Abstract
Purpose
Cotton Wool Spots (CWS) are a commonly described retinal finding in the posterior segment associated with an extensive number of systemic diseases. The appearance of a CWS in the setting of glaucoma has rarely been reported and has not been correlated with pathology to localized loss of the nerve fiber layer previously. In this case report, we augment a previous report of an 18 year old female with a diagnosis of low grade ciliary body melanoma. This patient experienced eventual mechanical angle closure with a CWS appearing in the posterior pole in the setting of acute elevation of intraocular pressure (IOP). This eye underwent enucleation and pathology evaluation.
Observations
Fundus photography documented a CWS in the posterior segment during a period of acute elevation in IOP. Subsequently the eye was enucleated due to pain from refractory angle closure glaucoma secondary to low grade iris-ciliary body ring melanoma. The specific site of the prior CWS was studied with 1μ Epon retinal step sections stained with a novel AgNO3 solution. Light microscopy demonstrated a retinal nerve fiber layer scar and inner nuclear layer collapse in the prior location of the CWS. Light microscopy and transmission electron microscopy shortly after enucleation had demonstrated temporal quadrant laminar optic nerve (ON) retrograde axonal transport block.
Conclusions and Importance
Although not commonly associated with glaucoma, CWS can present in the setting of acute elevations of IOP and may be associated with loss of nerve fiber layer. This loss of nerve fiber layer can confound the ability to judge glaucoma progression based on nerve fiber layer thickness via optical coherence tomography and changes in disc contours. Patient care may benefit from care provider's awareness of this possible phenomenon in the setting of angle closure.
Keywords: Cotton wool spots, Secondary angle closure glaucoma, Optic nerve, Retinal nerve fiber layer, Inner nuclear layer, Optical coherence tomography
1. Introduction
This case report extended from the original report, to our knowledge, is the first to provide histopathological co-localization of retinal damage corresponding to a long faded CWS in angle closure glaucoma.1 Cotton wool spots (CWS) are a well-described retinal finding occurring in association with many different well understood and idiopathic systemic retinal-vascular diseases, most commonly diabetes and hypertension.2 Typical CWS appear as transient gray to white areas with indistinct borders in the retinal nerve fiber layer (RNFL) usually less than 1/3 disc diameter, often adjacent to small retinal vessels. CWS contain clusters of cytoid bodies which form due to focal obstruction of orthograde or retrograde axonal transport in retinal ganglion cell axons.2, 3, 4 CWS usually fade over a few weeks following initial presentation and have only recently been associated with lasting retinal or disc damage.5, 6, 7 Most CWS will appear in the posterior fundus without any loss of visual acuity unless the central macula is involved. Traditional assumptions held that following the resolution of a CWS there were no pathological sequelae. Subsequent investigation with scanning laser ophthalmoscopy has shown localized loss of nerve fiber layer thickness corresponding with prior CWS 5, 6, 7. Therefore, CWS are not as innocuous as previously assumed. The incidence of CWS has rarely been reported in association with glaucoma (3) and subsequent co-localized pathologic examination following resolution of CWS has not previously been reported.
2. Case report
An 18 year old female was diagnosed with unilateral secondary angle closure as a result of ring melanoma of the ciliary body OS, detailed in a previous report(1). She was initially followed for iris abnormalities that were misdiagnosed initially as iridocorneal endothelial syndrome (ICE) and followed over three years during which she maintained an uncorrected visual acuity of 20/20 OD and between 20/20 and 20/25 OS. During the last three months of follow up prior to her histologic diagnosis of low grade iris melanoma, she developed increasingly frequent IOP spikes (30–60 mmHg) refractive to medical treatment and gonioscopy consistent with progressive angle closure secondary to an expanding iris-ciliary body ring melanoma. A CWS in the superior arcuate RNFL was first documented with fundus photography 5/6/79. The CWS had completely faded by subsequent fundus exam and photo 7/6/1979 (Fig. 1), the last before enucleation OS. The patient did not experience any vascular occlusive phenomenon or undergo radiotherapy prior to the appearance of the CWS on clinical exam. Her last Octopus visual field test (Fig. 2) demonstrated a stable early superior nasal step in the left eye. Disc cupping was minimal and stable in annual stereo disc photos prior to her spiking IOP and increasing angle closure (Fig. 3). Once the melanoma diagnosis was established and the tumor considered inoperable, enucleation was recommended. Low grade iris-ciliary body melanoma was proven histologically after enucleation in August of year 3 of follow up and confirmed partial angle closure by tumor extension in ring fashion in the ciliary body, iris and angle.
