Abstract
Purpose
Sleep disturbance is common in intensive care units. It is associated with detrimental psychological impacts and has potential to worsen outcome. Irregular exposure to sound and light may disrupt circadian rhythm and cause frequent arousals from sleep. We sought to review the efficacy of environmental interventions to reduce sound and light exposure with the aim of improving patient sleep on adult intensive care units.
Methods
We searched both PubMed (1966–30 May 2017) and Embase (1974–30 May 2017) for all relevant human (adult) studies and meta-analyses published in English using search terms ((intensive care OR critical care), AND (sleep OR sleep disorders), AND (light OR noise OR sound)). Bibliographies were explored. Articles were included if reporting change in patient sleep in response to an intervention to reduce disruptive intensive care unit sound /light exposure.
Results
Fifteen studies were identified. Nine assessed mechanical interventions, four of which used polysomnography to assess sleep. Five studies looked at environmental measures to facilitate sleep and a further two (one already included as assessing a mechanical intervention) studied the use of sound to promote sleep. Most studies found a positive impact of the intervention on sleep. However, few studies used objective sleep assessments, sample sizes were small, methodologies sometimes imperfect and analysis limited. Data are substantially derived from specialist (neurosurgical, post-operative, cardiothoracic and cardiological) centres. Patients were often at the ‘less sick’ end of the spectrum in a variety of settings (open ward beds or side rooms).
Conclusions
Simple measures to reduce intensive care unit patient sound/light exposure appear effective. However, larger and more inclusive high-quality studies are required in order to identify the measures most effective in different patient groups and any impacts on outcome.
Keywords: Sleep, intensive care, noise, light, sound
Introduction
Sleep disturbance is commonly experienced by intensive care unit (ICU) patients,1–3 affecting perhaps half of patients.4 Sleep quantity may be reduced but sleep quality (architecture) is worst affected: time spent in continuous sleep is reduced, and the circadian sleep pattern (when in a 24-h period one sleeps) and normal sleep ‘cycle’ (through its stages from ‘light’ to ‘deep’) disrupted. Subjectively, ICU patients report reduced, poor quality, irregular and fragmented sleep5 as one of their greatest emotional stressors,6 second only to pain.7 Sleep deprivation impacts negatively on objective neuropsychological function.8
Poor sleep quality and quantity may additionally cause physical harm, including increases in pro-inflammatory cytokines, labile (or elevated) blood pressure, altered salt handling, increased myocardial infarction risk, altered appetite, impaired immune function, exacerbated hormonal stress response and impaired glucose tolerance.8,9 Such effects may increase ICU morbidity and prolong admission.2,10,11
Sleep disturbance on ICU may thus be both distressing and harmful. But how can it be ameliorated? Some causal factors are not readily mitigated: the primary illness or treatments (mechanical ventilation or medications such as beta-agonists or steroids). However, environmental factors (nocturnal medical/nursing interventions and intrusive sound/light exposure) are major contributors and can be modified.1,11–13
Generation of a normal circadian sleep-wake pattern depends upon exposure to diurnal patterns of environmental sound and light,14 loss of which may thus worsen sleep patterns. Conversely, sound exposure on ICU can directly interrupt sleep: levels routinely exceed World Health Organization recommendations (35 dB at night, 45 dB by day),15 night peaks >85 dBA may occur up to and including 16 times/h,16 and levels of 90 dB are not unusual17 – the equivalent of a motorcycle at 25 ft (90 dB) or a freight train at 15 m (85 dB). Bright light may also disturb sleep, as can exposure to evening/night blue-spectrum light from monitors.18 Nocturnal care interactions can average 42.6 per night.12
We critiqued all published studies that investigated the use of conservative techniques to improve sound and light exposure and patient disruptions in the ICU and their impact on sleep and report our findings as a narrative review.
Methods
The PRISMA statement guided review and reporting.19 We searched PubMed (1966-) and Embase (1974-) to 30 May 2017 for relevant English-language (adult) human studies and meta-analyses, using search terms ((intensive care OR critical care), AND (sleep OR sleep disorders), AND (light OR noise OR sound)). Articles were included in the review if they were (i) original published experimental studies of adult ICU patients or healthy subjects in simulated ICU environments (ii) reporting either subjective or objective sleep measures following (iii) a conservative intervention that aimed to reduce sound and light exposure or patient disruptions (Figure 1). Abstracts, single case reports and review articles were excluded. Publications were not excluded based on some metric of ‘quality’ – the strengths and weaknesses of each study being described in narrative form in this review. Identified article titles/abstracts were assessed, and full text obtained for all appearing relevant/ambiguous. All bibliographies were hand-searched.
Figure 1.
