Abstract
AIM
To determine the effects of Rutin on methanol induced optic neuropathy and compare the results with the effects of ethanol.
METHODS
Totally 30 rats were divided into 5 groups, with 6 rats in each group as follows: healthy controls (C), methotrexate (MTX), methotrexate+methanol (MTM), methotrexate+methanol+ethanol (MTME) and methotrexate+ methanol+Rutin (MTMR). In all rabbits except those of the control group, MTX, diluted in sterile serum physiologic, 0.3 mg/kg per oral was applied for 7d by the aid of a tube. After this procedure to the rats of MTM, MTME and MTMR groups, 20% methanol with a dose of 3 g/kg per oral was given by the aid of a tube. In MTME group, 4h after the application of methanol, 20% ethanol was applied by the same way with a dose of 0.5 g/kg. On the other hand, in MTMR group 4h after the application of methanol, Rutin, which was dissolved in distilled water, was applied by the same way with a dose of 50 mg/kg.
RESULTS
There were statistically significant differences in tissue 8-hydroxy-2 deoxyguanine (8-OHdG), interleukin-1β (IL-1β), tumor necrosis factor-alpha (TNF-α), malondialdehyde (MDA), myeloperoxidase (MPO). glutathione peroxidase (tGSH) and superoxide dismutase (SOD) levels between groups (P<0.001). In MTMR group tissue 8-OHdG, IL-1β, MDA, and MPO levels were similar with the healthy controls but significantly different than the other groups. In histopathological evaluations, in MTX group there was moderate focal destruction, hemorrhage and decrease in number of astrocytes and oligodendrocytes; in MTM group there was severe destruction and edema with decrease in number of astrocytes and oligodendrocytes; in MTME group there was mild hemorrhage, mild edema, mildly dilated blood vessels with congestion while in MTMR group, optic nerve tissue was resembling the healthy controls.
CONCLUSION
Rutin may prevent methanol-induced optic neuropathy via anti-inflammatory effects and decreasing the oxidative stress. New treatment options are warranted in this disease to avoid loss of vision in patients.
Keywords: methanol, optic neuropathy, rutin, astrocyte, rat
INTRODUCTION
Methanol is a colorless alcohol that is commonly used as a component of some industrial products such as antifreeze, perfume and cologne[1]. Methanol intoxication, which may be accidental or intentional as a suicide attempt, is known to cause visual disturbances, central nervous system abnormalities such as confusion, coma or even death[2]. Visual loss associated with methanol toxicity usually starts within 12-48h due to relatively severe, painless, bilateral optic nerve damage; which may be transient or progressive[3]–[4].
Rutin (3,3′,4′,5,7-pentahydroxyflavone-3-rhamnoglucoside) is a flavonoid with anti-inflammatory, anti-oxidant and analgesic effects, found in many vegetables and fruits[5]–[6]. Rutin attenuates oxidative stress by inhibiting membrane lipid peroxidation and increasing antioxidant enzyme levels[7]. Recently, Rutin was reported to have promising effects on chronic painful peripheral neuropathy and diabetic neuropathy[8]–[9].
In this experimental study, we aimed to determine the effects of Rutin on methanol induced optic neuropathy and compare the results with the effects of ethanol. We also aimed to investigate tissue 8-hydroxy-2 deoxyguanine (8-OHdG) levels as a determinant of DNA damage, inflammation markers such as interleukin-1β (IL-1β) and tumor necrosis factor-alpha (TNF-α), oxidative stress parameters including Myeloperoxidase (MPO) and malondialdehyde (MDA) and anti-oxidants glutathione peroxidase (tGSH) and superoxide dismutase (SOD) to elucidate the mechanism of association. To the best of our knowledge, this is the first study in literature investigating the role of Rutin in this type of optic neuropathy.
MATERIALS AND METHODS
This study was approved by the Ataturk University Animal Care and Use Committee (date: Jul. 28, 2017; number: 75296309). The study was performed between Aug. 1, 2017 and Aug. 8, 2017.
