Abstract
Purpose
To present a modified technique for secure tightening and fixing of multilayer amniotic membranes in deep or perforating corneal ulcers.
Observations
The modified procedure for application and fixation of multilayer amniotic membranes is retrospectively described step by step, and the results of three patients treated with this technique were retrospectively analysed and presented.
The modification consists basically in fixing the inlays with one mini-overlay that is sutured intracorneally with resorbable and running Vicryl 10.0, before a corneoscleral overlay is fixed on top conjunctivally with a running nylon 10.0 suture. The resorbable Vicryl suture is left in place permanently.
Conclusions and Importance
The method described avoids any risk of destroying or displacing the inlays by removing sutures later. In each of the three patients demonstrated as case reports the cornea remained stable throughout the 3- to 5-month follow-up period. This modified technique represents a very useful auxiliary means of treating deep or perforating non-infectious corneal ulcers.
Keywords: Amniotic membrane transplantation, Corneal ulcer, Corneal perforation, Multilayer, Keratoplasty
1. Introduction
Various methods have been described for multilayer amniotic membrane (AM) transplantation to treat neurotrophic corneal ulcers or perforations1., 2., 3., 4., 5., 6., 7., 8., 9.: with or without glue, and with running or interrupted sutures.10., 11., 12. Apart from Hick et al.4 and Rodriguez-Ares and co-workers,5 who used running sutures, to our knowledge clinicians have generally preferred interrupted sutures, and all authors have used non-resorbable suture materials to fixate the inlays with a superficial AM layer to the cornea. However, subsequent removal of non-resorbable sutures particularly if interrupted sutures have been used, may destroy the new corneal epithelium and displace correctly positioned AM (Fig. 1),. Moreover, if interrupted sutures have been used, specifically in corneal perforation, fluids may pass through the AM even if the sutures are tightly fixed. This may separate the layers and prevent closure and proper wound healing. Furthermore, interrupted sutures may induce discomfort when an additionally used contact lens is lost.
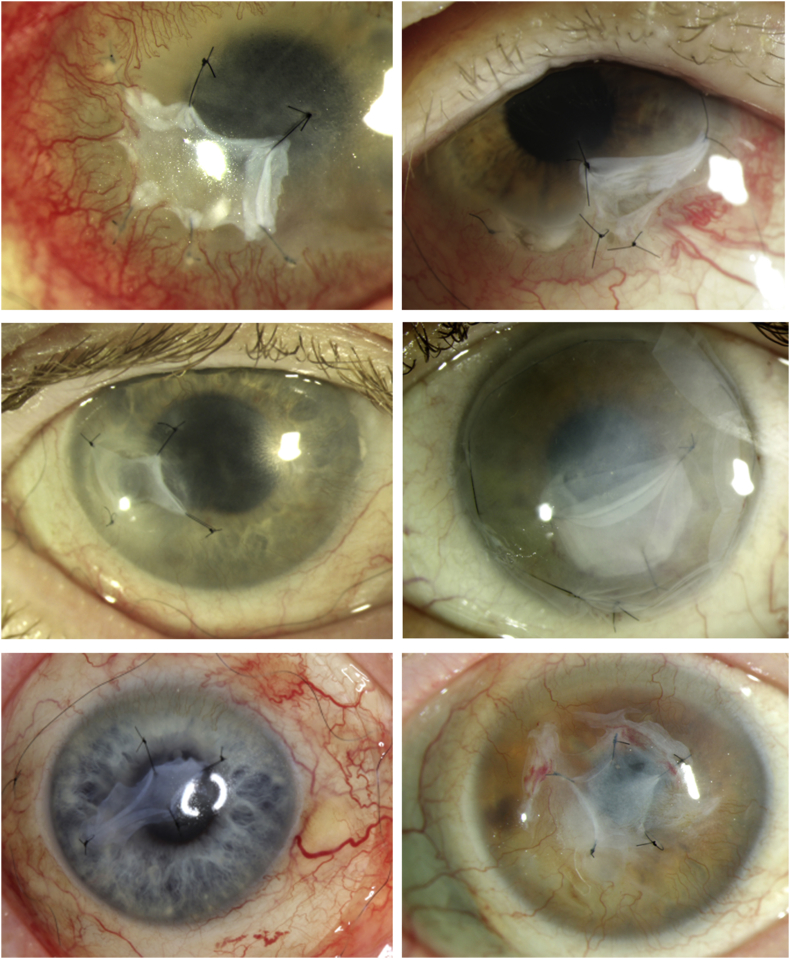
Fig. 1.