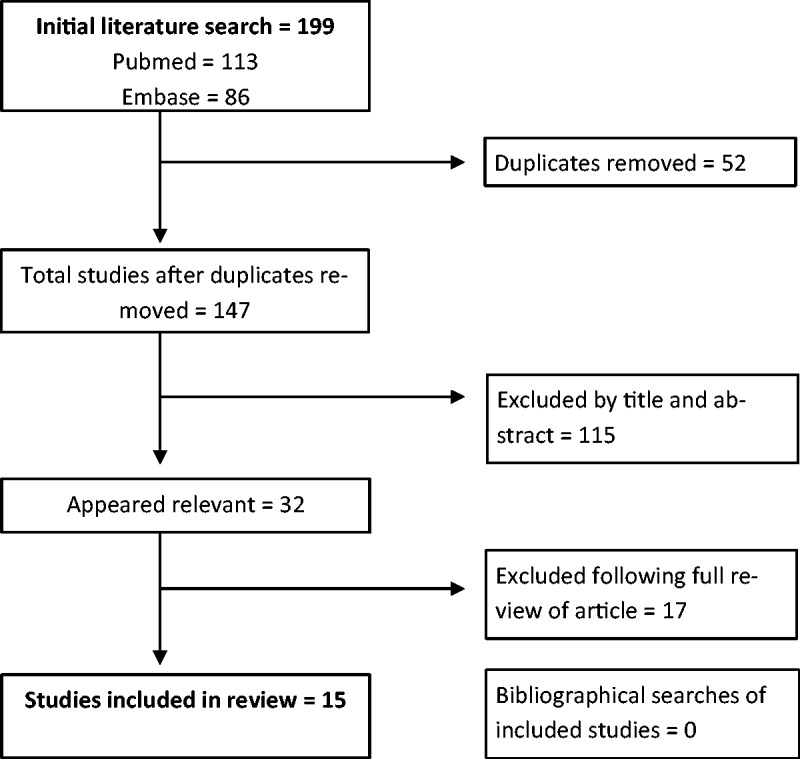
Selection process for review with the total number of studies identified by the literature search and the number excluded at each stage of the review process.
Analysis related to (i) use of mechanical interventions to limit sound levels and/or light exposure, (ii) environmental interventions to limit sound levels and/or light exposure or (iii) use of ‘pleasant sounds’ (e.g. music) to improve sleep.
Findings
The search terms yielded 199 studies: 52 were duplicates and 115 excluded following title/abstract review, leaving 15 included within the review (Table 1).
Table 1.
Summary of the studies included within the review that investigated a conservative technique to improve the sleep of patients in ICU.
| Publication | No. of subjects | Sex | Mean age (years) | Setting | Population | Intubated | Room type | Sleep measures | Environmental intervention | Objective environmental measurements | Intervention duration | Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dennis et al.20 | 50 (35 day + 15 night) | 19 M 16 F + 6 M 9 F | 55.5 + 52.9 | Neuro ICU | Neurological | None | Around core station | Nursing assessments (Sleep Observation Tool) | Quiet Time protocol twice daily 01:30–03:30 and 14:00–16:00 | Noise reduced by 9.0 dB (day) and 1.4 (night) Light reduced 142.6 lux (day) and 9.8 (night) | 6 months | Significantly more likely to sleep during the quiet time periods in afternoon, but not night |
| Foreman et al.21 | 6 vs 6 controls | 5 M 1 F vs. 4 M 2 F | 59 vs. 56 | Neuro ICU | Neurological | 7/12 | – | Polysomnography | Eyemasks, noise-cancelling headphones, and melatonin | Not recorded | <7 nights | Difficulty assessing sleep from PSG due to large number of records unscorable No difference in groups between night 1 and 3 |
| Hu et al.22 | 14 | 6 M 8 F | 31.1 | Simulated ICU | Healthy | None | – | Polysomnography Sleep diary Sleep visual analogue scale | Eyemasks and earplugs | N/A | 1 night | Increased REM sleep and reduced REM latency and arousals Improved subjective sleep quality |
| Hu et al.23 | 20 vs. 25 controls | 11 M 9 F vs. 16 M 9 F | 56.6 vs. 56.8 | Cardiac surgery ICU | Post cardiac surgery | Average duration for population 22–23 h | – | Richards-Campbell sleep questionnaire | Eyemasks, earplugs, and relaxing music at night and in the morning (30 min) vs. routine care | No difference in light/sound levels between groups (monitored 20:00 to 08:00) | 2 nights on ICU | Improved sleep scores on all sleep scales |
| Huang et al.24 | Four groups of 10 | 50% M vs. 40% M vs. 50% M vs. 60% M | 40.1 vs. 42.0 vs. 39.7 vs. 52.8 | Simulated ICU | Healthy | None | Private rooms | Polysomnography Sleep visual analogue scale | Eyemasks and earplugs vs. melatonin vs. placebo vs. control | N/A | 4 nights | Intervention reduced sleep latency, arousals, and awakenings |
| Jones and Dawson25 | 50 vs. 50 controls | 30 M, 20 F vs. 27 M, 23 F | 56.3 vs. 58.1 | ICU | Medical and surgical | None | Varied | Likert scales for sleep quantity and quality Factors facilitating and preventing sleep | Eyemasks and earplugs vs. routine care | Not recorded | ICU admission | Increased sleep duration but not sleep quality (no statistical analysis) |
| Kamdar et al.26 | 178 vs. 122 control | 7% M 93% F vs. 46% M 54% F | 54 vs. 54 | Medical ICU | Medical | 47% vs. 64% (during stay) | Private | Richards-Campbell sleep questionnaire (<45% completed by nurses) Sleep in the ICU questionnaire (abbreviated) | Sleep promoting intervention (multiple approaches in three additive stages with staff training and daily checklists) vs. routine care | Not recorded | ≥1 night | No significant difference in sleep quality ratings Reduced incidence of delirium |
