Abstract
Objective
To describe the process by which a group of subject matter experts in the area of return to work developed a resource tool to provide clinical decision support (CDS) for primary care clinicians.
Methods
A common musculoskeletal disorder, low back pain (LBP), was selected, pertinent literature reviewed, and specific recommendations for action in the clinical setting developed.
Results
Primary care practitioners (PCPs) are routinely expected to create work activity prescriptions. The knowledge base for a CDS tool that could be embedded in electronic health records has been developed.
Conclusions
Improved clinical support should help prevent and manage work limitations associated with LBP not caused by work. The proposed decision support should reduce administrative burden and stimulate PCPs to explore the role of occupation and its demands on patients.
Introduction
As discussed in the introductory article by Filios, et al, the National Institute for Occupational Safety and Health (NIOSH) engaged the Return-to-Work (RTW) Subject Matter Expert (SME) work group to prepare a knowledge resource report for musculoskeletal conditions not caused by work that summarizes the current state of the science behind RTW determinations. NIOSH instructed the SME work group to address non-work-related injuries in order to emphasize that personal health, not only occupational health, interacts with work. This report recommends ways to use existing science to develop clinical decision support (CDS) tools to assist primary care practitioners (PCPs) in RTW guidance. The CDS tool is intended to be embedded in electronic health record (EHR) systems. The entire technical report that forms the basis for this article is available on the American College of Occupational and Environmental Medicine’s (ACOEM) web site.*
Process for Selecting the Condition
Rationale for Choice of Acute Low Back Pain As the Focus of a Clinical Decision Support Tool
Because of its prevalence in primary care practice and its association with work disability and activity restriction, the work group chose to focus on acquired (non-congenital) acute, non-specific low back pain (LBP) without red flags—a condition that adds to the daily administrative burden of primary care because patients and other stakeholders frequently ask PCPs to write functional limitation prescriptions for patients with LBP.
LBP with its wide range of acuity and severity is the fourth most-common complaint for which patients seek medical care.1,2,3,4 It accounts for approximately 15 million visits a year to health care providers.5 In addition, LBP is the second most common cause of work disability in US adults.6 It has been estimated that 60-80% of the general population will experience at least one episode of LBP during their lifetime and this episode will be significant enough to disrupt their daily activities.7 The actions of PCPs can contribute to or mitigate acquired LBP-associated work disability.8 The focus on acute rather than chronic LBP was based on the greater opportunity for preventing work disability. The approach of excluding LBP with red flags (eg, spinal fractures) is justified as it is rare for patients with acute LBP to present with red flags.9-12 Red flags also create clinical priorities that generally contra-indicate work, such as in the case where emergency surgery is required for cauda equina or spinal fracture.
Evidence Underlying Clinical Decision Support Tool
As described in the entire technical report,* methods used to collect evidence to construct and support the recommendation triggered by the CDS included searches of MedLine/PubMed and Google Scholar from June 2008 to August 22, 2014. Search terms included:
primary care;
musculoskeletal;
return to work; and
risk assessment.
Search terms that yielded more than 250 articles were limited to studies of humans and those published in English. The search for disability (prevention OR treat* OR manage*) was further limited to systematic reviews or meta-analyses. Only studies published in peer-reviewed journals or government documents or publications from ACOEM7 or the American Medical Association13 publications were used to develop the work group’s conclusion. Grading criteria was based on the methodology used to develop the ACOEM Practice Guidelines, which is based on the Grading of Recommendations Assessment, Development and Evaluation (GRADE) standards for guideline development. In addition to the existing evidence, the work group relied on its members’ expertise to construct a recommendation as the basis for the CDS tool. Of particular interest to the reader may be a recent scoping review of CDS tools for selecting interventions for patients with disabling musculoskeletal conditions.14
What Were the Decision Points that Led to the Choice of the Default Limitation Duration?
