Abstract
Purpose
To describe a case of Multi-drug resistant Mycobacterium chelonae scleral buckle infection.
Observations
A 56 year-old male with history of retinal detachment repair with scleral buckle 20 years prior presented with 8 months of intermittent pain and redness in the left eye. The patient was diagnosed with scleral buckle infection, the buckle was removed, and cultures revealed multi-drug resistant Mycobacterium chelonae. The postoperative course included orbital cellulitis treated with systemic linezolid, clarithromycin, and imipenem. All systemic antibiotics were discontinued on post-operative day 25, visual acuity improved to 20/25, the retina remained attached, and no recurrence occurred over 3 years of follow-up.
Conclusions and importance
NTM infections are typically chronic and often require lengthy treatment. SB infection is rare, but often associated with biofilm and antibiotic resistance. In spite of removing the SB, anchoring sutures, sheath surrounding the buckle and associated biofilm, a prolonged course of systemic antibiotics may be necessary in some patients.
Keywords: Non-tuberculous mycobacterium, Scleral buckle, Orbital cellulitis
1. Introduction
Complications of scleral buckling include induced myopia, diplopia, foreign body sensation, infection, extrusion, and intrusion.1, 2, 3 Scleral buckle (SB) infections are rare, with rates as low as 0.2%.4 This case report will focus on the clinical course and duration of antibiotic management in a patient with SB infection due to multi-drug resistant Mycobacterium chelonae.
2. Case report
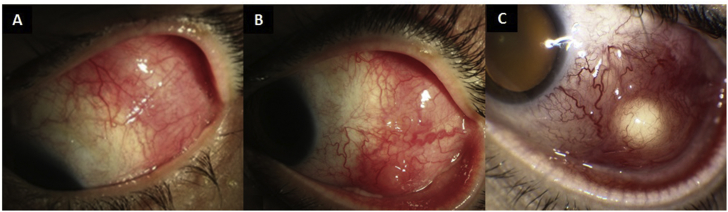
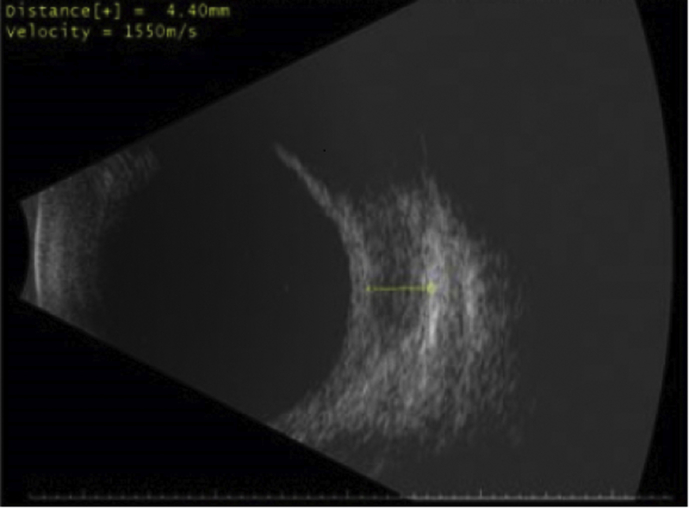
A 56 year-old male with history of retinal detachment (RD) repair with SB 20 years prior presented with 8 months of intermittent pain and redness in the left eye, improved transiently with oral antibiotics. Best-corrected visual acuity (VA) was 20/25 in both eyes. Examination of the left eye was significant for a nodular lesion with fistula, conjunctival congestion, and chemosis of the bulbar conjunctiva in the areas of SB (Fig. 1A–C). Intraocular exam was significant for SB and inactive chorioretinal scars from prior laser. Ocular ultrasound demonstrated fluid collection within Tenon's capsule (Fig. 2).
Fig. 1.
1A, 1B: Nodular inflammation of the bulbar conjunctiva in the distribution of the scleral buckle temporally and superiorly; 1C: Subconjunctival abscess formation.
Fig. 2.
Bscan demonstrating fluid collection within Tenon's capsule and surrounding the screlal buckle at the equator on ocular ultrasound.
The patient was diagnosed with SB infection and was advised to have the buckle removed.2 The patient was resistant to surgery, thus a compromise of incision and drainage was performed. The culture results identified Staphylococcus epidermidis, Streptococcus viridans, and Neisseria sicca and the patient was treated with topical Trimethoprim/Polymyxin B. Two weeks later due to lack of clinical improvement, the patient agreed to have the buckle removed and sent for culture. Gentamicin irrigation was used copiously in the subconjunctival space, and subconjunctival vancomycin and gentamicin were administered after closure of the conjunctival peritomy. Intraoperative cultures including the SB were held for several weeks due to clinical suspicion of atypical organisms, and culture identified multi-drug resistant Mycobacterium chelonae (Table 2). S. epidermidis, S. viridans, and N. sicca were not isolated from the removed scleral buckle culture, and the patient was treated post-operatively with Neomycin/Polymyxin B/Dexamethasone drops.