| Li et al.27 | 28 vs. 27 controls | 57% M 43% F vs. 78% M 22% F | 49.3 vs. 50.7 | Surgical ICU | Post-surgery | None | – | Richards-Campbell sleep questionnaire Sleep in the ICU questionnaire | Sleep care guidelines (changing nursing regimes and reducing noise/light at night with staff education course) vs. routine care | Peak and average noise significantly reduced Mean peak noise 51.3 vs. 59.2 dB (bed) Mean noise 50.1 vs. 57.7 dB (bed) | 3 months | Increased sleep quality and efficiency |
| Olson et al.28 | 121 vs. 118 controls | 53% M 47% F vs. 52% M 48% F | 51 vs. 48 | Neuro ICU | Neurology and neurosurgery | – | – | Nurse assessments | Quiet time protocol twice daily 02:00–04:00 and 14:00–16:00 | Significant reduction in noise/light during day/night | 2 months | 1.6 times more likely to be observed sleeping Significantly more likely to be asleep during afternoon period only |
| Patel et al.29 | Subgroup: 29 vs. 30 controls | 55% M 45% F vs. 47% M 53% F | 60.5 vs. 61.9 | ICU | Medical and surgical | – | – | Richards-Campbell sleep questionnaire Sleep in the ICU questionnaire | Care bundle (reducing sleep disturbance, noise, and light with staff training and champions, patients offered eyemasks/earplugs) vs. routine care | Nocturnal measures: Mean noise 61.8 vs. 68.8 dB Mean light 301 vs. 594 lux Interactions 23.4 vs. 33.6 Awoken by interactions 9.0 vs. 11.0 | 1 month | Increased sleep quality, efficiency, and reduced sleep during the day. Significantly more time asleep at night (8.6 h vs. 6.6) Lower incidence of delirium |
| Richardson et al.30 | 34 vs. 28 controls | 69% M 31% F | 18+ | Cardiothoracic ICU | Cardiothoracic | None | Cubicle and open bay | Likert scales for sleep quantity and quality Factors facilitating and preventing sleep | Eyemasks and earplugs vs. routine care | Not recorded | ICU admission | Increased sleep duration quality compared to normal sleep (no statistical analysis) |
| Ryu et al.31 | 29 vs. 29 controls | 19 M 10 F vs. 19 M 10 F | 61.2 | Cardiac ICU | Coronary angiography | None | – | Verran and Snyder-Halpern sleep scale Quantity of sleeping questionnaire | Eyemasks, earplugs, and sleep-inducing music (52 min) vs. eyemasks and earplugs | Not recorded | 1 night | Increased subjective sleep quantity and quality |
| Scotto et al.32 | 49 vs. 39 controls | 55% M 45% F vs. 67% M 33% F | 63.7 vs. 62.5 | Critical care | Medical and few surgical | None | – | Verran and Snyder-Halpern sleep scale | Earplugs vs. routine care | Not recorded | 1 night | Increased scores on sleep scales with exception of satisfaction falling asleep |
| Van Rompaey et al.33 | 69 vs. 67 controls | 68% M 32% F vs. 64% M 36% F | 57 vs. 62 | ICU | Medical and surgical | None | Separated spaces/rooms | Dichotomous sleep questions | Earplugs vs. routine care | Not recorded | <4 nights | Improved sleep scores on night one (earplugs decreased risk of confusion/delirium by 53%) |
| Wallace et al.34 | 6 | 100% M | 25 | Simulated ICU | Healthy | None | – | Polysomnography Subjective sleep duration | Earplugs | N/A | 1 night | Intervention reduced REM sleep latency and increased REM sleep duration |
Study patient demographics, settings, interventions, and outcome measures of the 15 studies included in the review.
ICU: intensive care unit.
Mechanical interventions
Nine articles were identified, most commonly relating to earplug/eyemask use.