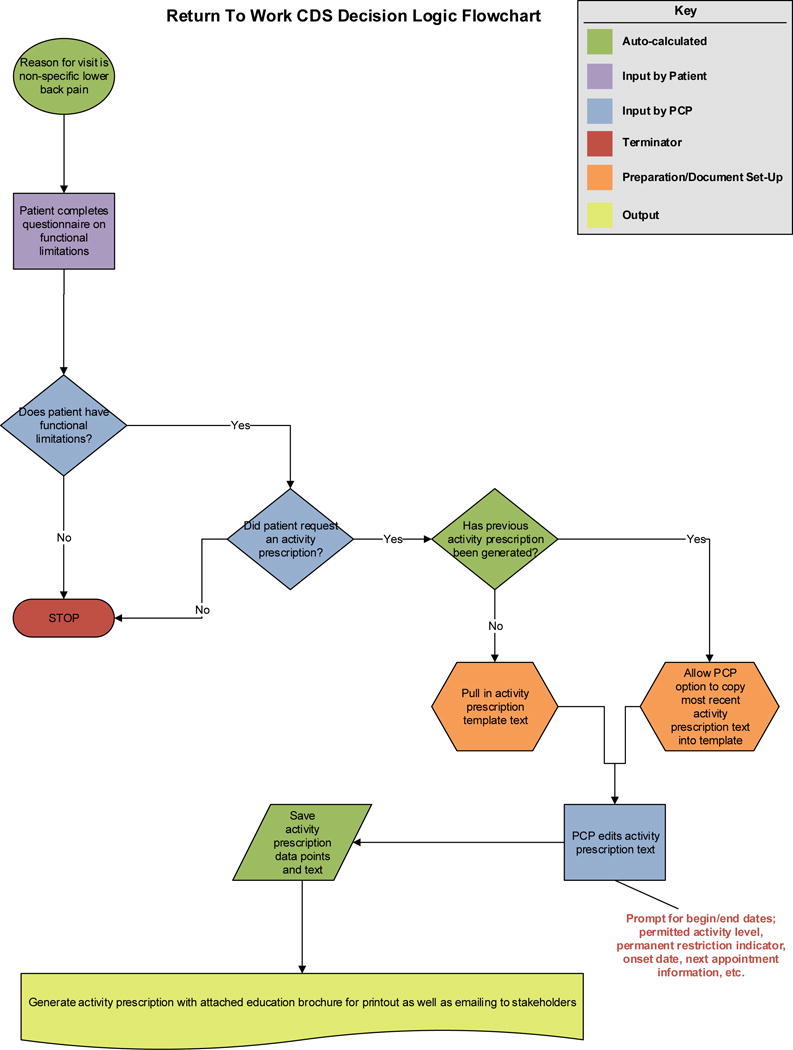
The work group used a deliberative process based on a combination of evidence and members’ expertise as described below to create a clinical work flow (Table 1).
Table 1.
Process/Elements of the EHR LBP CDS Tool
| Step | Process/Work Flow | Action/Outcome |
|---|---|---|
| 1 | Patient presents due to acute LBP with or without leg pain. | Patient completes questionnaire at check-in which asks how his LBP is affecting his activities of daily life (functional limitations). |
| 2 | PCP takes detailed history to evaluate LBP, including previous episodes and/or injuries. | Enter patient history and chief complaint into electronic health record (EHR). |
| 3 | Conduct physical examination:
|
Enter findings into EHR. PCP accesses information (eg, via button/hover-activated link) that provides summary of red flags in back pain. PCP accesses “functional limitations” table via link in EHR. Table provides examples of common limitations, eg, difficulty bending, kneeling, climbing, lifting. |
| Activity Prescription Triggers | ||
| 4a or |
Assessment of functional limitations leads to discussion of impact on work/life activities; patient asks for activity prescription/note for employer. | PCP activates activity prescription tool tab. Go to Step 6 … Or |
| 4b or |
Enter diagnosis based on history and physical examination into EHR | Entering Dx activates activity prescription tool tab. Or |
| 4c | Prescribe treatment plan/write order set
|
Activity prescription activated as part of the order set. PCP prescribes treatment (eg, medication) which activates tool to generate Activity Prescription report. |
| Activity Prescription | ||
| 5 | Generate activity prescription |
Activity prescription report tab opens in one of the three scenarios discussed above in Step 4. Based on the PCP’s choice of activity restrictions ranging from sedentary to medium per the Directory of Occupational Titles descriptions, the CDS autopopulates an activity prescription which specifies permitted activities and provides a specific date for elimination of activity restrictions that will limit unnecessary restrictions or trigger more contact with PCP if patient wants to extend restrictions/work disability beyond CDS date for return to full duty. Although autopopulated, the restrictions are fully editable. The activity prescription includes closing direction: “Over the next 4 weeks, the patient may gradually increase activity as tolerated to usual activities. If the patient is unable to tolerate activities as written above or has not returned to usual activities within 4 weeks, the employer, insurer, or patient should contact provider for further guidance.” The CDS tool also includes a box that the PCP can check to indicate that the activity limitation is permanent, thereby eliminating the need to recreate the activity prescription. |
| 6 | Discuss activity prescription with patient (if not already done in Step 4a) | Reviewing the activity prescription with the patient should result in a discussion of whether the prescription will restrict the patient from performing regular duties and elicit enough information to adjust the activity prescription accordingly. PCP discusses the activity prescription with patient to assure patient:
In addition to generating a detailed activity prescription for the patient (which can be shared with the employer or stakeholder*), the CDS tool generates a patient education brochure which discusses the value of returning to work and/or maintaining or increasing activity during recovery. *Patient permission needed. In many cases, the activity prescription will be handed directly to the patient, who can choose to provide it to another party. In cases such as short-term work disability or workers’ compensation, where a third party is requesting release or generation of this information, the patient needs to submit the request. This ensures all release forms are signed and the patient is aware of the request. If authorization is required, this form should be scanned into the EHR. |
| 7 | Follow-up | The CDS tool will not automatically specify return visits to revise the activity prescription. However, patients who do not recover by the date specified for elimination of activity restrictions should be reassessed. |
Discussion of Functional Limitations
The work group decided the CDS should trigger collection, documentation, and discussion of the impact of functional limitations because an activity prescription is not needed unless there is a problem that restricts the patient’s work and/or other activities. Recognizing that practices differ with respect to optimal clinical flow, the work group suggests two options for obtaining functional limitation information. The first and preferred option would be to collect information on functional limitations at the initial visit for every patient who presents with acute LBP. This information would be gathered in the waiting room by asking the patient to complete a questionnaire electronically or on paper. A second option envisions postponing discussion of functional limitations until an activity note has been requested by the patient or other stakeholder. While ideally all information should be entered by the patient with an interface directly into the medical record, in cases were a patient is not fluent in English, is functionally illiterate, or has difficulty with entering data electronically, a medical or administrative assistant could enter the data into the record as part of the initial note.