Study Animals
Totally 30 albino Wistar male rats (280-295 g) obtained from the Ataturk University Medical Experiments Application and Research Center were used in this study. The rats were housed at room temperature (22°C), fed twice a day and had access to water ad libitum.
The rats were divided into 5 study groups, with 6 rats in each group as follows: healthy controls (C), methotrexate (MTX), methotrexate+methanol (MTM), methotrexate+methanol+ethanol (MTME) and methotrexate+methanol+rutin (MTMR).
Experimental Design
In all rabbits except those of the control group, MTX, diluted in sterile serum physiologic, 0.3 mg/kg per oral was applied for 7d by the aid of a tube. After this procedure to the rats of MTM, MTME and MTMR groups, 20% methanol with a dose of 3 g/kg per oral was given by the aid of a tube. In MTME group, 4h after the application of methanol, 20% ethanol was applied by the same way with a dose of 0.5 g/kg. On the other hand, in MTMR group 4h after the application of methanol, Rutin (Solgar, USA), which was dissolved in distilled water, was applied by the same way with a dose of 50 mg/kg. Eight hours after the application of ethanol or rutin, all rats were sacrificed with high dose (50 mg/kg) thiopental (IE Ulagay, Turkey) anesthesia and optic nerves of all rats were dissected and obtained for the measurement of 8-OHdG levels, which is the end product of DNA damage, and for the histopathological evaluations; as defined before in literature before[10]. Tissue samples underwent routine processing, paraffin embedding, and sectioning. The tissues were stained with hematoxylin and eosin (H&E) and examined under light microscopy. Moreover, blood samples were also obtained from the animals in order to determine serum MDA, MOP, tGSH, SOD, IL-1β and TNF-α levels.
In experimental models of methanol intoxication, due to the high liver folic acid content and rapid formic acid metabolism, rats do not exhibit intoxication. For that reason, since Methotrexate is a folic acid antagonist, foliate-dependent formic acid metabolism is impaired with MTX treatment as defined in literature before[11].
Biochemical Analyses
DNA oxidation analysis
The levels of 8-OHdG in hydrolyzed DNA samples were measured at various wavelengths by high performance liquid chromatography (HPLC) with HPLC-UV and HPLC-ECD electrochemical detectors[12]. The final volume consisted of final hydrolysate, HPLC-ECD (HP, HP 1049A ECD detector, Agilent 1100 modular systems HP 1049A ECD detector, Germany), reverse-phase C18 column (250 mm×4.6 mm×4.0 µm; Phenomenex, Torrance, CA, USA) and a potassium phosphate (pH 5.5) tampon that contains acetonitrile (97:3, v/v) with 1 mL flow velocity per minute as the mobile phase. The 8-OHdG concentration was observed with electrochemical readings by measuring the absorbance at 245 nm. The 8-OHdG amounts, defined as the marker of DNA damage, were identified using 8-OHdG standards (Sigma, St. Louis, MO, USA).
IL-1β and TNF-α analysis in serum
Serum IL-1β and TNF-α concentrations were measured using rat-specific sandwich enzyme-linked immunosorbent assay: rat IL-1β ELISA kit: (Cat No.YHB0616Ra; Shanghai LZ, China) and rat TNF-α ELISA kits (Cat No.YHB1098Ra; Shanghai LZ, China). Analyses were performed according to the manufacturers' instructions.
tGSH analysis in serum
The 5,5′-dithiobis (2-nitrobenzoic acid) (DTNB) disulfide is chromogenic in the medium[13]. The yellow color produced during the reduction DTNB by sulfhydryl groups is measured by spectrophotometry at 412 nm. For measurement, a cocktail solution was prepared and added to the supernatant of the centrifuged serum. The standard curve was obtained by using glutathion.
MDA analysis in serum
MDA measurements were based on the method used by Ohkawa et al[14] involving spectrophotometrical measurement of absorbance of the complex formed by thiobarbituric acid (TBA) and MDA. The standard curve was obtained by using 1,1,3,3-tetramethoxypropane.