Subjective assessment of sleep quantity and quality used questionnaires
The two (Verran/Snyder-Halpern Sleep Scale (VSHSS) and the Richards-Campbell Sleep Questionnaire (RCSQ)) validated against objective sleep measures (actigraphy or polysomnography (PSG))35 were only used in two studies.23,32
The first studied 88 adults on two USA teaching hospital ICUs. Over 70% had cardiac medical conditions. About a fifth were surgical patients. Those with diagnosed sleep disorders or hearing loss, who had received sedation or anaesthesia in the previous 12 h or who required mechanical ventilation were excluded. ‘As needed’ sedative/hypnotic administration was not permitted. Of the 88 subjects, 49 were randomized to earplug use overnight (hours not specified, removed only for brief communication/nursing intervention). There were 39 controls. All completed the VSHSS before noon the next day. Intervention was associated with improvements in every one of seven measures of sleep, with the exception of time to fall asleep.32
The second studied postoperative elective cardiac surgical patients expected to stay >2 nights in a Chinese Cardiac ICU, randomized to sleep with/without earplugs and eyemasks combined with 30-min relaxing music. Of 45 subjects, three would not accept the interventions and two were withdrawn, yielding 20 and 25 subjects in the intervention and control groups, respectively. The RCSQ (visual-analogue scale) was completed 1–2 days following transfer from ICU. Intervention improved depth of sleep, ease of falling asleep, readiness to fall asleep again after awakening, and overall sleep quality (p < 0.05). The score relating to the number of awakenings was substantially reduced (51.2 ± 26.7 vs 25.3 ± 16.2. p < 0.01). Perceived sleep quality was better (score 54 ± 25.5 vs 23.7 ± 20.6, p < 0.01). Of note, patients were young (mean age 58 years), ventilated for an average of only 22 h, and stayed on ICU for a mean of 58.9 and 35 h (controls vs intervention respectively). Hospital stay appeared unusually long- 22.6 and 20.7 days respectively.23
Data from these two studies (which related to different locations and patient types) suggest that mechanical interventions can improve ICU sleep. However, whether this might apply to sicker patients, or to those with more prolonged admissions, is not demonstrated, and caution should be applied in drawing such inferences. Furthermore, although loss of circadian rhythm and sleep may contribute to delirium, most guidelines recommend optimizing sensory input to patients (for example glasses, hearing aids) to help prevent and treat delirium in a non-pharmacological manner. Earplugs may therefore impede beneficial sensory input. It seems likely that the benefit of better sleep quality and quantity would outweigh these negatives.
Three further studies used non-validated sleep questionnaires and did not report objective environmental sound or light levels.25,30,33 One studied general ICU patients with an expected ICU stay of >24 h and GCS >10, who were not receiving sedative agents.21 Sleep was assessed through responses to five questions: ‘Did you sleep (i) well (ii) better than expected (iii) better than at home?’ (iv) ‘Were you awake for a long time before falling asleep?’ and (v) ‘Do you feel sufficiently rested?’ Sum scores were categorized as bad (<2), moderate (2–3), or good (≥4). Compared to 67 controls, the 69 patients using earplugs slept better after the first night (borderline significance, p = 0.042). Good sleep was reported by 45% vs 25% (33% vs 48% for ‘poor sleep’) of earplug vs control patients, respectively. Differences no longer remained significant after the second night, and more patients with earplugs reported poor sleep after the third. Attrition in numbers limits the ability to draw robust conclusions, as does the use of an unvalidated sleep assessment scale (where responses appear likely interdependent). Nonetheless, earplug use was associated with better NEECHAM (Confusion) Scale scores (26 vs. 24, p = 0.04). Two further articles used Likert scales to assess sleep quantity/quality in patients using earplugs and eyemasks in a cardiothoracic30 or general ICU.25 The first was a pilot study of a convenience sample of high-dependency cardiothoracic planned and emergency admissions.30 All had to be lucid, orientated, able to apply/remove eyemasks/earplugs themselves and >24 h following administration of any anaesthetic/sedative. Duration of ICU stay prior to enrolment was highly variable (1 to >14 days), the area in ICU in which patients resided was mixed (open areas and cubicles), and some were extubated whilst others had tracheostomies. Thirty-four received earplugs and eyemasks (vs 28 controls, with two missing datasets). In the two low ranges of h slept (0–2 h and 2–4 h), a greater percentage of patients were in the non-intervention (65%) than intervention group (56%). Similarly, more patients in the intervention group rated their sleep ‘more than average’ than in the non-intervention group (18 vs 7%). However, no statistical analysis was performed, and patients self-selected their allocated group. The second study, of emergency medical/surgical patients and elective surgical HDU patients,25 used a convenience sample of 50 controls, and 50 with an eyemask and earplug intervention. Age range was large (21–90 years), some were in side-rooms and others not. Again, sleep measures (those reported by Richardson et al.30) suggested possible benefit, but no statistical analysis was performed.
