Abstract
Purpose
To report a case with macular edema associated with uveitis, a decreased corneal endothelial cell density, and vitreous opacity caused by migrated intraocular antibiotic ointment after uneventful cataract surgery.
Observations
A 63-year-old man underwent uneventful sutureless superior clear corneal phacoemulsification and implantation of an intraocular lens in his right eye. Eleven months later, he complained of blurred vision when he gazed downward. Three months later, uveitis, vitreous opacity, and retinal hemorrhage were noted. Optical coherence tomography and fluorescein angiography demonstrated macular edema in the right eye. A slit-lamp examination revealed many tiny oily deposits on the iris surface. One month later, a globular oily droplet was detected at the 12 o'clock position of the iridocorneal angle. Because the corneal endothelial cell density appeared to be progressively decreased, the oily droplet was removed, and the anterior chamber was irrigated with a balanced salt solution using an irrigation-aspiration cannula. After surgery, the macular edema, vitreous opacity, and retinal hemorrhage disappeared.
Conclusions and importance
In this case, ofloxacin ointment had presumably migrated into the anterior chamber through a corneal incision after cataract surgery. The fact that the droplet of ointment was able to be detected more than one year after the cataract surgery suggests that dispersed tiny droplets can slowly coalesce into a globular droplet and wander between the anterior and posterior chambers, thereby causing uveitis, corneal endothelial cell damage, and macular edema. The removal of the intraocular ointment resolved these complications. This is the second report of intraocular ointment causing macular edema.
Keywords: Ofloxacin ointment, Corneal incision, Cataract surgery, Macular edema
1. Introduction
While rare, the intraocular migration of antibiotic ointment and its ocular complications have been reported.1, 2, 3, 4, 5, 6, 7 These complications include uveitis, secondary glaucoma, corneal decompensation, and toxic anterior segment syndrome.1, 2, 3 However, oily droplets of ointment have also been found late in the postoperative period without causing any ocular damage.5 To the best of our knowledge, there has only been one previous report regarding posterior segment complications caused by migrated intraocular ointment.6
We herein report the second rare case of macular edema associated with uveitis, vitreous opacity, retinal hemorrhage, and corneal endothelial density loss, presumably caused by migrated intraocular ointment, after uneventful cataract surgery with a clear-corneal incision.
2. Case report
A 63-year-old man underwent phacoemulsification and aspiration with intraocular lens (a single piece acrylic lens, Acrysof IQ®, Alcon) implantation for a cataract in the right eye. Preoperatively, there were no signs of uveitis or retinopathy, although he had diabetes mellitus and systemic hypertension that were well controlled by medical treatments. The surgery was uneventfully performed by one of our team (DT) employing a routine suture-less 2.0 mm superior clear-corneal incision. Ofloxacin ointment (Tarivid®, Santen, Osaka, Japan) was instilled at the end of surgery. The postoperative course was uneventful, the best-corrected visual acuity (BCVA) improved from preoperative 20/130 OD to 20/20 OD postoperatively. The corneal endothelial cell density was measured at 2053 cells/mm2 at the seventh day postoperatively. Eleven months later, he visited DT complaining of blurred vision in his right eye particularly when he gazed downward. His BCVA had dropped to 20/30 OD. Although he was being treated with topical 0.1% fluorometholone 3 times a day because of a conjunctival injection, there was no improvement, and the conjunctival injection worsened. One month later, although fluorometholone had been switched to 0.1% betamethasone and levofloxacin eyedrops 4 times a day, the vitreous became diffusely cloudy, and his BCVA decreased to 20/50 OD. One month after that, his BCVA further worsened to 20/70 OD, and retinal hemorrhage was noted in the right eye (Fig. 1). In addition, because many tiny oily particles were detected on the iris surface of his right eye (Fig. 2A), he was referred to Hirosaki University Hospital.
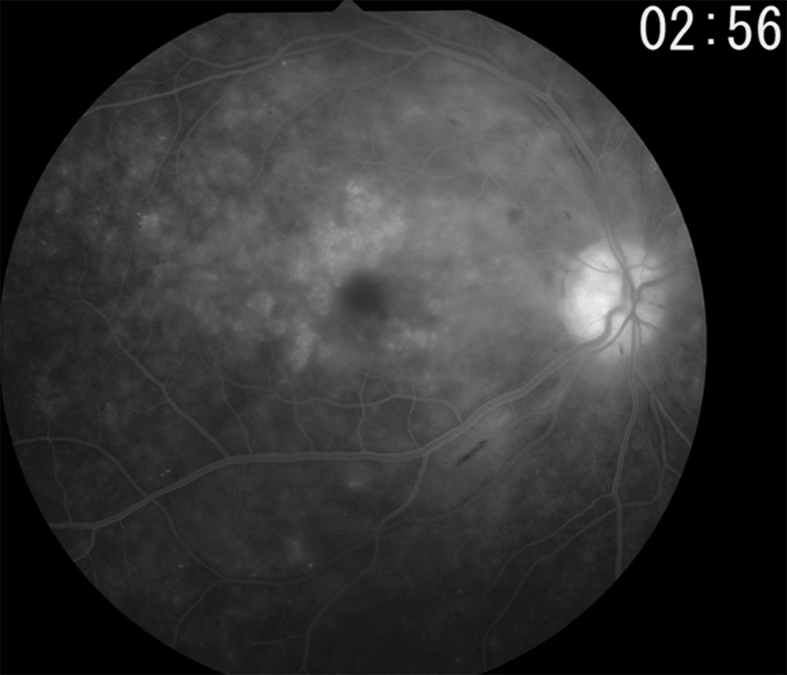
Fig. 1.