Analysis of myeloperoxidase activity in serum
H2O2 involving in phosphate buffer was used as substrate to determine MPO activity in serum[15]. Serum/tissue-homogenate was added to assay buffer and MPO activity was kinetically measurement at 460 nm for 5min.
Analysis of superoxide dismutuse activity in serum
Measurements were performed according to the method described by Sun et al[16] depending on the conversion of xanthine into uric acid by xanthine oxidase.
Analysis of histopathological data
Histopathological data including destruction, hemorrhage, congestion, edema, and decrease in oligodendrocyte and astrocyte counts were analyzed by the same pathologist and quantified between 0 and 3.
Statistical Analysis
The statistical analyses were performed with the Software SPSS version 21.0 (SPSS for Windows software; SPSS Inc., Chicago, IL, USA). Numerical variables were expressed as mean±standard deviation. For the analysis of continuous variables, one way variance analysis (ANOVA) was performed. Subsequently, in determination of different groups, Duncan multiple comparison test was performed. For the analysis of quantified data of histopathological analyses, Kruskal-Wallis test was performed. Statistical significance was set at P<0.05.
RESULTS
At the end of the study, all rats were evaluated without any failure. Regarding the biochemical results, there were statistically significant differences in 8-OHdG, IL-1β, TNF-α, MDA, MPO, tGSH and SOD levels between groups (Table 1). The highest tissue 8-OHdG and serum IL-1β, TNF-α, MDA, and MPO levels were determined in MTM and MTME groups while the anti-oxidant tGSH and SOD levels were the lowest in those groups. In MTMR group, tissue 8-OHdG, and serum IL-1β, MDA, and MPO levels were similar with the healthy controls but significantly different than other groups. In that aspect Rutin was effective to prevent the increases in systemic oxidative stress and inflammation markers.
Table 1. Results of biochemical analysis.
| Parameters | C | MTX | MTM | MTME | MTMR | fP |
| 8-OHdG | 0.81 ±0.03b,c,d | 1.57±0.09a,c,d,e | 2.9±0.28a,b,d,e | 2.10±0.14a,b,c,e | 0.92±0.04b,c,d | 0.001 |
| IL-1β | 1.65±0.18b,c,d | 2.81±0.24a,c,d,e | 9.18±0.33a,b,d,e | 4.7±0.42 a,b,c,e | 1.98±0.23b,c,d | 0.001 |
| TNF-α | 1.07±0.15b,c,d | 2.16±0.21a,c,d,e | 7.75±0.30a,b,d,e | 4.21±0.27a,b,c,e | 1.63±0.25b,c,d,e | 0.001 |
| MDA | 2.65±0.27b,c,d | 3.71±0.54a,c,d,e | 7.98±0.37a,b,d,e | 4.85±0.28a,b,c,e | 3.0±0.31b,c,d | 0.001 |
| MPO | 3.20±0.30b,c,d | 6.35±0.56a,c,d,e | 20.33±2.25a,b,d,e | 9.43±0.93a,b,c,e | 3.52±0.54b,c,d | 0.001 |
| tGSH | 6.68±0.48b,c,d | 4.21±0.41a,c,e | 1.85±0.18a,b,d,e | 3.73±0.36a,c,e | 6.18±0.45b,c,d | 0.001 |
| SOD | 20.0±2.61b,c,d,e | 6.0±0.56a,c,e | 2.88±0.23a,b,d,e | 5.20±0.61a,c,e | 9.95±0.55a,b,c,d | 0.001 |
C: Controls; MTX: Methotrexate group; MTM: Methotrexate+methanol group; MTME: Methotrexate+methanol+ethanol group; MTMR: Methotrexate+methanol+rutin group; 8-OHdG: 8-hydroxy-2 deoxyguanine; IL-1β: Interleukin-1β; TNF-α: Tumor necrosis factor-alpha; MPO: Myeloperoxidase; MDA: Malondialdehyde; tGSH: Glutathione peroxidase; SOD: Superoxide dismutase. aStatistically significantly different when compared with control group; bStatistically significantly different when compared with MTX group; cStatistically significantly different when compared with MTM group; dStatistically significantly different when compared with MTME group; eStatistically significantly different when compared with MTMR group; fP value of ANOVA test.