Objective assessment of sleep quantity and quality includes the gold standard of PSG (in which the electroencephalogram and physiological variables determine sleep/wake stages).36 Four studies used PSG. One studied twelve neuro-ICU (acute brain injury, cardiac arrest, or sepsis) patients (58% mechanically ventilated),21 of which half were randomized to receive noise-cancelling headphones, eyemasks and oral melatonin for ≤7 days. Of PSG recordings, 65% could not be scored due to abnormal sleep. Whilst there was no difference in sleep quantity or time spent in specific sleep stages, the small dataset limits the ability to draw robust conclusions.
PSG was used in three studies of healthy volunteers in simulated ICU environments with ambient lighting and ICU sound level recording.22,24,34 In the first, which used a repeated measures design, mean rapid-eye-movement (REM) sleep latency was reduced (147.8 vs 106.7 min) and mean REM sleep duration increased (14.9 to 19.9%) in those using earplugs.34 In a study of similar design, but with added recovery nights, 14 subjects using earplugs and eyemasks had the same improvement in REM sleep changes (mean latency 146.9 min in controls vs 105.7, p = 0.013), and fewer sleep arousals (arousals index 15.1 vs 12.2, p = 0.04).22
A more recent study in a simulated ICU environment, 40 subjects were randomized to receive either earplugs and eyemasks, oral melatonin, placebo, or no treatment, for four nights.24 Compared to no treatment, the 10 who slept with earplugs and eyemasks had reduced sleep latency (mean 46.6 ± 21.6 vs 71.4 ± 25.6, p = 0.01) and fewer arousals (5.5 ± 2.1 vs 9.8 ± 3.0, p < 0.001) and awakenings (10.5 ± 3.2 vs 15.1 ± 3.3, p = 0.001) and, when compared to the oral melatonin group, had significantly fewer awakenings (6.5 ± 1.8 vs 10.5 ± 3.2, p = 0.004). However, simulated ICU environments do not include the many patient, treatment, and environmental factors that contribute to poor ICU sleep. Nor can the role of each intervention component be differentiated, whilst any melatonin action cannot be assumed to be the same in ICU patients and the healthy.
In summary, mechanical devices to improve subjective sleep on ICU appear beneficial, but interventions were often mixed, only occasionally reported environmental factors, studied heterogeneous patients at different time-points, and provided limited data relating to objective sleep assessments. Sample sizes were generally small, and methodologies sometimes unvalidated or weak.
Environmental interventions
Five studies assessed environmental techniques (including reducing ICU sound and light exposure, and patient disruptions such as for nursing care or investigations).
Two related to incorporation of a ‘quiet time’ (QT) protocol on neuro-ICUs.20,28 Sleep was assessed by nurses using a validated sleep observation tool37 at 15–30 min intervals. Such assessments correlate well with those determined by PSG, but may overestimate total sleep time, and sleep quality cannot be inferred.35
In the first (118 control and 121 intervention subjects with GCS >10, in a pre-post study design), QTs (dimmed lights, decreased telephone volumes, quiet staff conversations, minimal nursing activities, no visitors where possible) were from 14:00 to 16:00 and 02:00 to 04:00. Data were collected by 6 trained nurses at 02:45 and 03:30, and 14:45 and 15:30. Patients were 1.6 times more likely to be observed sleeping during QT than at the same times prior to their introduction (95% CI, 1.03–2.57, p < 0.001).28 Both sound levels and light exposure were consistently reduced during QT, and such reductions were independent sleep predictors (p < 0.001). However, when individual time-points were compared for percentage of patients asleep, only the afternoon periods significantly differed from baseline (p = 0.008). Additionally, such significant effects could remain attributable to the Hawthorne effect as patient awareness of QT could result in modified behaviour during these periods.
Dennis et al.20 studied trauma neuro-ICU patients with GCS >10 (none sedated or ventilated). Thirty-five patients were observed during daytime shifts, and a different group (15) at night.20 As before, two QTs were introduced (14:00–16:00 and 02:00–04:00). Data relating to sound and light exposure were collected six times/day for very brief periods (5 s), with measurement being made 30 min before and after the QT, and 30–60 min before its end. During the daytime QT, bedside sound exposure fell by 15% (p < 0.025), with a significant but smaller reduction at night. The same was found for light measurements (daytime light levels were 15–25% of those pre-intervention at the same timepoint, p < 0.025, whilst nighttime levels remained low independent of intervention). Patients were four times more likely to be observed sleeping during the afternoon QT than in the half hour before. The very brief objective measurements made – and their scarcity – limit conclusions, as does small sample size. The type of patient (unventilated, unsedated neurosurgical patients) limits conclusion generalizability.