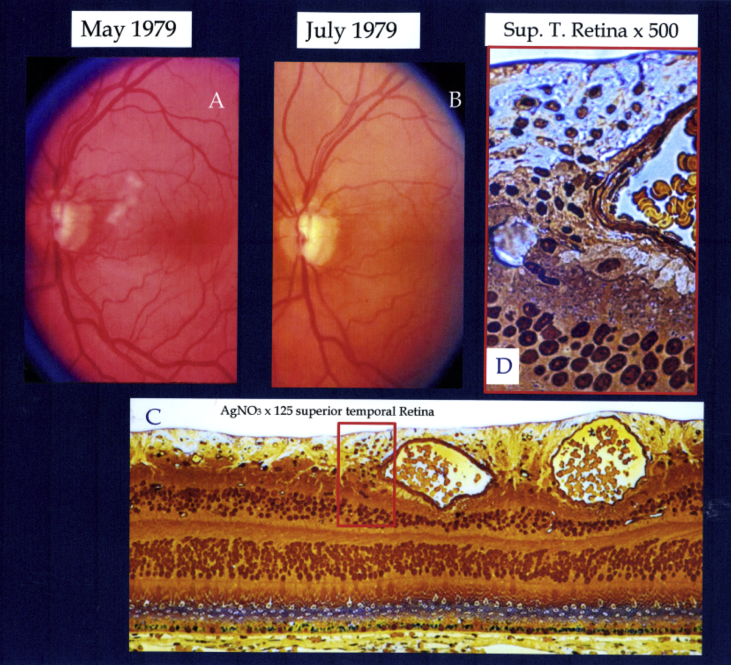
Fig. 1.
Fundus Photo OS during and after resolution of cotton wool spots and correlating histopathology from superior temporal macula. Relevant findings include a collection of glial cells in the nerve fiber layer and partial collapse of the middle nuclear layer. AGNO3, Epon 1μ section X 27.5 & 125.
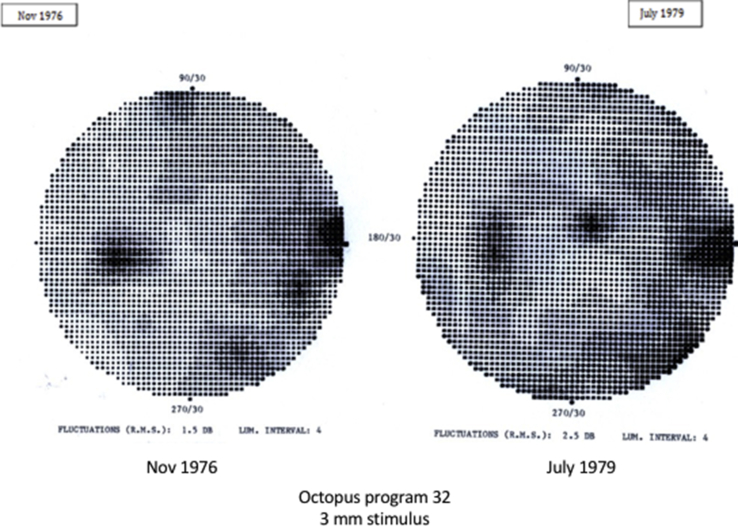
Fig. 2.
An Octopus VF in Nov 1976 OS revealed an early nasal step clearly progressed by August 1979.
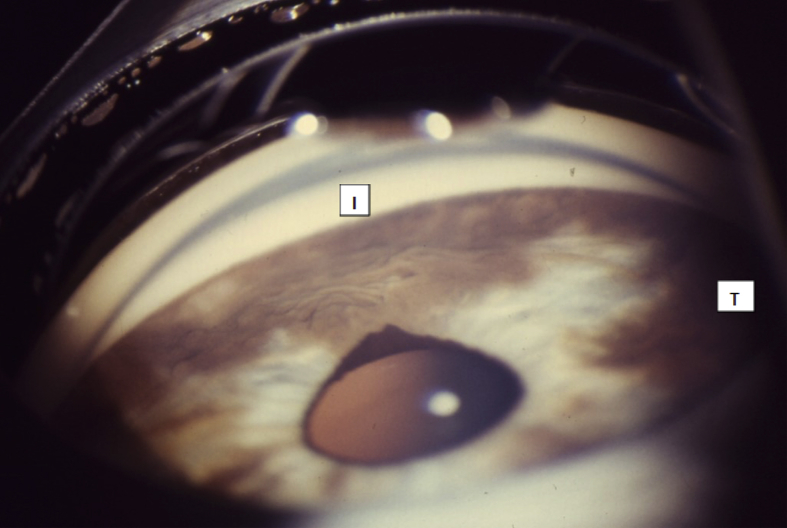
Fig. 3.