Slit lamp photography following single suture multilayer amniotic membrane transplantations in six of our patients who suffered from sterile corneal ulcers, demonstrating unwanted retractions of the superficial multilayers. Microsurgical procedures were comparable to the above mentioned modification technique, except that the most superficial corneal layers were single sutured with nonresorbable Nylon 10.0.
To counter these problems, we modified our transplantation method by using resorbable and running sutures to fixate the inlays with the most superficial corneal membrane layer.
2. Material and methods
The modified procedure for application and fixation of multilayer amniotic membranes is described step by step, and the results of three patients treated with this technique are retrospectively analysed with slit lamp photography and ocular coherence tomography and presented. Informed written consent for the research was obtained from all three patients. Ethics approval was not necessary.
3. Results
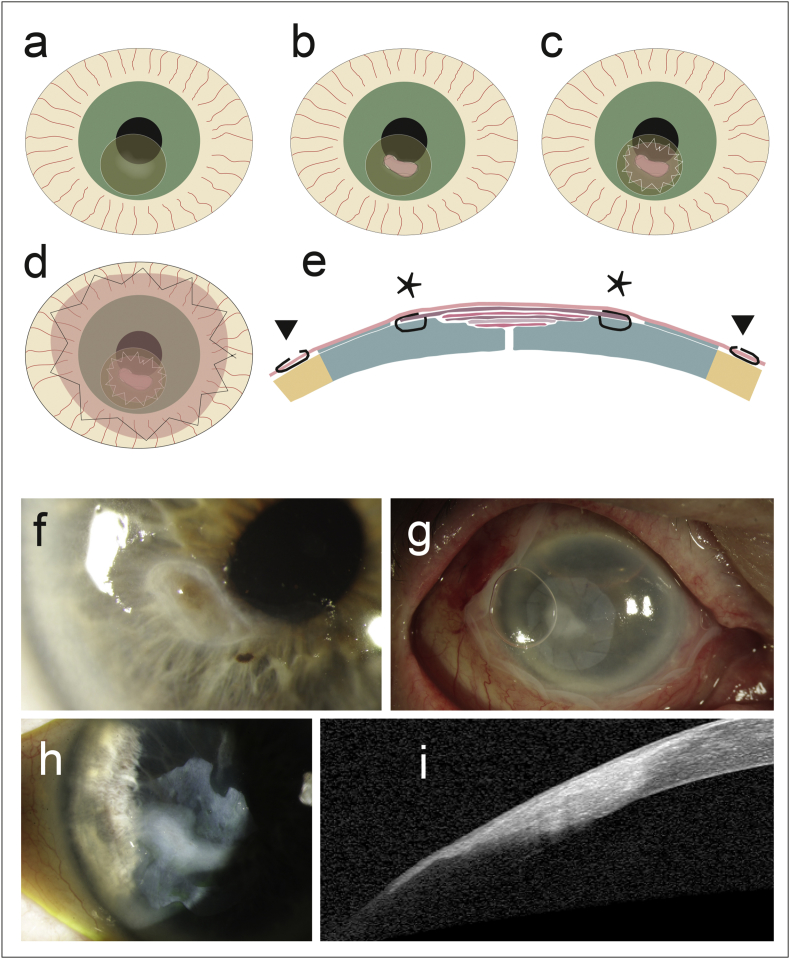
3.1. Case 1
A 91-year-old man presented with a sterile perforating corneal ulcer (diameter 4 mm) in his right eye (RE) (Fig. 2f). With the patient under general anaesthesia, the epithelium was scraped (Fig. 2a) and two inlays (diameter 3mm and 4mm), acquired and processed as previously described,6 were placed into the corneal ulcer (Fig. 2b) and then covered by a superficial AM (diameter 6mm) that was fixed to the cornea with one running, resorbable suture (Vicryl0.0; Ethicon, Norderstedt, Germany) (Fig. 2c). From that time onward, the anterior chamber remained stable. Additionally, an AM (21 mm in diameter) was positioned as a corneoscleral overlay over the complete cornea and conjunctivally fixated with non-resorbable running nylon 10.0 (Alcon, Freiburg im Breisgau, Germany) (Fig. 2d and e) to support proliferation of the corneal epithelium.1,3,10 Finally, a contact lens (diameter 18 mm; Wuk Vision, Au bei Freiburg, Germany) was applied (Fig. 2g) as described elsewhere2, 6, 7, and ofloxacin eye drops were administered three times a day. Two weeks later, the nylon suture and the most superficial AM were removed but the resorbable subepithelial suture was left in place. Eight weeks later, corneal epithelialisation was complete and stable (Fig. 2h and i).
Fig. 2.
