Abstract
Purpose
To report two cases of retinal vasculitis associated with CREST syndrome, a novel ocular finding.
Observations
We report two cases of patients with CREST syndrome with ocular inflammatory disease. Patient 1 presented with a right unilateral panuveitis with extensive retinal vasculitis and evidence of prior uveitis in the contralateral eye. Patient 2 presented with a left branch retinal artery occlusion and bilateral retinal vasculitis. Both patients underwent treatment with prednisone and mycophenolate motefil.
Conclusions and importance
Retinal vasculitis has not been previously reported in CREST syndrome. Prompt therapy with immunomodulatory therapy can potentially minimize ocular morbidity.
Keywords: CREST syndrome, Retinal vasculitis
1. Introduction
The CREST syndrome (calcinosis, Raynaud's phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) is a form of progressive systemic sclerosis (scleroderma). CREST syndrome is distinct from progressive systemic sclerosis in that it is often associated with anti-centromere antibodies and rarely affects lung parenchyma or causes hypertensive renal crisis.1 Ocular manifestations of scleroderma most commonly involve the anterior segment and include eyelid abnormalities and keratoconjunctivitis sicca. Hypertensive retinopathy secondary to underlying hypertension has also been observed in more advanced cases of scleroderma. Other types of ocular involvement are rarer and include retinal involvement such as vascular tortuosity, non-specific retinal pigment epithelial atrophy and vascular occlusions, and parafoveal retinal telangiectasia.2 To our knowledge, retinal vasculitis has not been previously reported in patients with either systemic sclerosis or CREST syndrome. Here, we present two patients with the CREST variant of progressive systemic sclerosis who developed retinal vasculitis. Systemic physical examination and laboratory evaluations failed to suggest evidence for alternative systemic diagnoses as a possible cause of their retinal vasculitis.
2. Case reports
2.1. Case 1
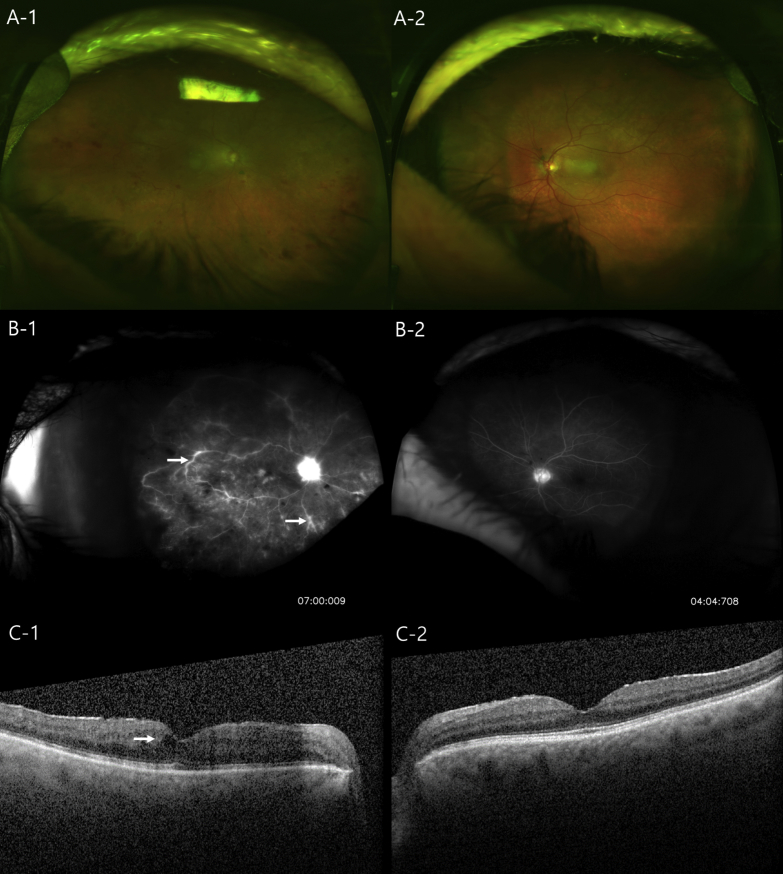
A 77-year-old woman with a past medical history of CREST syndrome, which was diagnosed 15 years ago and primary open angle glaucoma and a remote history of anterior uveitis after cataract extraction presented with progressive haziness in her right vision. Review of systems at that time was notable for recent weight loss (10–15 pounds), ongoing Raynaud's phenomenon and cough for several months. She had known history of esophageal dysmotility. She underwent left index finger amputation secondary to severe Raynaud's phenomenon and ischemia 10 years prior to presentation. The