Abstract
Purpose
We report a case of pigment dispersion glaucoma secondary to uncomplicated phakic intraocular collamer lens (ICL) (Visian ICL™, Staar Inc., Monrovia, CA) implant that resulted in advanced visual field loss.
Observations
A 50-year-old man presented for routine follow-up status post bilateral phakic intraocular collamer lens (ICL) placement 8 years earlier. He was incidentally found to have a decline in visual acuity from an anterior subcapsular cataract and elevated intraocular pressure (IOP) in the left eye. There were signs of pigment dispersion and no evidence of angle closure. Diffuse optic nerve thinning was consistent with advanced glaucomatous visual field defects. Pigment dispersion was also present in the patient's right eye, but without elevated IOP or visual field defects. The patient was treated with topical glaucoma medications and the phakic ICL in the left eye was removed concurrently with cataract surgery to prevent further visual field loss.
Conclusions and importance
Pigment dispersion glaucoma is a serious adverse outcome after phakic ICL implantation and regular post-operative monitoring may prevent advanced visual field loss.
Keywords: Phakic intraocular lens, Intraocular collamer lens, Pigment dispersion, Glaucoma
1. Introduction
Myopia affects over 40% of adults in the US.1 Refractive surgery using a phakic posterior chamber intraocular collamer lens (ICL) (Visian ICL™, Staar Inc., Monrovia, CA) is FDA-approved for the correction of myopia.2 Patient selection criteria include the absence of ocular comorbidities at the time of implantation and adequate anterior chamber depth. Since implantation is contraindicated in patients over the age of 45 years, complications have been primarily reported in younger patients. These include chronic uveitis, cataract formation, corneal endothelial cell loss, angle closure glaucoma, and pigment dispersion syndrome.3 However, the manufacturer has not reported glaucoma secondary to pigment dispersion as a serious adverse outcome. Prior cases of pigment dispersion syndrome from this phakic ICL have been previously reported, with no resultant visual field loss or optic nerve damage.2,4,5 We report a new case of pigment dispersion glaucoma following phakic ICL implantation that resulted in advanced visual field loss.
1.1. Case report
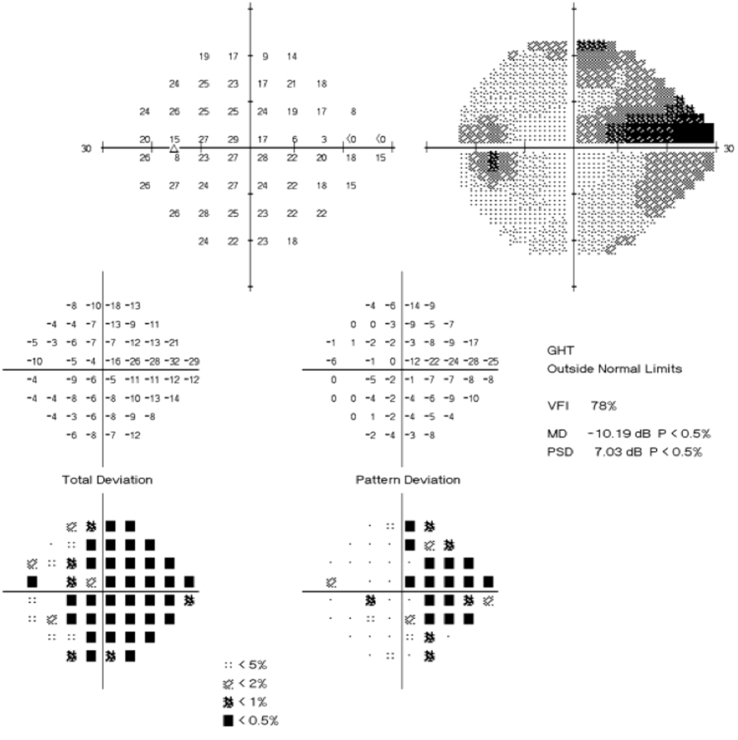
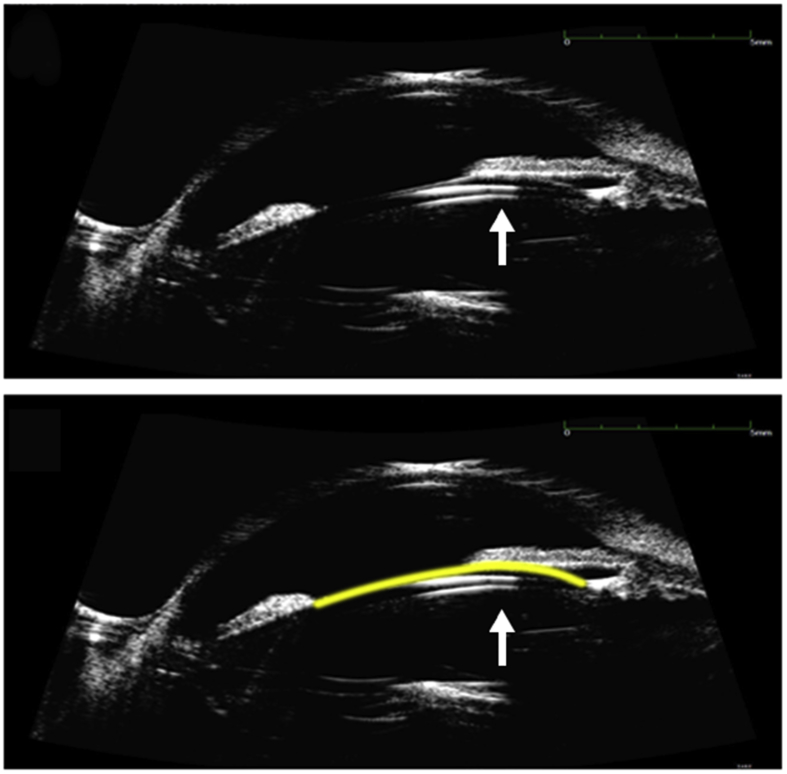
A 50-year-old man was evaluated by his ophthalmologist at a routine follow-up visit after uncomplicated bilateral phakic ICL placement (Visian ICL™ model ICMV4, Staar Inc., Monrovia, CA) 8 years earlier. His pre-operative evaluation included a comprehensive slit-lamp examination and indirect ophthalmoscopy. The patient had a stable refractive history and open angles on gonioscopy. The anterior chamber depth was >3.0 mm and the endothelial cell count was adequate (>2000 cell/mm2) with normal morphology. The patient's post-operative examinations had been unremarkable. He had no prior history of glaucoma, pigment dispersion or eye injury. On exam, he was found to have a decline in