In the context of the office visit, the PCP would rule out red flags and document whether the patient reports functional limitations. The CDS would include a table activated through a link or hover-over option that would provide short text or pictoral examples of common limitations (eg, difficulty bending, kneeling, climbing, lifting, etc.) to discuss with the patient. These general examples would not be specific to work as the activity prescription is intended to be used for both occupational and non-occupational activities restrictions. The work group believes that without too much prompting, the patient will indicate those areas of her/his life that are affected by LBP.
Creating, Discussing, and Transmitting an Activity Prescription
Employers often expect PCPs to provide activity prescriptions for patients with acute LBP. Patients also commonly seek specific recommendations from their PCPs regarding which activities they can perform or should avoid in order to facilitate recovery.15 To assist the PCP in providing these recommendations, the CDS would generate an activity prescription using a standard format. The term “activity prescription” rather than “return to work note” is used to emphasize the universality of the prescription for a variety of purposes. It informs the patient equally about occupational and non-occupational limitations and is also meant to serve as a report that satisfies stakeholders besides employers, eg, disability carriers, athletic coaches, etc., about the patient’s limitations.
When the activity prescription tool is triggered, a report specifying permitted activities is created using actuarial data and expert consensus consistent with the Dictionary of Occupational Titles’ job physical demands classifications.16 The report includes both duration of restrictions and commonly requested details such as weight lifting and bending limitations (see entire report*). The CDS tool does not require the PCP to collect occupational health data before generating the activity prescription because job demand information is not likely to be present in the chart and collecting occupational data adds to the provider’s burden.
The activity prescription will by default provide a specific date—usually 4 weeks from the initial visit—at which time the activity restrictions will expire. This time frame was chosen because the majority of activity limiting, acute LBP exacerbations substantially resolve within 4 weeks. This approach aims to limit unnecessary work disability. While it is possible that some patients will have more limitations, the 4-week cap should help prevent prolonged activity restriction. Unlike common occupational medicine practice, the work group decided it was prudent not to require follow-up visits with the PCP for full release. Limited access to primary care, the expense of return visits, likelihood of resolution of functional impairment within 4 weeks, and the common ability for workers to negotiate a gradual increase of activity led to this decision.
Additionally, the medical necessity for re-evaluation before RTW is unlikely to be helpful for a variety of reasons, including that back pain is not clearly related to physical damage to the back. Advice to stay active has consistently shown to be beneficial, therefore instilling the expectation in patients that they should recover constitutes good treatment, and light- to medium-duty activity is probably beneficial.17-35 However, providers should reassess patients if they do not recover by the date specified or if problems arise when activities are gradually increased. The work group is not recommending an automatic 4 weeks of work restriction, thus the form, although auto-populated, can be edited for shorter time frames. According to data in MDGuidelines, the maximum expected functional limitation is 28 days for non-work-related degenerative disc condition, but more than 75% of patients actually take more days off—thus a 4 week cap is not only reasonable, but should trigger additional investigation.36
The work group envisions that the CDS will be capable of importing the data from the most recent previous activity prescription into the current encounter prescription while allowing for the new activity prescription to be edited. This should further ease the PCP’s task of writing activity prescriptions. The CDS will also include a box that the PCP can check to indicate that the activity limitation is permanent, thus eliminating the need to create future activity prescriptions.