Table 2.
In vitro antibiotic susceptibility data of M. chelonae from explanted scleral buckle culture.
| Antimicrobial | MIC (mcg/mL)a | Interpretationb |
|---|---|---|
| Amikacin | 8 | Susceptible |
| Cefoxitin | 64 | Intermediate |
| Ciprofloxacin | >4 | Resistant |
| Clarithromycin | 16 | Resistant |
| Doxycycline | >16 | Resistant |
| Imipenem | 16 | Intermediate |
| Linezolid | 16 | Intermediate |
| Moxifloxacin | >8 | Resistant |
| Tigecycline | 1 | c |
| Tobramycin | 8 | Resistant |
| Trimethoprim/Sulfamethoxazole | >8/152 | Resistant |
Minimum inhibitory concentration.
All break points are based on Clinical and Laboratory Standards Institute (CLSI) guidelines.
Tigecycline has no CLSI interpretations and only MIC values are reported.
On postoperative day four, the patient returned to the emergency room with pain, proptosis, restriction of ocular motility, afferent pupillary defect, and decreased vision. He was diagnosed with orbital cellulitis possibly associated with residual infection material or biofilm after SB removal, and was admitted for treatment with systemic clarithromycin 500mg BID, linezolid 600mg TID, and IV imipenem 1000mg TID. The patient demonstrated resolution of orbital cellulitis and pain, thus all antibiotics were stopped at post-operative day 25. Without any further treatment, visual acuity improved to 20/25, the retina remained attached, and no recurrence occurred over 3 years of follow-up.
3. Discussion
Infections after SB are rare.4 SB exposure is a major risk factor,4 and removal of the SB is well tolerated, carries a low rate of recurrent RD,5 and has a high rate of culture positive identification of the organism.4,6, 7, 8 Common organisms include coagulase negative staphylococci,6 Mycobacterium chelonae,9 Proteus mirabilis,6 gram positive cocci, and acid-fast bacilli.8 Vancomycin, ciprofloxacin, and amikacin provide the best coverage in SB-related infections (Table 1).4,6, 7, 8 Topical besifloxacin has been recently used as an adjunct treatment in M. chelonae keratitis and nodular conjunctivitis, and its potential role in these cases can be considered.10
Table 1.
Summary of microbial isolates and treatment recommendations for removed scleral buckles.
| Study | Smiddy et al.6 | Pathengay et al.7 | Chhlabani et al.4 | Mohan et al.8 |
|---|---|---|---|---|
| Years | 1985–1991 | 1992–2002 | 2003–2012 | 2007–2012 |
| Number of buckles analyzed | 45 | 73 | 51 | 25 |
| Location | Miami | India | India | India |
| Culture Positivity Rate, % | 73.3 | 83.3 | 78.3 | 83.33 |
| Most common culture isolate, % | Coagulase-negative Staph (52) | Coagulase-negative Staph (27.4) | Gram negative bacteria (25) | Atypicala mycobacteria (23.8) |
| Atypicala mycobacteria, % | 18 | 20.5 | 18 | 23.8 |
| Fungal isolates, % | 2.3 | 15.1 | 16 | 19 |
| Polymycrobial infection, % | 32.7 | 21.1 | 7.8 | 5 |
| Suggested first-line treatment | Vancomycin, Aminoglycoside | Vancomycin, Ciprofloxacin, Amikacin | Vancomycin, Ciprofloxacin, Amikacin | Vancomycin, Amikacin |
Atypical mycobacteria: Acid-fast mycobacteria that do not cause tuberculosis nor leprosy.
Nontuberculous mycobacterium (NTM) infections are typically challenging to manage due to delayed laboratory identification, poor drug penetration, slow response to therapy, and need for prolonged and combined treatment. Risk factors for NTM ocular infection include biomaterial implants such as SB or orbital implant, ocular surgery, and steroid exposure.11 Biofilm formation may occur even without exposure, and is thought to be responsible for SB infections that persist despite systemic antibiotic therapy.12,13
The unique features of this case were late presentation with subconjunctival abscess in the absence of buckle exposure, progression to orbital cellulitis despite removal of scleral buckle, and resolution of infection within 3 weeks of systemic antibiotics. Orbital cellulitis has been associated with silicone-sponge buckles; however, cellulitis is uncommon after buckle removal.15 Infectious disease literature recommend lengthy antibiotic treatment greater than 10 weeks.14 The challenge in managing this patient's SB-related NTM ocular infection was in deciding when to discontinue systemic antibiotics, particularly given concern for the orbital cellulitis. An inadequate course of antibiotics could lead to chronic orbital infection, but prolonged use of Amikacin could potentially result in nephrotoxicity and ototoxicity. The decision for SB removal was made to eliminate both the infectious nidus as well as its associated biofilm. With no source of infection present, no pain, visual complaints, fever, leukocytosis, nor elevated sedimentation rate, the ophthalmology team felt that it was clinically safe and appropriate to discontinue systemic antibiotics on post-operative day 25, much earlier than 10 weeks of therapy recommended by the infectious disease team. The patient chose to stop systemic therapy and demonstrated no recurrence over 3 years of follow-up.