best-corrected visual acuity from 20/20 to 20/40, an intraocular pressure (IOP) of 41 mmHg, and an anterior subcapsular cataract in his left eye. Slit-lamp examination revealed a well-centered phakic ICL with no evidence of angle closure and 2 patent peripheral iridotomies. Gonioscopy showed a targetoid pattern of pigment deposition on the surface of the phakic ICL, pigmentation on the corneal endothelium (i.e. Krukenberg spindle), and 4 + heavy pigmentation of the trabecular meshwork. Furthermore, the iris showed diffuse 360-degree transilllumination defects. There was diffuse optic nerve thinning consistent with reproducible advanced glaucomatous visual field defects (Fig. 1). The patient's right eye also had similar evidence of pigment dispersion, but no IOP elevation, visual field defects or glaucomatous optic nerve damage. Ultrasound biomicroscopy (UBM) showed direct contact of the phakic ICL against the posterior iris (Fig. 2) in both eyes. He was started on topical glaucoma medications, which lowered the IOP in the left eye to the mid-to high-teens. Given the presence of a visually-significant cataract and his elevated IOP, the phakic ICL in the left eye was removed concurrently with cataract surgery to prevent further visual field loss. The patient's IOP remained controlled on topical glaucoma medications post-operatively and his best-corrected visual acuity improved to 20/20 in this eye. However, he continued to note subjectively diminished vision and advanced visual field defects that persisted after cataract surgery.
Fig. 1.
Reproducible advanced visual field defects. Humphrey visual field testing (24-2 SITA-standard) in the left eye showed reproducible visual field defects encroaching on central vision that persisted after cataract surgery.
Fig. 2.
Direct contact between the phakic intraocular collamer lens (ICL) and iris. A) Ultrasound biomicroscopy demonstrating direct contact (arrow) between the phakic ICL and the posterior iris in the left eye with anterior displacement of the iris. B) The position of the phakic ICL is highlighted in yellow. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
2. Discussion
We have presented a case of pigment dispersion glaucoma with advanced visual field defects following phakic ICL implantation. In our patient, no evidence of pigment dispersion or glaucoma was present prior to phakic ICL implantation. Although secondary pigment dispersion glaucoma has been described with other models of phakic intraocular, sulcus-placed, and piggyback pseudophakic intraocular lenses,6,7 the manufacturer of this phakic ICL has not reported pigment dispersion glaucoma as a serious adverse event. A few studies have reported elevated intraocular pressures—some even requiring trabeculectomy—but have not documented any visual field loss or optic nerve damage.2,4 Brandt et al. described medically-controlled pigment dispersion syndrome with no resultant vision loss in a patient following implantation of the Visian ICL™ model ICMV3 (Staar, Inc., Monrovia, CA),5 which was the predecessor to the model ICMV4 implanted in our patient.