The PCP and patient should discuss the activity prescription to assure the patient understands the prescription and has the opportunity to ask for a modification if the prescription does not accommodate his or her circumstances. Along with a copy of the printed activity prescription, the PCP should provide educational material about the benefit of gradually increasing activities. Evidence supports the recommendation that framing the patient’s expectation for full functional recovery will increase the likelihood of an early return to normal activity.8
Although NIOSH directed the SME work group to develop a tool to provided guidance to PCPs for preventing and managing disability due to non-occupational causes, this tool can be applied equally to work-related acute back pain. Further, the activity prescription could serve as the standard response to any request or form requiring an activity prescription, not just as a RTW prescription. If required, the provider could attach the activity prescription produced by the CDS tool to other signed forms with a comment on the form to see the attached prescription.
How Did the SMEs Evaluate the Evidence for the Recommendation?
In addition to using the evidence-grading criteria of ACOEM’s Practice Guidelines, based on the GRADE standards, tools developed by Yale Center for Medical Informatics,37 and the American Academy of Pediatrics Steering Committee on Quality Improvement and Management,38 were used to develop the CDS (Appendix F*).
Work Disability Detrimental to Health and Quality of Life
Investigation of the negative impact of work disability to patient health is not amenable to randomized, controlled studies. However, strong, observational evidence exists that work disability results in adverse health effects and increasing activity promotes rehabilitation. As previously noted, acute LBP that results in intolerance or loss of work, can lessen a patient’s quality and duration of life.39,40 Evidence has shown that long-term absence from work degrades a patients’ mental, physical, social, and financial well-being.7,8,13,41 A recent systematic review and meta-analysis found that unemployment has a hazard ratio of 1.6 for premature mortality.42 Systematic reviews have also shown that staying active improves health.43 Thus, PCPs who are competent in writing appropriate activity prescriptions for patients with LBP, can help guide their patients’ recovery and return to normal activities.
Primary Care Providers Are Currently Expected to Produce Activity Prescriptions for Patients with LBP
Completing work restriction paperwork and activity prescriptions add to the administrative burden of primary care. There is strong “administrative” (observational) evidence supporting the potential benefit of a CDS tool that would facilitate the process for PCPs to create an activity prescription. Because many patients with LBP require an activity prescription, these prescriptions are an administrative “fact” of practice for PCPs.44
Choice of a Default Limitation Duration
Actuarial data from the US Bureau of Labor Statistics documents the mean and range of work disability durations associated with LBP; however, there is little good evidence—beyond expert opinion—concerning what is the appropriate level of default restrictions. Therefore, the work group had to rely on moderate-level evidence that setting an expectation of early, graded return to normal activity allows most patients with LBP to recover within 4 weeks.45,46 The work group also relied on its expert opinion to support the value of a default activity prescription in EHR systems to reduce work disability.
Recommendation Strength
Overall, the work group concludes that the Evidence Quality is “B” for the proposed CDS tool because it is supported by trials or diagnostic studies with minor limitations, and is consistent with the findings from multiple observational studies. This B rating and a balance of benefits over harms, led the work group to conclude that its Recommendation Strength is Moderate (Appendix B*).
Recommended Intervention
Guidelines, such as those published by ACOEM, review evidence and provide guidance on best practice. The key action statement spells out under what clinical circumstances the PCP should take specific actions. The CDS would be triggered in the EHR whenever this clinical scenario is encountered.
IF a patient presents with acute LBP with or without leg pain AND without red flags (potentially serious disorders that include acute fractures, acute dislocations, infection, tumor, progressive neurologic deficit, or cauda equina syndrome AND has functional limitations AND the patient requests or requires an activity note or instructions about activity;
THEN the treating primary care provider SHOULD:
- ■
discuss the impact of the functional limitations on the patient’s work and other activities AND
- ■
write an activity prescription for the patient AND
- ■
transmit the activity prescription to other stakeholders who legitimately request the prescription AND accompany the prescription with a printed education brochure regarding the value of return to work and/or maintaining and increasing activity during recovery.
Case Example
In the case of a 22-year-old male who presents to his PCP on Monday morning for acute onset severe midline LBP which occurred after moving a large stone at home the day before, the work group developed a process (Table 1*) which describes how the PCP would use the CDS tool to support a common case scenario.