Fundus photograph of the right eye revealed diffuse vitreous opacity and retinal hemorrhage.
Fig. 2.
A) Slit-lamp microscopy showed tiny oily particles attached to the iris surface. B) A globular oily droplet was found at the 12 o'clock position of the anterior chamber. C) Gonioscopy revealed isolated, semi-translucent, globular oily droplet. D) Gonioscopic findings showed peripheral anterior synechia at the 12 o'clock position, associated with tiny oily droplets on the iris surface.
On an examination, his BCVA was 20/70 OD and 20/15 OS and his intraocular pressure was 19 mmHg OD and 15 mmHg OS. Slit-lamp biomicroscopy revealed a globular oily droplet at the 12 o'clock position of the iridocorneal angle (Fig. 2B and C), and optical coherence tomography (OCT) showed macular edema, particularly in the pericentral area (Fig. 3A and B). The macular edema was confirmed by fluid pooling in the macular area on fluorescein angiography (Fig. 4). The oily droplet was not always present in the anterior chamber. When the droplet was absent in the anterior chamber, gonioscopy revealed peripheral anterior synechia associated with tiny deposits attached on the surface (Fig. 2D). The corneal endothelial cell density was 915 cells/mm2 OD and 2690 cells/mm2 OS. Although the vitreous opacity gradually recovered with the administration of topical blomfenac sodium 4 times a day, the BCVA remained at 20/70 OD, and the corneal endothelial cell density further decreased to 822 cells/mm2. Because of progressive corneal endothelial cell loss, we decided to surgically remove the oily droplet and irrigate the anterior chamber.
Fig. 3.
A) Optical coherence tomography (OCT) showed thickening of the perimacular area, indicating macular edema. A retinal thickness analysis (internal limiting membrane – retinal pigment epithelial layer) revealed that the central macular thickness was 367 μm and that the averaged paracentral macular thickness was 420 μm. B) The b-mode image at the foveal center. C) and D) OCT findings at two months after the removal of the ointment. The retinal thickness was reduced (central macular thickness, 323 μm; averaged paracentral macular thickness, 359 μm) (C) and the macular edema had disappeared (D).
Fig. 4.
Fluorescein angiography revealed pooling of fluorescein dye, indicating macular edema.
At surgery, the anterior chamber was gently irrigated with a balanced salt solution (BSS plus®) using an irrigation-aspiration cannula (Simcoe cannula) inserted through a limbal incision (18G) at 9 o'clock. During the irrigation procedure, the oily droplet moved from the posterior chamber to the anterior chamber and was successfully aspirated using the cannula. At the end of surgery, 20 mg/0.5 ml of triamcinolone solution was injected into the Tennon's capsule.
Postoperatively, the patient's BCVA improved to 20/25 OD, his macular edema was found to have recovered on OCT (Fig. 3C and D), and the vitreous opacity and retinal hemorrhage disappeared.
3. Discussion
Antibiotic ointment instilled at the end of eye surgery can rarely but occasionally migrate into the anterior chamber through a clear-corneal incision.1, 2, 3, 4, 5, 6, 7 Most previous reports on this subject were cases of small-incision cataract surgery employing a suture-less clear-corneal incision,1, 2, 3, 4, 5, 6 and one case was reported after a penetrating corneal transplantation.7 Although most of cataract surgeries with clear-corneal incisions are uneventful, the instilled ointment may be inadvertently aspirated into the anterior chamber by negative pressure created by the removal of the lid speculum, pushing on the eye ball, or lid squeezing.5 Vasavada et al. reported that even stromal hydration cannot completely prevent the ingress of trypan blue into the anterior chamber, although stromal hydration is statistically more effective in preventing trypan blue ingress than non-hydration.8
Intraocular ointment is found at various periods throughout the postoperative course. Aralitatti et al. reported the presence of migrated ointment early in the postoperative period after noting smearing on the surface of the intraocular lens.2 Wong et al. noted a spherical droplet two months after cataract surgery.3 Wong et al. in another group have speculated that tiny particles of ointment might gradually coalesce into a large droplet, as the droplet in their case was detected two years after cataract surgery.5 In our case, the fact that an oily droplet was found more than a year after cataract surgery supports this possibility. In addition, we observed the movement of the droplet from the posterior chamber to the anterior chamber during the removal surgery. This phenomenon suggests two possibilities. The first is that a droplet may wander between the anterior and posterior chambers, depending on the patient's face position. This might explain why the patient complained of blurred vision only when he gazed downward. The second is that the droplet may cause corneal endothelial cell damage and/or uveitis that subsequently induces vitreous opacity and macular edema. Although Lee et al. first reported a case of macular edema associated with the inadvertent entry of ointment,6 this complication seems to be rare. Our case is the second report of macular edema as a complication of migrated intraocular ointment.