patient reported long standing systemic therapy with nifedipine. Topical therapy with 0.05% of difluprednate and 0.09% bromfenac was started the day prior to our initial examination. At initial examination, her visual acuity was 20/125 OD and 20/50 OS with a right afferent pupillary defect. Anterior segment examination was notable for lid margin telangiectasia in both eyes. The right eye demonstrated diffuse fine keratic precipitates, trace anterior chamber cell, 1 + vitreous haze, a blunted foveal light reflex, peripheral vascular sheathing with abnormal vessel anastomoses and intraretinal hemorrhages with retinal pigment epithelial mottling throughout the fundus. The left eye demonstrated pigmented keratic precipitates without anterior chamber cell and peripheral retinal pigment epithelial mottling (Fig. 1, A-1, A-2). Fluorescein angiogram showed extensive retinal vasculitis with capillary nonperfusion and optic disc leakage in the right eye, and mild optic nerve staining in the left eye (Fig. 1, B-1, B-2). Optical coherence tomography (OCT) showed macular edema in her right (Fig. 1, C-1) and vitreous opacities in both eyes (Fig. 1, C-1, C-2). Laboratory findings were notable for positive antinuclear antibody (>1: 2560 titer) with centromere pattern and anti-centromere antibody. Rapid plasma reagin, fluorescent treponemal antibody, quantiferon gold, rheumatoid factor, anti-neutrophil cytoplasmic antibody, and angiotensin converting enzyme tests were all unrevealing. Chest CT demonstrated moderate emphysematous changes, no hilar adenopathy, and mild diffuse dilation of the esophagus. The patient was started on 1 mg/kg oral prednisone with improvement of her ocular inflammation, although with limited visual recovery. She underwent repeat evaluation with rheumatology with agreement on a diagnosis of limited scleroderma/CREST syndrome. The patient was started on mycophenolate motefil; however, she passed away subsequent to complications from a colonic obstruction prior to an adequate therapeutic trial on immunosuppression.
Fig. 1.
Wide field color fundus photos and fluorescein angiogram of case 1.
Color fundus photos showed peripheral intraretinal hemorrhages throughout the retina with retinal pigment epithelial mottling in the right eye (A-1) and mild retinal pigment mottling in the left eye (A-2). Late phase fluorescein angiogram showed extensive retinal vasculitis with capillary nonperfusion, vascular tortuosity, severe optic nerve staining in the right eye (White arrows, B-1)., there was mild optic nerve staining in the left eye (B-2). OCT revealed mild macular edema in the right eye (C-1) and vitreous opacities in both eyes (C-1, C-2).