Limitations
Clinicians are only one of the many stakeholders in a complex network of people and circumstances influencing return to work associated with LBP. While LBP may be a non-work-related condition, its impact on RTW involves four categories of workplace factors: 1) physical job demands; 2) psychosocial job demands; 3) work organization and support; and 4) workplace beliefs and attitudes.47,48 Other factors include patient’s co-morbidities and psychological resilience, job satisfaction, and the patient’s relationship with his/her supervisors and co-workers and social conventions.49 The CDS tool affects just one aspect of this complex system.
Additional important limitations of the tool include the current lack of evidence that providing default activity prescriptions will actually reduce unnecessary work limitation. The effectiveness of this tool remains to be tested. The complete report outlines a variety of outcomes as well process measures that could be used to assess the effectiveness of the CDS RTW tool (Appendix N*).
The work group recognizes that there are potential risks associated with the CDS tool. These may include inadvertently creating more work limitations by providing more restrictions for patients and/or the duplication of work for the PCP by creating another form to complete if the requesting stakeholder does not accept this automatically generated activity prescription. In addition, some patients may be unhappy with less strict work restrictions and more limited time off.
Alternatively, the work group envisions many potential benefits for both the patient and the PCP. For the patient, the CDS tool should encourage continuation of or quick return to normal activities and prevent maladaptive behavior which may lead to permanent and total work disability. This in turn protects/improves the patient’s emotional state and helps maintain his/her financial status (no loss of salary), thereby preventing the adverse health effects of declining income. The benefits to the PCP include improved workflow and improved quality of care for the patient. In addition, the tool promotes equal treatment of patients and reduces both the direct and indirect costs to employers and society.
Anticipated Impact on Clinical Care, Public Health, and Population Health
The intent of the CDS tool is to assist the PCP achieve specific aims:
-
■
prevent unnecessary work disability;
-
■
improve the quality of medical care by addressing a key aspect of the patient’s quality of life (physical, mental health, economic, social, and functional status);
-
■
make a common provider task easier by facilitating the creation and communication of an activity prescription to employers (and often insurers) for which there is already a social, legal, and patient expectation of the PCP;
-
■
reduce economic burden of work disability on society;
-
■
stimulate the PCP to consider the interaction between patients’ work and health and respond in ways that have a more positive impact;
-
■
enhance consistency in activity recommendations, and better alignment with available evidence; and,
-
■
strive to increase PCP interest in capturing occupational health data in electronic health records (EHRs).
Conclusion
Preventing work disability is important from a clinical, public health, and societal standpoint as prolonged absence from work leads to poor health, negative economic consequences, and secondary impacts of lower income on health, self-esteem, and well-being.41 Back pain is common and PCPs are often asked to generate activity prescriptions, but have little training on how these prescriptions can prevent and manage LBP-associated functional limitations. By supporting the creation and communication of evidence-based activity prescriptions, the CDS tool should help improve patients’ quality of life by preventing unnecessary work disability. Although designed specifically to provide guidance regarding activity associated with acute LBP, the CDS could be expanded to other conditions and support both non-work-related and work-related disability. By facilitating the generation of the activity prescription—already a social, legal, and patient expectation of PCPs—this tool should reduce administrative burden. The tool may also help PCPs understand the role of occupation and its demands on patients and the need to capture occupational health data in the EHR.
Figure 1.
Footnotes
The authors report no conflicts of interest.
The entire technical report from which this article is drawn, is available online at www.acoem.org/.
References
- 1.Williams CM, Maher CG, Hancock MD, McAuley JH, McLachlan AJ, Britt H, Fahridin S, Harrison C, Latimer J. Low back pain and best practice care: a survey of general practice physicians. Arch Intern Med. 2010;170:271–7. doi: 10.1001/archinternmed.2009.507. [DOI] [PubMed] [Google Scholar]
- 2.Finestone AS, Raveh A, Mirovsky Y, Lahad A, Milgrom C. Orthopaedists’ and family practitioners’ knowledge of simple low back pain management. Spine (Phila Pa 1976) 2009;34:1600–3. doi: 10.1097/BRS.0b013e3181a96622. [DOI] [PubMed] [Google Scholar]
- 3.Somerville S, Hay E, Lewis M, van der Windt D, Hill J, Sowden G. Content and outcome of usual primary care for back pain: a systematic review. Br J Gen Pract. 2008;58:790–7. doi: 10.3399/bjgp08X319909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Centers for Disease Control and Prevention. