and longevity. Our findings provide empirical support for this model suggesting that higher levels of achievement are associated with lower levels of inflammatory markers via more physical activity and suggest that personality may be contributing to our biological health in very real ways. Physical activity is an important mechanism by which personality gets under the skin and may help future researchers and practitioners understand how’s and why’s of the associations between personality, inflammation, and downstream health.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval was not sought for the present study because this was an analysis of pre-existing data.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This projects was funded by R01-AG018436 (PI: Mroczek): Personality & Well-Being Trajectories in Adulthood; U19-AG051426 (PI: Ryff): Mid-Life in the United States: A National Study of Health and Well-Being.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iD: Eileen K Graham  https://orcid.org/0000-0003-3095-4625
https://orcid.org/0000-0003-3095-4625
References
- 1. Fougere B, Boulanger E, Nourhashemi F, et al. Chronic inflammation: accelerator of biological aging. J Gerontol A Biol Sci Med Sci 2017; 72(9): 1218–1225. [DOI] [PubMed] [Google Scholar]
- 2. Walston JD. The fire of chronic inflammation in older adults: etiologies, consequences, and treatments. Innov Aging 2017; 1(Suppl. 1): 961. [Google Scholar]
- 3. Luchetti M, Barkley JM, Stephan Y, et al. Five-factor model personality traits and inflammatory markers: new data and a meta-analysis. Psychoneuroendocrinology 2014; 50: 181–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sutin AR, Terracciano A, Deiana B, et al. High neuroticism and low conscientiousness are associated with interleukin-6. Psychol Med 2010; 40(9): 1485–1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Turiano NA, Mroczek DK, Moynihan J, et al. Big 5 personality traits and interleukin-6: evidence for “healthy Neuroticism” in a US population sample. Brain Behav Immun 2013; 28: 83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ertek S, Cicero A. Impact of physical activity on inflammation: effects on cardiovascular disease risk and other inflammatory conditions. Arch Med Sci 2012; 8(5): 794–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kasapis C, Thompson PD. The effects of physical activity on serum C-reactive protein and inflammatory markers: a systematic review. J Am Coll Cardiol 2005; 45(10): 1563–1569. [DOI] [PubMed] [Google Scholar]
- 8. Woods JA, Vieira VJ, Keylock KT. Exercise, inflammation, and innate immunity. Immunol Allergy Clin North Am 2009; 29(2): 381–393. [DOI] [PubMed] [Google Scholar]
- 9. Woods JA, Wilund KR, Martin SA, et al. Exercise, inflammation and aging. Aging Dis 2012; 3(1): 130–140. [PMC free article] [PubMed] [Google Scholar]
- 10. Kritchevsky SB, Cesari M, Pahor M. Inflammatory markers and cardiovascular health in older adults. Cardiovasc Res 2005; 66(2): 265–275. [DOI] [PubMed] [Google Scholar]
- 11. Scheller J, Ohnesorge N, Rose-John S. Interleukin-6 trans-signalling in chronic inflammation and cancer. Scand J Immunol 2006; 63: 321–329. [DOI] [PubMed] [Google Scholar]
- 12. Ansar W, Ghosh S. C-reactive protein and the biology of disease. Immunol Res 2013; 56(1): 131–142. [DOI] [PubMed] [Google Scholar]
- 13. Davalos D, Akassoglou K. Fibrinogen as a key regulator of inflammation in disease. Semin Immunopathol 2012; 34(1): 43–62. [DOI] [PubMed] [Google Scholar]
- 14. Collaboration ERF. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med 2012; 367(14): 1310–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Coussens LM, Zitvogel L, Palucka AK. Neutralizing tumor-promoting chronic inflammation: a magic bullet? Science 2013; 339(6117): 286–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Funder DC. The personality puzzle. 3rd ed. New York: W.W. Norton & Company, 2004. [Google Scholar]