Three more recent studies have used multiple simultaneous approaches to improve night sleeping conditions.26,27,29 All found improvements in environmental parameters but one found no difference in perceived sleep quality.26 Li et al. studied 55 surgical ICU patients. Routine care was compared to a three-month period following an intervention that included dimming of lights (23:00–05:00), lowering alarm volumes, and avoiding overnight investigations.27 Staff were educated by an in-service course and discussions. A sleep efficiency index (SEI, hours asleep/hours in bed) was calculated from the RCSQ35: SEI > 85% is indicative of good sleep quality,38 although in an intensive care setting where the majority of patients are bedbound this threshold may be too strict. This was significantly improved with intervention (72.2 ± 7.5 vs 69.3 ± 10.2, p = 0.047). Through the ‘Sleep in the ICU’ questionnaire (SICUQ) visual analogue scale (0–10), intervention patients reported less daytime sleepiness (6.75 ± 2.19 vs 5.33 ± 1.69, p = 0.01) than controls. However, unlike the RCSQ, the SICUQ is not validated against PSG in ICU patients.
The second study used an intervention bundle to reduce sound levels, light exposure and nocturnal disruptions in a general ICU.29 Staff training was supported by posters and by local champions. Non-ventilated and ventilated, elective and non-elective, medical and surgical patients were included. Patients discharged from the ICU earlier in the hospital admission, those with pre-existing cognitive disturbance or sleep pathology, and neurosurgical patients, were excluded. All were offered earplugs and eyemasks and were assessed for delirium daily (Confusion Assessment Method for ICU). RCSQ was completed each morning (with one randomly chosen for analysis), with SICUQ following discharge. Compared to baseline, patients had improved sleep duration (6.6 h vs 8.6 h, p < 0.001) and increased sleep efficiency/quality, with reduced daytime sleep (p = 0.042). Increase in the RCSQ SEI was associated with lower odds of developing delirium (OR 0.90, 95% confidence interval 0.85–0.97).
In contrast, one larger pre-post study (300 medical ICU patients) found no significant impact when environmental improvements to facilitate sleep, conservative methods (earplugs, eyemasks, or relaxing music), and a pharmacological sleeping aid (zolpidem or haloperidol) if patients were unable to sleep, were introduced in stages.26 Staff were extensively trained and used a daily checklist to aid implementation. Unlike the previous two articles, RCSQ was completed daily and all data for each patient analysed with a repeated measures design. However, patients were cared for in private rooms, there was no record of objective environmental sound or light exposure, and inclusion of patients with delirium/reduced consciousness led nurses to complete the RCSQ in 45% of cases. In addition, evidence that hypnotics and major tranquillisers improve sleep quantity/quality on ICU is lacking. Although RCSQ nurse-completion may be useful when patients are unable to do this themselves (Bourne, 2007), these differences between studies make them difficult to compare. Nonetheless, these data do suggest that interventions such as these may benefit the more alert (and potentially less unwell or confused) patients.
In summary, strategies to improve environmental sound levels and light exposure on the ICU mostly appear to subjectively improve sleep, but no studies used objective assessment methods. Heterogeneity between study locations, durations, interventions, and assessment measures and in the reporting of environmental factors, all hamper interpretation.
Sound interventions
Only two studies investigated the effects of applied sound or music to improve ICU sleep.23,31 Kamdar et al. also used music as part of a multifaceted intervention, but the effect of the ‘music component’ was not analysed separately. Both were conducted on either a cardiac or cardiac surgical ICU and used patient-completed validated sleep questionnaires.23,31 In the first, 58 patients were given eyemasks and earplugs, with half randomized to receive additional headphone sleep-inducing music that included nature sounds, delta wave control music, and Goldberg Variations BMV 988 (a composition by Bach).31 Delta-wave music describes music which produces higher levels of delta-wave brain pattern sleep. The choice of music in this study was based on an unpublished thesis, suggesting a lack of evidence to guide selection. Environmental sound levels and light exposure were not recorded. However, VSHSQ identified significantly improved subjective sleep quality (p < 0.001) in the intervention group with an additional 36 min of sleep when measured by the non-validated Quantity of Sleeping Questionnaire.
The second (more recent) study randomized 45 cardiac surgical ICU patients to routine care or an intervention that involved relaxing music of waves and frogs before bed, nature and bird songs in the morning, and to sleep with earplugs and eyemasks.23 Sleep quality, perceived nighttime noise, and sleep latency (by RCSQ) were significantly improved (p < 0.05) when compared to routine care. Given that there was no difference in environmental light and sound exposure between groups, it is unlikely these factors confounded the results.
Like many others in the field, neither of these studies reported room or bed types, and the results may not be transferrable to potentially more unwell general medical or surgical patients. Furthermore, evidence for the selection of music or sounds was lacking. Further studies would benefit from a greater reporting of known additional patient and environmental factors that could disturb the sleep of patients.