Compared to the earlier model, the ICMV4 has a greater vault height requirement. Schmidinger et al. found that central vaulting of the ICMV4 consistently declined over a period of 10 years.8 A reduction in adequate vault height over time has been linked to the development of anterior subcapsular cataracts,8,9 which may have contributed to the cataract found in our patient. Additionally, as the crystalline lens thickens with cataract formation, the posterior chamber becomes increasingly crowded,10 further reducing the space available to accommodate the phakic ICL. Inadequate space in the posterior chamber may precipitate pigment dispersion and chronic uveitis due to iris chaffing from direct implant-iris contact.3 Ultrasound biomicroscopy imaging can be helpful in assessing post-operative phakic ICL position and the assessment of anatomical changes over time.11
Given the risk of permanent visual field loss, patients and providers should be aware that pigment dispersion glaucoma is a serious, vision-threatening post-operative complication that may occur several years following phakic ICL implantation due to dynamic changes in the posterior chamber over time. Thus, IOP should be closely monitored and careful slit-lamp examination should be performed to assess for signs of pigment dispersion, including increased pigmentation of the trabecular meshwork on gonioscopy. UBM can aid in evaluation of changes in phakic ICL positioning over time. Medical and surgical glaucoma intervention may be increasingly common to prevent vision loss as patients with phakic ICLs experience changes in their posterior chamber anatomy with age. Therefore, patients with phakic ICL implants should have vigilant long-term monitoring for glaucoma.
Patient consent
Informed consent was obtained orally from the patient for publication of this case report and accompanying images.
Funding
This study was supported, in part, by an institutional grant from Research to Prevent Blindness, to the University of Wisconsin Dept. of Ophthalmology and Visual Sciences.
Conflicts of interest
None of the authors of this paper has a financial or personal relationship with other people or organizations that could inappropriately influence or bias the content of the paper.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Acknowledgements
None.
References
- 1.Vitale S., Sperduto R.D., Ferris F.L. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009;127(12):1632–1639. doi: 10.1001/archophthalmol.2009.303. [DOI] [PubMed] [Google Scholar]
- 2.Huang D., Schallhorn S.C., Sugar A. Phakic intraocular lens implantation for the correction of myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2009;116(11):2244–2258. doi: 10.1016/j.ophtha.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 3.Pérez-Cambrodí R.J., Piñero D.P., Ferrer-Blasco T., Cerviño A., Brautaset R. The posterior chamber phakic refractive lens (PRL): a review. Eye. 2013;27(1):14–21. doi: 10.1038/eye.2012.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sánchez-Galeana C.A., Zadok D., Montes M., Cortés M.A., Chayet A.S. Refractory intraocular pressure increase after phakic posterior chamber intraocular lens implantation. Am J Ophthalmol. 2002;134(1):121–123. doi: 10.1016/s0002-9394(02)01414-9. [DOI] [PubMed] [Google Scholar]
- 5.Brandt J.D., Mockovak M.E., Chayet A. Pigmentary dispersion syndrome induced by a posterior chamber phakic refractive lens. Am J Ophthalmol. 2001;131(2):260–263. doi: 10.1016/s0002-9394(00)00606-1. [DOI] [PubMed] [Google Scholar]
- 6.Chang S.H., Lim G. Secondary pigmentary glaucoma associated with piggyback intraocular lens implantation. J Cataract Refract Surg. 2004;30(10):2219–2222. doi: 10.1016/j.jcrs.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 7.Micheli T., Cheung L.M., Sharma S. Acute haptic-induced pigmentary glaucoma with an AcrySof intraocular lens. J Cataract Refract Surg. 2002;28(10):1869–1872. doi: 10.1016/s0886-3350(02)01644-9. [DOI] [PubMed] [Google Scholar]
- 8.Schmidinger G., Lackner B., Pieh S., Skorpik C. Long-term changes in posterior chamber phakic intraocular collamer lens vaulting in myopic patients. Ophthalmology. 2010;117(8):1506–1511. doi: 10.1016/j.ophtha.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 9.Gonvers M., Bornet C., Othenin-Girard P. Implantable contact lens for moderate to high myopia: relationship of vaulting to cataract formation. J Cataract Refract Surg. 2003;29(5):918–924. doi: 10.1016/s0886-3350(03)00065-8. [DOI] [PubMed] [Google Scholar]
- 10.McCaughey M.V., Mifflin T., Fenzl C.R., Goldsmith J., Moshirfar M. Pseudophacomorphic glaucoma along with pupillary block after Visian™ implantable collamer lens implantation for high myopia. Open J Ophthalmol. 2014;4(4):107–111. doi: 10.4236/ojoph.2014.44017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elshafei A.M., Genaidy M.M., Moharram H.M. Vivo positional analysis of implantable collamer lens using Ultrasound biomicroscopy. J Ophthalmol. 2016;2016:4060467. doi: 10.1155/2016/4060467. [DOI] [PMC free article] [PubMed] [Google Scholar]