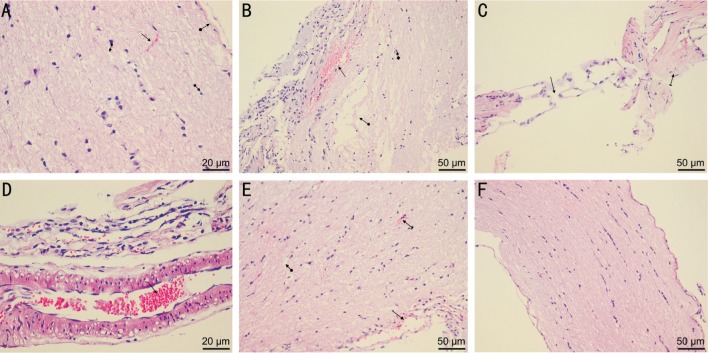
The results of quantified data in pathological analyses are summarized in Table 2. In that aspect, regarding all parameters, MTMR group was similar with the control group. The worst pathological alterations were determined in MTM group followed by MTME group. In histopathological evaluations; in MTX group, there was moderate focal destruction, hemorrhage and decrease in number of astrocytes and oligodendrocytes; in MTM group, there was severe destruction and edema with decrease in number of astrocytes and oligodendrocytes and dilated blood vessels; in MTME group, there was mild hemorrhage, mild edema, mildly dilated blood vessels with congestion while in MTMR group optic nerve tissue was resembling the healthy controls (Figure 1).
Table 2. Results of pathological analysis.
| Parameters | C | MTX | MTM | MTME | MTMR | fP |
| Destruction | 0b,c | 2.0±0.6a,c,d,e | 3.0±0.0a,b,d,e | 0b,c | 0b,c | <0.001 |
| Hemorrhage | 0b,c,d | 2.0±0.6a,c,d,e | 3.0±0.0a,b,d,e | 1.0±0.6a,b,c,e | 0b,c,d | <0.001 |
| Congestion | 0b,c | 0c,d | 3.0±0.0a,b,d,e | 1.0±0.6a,b,c,e | 0c,d | <0.001 |
| Edema | 0b,c | 0c,d | 3.0±0.0a,b,d,e | 1.0±0.6a,b,c,e | 0c,d | <0.001 |
| Decrease in oligodendrocytes | 0b,c | 2.0±0.6a,c,d,e | 2.8±0.4a,b,d,e | 0b,c | 0b,c | <0.001 |
| Decrease in astrocytes | 0b,c | 2.0±0.6a,c,d,e | 3.0±0.0a,b,d,e | 0b,c | 0b,c | <0.001 |
C: Controls; MTX: Methotrexate group; MTM: Methotrexate+methanol group; MTME: Methotrexate+methanol+ethanol group; MTMR: Methotrexate+methanol+rutin group; 8-OHdG: 8-hydroxy-2 deoxyguanine. aStatistically significantly different when compared with control group; bStatistically significantly different when compared with MTX group; cStatistically significantly different when compared with MTM group; dStatistically significantly different when compared with MTME group; eStatistically significantly different when compared with MTMR group; fP value of Kruskal-Wallis test.
Figure 1. Optic nerve of a rat in each group.
A: Optic nerve of a rat in control group. Square arrow is the meninx, straight arrow is the vessel, bilateral ended arrow is the astrocyte and circular arrow is the oligodendrocyte. H&E×400; B: Optic nerve of a rat in MTX group. There was moderate focal destruction (circular arrow), hemorrhage (straight arrow) and decrease in number of astrocytes and oligodendrocytes (square arrow). H&E×200; C: Optic nerve of a rat in MTM group. Severe destruction and edema (straight arrow) and decrease in number of astrocytes and oligodendrocytes (lined arrow). H&E×200; D: Optic nerve of a rat in MTM group. Dilated blood vessels with congestion (straight arrow). H&E×400; E: Optic nerve of a rat in MTME group. Mild hemorrhage (lined arrow), mild edema (squared arrow), mildly dilated blood vessels with congestion (straight arrow) H&E×200; F: Optic nerve of a rat in MTMR group. Optic nerve tissue resembling control group. H&E×200.