2.2. Case 2
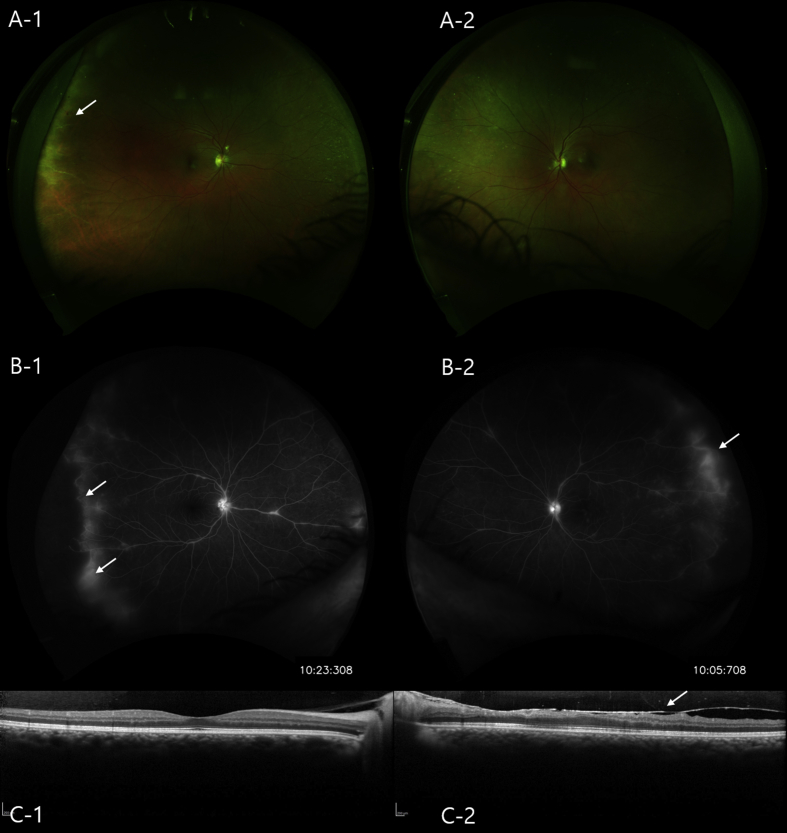
A 51-year-old woman was evaluated for cloudy vision in her left eye secondary to a possible branch retinal arterial occlusion (BRAO) and retinal vasculitis in her left eye. She had short course of prednisone using a tapering schedule from 60 mg to 10 mg/day. Past medical history was significant for Raynaud's involving the digits for 8 years, telangiectasia at the cuticle of her left index finger. Her vision was 20/20 in the right eye and 20/40 in the left eye. Intraocular pressure was 19 mmHg in the right eye and 18 mmHg in the left eye at initial presentation. Slit lamp exam showed no active inflammation in the anterior chamber or anterior vitreous in either eye. Fundus examination revealed perivascular sheathing and multiple yellow punctate lesions in both eyes (Fig. 2, A-1, A-2). FA showed periphlebitis and diffuse vascular leakage in both eyes. The left eye was notable for delayed transit time in a few vessels (Fig. 2, B-1, B-2). But BRAO lesion was not definite on FA. OCT image revealed mild vitreous opacity in both eyes and epiretinal membrane in her left eye (Fig. 2, C-1, C-2). Laboratory finding was remarkable with positive ANA with centromere type with titer >1:2560. Rheumatoid factor was weakly positive also. The patient was started on mycophenolate motefil 1000mg twice a day and her symptoms and retinal vascular findings have improved after about two months.
Fig. 2.
Wide field color fundus photos and fluorescein angiogram of case 2.
Color fundus photos showed peripheral vascular sheathing in both eyes (A-1, A-2). Late phase fluorescein angiogram showed peripheral retinal vascular leakage from retinal vasculitis with capillary nonperfusion, which was significant at temporal area. Mild vascular tortuosity was also shown in both eyes with optic disc staining (B-1, B-2). There was no definite feature of BRAO. OCT examination showed vitreous opacities in both eyes (C-1, C-2) and epiretinal membrane in the left eye (C-2).
3. Discussion
To our knowledge, we report the first cases of retinal vasculitis associated with CREST syndrome. Prior reports of ocular findings in systemic sclerosis (scleroderma) found eyelid involvement (stiffness and telangiectasia) and keratoconjunctivitis sicca as the most common ocular manifestations.3,4 Retinal microvascular abnormalities including arteriosclerotic changes and tortuosity have also been reported, but were not distinguishable from those related to systemic hypertension.