A modification to fix amniotic membrane layers in corneal ulcers and perforations (a–e). The corneal ulcer is cleaned, the surrounding epithelium is scraped (a), inlays are applied (b) and a corneal overlay is placed on top and fixed with a resorbable running suture (Vicryl 10.0) (c). A corneoscleral overlay is added and fixed with running resorbable 10.0 nylon (d). (e) The situation from the side, with asterisks depicting resorbable Vicryl 10.0 fixating the corneal overlay, and arrows representing non-resorbable nylon 10.0 to conjunctivally fixate the corneoscleral overlay. Case 1 (f–i). Photographs of the perforating corneal ulcer before treatment (f) and after microsurgery using the modified technique, with a contact lens in place (g). The situation at 8 weeks as seen on slit lamp photography (h) and on OCT (i).
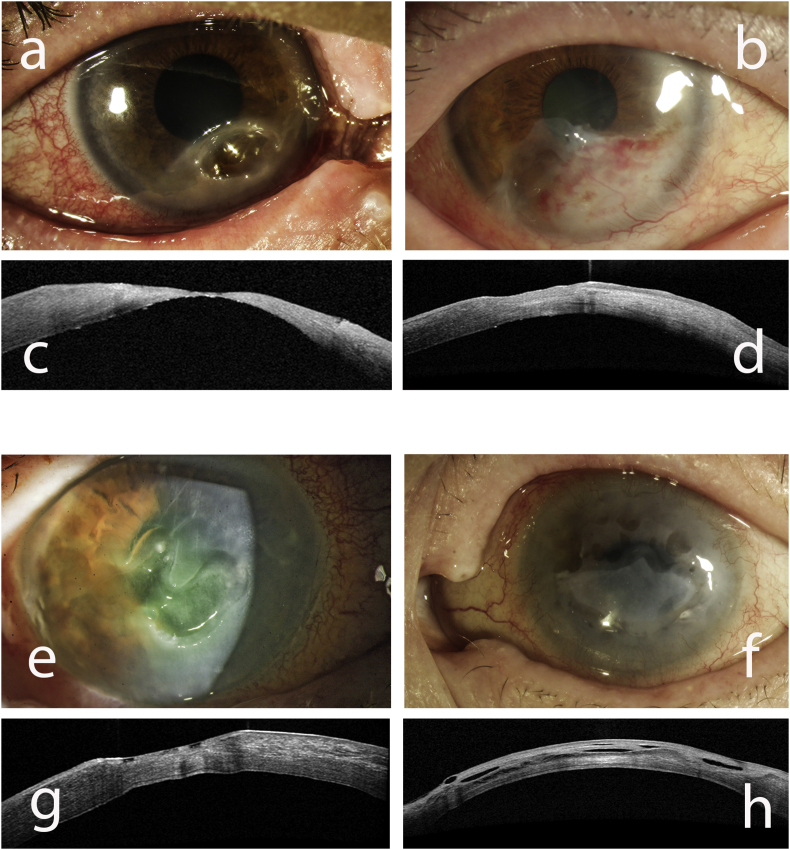
3.2. Case 2
A 64-year-old man presented with a sterile non-perforating marginal corneal ulcer with descemetocele (diameter 1–2 mm) in his RE (Fig. 3a, c). Analogous to the aforementioned method, five inlays, two of them doubled, were used, and one AM (diameter 11 mm) was sutured on top with running Vicryl 10.0, partially to the episclera while the conjunctiva was lifted temporarily for this purpose. An overlay (diameter 21 mm) was conjunctivally fixed with running nylon 10.0, a contact lens applied, and ofloxacin eye drops administered. Four weeks later, the nylon suture and the superficial AM were removed but the resorbable suture was left in place. Epithelialisation was complete. At 6 weeks (Fig. 3b, d) and 3 months, the corneal surface was macroscopically stable.
Fig. 3.
(a–d) Case 2 with a marginal corneal ulcer at the slit lamp (a), and on OCT (c) at baseline, and 6 weeks later (b, d). (e–h) Slit lamp photography and OCT of case 3 at baseline (e, g), and 5 months later (f, h).
3.3. Case 3
An 85-year-old woman presented with a large non-perforating corneal ulcer (diameter 6mm) in her left eye (LE) (Fig. 3e, g). One inlay (diameter 6 mm) was applied, and an AM (diameter 9 mm) sutured on top with running Vicryl 10.0. An overlay (diameter 21 mm) was conjunctivally fixed with running nylon 10.0, a contact lens applied, and ofloxacin eye drops administered. Four weeks later, the nylon suture and the superficial AM were removed but the resorbable suture was left in place. The subepithelial layers soon appeared smoothly attached on optical coherence tomography (OCT), but remained stable. At 5 months, the ocular surface presented a regular epithelium (Fig. 3f, h).