Inferior view via Köeppe gonioscopy demonstrating extensive angle involvement by subsequently proven low-grade malignant melanoma of ciliary body and iris. Pupil peaking and ectropion toward the largest area of iris surface tumor inferiorly (I) and temporally (T), a classic sign of iris malignancy, spurred the need for a biopsy and eventual enucleation. Neovascularization of the iris was not present clinically or histologically, but tumor did invade the dilator muscle in the periphery of the more involved inferior and temporal iris. Tumor effectively closed one-half to two-thirds of the angle OS.
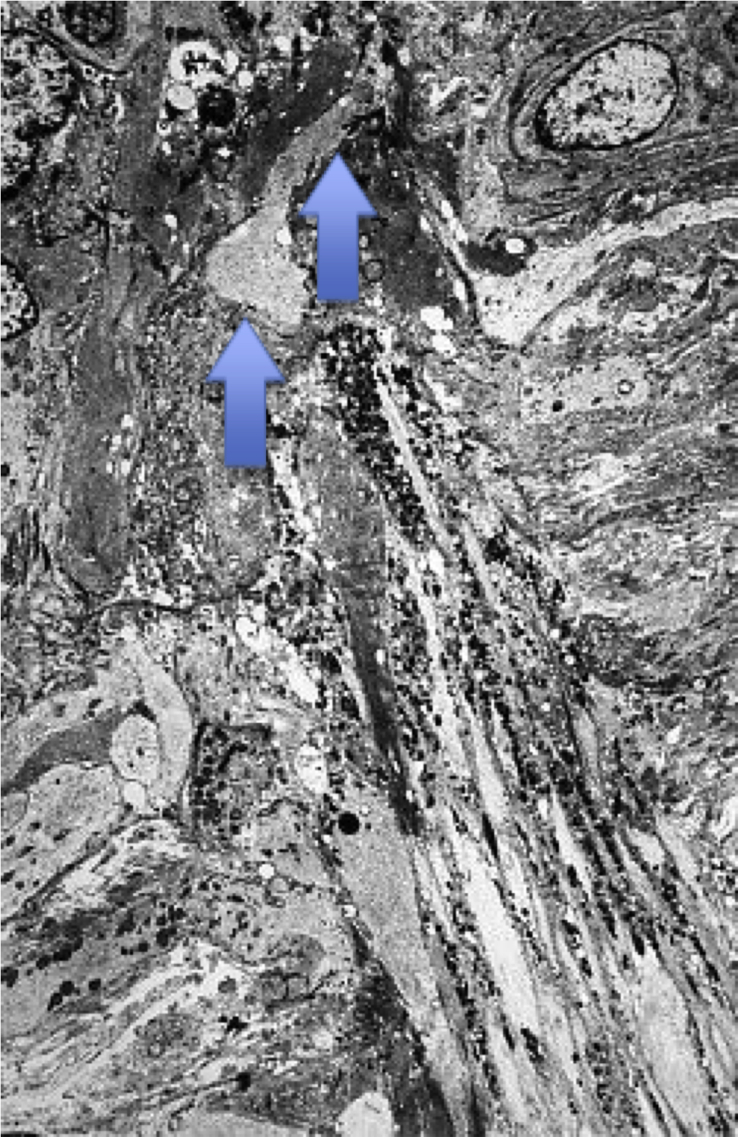
This report augments a prior report 1. On review, 36 years later prompted by a recent complex imaging study,5 1μ Epon retinal step sections originally stained with a novel AgNO3 solution demonstrated a retinal nerve fiber layer (RNFL) scar and inner nuclear layer (INL) collapse in the prior location of the CWS.5,8 (Fig. 1). Light microscopy (LM) and transmission electron microscopy (TEM) (Fig. 4) shortly after enucleation had demonstrated temporal quadrant laminar optic nerve (ON) retrograde axonal transport block.1
Fig. 4.