It goes without saying that the toxicity of intraocular ointment largely depends on its ingredients. In the previous case reported by Wong et al.,5 gas chromatography-mass spectrometry revealed that the removed ointment contained several peaks for docosane (C22), tricosane (C23), and tetracosane (C24) hydrocarbones that coincided with those of the control ointment of dexamethasone, neomycin, and polymyxin B in a petrolatum and lanolin base. These ingredients do not seem to be harmful for at least two years postoperatively.5 However, in our present case and other cases reported previously,1, 2, 3, 4 ocular complications occurred due to intraocular ointment. Because the removal of the intraocular ointment resulted in the resolution of macular edema and improvement of the BCVA, the toxicity of the ointment is obvious. Ofloxacin ointment was used in our case, and chrolamphenicol,3,6 or antibiotics/steroid ointment4 and pilocarpine gel4 were used in the previous cases. Moreover, not only medical properties but also other ingredients such as petrolatum (C15∼C20 poly-saturated hydrocarbons), paraffin (C20∼ poly-unsaturated hydrocarbons), or lanolin (C13∼C24 esterified fat) should be considered. It remains to be studied in the future which ingredients demonstrate ocular toxicity.
4. Conclusion
Although instilled ointment may rarely and inadvertently migrate into the anterior chamber through a suture-less clear-corneal incision in the early postoperative periods, a globular droplet of retained ointment may be formed in the late postoperative periods. Intraocular ofloxacin ointment can cause uveitis, vitreous opacity, macular edema, and corneal endothelial loss. However, uveitis, vitreous opacity, and macular edema may disappear after removal of the intraocular ointment.
Patient consent
Written consent to publish the report was obtained from the patient.
Acknowledgement and disclosures
Research funds
Alcon Japan, Santen, K-vision, Novertis, AMO, and Phizer. Grant-in-aids (15K20145, 17K16954, 17K11416) for Scientific Research from the Japanese Society for Promotion of Science.
Conflicts of interest
The following authors have no financial disclosures: AK, TK, DT, TM, YS, MN.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Acknowledgement
The authors would like to thank Mr. Brian Quinn for his English editing.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ajoc.2018.02.027.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Riedl M., Maca S., Amon M., Nennadal T., Kruger A., Barisani T. Intraocular ointment after small-incision cataract surgery causing chronic uveitis and secondary glaucoma. J Cataract Refract Surg. 2003;29(5):1022–1025. doi: 10.1016/s0886-3350(03)00060-9. [DOI] [PubMed] [Google Scholar]
- 2.Aralitatti A.K.V., Needham A.D., Lee M.W., Prasad S. Entry of antibiotic ointment into the anterior chamber after uneventful phacoemulsification. J Cataract Refract Surg. 2003;29(3):595–597. doi: 10.1016/s0886-3350(02)01503-1. [DOI] [PubMed] [Google Scholar]
- 3.Wong J.G., Bank A. Surgical removal of intraocular antibiotic ointment after routine cataract phacoemulsification. J Cataract Refract Surg. 2006;32(5):890–892. doi: 10.1016/j.jcrs.2006.01.071. [DOI] [PubMed] [Google Scholar]
- 4.Werner L., Sher J.H., Taylor J.R. Toxic anterior segment syndrome and possible association with ointment in the anterior chamber following cataract surgery. J Cataract Refract Surg. 2006;32(2):227–235. doi: 10.1016/j.jcrs.2005.12.093. [DOI] [PubMed] [Google Scholar]
- 5.Wong V.W., Chu K.O., Lam P.T., Yam G.H., Lai T.Y. Late appearance of an intracameral ophthalmic ointment globule after uneventful phacoemulsification. Jpn J Ophthalmol. 2009;53(3):553–555. doi: 10.1007/s10384-009-0701-8. [DOI] [PubMed] [Google Scholar]
- 6.Lee E.J., Wong R., Laidlaw D.A. Late-onset cystoid macular edema associated with small-incision cataract surgery and inadvertent entry of chloramphenicol ointment into the anterior chamber. Ophthalmic Surg Laser Imag. 2010 Mar 9:1–3. doi: 10.3928/15428877-20100216-09. [DOI] [PubMed] [Google Scholar]
- 7.Chan E., Smallwood R., Fernández López E. Intracameral antibiotic ointment following penetrating keratoplasty. Ophthalmology. 2016;123(6):1374. doi: 10.1016/j.ophtha.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Vasavada A.R., Praveen M.R., Pandita D. Effect of stromal hydration of clear corneal incisions: quantifying ingress of trypan blue into the anterior chamber after phacoemulsification. J Cataract Refract Surg. 2007;33(4) doi: 10.1016/j.jcrs.2007.01.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.