In conclusion, NTM infections are typically chronic and often require lengthy treatment. SB infection is rare, but often associated with biofilm and antibiotic resistance. In spite of removing the SB, anchoring sutures, sheath surrounding the buckle and associated biofilm, a prolonged course of systemic antibiotics may be necessary in some patients.
4. Patient consent
This report does not contain any personal information that could lead to the identification of the patient.
Acknowledgements and disclosures
Funding
This report is supported in part by NIH Center Core Grant P30EY014801 and Research to Prevent Blindness Unrestricted Grant.
Conflicts of interest
The following authors have no financial disclosures: DSC, KDT, RCY, NG, CA, HWF.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Ulrich R.A., Burton T.C. Infections following scleral buckling procedures. Arch Ophthalmol. 1974;92(3):213–215. doi: 10.1001/archopht.1974.01010010221007. [DOI] [PubMed] [Google Scholar]
- 2.Tsui I. Scleral buckle removal: indications and outcomes. Surv Ophthalmol. 2012;57(3):253–263. doi: 10.1016/j.survophthal.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Farr A.K., Guyton D.L. Strabismus after retinal detachment surgery. Curr Opin Ophthalmol. 2000;11(3):207–210. doi: 10.1097/00055735-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Chhablani J., Nayak S., Jindal A. Scleral buckle infections: microbiological spectrum and antimicrobial susceptibility. J Ophthalmic Inflamm Infect. 2013;3(1):67. doi: 10.1186/1869-5760-3-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwartz P.L., Pruett R.C. Factors influencing retinal redetachment after removal of buckling elements. Arch Ophthalmol. 1977;95(5):804–807. doi: 10.1001/archopht.1977.04450050082007. [DOI] [PubMed] [Google Scholar]
- 6.Smiddy W.E., Miller D., Flynn H.W., Jr. Scleral buckle removal following retinal reattachment surgery: clinical and microbiologic aspects. Ophthalmic Surg. 1993;24(7):440–445. [PubMed] [Google Scholar]
- 7.Pathengay A., Karosekar S., Raju B., Sharma S., Das T. Hyderabad Endophthalmitis Research G. Microbiologic spectrum and susceptibility of isolates in scleral buckle infection in India. Am J Ophthalmol. 2004;138(4):663–664. doi: 10.1016/j.ajo.2004.04.056. [DOI] [PubMed] [Google Scholar]
- 8.Mohan N., Kar S., Padhi T.R., Basu S., Sharma S., Das T.P. Changing profile of organisms causing scleral buckle infections: a clinico-microbiological case series. Retina. 2014;34(2):247–253. doi: 10.1097/IAE.0b013e3182979e4a. [DOI] [PubMed] [Google Scholar]
- 9.Eifrig C.W., Scott I.U., Flynn H.W., Smiddy W.E., Newton J. Endophthalmitis after pars plana vitrectomy: incidence, causative organisms, and visual acuity outcomes. Am J Ophthalmol. 2004;138(5):799–802. doi: 10.1016/j.ajo.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen A.T., Hong A.R., Baqai J., Lubniewski A.J., Huang A.J. Use of topical besifloxacin in the treatment of Mycobacterium chelonae ocular surface infections. Cornea. 2015;34(8):967–971. doi: 10.1097/ICO.0000000000000492. [DOI] [PubMed] [Google Scholar]
- 11.Girgis D.O., Karp C.L., Miller D. Ocular infections caused by non-tuberculous mycobacteria: update on epidemiology and management. Clin Exp Ophthalmol. 2012;40(5):467–475. doi: 10.1111/j.1442-9071.2011.02679.x. [DOI] [PubMed] [Google Scholar]
- 12.Holland S.P., Pulido J.S., Miller D. Biofilm and scleral buckle-associated infections. A mechanism for persistence. Ophthalmology. 1991;98(6):933–938. doi: 10.1016/s0161-6420(91)32199-7. [DOI] [PubMed] [Google Scholar]
- 13.Asaria R.H., Downie J.A., McLauglin-Borlace L., Morlet N., Munro P., Charteris D.G. Biofilm on scleral explants with and without clinical infection. Retina. 1999;19(5):447–450. doi: 10.1097/00006982-199909000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Wallace R.J., Jr., Swenson J.M., Silcox V.A., Bullen M.G. Treatment of nonpulmonary infections due to Mycobacterium fortuitum and Mycobacterium chelonei on the basis of in vitro susceptibilities. J Infect Dis. 1985;152(3):500–514. doi: 10.1093/infdis/152.3.500. [DOI] [PubMed] [Google Scholar]
- 15.Nemet A.Y., Ferencz J.R., Segal O., Meshi A. Orbital cellulitis following silicone-sponge scleral buckles. Clin Ophthalmol. 2013;7:2147–2152. doi: 10.2147/OPTH.S50321. [DOI] [PMC free article] [PubMed] [Google Scholar]