Abstract
Eccrine angiomatous hamartoma (EAH) is a rare benign malformation characterized by eccrine and vascular components. It usually presents at birth or during early infancy or childhood on lower extremities as a nodule or plaque. We report a case of asymptomatic tumoral swelling over the left leg in a 5-month-old Indian infant since birth. This was diagnosed as EAH on histopathology and confirmed on immunohistochemistry.
Keywords: Dermatopathology, pediatric dermatology, vascular malformation
Introduction
Eccrine angiomatous hamartoma (EAH) was first described by Lotzbeck (1859), although the term was coined by Hyman et al. (1968). It is a benign, uncommon, nevoid proliferation of vascular, eccrine, and occasionally fatty tissues and pilar structures. EAH mostly presents in children and young adults, although congenital and elderly cases have been reported.[1] It lacks sex predilection and is characterized by single or multiple red, violaceous, blue, yellow, brown or skin-colored plaques or nodules, and rarely macules with acral predominance that enlarge commensurate with patient's growth or rapidly proliferate during puberty or pregnancy due to hormonal factors.[2] Late-onset lesions are related to recurrent trauma.[3]
Case Report
A 5-month-old otherwise healthy girl presented with asymptomatic red swelling over the left knee since birth. It gradually progressed in size, became more raised, and darkened over time. It was not associated with pain, itching, or increased sweating. Cutaneous examination showed solitary erythematous, irregular, soft, nontender, nodulo-plaque measuring 10 × 8 cm present on the left knee. The surface was studded with multiple erythematous papules [Figure 1]. Local rise of temperature over the plaque was noted. Hypertrichosis was absent. There was no underlying bony abnormality, and the range of motion of both knee joints was normal. Systemic examination was insignificant. Clinically, a differential diagnosis of congenital hemangioma, arteriovenous malformation, and EAH was kept. Ultrasound Doppler revealed hypoechoic spaces in the subcutaneous plane. Histopathological examination showed unremarkable epidermis and proliferation of appendages mainly comprising eccrine glands along with capillary proliferation in the mid and deep dermis with smooth muscle proliferation and thick-walled blood vessels, which was consistent with the diagnosis of EAH [Figure 2a and b]. Immunohistochemistry revealed EMA positivity in eccrine glands and nuclear positivity for S100 [Figure 3].
Figure 1.

Solitary erythematous, irregular, nodulo-plaque with multiple erythematous papules measuring 10 × 8 cm on the left knee
Figure 2.
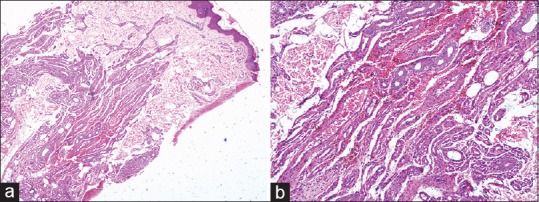
(a) H and E stain showing proliferation of appendages mainly comprising eccrine glands and capillaries in the mid and deep dermis (×100). (b) H and E stain showing proliferation of eccrine glands, capillaries, and smooth muscles in the dermis (×400)
Figure 3.