DISCUSSION
In this experimental study we have investigated the role of Rutin in treatment of methanol-induced optic neuropathy and we determined that, Rutin was highly effective in decreasing the inflammatory substances and oxidative stress markers while increasing the antioxidants in rats with methanol toxicity. Histopathological evaluations of optic nerve were also supporting the promising effects of Rutin in treatment of methanol-induced optic neuropathy. To the best of our knowledge, this is the first study in literature evaluating the role of Rutin in optic neuropathy.
Methanol is an oxidant inducing free radical changes and oxidative damages. In an experimental study, Rajamani et al[17] reported that methanol exposure causes increased generation of free radicals and significant oxidative damage in retina and optic nerve. Clinically, acute methanol intoxication is known to cause visual disturbances that may be transient or persistent. Although the personal susceptibilities may vary regarding the toxic effects of different methanol doses, as little as 10 mL may cause blindness[18]. Zakharov et al[19] reported that, totally 13 of 50 patients diagnosed with acute methanol intoxication were discharged with visual squeal and during follow-ups 20/50 (40%) of the patients had long-term visual sequel, with 8% of blindness. In that aspect, clinicians should be aware of long-term visual sequelae associated with methanol intoxication which may be underestimated during discharge.
Methanol is metabolized in the liver by alcohol dehydrogenase enzyme to formaldehyde, and then by formaldehyde dehydrogenase to formic acid rapidly[20]. Formic acid is a toxic substance that inhibits aerobic metabolism and energy production inducing acidosis with high plasma anion gap. Due to the inhibition of cytochrome oxidase activity and prevention of mitochondrial oxygen production in optic nerve by formic acid, optic neuropathy takes place in methanol toxicity causing damaged axonal flow with mitochondrial edema and fragmentation of neurofilaments[21]–[22]. Another important point in methanol metabolism is the requirement of foliate in the metabolism of formic acid to CO2 and H2O. Enhancing formic acid elimination may also improve the visual disturbances in methanol toxicity.
Optic nerve, retina, and basal ganglia are the main tissues that are at risk from methanol intoxication which may be associated with the high mitochondrial energy requirement in these tissues. Usually following a latent period of 12-36h after the ingestion time, most probably required for the methanol metabolism and formic acid accumulation, visual symptoms start which are generally painless, bilateral and severe[23]. Paasma et al[24] reported the 6y follow-up results after a methanol outbreak of 111 hospitalized patients and described that new neurological and visual complications were identified in more than one third of the patients. In order to avoid neurological and visual sequelae, prompt treatment of methanol ingestion including the correction of the systemic acidosis, foliate supplementation and inhibition of methanol metabolism are essential.
Prevention of formic acid formation by inhibiting liver alcohol dehydrogenase enzyme and restoration of normal pH to diminish the cellular formic acid entry by sodium bicarbonate or dialysis are the main steps in treatment[1]. Ethanol is a competitive inhibitor of liver alcohol dehydrogenase, which is one of the main treatment options in methanol intoxication[25]. Fomepizole is another competitive inhibitor of aldehyde dehydrogenase that also prevents formic acid formation in methanol toxicity[26]–[27]. Some other treatment options, such as high dose prednisolone, erythropoietin and alpha-lipoic acid as an anti-oxidant were also reported to have promising effects in methanol-induced toxic optic neuropathy but prospective studies are required to determine the exact role of those treatment options[28]–[30].