Ocular manifestations associated with CREST syndrome are rarely reported. Two reports found juxtafoveal telangiectasis.5,6 Three case reports identified granulomatous uveitis in CREST patients. Of these, two cases were controlled with topical steroid and mydriatics.7,8 One case was also associated with primary biliary cirrhosis and required topical steroid, mydriatics and systemic corticosteroids.9
Siliva et al. reported vascular endothelial dysfunction, microvascular damage and ischemic peripheral vasculopathy in scleroderma.10 Thus it seems that abnormal retinal vasculature could be a manifestation of CREST syndrome.
In both of our cases, systemic therapy with immunomodulatory therapy was indicated. Unfortunately, one patient died from systemic disease complications prior to being able to assess the efficacy of mycophenolate motefil. The other patient demonstrated improvement in her examination and clinical symptoms following mycophenolate motefil treatment. As retinal vasculitis is a previously unreported manifestation of CREST syndrome, it remains to be seen if all cases require long-term immunosuppressive therapy; however, given the potential for vision loss, consideration for treatment should be made.
4. Conclusion
Retinal vasculitis is a possible ocular manifestation of CREST syndrome. Treatment with systemic corticosteroids and potentially immunosuppressive therapy may be required to control inflammation and limit ocular morbidity.
Patient consent
The Oregon Health & Science University Institutional Review Board deemed protocol approval not necessary for such a case series.
Funding
This work was supported in part in NIH Grant RO1 EY026572 to Dr. Rosenbaum. We have also received financial support from Research to Prevent Blindness, the William and Mary Bauman Foundation, and the Stan and Madelle Rosenfeld Family Trust.
Conflicts of interest
The authors have no financial disclosures relating this topic.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ajoc.2018.02.022.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Miyawaki S., Asanuma H., Nishiyama S., Yoshinaga Y. Clinical and serological heterogeneity in patients with anticentromere antibodies. J Rheumatol. 2005;32:1488–1494. [PubMed] [Google Scholar]
- 2.Gomes Bde A., Santhiago M.R., Magalhaes P., Kara-Junior N., Azevedo M.N., Moraes H.V., Jr. Ocular findings in patients with systemic sclerosis. Clinics (Sao Paulo) 2011;66:379–385. doi: 10.1590/S1807-59322011000300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tailor R., Gupta A., Herrick A., Kwartz J. Ocular manifestations of scleroderma. Surv Ophthalmol. 2009;54:292–304. doi: 10.1016/j.survophthal.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 4.West R.H., Barnett A.J. Ocular involvement in scleroderma. Br J Ophthalmol. 1979;63:845–847. doi: 10.1136/bjo.63.12.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huerva V., Sanchez M.C. Juxtafoveolar telangiectasis associated with CREST syndrome. Ocul Immunol Inflamm. 2008;16:195–197. doi: 10.1080/09273940802217867. [DOI] [PubMed] [Google Scholar]
- 6.Proctor B., Chang T., Hay D. Parafoveal telangiectasia in association with CREST syndrome. Arch Ophthalmol. 1998;116:814–815. [PubMed] [Google Scholar]
- 7.Akman A., Akova Y.A., Yucel E., Aydin P. Granulomatous anterior uveitis in a patient with CREST syndrome. Ocul Immunol Inflamm. 2000;8:201–203. [PubMed] [Google Scholar]
- 8.Courtade M., Gicquel J.J., Mercie M., Vabres B., Dighiero P. Granulomatous uveitis and CREST syndrome: a case study. J Fr Ophtalmol. 2004;27:918–920. doi: 10.1016/s0181-5512(04)96237-7. [DOI] [PubMed] [Google Scholar]
- 9.Santos P.S., Oliveira L., Moraes M.F. Granulomatous uveitis, CREST syndrome, and primary biliary cirrhosis. Br J Ophthalmol. 2000;84:548–549. doi: 10.1136/bjo.84.5.546c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silva I., Teixeira A., Oliveira J., Ameida R., Vasconcelos C. Endothelial dysfunction, microvascular damage and ischemic peripheral vasculopathy in systemic sclerosis. Clin Hemorheol Microcirc. 2017;66:117–130. doi: 10.3233/CH-150044. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.