- 17. Turiano NA, Chapman BP, Gruenewald TL, et al. Personality and the leading behavioral contributors of mortality. Health Psychol 2015; 34: 51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Graham EK, Lachman ME. Personality traits, facets and cognitive performance: age differences in their relations. Pers Individ Dif 2014; 59: 89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cotter KA, Lachman ME. No strain no gain: psychosocial predictors of physical activity across the adult lifespan. J Phys Act Health 2010; 7(5): 584–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Graham EK, Rutsohn JP, Turiano NA, et al. Personality predicts mortality risk: an integrative data analysis of 15 international longitudinal studies. J Res Pers 2017; 70: 174–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Costa PT, McCrae RR. Normal personality assessment in clinical practice: the NEO Personality Inventory. Psychol Assess 1992; 4(1): 5–13. [Google Scholar]
- 22. Lachman ME, Weaver SL. The Midlife Development Inventory (MIDI) Personality Scale: scale construction and scoring. Waltham, MA: Department of Psychology, Brandeis University, 1997. [Google Scholar]
- 23. Costa PT, Jr, Weiss A, Duberstein PR, et al. Personality facets and all-cause mortality among Medicare patients aged 66 to 102 years: a follow-on study of Weiss and Costa (2005). Psychosom Med 2014; 76(5): 370–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Paunonen SV, Ashton MC. Big five factors and facets and the prediction of behavior. J Pers Soc Psychol 2001; 81(3): 524–539. [PubMed] [Google Scholar]
- 25. Graham EK, Lachman ME. Personality traits, facets, and cognitive performance: Age differences in their relations. Personal Individ Differ 2013; 59 : 89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Armon G, Melamed S, Shirom A, et al. The associations of the Five Factor Model of personality with inflammatory biomarkers: a four-year prospective study. Pers Indiv Differ 2013; 54(6): 750–755. [Google Scholar]
- 27. Mottus R, Luciano M, Starr JM, et al. Personality traits and inflammation in men and women in their early 70s: the Lothian Birth Cohort 1936 study of healthy aging. Psychosom Med 2013; 75(1): 11–19. [DOI] [PubMed] [Google Scholar]
- 28. Brummett BH, Boyle SH, Ortel TL, et al. Associations of depressive symptoms, trait hostility, and gender with C-reactive protein and interleukin-6 response following emotion recall. Psychosom Med 2010; 72(4): 333–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mwendwa DT, Ali MK, Sims RC, et al. Dispositional depression and hostility are associated with inflammatory markers of cardiovascular disease in African Americans. Brain Behav Immun 2013; 28: 72–82. [DOI] [PubMed] [Google Scholar]
- 30. Sutin AR, Milaneschi Y, Cannas A, et al. Impulsivity-related traits are associated with higher white blood cell counts. J Behav Med 2012; 35(6): 616–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chapman BP, van Wijngaarden E, Seplaki CL, et al. Openness and conscientiousness predict 34-week patterns of Interleukin-6 in older persons. Brain Behav Immun 2011; 25(4): 667–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Henningsson S, Baghaei F, Rosmond R, et al. Association between serum levels of C-reactive protein and personality traits in women. Behav Brain Funct 2008; 4: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gleeson M, Bishop NC, Stensel DJ, et al. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol 2011; 11(9): 607–615. [DOI] [PubMed] [Google Scholar]
- 34. Andersson J, Jansson JH, Hellsten G, et al. Effects of heavy endurance physical exercise on inflammatory markers in non-athletes. Atherosclerosis 2010; 209(2): 601–605. [DOI] [PubMed] [Google Scholar]
- 35. Mroczek DK, Spiro A, Turiano N. Do health behaviors explain the effect of neuroticism on mortality? Longitudinal findings from the VA Normative Aging Study. J Res Pers 2009; 43(4): 653–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Smith TW. Personality as risk and resilience in physical health. Curr Dir Psychol Sci 2006; 15(5): 227–233. [Google Scholar]
- 37. Friedman HS. Long-term relations of personality and health: dynamisms, mechanisms, tropisms. J Pers 2000; 68(6): 1089–1107. [DOI] [PubMed] [Google Scholar]
- 38. Bogg T, Roberts BW. Conscientiousness and health-related behaviors: a meta-analysis of the leading behavioral contributors to mortality. Psychol Bull 2004; 130(6): 887–919. [DOI] [PubMed] [Google Scholar]