Flavonoids are a group of natural poly-phenolic compounds playing significant roles in detoxification of free radicals[31]. Rutin is a flavonoid with strong proton donating and free radical stabilizing properties; thus reducing generation of reactive oxygen species[32]. Rutin may also improve endothelial function by enhancing nitric oxide production in human endothelial cells which is also an anti-oxidant action[33]. Recently, it was reported to inhibit glycation and creation of advanced glycation end products on eye lens protein[34]. Rutin was also reported to prevent oxaliplatin induced painful peripheral neuropathy in an experimental model[9]. Moreover, the beneficial effects of Rutin on diabetic neuropathy were reported via attenuation of the oxidative stress and neuro-inflammation[8]. To the best of our knowledge, Rutin was not studied before in treatment of methanol-induced optic neuropathy. In this study we also determined promising effects of Rutin in prevention of methanol induced optic neuropathy with its anti-inflammatory and anti-oxidant effects.
There are some limitations of this study that should be mentioned. First, as all experimental studies, it carries the bias associated with the differences between metabolisms of animals and human beings. Second is the short follow-up time in that study.
In conclusion, Rutin may prevent methanol-induced optic neuropathy via anti-inflammatory effects and decreasing the oxidative stress. New treatment options are warranted in this disease to avoid loss of vision in patients.
Acknowledgments
Conflicts of Interest: Taşli NG, None; Çimen FK, None; Karakurt Y, None; Uçak T, None; Mammadov R, None; Süleyman B, None; Kurt N, None; Süleyman H, None.
REFERENCES
- 1.Kraut JA, Kurtz I. Toxic alcohol ingestions: clinical features, diagnosis, and management. Clin J Am Soc Nephrol. 2008;3(1):208–225. doi: 10.2215/CJN.03220807. [DOI] [PubMed] [Google Scholar]
- 2.Jain N, Himanshu D, Verma SP, Parihar A. Methanol poisoning: characteristic MRI findings. Ann Saudi Med. 2013;33(1):68–69. doi: 10.5144/0256-4947.2012.26.5.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galvez-Ruiz A, Elkhamary SM, Asghar N, Bosley TM. Visual and neurologic sequelae of methanol poisoning in Saudi Arabia. Saudi Med J. 2015;36(5):568–574. doi: 10.15537/smj.2015.5.11142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tanrivermis Sayit A, Aslan K, Elmali M, Gungor I. Methanol-induced toxic optic neuropathy with diffusion weighted MRI findings. Cutan Ocul Toxicol. 2016;35(4):337–340. doi: 10.3109/15569527.2015.1122031. [DOI] [PubMed] [Google Scholar]
- 5.Di Carlo G, Mascolo N, Izzo AA, Capasso F. Flavonoids: old and new aspects of a class of natural therapeutic drugs. Life Sci. 1999;65(4):337–353. doi: 10.1016/s0024-3205(99)00120-4. [DOI] [PubMed] [Google Scholar]
- 6.Asgary S, Naderi GA, Zadegan NS, Vakili R. The inhibitory effects of pure flavonoids on in vitro protein glycosylation. J Herb Pharmacother. 2002;2(2):47–55. [PubMed] [Google Scholar]
- 7.Magalingam KB, Radhakrishnan A, Haleagrahara N. Rutin, a bioflavonoid antioxidant protects rat pheochromocytoma (PC-12) cells against 6-hydroxydopamine (6-OHDA)-induced neurotoxicity. Int J Mol Med. 2013;32(1):235–240. doi: 10.3892/ijmm.2013.1375. [DOI] [PubMed] [Google Scholar]
- 8.Tian R, Yang W, Xue Q, Gao L, Huo J, Ren D, Chen X. Rutin ameliorates diabetic neuropathy by lowering plasma glucose and decreasing oxidative stress via Nrf2 signaling pathway in rats. Eur J Pharmacol. 2016;771:84–92. doi: 10.1016/j.ejphar.2015.12.021. [DOI] [PubMed] [Google Scholar]