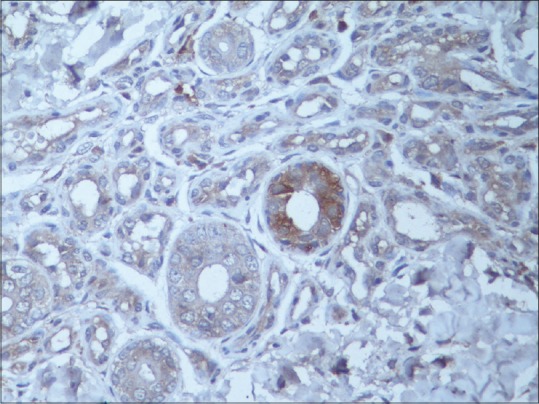
Special stains showing EMA positivity of eccrine glands (×400)
Discussion
EAH is a rare, benign malformation of hyperplastic eccrine and vascular structures. We report this case for its rarity. Approximately 70 cases of EAH have been reported worldwide.[4] It is mostly seen in children and presents as well-defined red, violaceous, blue, yellow, brown or skin-colored plaques or nodules, which may be solitary or grouped usually located over extremities. It is generally asymptomatic but may be associated with pain or hyperhidrosis (in one-third of the cases) due to small infiltrating nerves or eccrine glands, respectively. On histopathology, usually eccrine glands and capillaries are seen in the dermis, but sometimes other structures such as mucin secreting cells, adipose tissue, apocrine glands, hair follicles, or bony structures may be seen. Immunohistochemistry reveals specific positive staining for vascular elements and eccrine glands.[5]
Hamartoma develops due to abnormality of heterotypic dependency in early childhood. Impairment of biochemical interactions between differentiating epithelium and underlying mesenchyme leads to abnormal proliferation of adenexal and vascular structures in congenital causes.[3]
Our case showed typical clinical features of classical EAH in the form of a well-defined erythematous plaque over the acral location, as seen in a majority of the cases. Ultrasound Doppler revealed its location in the subcutaneous plane, and histopathology showed proliferation of eccrine glands and capillaries consistent with the diagnosis of EAH. Our patient interestingly showed marked increase in local temperature, as reported by Larralde et al. in tumoral EAH.[3] However, it was not associated with other commonly reported associations such as hypertrichosis, hyperhidrosis, or pain. It is believed that infiltration of small nerves, hormonal influences, and fluid retention during menstruation or pregnancy has been speculated to be the cause of pain, which lacked in our patient.
EAH can mimic vascular malformations, tufted angioma, smooth muscle hamartoma, glomus tumor, blue rubber bled nevus, and macular telangiectatic mastocytosis, and differentiation and confirmation can be done on the basis of histopathology findings and positive immunohistochemistry.[5]
EAH commonly do not require treatment due to their benign nature and malignant transformation has not been reported yet. Surgical excision or medical intervention (intralesional sclerosants/botulinum toxin or lasers) is indicated for aesthetic reasons, progressive enlargement, or undesirable symptoms such as pain or hyperhidrosis.[6] No treatment was administered to our patient due to its asymptomatic and benign nature.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initial will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cebreiro C, Sanchez-Aguilar D, Gomez Centeno P, Fernandez-Redondo V, Toribio J. Eccrine angiomatous hamartoma: report of seven cases. Clin Exp Dermatol. 1998;23:267–70. doi: 10.1046/j.1365-2230.1998.00391.x. [DOI] [PubMed] [Google Scholar]
- 2.Kwon OC, Oh ST, Kim SW, Park GS, Cho BK. Eccrine angiomatous hamartoma. Int J Dermatol. 1998;37:787–9. doi: 10.1046/j.1365-4362.1998.00506.x. [DOI] [PubMed] [Google Scholar]
- 3.Lin YT, Chen CM, Yang CH, Chuang YH. Eccrine angiomatous hamartoma: A retrospective study of 15 cases. Chang Gung Med J. 2012;35:167–77. doi: 10.4103/2319-4170.106154. [DOI] [PubMed] [Google Scholar]
- 4.Chien AJ, Asgari M, Argenyi ZB. Eccrine angiomatous hamartoma with elements of an arterio-venous malformation: A newly recognized variant. J Cutan Pathol. 2006;33:433–6. doi: 10.1111/j.0303-6987.2006.00272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pelle MT, Pride HB, Tyler WB. Eccrine angiomatous hamartoma. J Am Acad Dermatol. 2002;47:429–35. doi: 10.1067/mjd.2002.121030. [DOI] [PubMed] [Google Scholar]
- 6.Kaliyadan F, Sundeep V, Hiran KR. Late onset eccrine angiomatous hamartoma treated with intralesional sclerosant: A case report. Ind J Dermatol. 2007;52:99–101. [Google Scholar]