Conclusion
Our narrative review identified 15 publications that assessed the effect of non-pharmacological techniques to improve sound or light exposure on the sleep of adults on ICU and simulated ICU environments. The majority focused on the use of earplugs/eyemasks or environmental interventions and were generally favourable to different aspects of sleep such as subjective duration and quality.
Few studies used objective sleep assessments, and sleep assessment measures were not always validated. Sample sizes were often small. Methodologies were sometimes imperfect and analysis limited (e.g. subjects allocating themselves to one arm or another, and no statistical analysis of resulting data). Data substantially derive from specialist (neurosurgical, post-operative, cardiothoracic, cardiological) centres. Patients were often at the ‘less sick’ end of the spectrum and were in a variety of settings (open ward beds or side rooms).
Future research should be extended at scale to the broader ICU population. Studies should include objective measures of sound/light exposure, and the use of validated sleep questionnaires and PSG where appropriate. Studies should be prospectively powered, and appropriate control groups utilized. Confounding factors should be addressed. All of these factors are important if the impact of conservative techniques on the ICU environment and quantitative improvements in sleep is to be assessed.
Meanwhile, cheap and simple measures appear available which have low risk of harm and which may substantially improve patient experience.
Acknowledgements
We would like to thank Dr Ben O’Brien for his external input in reviewing and editing the manuscript.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: HM and the Institute for Sport Exercise and Health are supported by the University College London Hospitals NHS Trust/University College London (UCLH/UCL) NIHR Comprehensive Biomedical Research Centre.
References
- 1.Freedman NS, Kotzer N, Schwab RJ. Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Resp Crit Care Med 1999; 159: 1155–1162. [DOI] [PubMed] [Google Scholar]
- 2.Weinhouse GL, Schwab RJ. Sleep in the critically ill patient. Sleep 2006; 29: 707–716. [DOI] [PubMed] [Google Scholar]
- 3.Tembo AC, Parker V, Higgins I. The experience of sleep deprivation in intensive care patients: findings from a larger hermeneutic phenomenological study. Intens Crit Care Nurs 2013; 29: 310–316. [DOI] [PubMed] [Google Scholar]
- 4.Franck L, Tourtier JP, Libert N, et al. How did you sleep in the ICU? Crit Care 2011; 15: 408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andersen JH, Boesen HC, Skovgaard Olsen K. Sleep in the Intensive Care Unit measured by polysomnography. Minerva Anesthesiol 2013; 79: 804–815. [PubMed] [Google Scholar]
- 6.Novaes MA, Knobel E, Bork AM, et al. Stressors in ICU: perception of the patient, relatives and health care team. Intens Care Med 1999; 25: 1421–1426. [DOI] [PubMed] [Google Scholar]
- 7.Nelson JE, Meier DE, Oei EJ, et al. Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med 2001; 29: 277–282. [DOI] [PubMed] [Google Scholar]
- 8.Banks S, Dinges DF. Behavioral and physiological consequences of sleep restriction. J Clin Sleep Med 2007; 3: 519–528. [PMC free article] [PubMed] [Google Scholar]
- 9.Delaney LJ, Haren FV, Lopez V. Sleeping on a problem: the impact of sleep disturbance on intensive care patients - a clinical review. Ann Intens Care 2015; 5: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Figueroa-Ramos MI, Arroyo-Novoa CM, Lee KA, et al. Sleep and delirium in ICU patients: a review of mechanisms and manifestations. Intens Care Med 2009; 35: 781–795. [DOI] [PubMed] [Google Scholar]
- 11.Kamdar BB, Needham DM, Collop NA. Sleep deprivation in critical illness: its role in physical and psychological recovery. J Intens Care Med 2012; 27: 97–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tamburri LM, DiBrienza R, Zozula R, et al. Nocturnal care interactions with patients in critical care units. Am J Crit Care 2004; 13: 102–112. [PubMed] [Google Scholar]
- 13.Xie H, Kang J, Mills GH. Clinical review: The impact of noise on patients’ sleep and the effectiveness of noise reduction strategies in intensive care units. Crit Care 2009; 13: 208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Golombek DA, Ruth E. Rosenstein physiology of circadian entrainment. Physiol Rev 2010; 90: 1063–1102. [DOI] [PubMed] [Google Scholar]
- 15.Berglund B, Lindvall T, Schwela DH. Guidelines for community noise, Geneva: World Health Organization, 1999. [Google Scholar]