- 9.Azevedo MI, Pereira AF, Nogueira RB, Rolim FE, Brito GA, Wong DV, Lima-Júnior RC, de Albuquerque Ribeiro R, Vale ML. The antioxidant effects of the flavonoids rutin and quercetin inhibit oxaliplatin-induced chronicpainful peripheral neuropathy. Mol Pain. 2013;9:53. doi: 10.1186/1744-8069-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sahin A, Kaya S, Türkcü G, Cingü AK, Yüksel H, Türkcü FM, Yüksel H, Cınar Y, Arı S, Sahin M, Caça I, Gökalp O. The effects of caffeic acid phenethyl ester in acute methanol toxicity on rat retina and optic nerve. Cutan Ocul Toxicol. 2013;32(4):263–267. doi: 10.3109/15569527.2013.771642. [DOI] [PubMed] [Google Scholar]
- 11.Eells JT, Henry MM, Lewandowski MF, Seme MT, Murray TG. Development and characterization of a rodent model of methanol-induced retinal and optic nerve toxicity. Neurotoxicology. 2000;21(3):321–330. [PubMed] [Google Scholar]
- 12.Shigenaga MK, Aboujaoude EN, Chen Q, Ames BN. Assays of oxidative DNA damage biomarkers 8-oxo-2′-deoxyguanosine and 8-oxoguanine in nuclear DNA and biological fluids by high-performance liquid chromatography with electrochemical detection. Meth Enzymol. 1994;234:16–33. doi: 10.1016/0076-6879(94)34073-0. [DOI] [PubMed] [Google Scholar]
- 13.Sedlak J, Lindsay RH. Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman'sreagent. Anal Biochem. 1968;25(1):192–205. doi: 10.1016/0003-2697(68)90092-4. [DOI] [PubMed] [Google Scholar]
- 14.Ohkawa H, Ohishi N, Yagi K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem. 1979;95(2):351–358. doi: 10.1016/0003-2697(79)90738-3. [DOI] [PubMed] [Google Scholar]
- 15.Bradley PP, Priebat DA, Christensen RD, Rothstein G. Measurement of cutaneous inflammation: estimation of neutrophil content with an enzyme marker. J Invest Dermatol. 1982;78(3):206–209. doi: 10.1111/1523-1747.ep12506462. [DOI] [PubMed] [Google Scholar]
- 16.Sun Y, Oberley LW, Li Y. A simple method for clinical assay of superoxide dismutase. Clin Chem. 1988;34(3):497–500. [PubMed] [Google Scholar]
- 17.Rajamani R, Muthuvel A, Senthilvelan M, Sheeladevi R. Oxidative stress induced by methotrexate alone and in the presence of methanol in discrete regions of the rodent brain, retina and optic nerve. Toxicol Lett. 2006;165(3):265–273. doi: 10.1016/j.toxlet.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 18.Bennett IL, Jr, Cary FH, Mitchell GL, Jr, Cooper MN. Acute methyl alcohol poisoning: a review based on experiences in an outbreak of 323 cases. Medicine (Baltimore) 1953;32(4):431–463. doi: 10.1097/00005792-195312000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Zakharov S, Pelclova D, Diblik P, Urban P, Kuthan P, Nurieva O, Kotikova K, Navratil T, Komarc M, Belacek J, Seidl Z, Vaneckova M, Hubacek JA, Bezdicek O, Klempir J, Yurchenko M, Ruzicka E, Miovsky M, Janikova B, Hovda KE. Long-term visual damage after acute methanol poisonings: Longitudinal cross-sectional study in 50 patients. Clin Toxicol (Phila) 2015;53(9):884–892. doi: 10.3109/15563650.2015.1086488. [DOI] [PubMed] [Google Scholar]
- 20.Lee SL, Shih HT, Chi YC, Li YP, Yin SJ. Oxidation of methanol, ethylene glycol, and isopropanol with human alcohol dehydrogenases and the inhibition by ethanol and 4-methylpyrazole. Chem Biol Interact. 2011;191(1-3):26–31. doi: 10.1016/j.cbi.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Hayreh MS, Hayreh SS, Baumbach GL, Cancilla P, Martin-Amat G, Tephly TR, McMartin KE, Makar AB. Methyl alcohol poisoning III. Ocular toxicity. Arch Ophthalmol. 1977;95(10):1851–1858. doi: 10.1001/archopht.1977.04450100153022. [DOI] [PubMed] [Google Scholar]