Electronmicrograph from the inferior pole of the optic nerve of our Case with secondary angle closure glaucoma demonstrating primarily retrograde axonal transport block in the temporal lamina cribrosa. The accumulation of intra-axonal debris is most prominent posterior to a glial-collagen beam (blue arrows) and confined to the axonal bundle in between horizontally oriented glial column cells. Vitreous up. (X 4600). Reproduced by Permission of the Survey of Ophthalmology.1. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Wolter previously mentioned the occurrence of CWS in angle closure glaucoma and described the morphology of terminal end bulb swelling in nerve fiber layer axons via a silver stain and light microscopy but offered no explanation of the pathophysiology.3 This case again demonstrates that angle closure glaucoma can lead to a CWS. Prior literature has concluded that the underlying mechanism for CWS is localized retinal arteriolar insufficiency. Glaucoma has generally not been listed among the possible causes.2 Malignancy has been reported as a possible etiology of CWS as it can result in localized vascular insufficiency due to shunting of blood flow or metastatic blockade of small retinal vessels. In this case, an asymptomatic CWS appeared in the posterior fundus far from the malignant site in the iris and ciliary body and there was no evidence of spread of the spindle melanoma beyond those sites. Since the appearance of the CWS corresponded with a period of unstable highly spiking IOP we speculate that the CWS most likely was triggered by high IOP, documented as elevated intermittently to 60 mmHg.
3. Discussion
To our knowledge, this delayed follow-up case report is the first to describe a CWS appearing during the course of secondary angle closure glaucoma with subsequent co-localization of a retinal nerve fiber layer (RNFL) scar and inner nuclear layer (INL) collapse corresponding to the prior CWS. Other investigators have shown alterations in clinical glaucoma testing with OCT and scanning laser ophthalmoscopy corresponding to prior occurrence of CWS in AIDS and systemic hypertension.5, 6, 7 Although detection of peripapillary disc hemorrhages has been regarded as a sign of ongoing glaucomatous disease, especially in low tension glaucoma, the finding of a CWS in the setting of angle closure glaucoma warrants caution in attributing loss of RNFL thickness to glaucomatous injury. Although we are reporting a correlation between CWS and angle closure glaucoma, the exact mechanism of occurrence is unclear. We theorize that an acute rise in intraocular pressure may result in focal retinal vascular insufficiency due to abrupt change in ocular perfusion pressure. Our patient's young age and good general health seem inconsistent with systemic vascular compromise. Although our patient experienced high IOP in the setting of angle closure, it is unlikely that the CWS found on examination is specific to angle closure, and could also occur in the setting of high IOP due to other mechanisms.
4. Conclusions
In summary, CWS can occur in angle closure glaucoma and ophthalmologists should be aware of this possibility as the subsequent testing of VFs, nerve fiber layer integrity and disc contours can be altered as a result of focal damage associated with the CWS. Eye care providers are encouraged to note and document CWS in glaucoma as they are not generally recognized as an associated sign. The localized loss of the RNFL as a sequelae of CWS can potentially be confused with progression of glaucomatous injury.
5. Patient consent
Written consent to publish case details has been obtained from each patient. Approval was obtained in writing and in compliance with HIPPA and Declaration of Helsinki.
Acknowledgements and disclosures
Funding
No funding or grant support.
Conflicts of interest
The following authors have no financial disclosures (AB, CN, SM, DM).
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
This research was in part supported by an unrestricted grant from Research to Prevent Blindness.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ajoc.2018.02.028.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Minckler D.S., Spaeth G.L. Optic nerve damage in glaucoma. Surv Ophthalmol. 1981;26:126–148. doi: 10.1016/0039-6257(81)90061-8. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt D. The mystery of cotton-wool spots-a review of recent and historical descriptions. Eur J Med Res. 2008;13(6):231. [PubMed] [Google Scholar]
- 3.Wolter J.R. Pathology of a cotton-wool spot. Am J Ophthalmol. 1959;48(4):473–485. doi: 10.1016/0002-9394(59)90883-9. [DOI] [PubMed] [Google Scholar]
- 4.McLeod D., Marshall J., Kohner E.M., Bird A.C. The role of axoplasmic transport in the pathogenesis of retinal cotton-wool spots. Br J Ophthalmol. 1977;61(3):177–191. doi: 10.1136/bjo.61.3.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomez M.L., Mojana F., Bartsch D.U., Freeman W.R. Imaging of long-term retinal damage after resolved cotton wool spots. Ophthalmol Times. 2009;116(12):2407–2414. doi: 10.1016/j.ophtha.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alencar L.M., Medeiros F., Weinreb R. Progressive localized retinal nerve fiber layer loss following a retinal cotton wool spot. Semin Ophthalmol. 2007;22(issue 2) doi: 10.1080/08820530701420058. [DOI] [PubMed] [Google Scholar]
- 7.Chihara E., Yoshihito H. Topographic changes in the optic disc in eyes with cotton-wool spots and primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 1991;229(1):13–18. doi: 10.1007/BF00172255. [DOI] [PubMed] [Google Scholar]
- 8.Minckler D.S. Appendix page 452, TR. Am. Ophth. Soc. 1986;LXXXIV page 452. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.