- 39. Raynor DA, Levine H. Associations between the five-factor model of personality and health behaviors among college students. J Am Coll Health 2009; 58(1): 73–81. [DOI] [PubMed] [Google Scholar]
- 40. Hampson SE, Goldberg LR, Vogt TM, et al. Mechanisms by which childhood personality traits influence adult health status: educational attainment and healthy behaviors. Health Psychol 2007; 26(1): 121–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Munafo MR, Zetteler JI, Clark TG. Personality and smoking status: a meta-analysis. Nicotine Tob Res 2007; 9(3): 405–413. [DOI] [PubMed] [Google Scholar]
- 42. Terracciano A, Lockenhoff CE, Crum RM, et al. Five-factor model personality profiles of drug users. BMC Psychiatry 2008; 8: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kotov R, Gamez W, Schmidt F, et al. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull 2010; 136(5): 768–821. [DOI] [PubMed] [Google Scholar]
- 44. Allen MS, Laborde S. The role of personality in sport and physical activity. Curr Dir Psychol Sci 2014; 23(6): 460–465. [Google Scholar]
- 45. Rhodes RE, Smith NE. Personality correlates of physical activity: a review and meta-analysis. Br J Sports Med 2006; 40(12): 958–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wilson KE, Dishman RK. Personality and physical activity: a systematic review and meta-analysis. Pers Indiv Differ 2015; 72: 230–242. [Google Scholar]
- 47. McCrae RR. A more nuanced view of reliability: specificity in the trait hierarchy. Pers Soc Psychol Rev 2015; 19(2): 97–112. [DOI] [PubMed] [Google Scholar]
- 48. Hoyt AL, Rhodes RE, Hausenblas HA, et al. Integrating five-factor model facet-level traits with the theory of planned behavior and exercise. Psychol Sport Exerc 2009; 10(5): 565–572. [Google Scholar]
- 49. Brim OG, Ryff CD, Kessler RC. How healthy are we? A national study of well-being at midlife. Chicago, IL: University of Chicago Press, 2004. [Google Scholar]
- 50. Radler BT, Ryff CD. Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. J Aging Health 2010; 22(3): 307–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Goldberg LR. The development of markers for the Big-Five factor structure. Psychol Assess 1992; 4: 26–42. [Google Scholar]
- 52. Tellegen A. Structure of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report. In: Tuma AH, Maser JD. (eds) Anxiety and the anxiety disorders. Hillsdale, NJ: Lawrence Erlbaum, 1985, pp. 681–706. [Google Scholar]
- 53. Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychol Assess 2002; 14(2): 150–163. [DOI] [PubMed] [Google Scholar]
- 54. Ryff CD, Seeman T, Weinstein M. National survey of Midlife Development in the United States (MIDUS 2): biomarker project, 2004–2009. Ann Arbor, MI: Inter-university Consortium for Political and Social Research, 2013. [Google Scholar]
- 55. John OP, Naumann LP, Soto CJ. Paradigm shift to the integrative big-five trait taxonomy: history, measurement, and conceptual issues. In: John OP, Robins RW, Pervin LA. (eds) Handbook of personality: theory and research. New York: Guilford Press, 2008, pp. 114–158. [Google Scholar]
- 56. Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods 2010; 15(4): 309–334. [DOI] [PubMed] [Google Scholar]
- 57. Tingley D, Yamamoto T, Hirose K, et al. mediation: R package for causal mediation analysis. J Stat Softw 2014; 59(5): 38. [Google Scholar]
- 58. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986; 51(6): 1173–1182. [DOI] [PubMed] [Google Scholar]
- 59. MacKinnon DP, Fairchild AJ. Current directions in mediation analysis. Curr Dir Psychol Sci 2009; 18: 16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. MacKinnon DP. Introduction to statistical mediation analysis. Abingdon, UK: Routledge, 2008. [Google Scholar]
- 61. Roberts BW, Kuncel NR, Shiner R, et al. The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspect Psychol Sci 2007; 2(4): 313–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Loucks EB, Sullivan LM, D’Agostino RB, Sr, et al. Social networks and inflammatory markers in the Framingham Heart Study. J Biosoc Sci 2006; 38(6): 835–842. [DOI] [PubMed] [Google Scholar]
- 63. Hampson SE. Personality processes: mechanisms by which personality traits “get outside the skin.” Annu Rev Psychol 2012; 63: 315–339. [DOI] [PMC free article] [PubMed] [Google Scholar]