4. Discussion
Due to the fine needle and suture material, the fixation of the corneal overlay initially presents problems for learners, but can be performed in just a few minutes by experienced microsurgeons. The modified method for multilayer AM transplantation stabilized the cornea of all three patients with one microsurgical treatment from the beginning and presented no complications. It enabled an immediate and efficient corneal seal and helped to avoid corneal epithelial disruption and patient discomfort during healing.
Due to adverse effects, e.g. self retracting borders of the amniotic membranes, 52.77% of our patients (n = 36) who had been operated with interrupted sutures necessitated subsequent microsurgical procedures while these were only 28.57% of our patients who underwent the modified procedure (n = 21; results non published yet). Therefore, we hypothesize, that the modified procedure may spare elderly people from unsuccessful or long-drawn-out corneal transplantation procedures. The method does not treat the cause of the ulcer, and artificial tears always remain necessary, but it seems to be a useful option for stabilisation of ocular surfaces with large sterile deep or perforating corneal ulcers. Whether this technique is statistically superior to nonresorbable and interrupted sutures or application methods with fibrin glue should be scientifically investigated with prospective studies in the future.
Patient consent
Written informed consent was obtained from all three patients to publish personal information and case details.
Funding
No funding or grant support.
Conflicts of interest
The authors declare no conflict of interest.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Acknowledgements
We acknowledge support by Open Access Publication Fund of University of Muenster.
Contributor Information
Constantin E. Uhlig, Email: uhligc@uni-muenster.de.
Viktoria C. Müller, Email: Viktoria.Mueller@ukmuenster.de.
References
- 1.Meller D., Tseng S.C. Conjunctival epithelial cell differentiation on amniotic membrane. Invest Ophthalmol Vis Sci. 1999;40:878–886. [PubMed] [Google Scholar]
- 2.Solomon A., Meller D., Prabhasawat P. Amniotic membrane grafts for nontraumatic corneal perforations, descemetoceles, and deep ulcers. Ophthalmology. 2002;109:694–703. doi: 10.1016/s0161-6420(01)01032-6. [DOI] [PubMed] [Google Scholar]
- 3.Meller D., Dabul V., Tseng S.C. Expansion of conjunctival epithelial progenitor cells on amniotic membrane. Exp Eye Res. 2002;74:537–545. doi: 10.1006/exer.2001.1163. [DOI] [PubMed] [Google Scholar]
- 4.Hick S., Demers P.E., Brunette I. Amniotic membrane transplantation and fibrin glue in the management of corneal ulcers and perforations: a review of 33 cases. Cornea. 2005;24:369–377. doi: 10.1097/01.ico.0000151547.08113.d1. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez-Ares M.T., Tourino R., López-Valladares M.J. Multilayer amniotic membrane transplantation in the treatment of corneal perforations. Cornea. 2004;23:577–583. doi: 10.1097/01.ico.0000121709.58571.12. [DOI] [PubMed] [Google Scholar]
- 6.Uhlig C.E., Frings C., Rohloff N. Long-term efficacy of glycerine-processed amniotic membrane transplantation in patients with corneal ulcer. Acta Ophthalmol. 2015;93:e481–e487. doi: 10.1111/aos.12671. [DOI] [PubMed] [Google Scholar]
- 7.Liu J., Sheha H., Fu Y. Update on amniotic membrane transplantation. Expert Rev Ophthalmol. 2010;5:645–661. doi: 10.1586/eop.10.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan E., Shah A.N., O'Brart D.P. “Swiss rollˮ amniotic membrane technique for the management of corneal perforations. Cornea. 2011;30:838–841. doi: 10.1097/ICO.0b013e31820ce80f. [DOI] [PubMed] [Google Scholar]
- 9.Fan J., Wang M., Zhong F. Improvement of amniotic membrane method for the treatment of corneal perforation. BioMed Res Int. 2016;2016 doi: 10.1155/2016/1693815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kruse F.E., Meller D. Amniotic membrane transplantation for reconstruction of the ocular surface. Ophthalmologe. 2001;98:801–810. doi: 10.1007/s003470170055. [DOI] [PubMed] [Google Scholar]
- 11.Uhlig C.E., Busse H., Groppe M. Use of fibrin glue in fixation of amniotic membranes in sterile corneal ulceration. Am J Ophthalmol. 2006;142:189–191. doi: 10.1016/j.ajo.2006.02.043. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann S., Szentmary N., Seitz B. Amniotic membrane transplantation for the treatment of infectious ulcerative keratitis before elective penetrating keratoplasty. Cornea. 2013;32:1321–1325. doi: 10.1097/ICO.0b013e318298de10. [DOI] [PubMed] [Google Scholar]