- 22.Baumbach GL, Cancilla PA, Martin-Amat G, Tephly TR, McMartin KE, Makar AB, Hayreh MS, Hayreh SS. Methyl alcohol poisoning. IV. Alterations of the morphological findings of the retina and optic nerve. Arch Ophthalmol. 1977;95(10):1859–1865. doi: 10.1001/archopht.1977.04450100161023. [DOI] [PubMed] [Google Scholar]
- 23.Sanaei-Zadeh H, Zamani N, Shadnia S. Outcomes of visual disturbances after methanol poisoning. Clin Toxicol (Phila) 2011;49(2):102–107. doi: 10.3109/15563650.2011.556642. [DOI] [PubMed] [Google Scholar]
- 24.Paasma R, Hovda KE, Jacobsen D. Methanol poisoning and long term sequelae - a six years follow-up after a large methanol outbreak. BMC Clin Pharmacol. 2009;9:5. doi: 10.1186/1472-6904-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sadun A. Acquired mitochondrial impairment as a cause of optic nerve disease. Trans Am Ophthalmol Soc. 1998;96:881–923. [PMC free article] [PubMed] [Google Scholar]
- 26.Mégarbane B, Borron SW, Trout H, Hantson P, Jaeger A, Krencker E, Bismuth C, Baud FJ. Treatment of acute methanol poisoning with fomepizole. Intensive Care Med. 2001;27(8):1370–1378. doi: 10.1007/s001340101011. [DOI] [PubMed] [Google Scholar]
- 27.Hovda KE, Froyshov S, Gudmundsdottir H, Rudberg N, Jacobsen D. Fomepizole may change indication for hemodialysis in methanol poisoning: prospective study in seven cases. Clin Nephrol. 2005;64(3):190–197. doi: 10.5414/cnp64190. [DOI] [PubMed] [Google Scholar]
- 28.Sanaei-Zadeh H. What are the therapeutic effects of high-dose intravenous prednisolone in methanol-induced toxic optic neuropathy? J Ocul Pharmacol Ther. 2012;28(4):327–328. doi: 10.1089/jop.2011.0209. [DOI] [PubMed] [Google Scholar]
- 29.Pakravan M, Sanjari N. Erythropoietin treatment for methanol optic neuropathy. J Neuroophthalmol. 2012;32(4):325–328. doi: 10.1097/WNO.0b013e318262a7c2. [DOI] [PubMed] [Google Scholar]
- 30.Rajamani R, Muthuvel A, Manikandan S, Srikumar R, Sheeladevi R. Efficacy of DL-alpha-lipoic acid on methanol induced free radical changes, protein oxidative damages and hsp70 expression in folate deficient rat nervous tissue. Chem Biol Interact. 2007;167(3):161–167. doi: 10.1016/j.cbi.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 31.AlSharari SD, Al-Rejaie SS, Abuohashish HM, Ahmed MM, Hafez MM. Rutin attenuates hepatotoxicity in high-cholesterol-diet-fed rats. Oxid Med Cell Longev. 2016;2016:5436745. doi: 10.1155/2016/5436745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Verma S, Gupta ML. Radiation-induced hematopoietic myelosuppression and genotoxicity get significantly countered by active principles of Podophyllum hexandrum: a study in strain ‘A’ mice. Int J Radiat Biol. 2015;91(9):757–770. doi: 10.3109/09553002.2015.1062576. [DOI] [PubMed] [Google Scholar]
- 33.Al-Dhabi NA, Arasu MV, Park CH, Park SU. An up-to-date review of rutin and its biological and pharmacological activities. EXCLI J. 2015;14:59–63. doi: 10.17179/excli2014-663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muthenna P, Akileshwari C, Saraswat M, Bhanuprakash Reddy G. Inhibition of advanced glycation end-product formation on eye lens protein by rutin. Br J Nutr. 2012;107(7):941–949. doi: 10.1017/S0007114511004077. [DOI] [PubMed] [Google Scholar]