- 16.Young JD, Darbyshire JL. An investigation of sound levels on intensive care units with reference to the WHO guidelines. Crit Care 2013; 17: R187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kam PCA, Kam AC, Thompson JF. Noise pollution in the anaesthetic and intensive care environment. Anaesthesia 1994; 49: 982–986. [DOI] [PubMed] [Google Scholar]
- 18.Yasukouchi A, Ishibashi K. Non-visual effects of the color temperature of fluorescent lamps on physiological aspects in humans. J Physiol Anthropol Appl Human Sci 2005; 24: 41–43. [DOI] [PubMed] [Google Scholar]
- 19.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009; 62: e1–e34. [DOI] [PubMed] [Google Scholar]
- 20.Dennis CM, Lee R, Woodard EK, et al. Benefits of quiet time for neuro-intensive care patients. J Neurosci Nurs 2010; 42: 217–224. [DOI] [PubMed] [Google Scholar]
- 21.Foreman B, Westwood AJ, Claassen J, et al. Sleep in the neurological intensive care unit: feasibility of quantifying sleep after melatonin supplementation with environmental light and noise reduction. J Clin Neurophysiol 2015; 32: 66–74. [DOI] [PubMed] [Google Scholar]
- 22.Hu RF, Jiang XY, Zeng YM, et al. Effects of earplugs and eye masks on nocturnal sleep, melatonin and cortisol in a simulated intensive care unit environment. Crit Care 2010; 14: R66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu RF, Jiang XY, Hegadoren KM, et al. Effects of earplugs and eye masks combined with relaxing music on sleep, melatonin and cortisol levels in ICU patients: a randomized controlled trial. Crit Care 2015; 27: 115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang HW, Zheng BL, Jiang L, et al. Effect of oral melatonin and wearing earplugs and eye masks on nocturnal sleep in healthy subjects in a simulated intensive care unit environment: which might be a more promising strategy for ICU sleep deprivation? Crit Care 2015; 19: 124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jones C, Dawson D. Eye masks and earplugs improve patient’s perception of sleep. Nurs Crit Care 2012; 17: 247–254. [DOI] [PubMed] [Google Scholar]
- 26.Kamdar BB, King LM, Collop NA, et al. The effect of a quality improvement intervention on perceived sleep quality and cognition in a medical ICU. Crit Care Med 2013; 41: 800–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li SY, Wang TJ, Vivienne Wu SF, et al. Efficacy of controlling night-time noise and activities to improve patients’ sleep quality in a surgical intensive care unit. J Clin Nurs 2011; 20: 396–407. [DOI] [PubMed] [Google Scholar]
- 28.Olson DM, Borel CO, Laskowitz DT, et al. Quiet time: a nursing intervention to promote sleep in neurocritical care units. Am J Crit Care 2001; 10: 74–78. [PubMed] [Google Scholar]
- 29.Patel J, Baldwin J, Bunting P, et al. The effect of a multicomponent multidisciplinary bundle of interventions on sleep and delirium in medical and surgical intensive care patients. Anaesthesia 2014; 69: 540–549. [DOI] [PubMed] [Google Scholar]
- 30.Richardson A, Allsop M, Coghill E, et al. Earplugs and eye masks: do they improve critical care patients’ sleep? Nurs Crit Care 2007; 12: 278–286. [DOI] [PubMed] [Google Scholar]
- 31.Ryu MJ, Park JS, Park H. Effect of sleep-inducing music on sleep in persons with percutaneous transluminal coronary angiography in the cardiac care unit. J Clin Nurs 2012; 21: 728–735. [DOI] [PubMed] [Google Scholar]
- 32.Scotto CJ, McClusky C, Spillan S, et al. Earplugs improve patients’ subjective experience of sleep in critical care. Nurs Crit Care 2009; 14: 180–184. [DOI] [PubMed] [Google Scholar]
- 33.Van Rompaey B, Elseviers MM, Van Drom W, et al. The effect of earplugs during the night on the onset of delirium and sleep perception: a randomized controlled trial in intensive care patients. Crit Care 1012; 16: R73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wallace CJ, Robins J, Alvord LS, et al. The effect of earplugs on sleep measures during exposure to simulated intensive care unit noise. Am J Crit Care 1999; 8: 210–219. [PubMed] [Google Scholar]
- 35.Bourne RS, Minelli C, Mills GH, et al. Clinical review: Sleep measurement in critical care patients: research and clinical implications. Crit Care 2007; 11: 226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Watson PL, Pandharipande P, Gehlbach BK, et al. Atypical sleep in ventilated patients: empirical electroencephalography findings and the path toward revised ICU sleep scoring criteria. Crit Care Med 2013; 41: 1958–1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Edwards GB, Schuring LM. Pilot study: Validating staff nurses’ observations of sleep and wake states among critically ill patients, using polysomnography. Am J Crit Care 1993; 2: 125–131. [PubMed] [Google Scholar]
- 38.Richards KC, O’Sullivan PS, Phillips RL. Measurement of sleep in critically ill patients. J Nurs Meas 2000; 8: 131–144. [PubMed] [Google Scholar]


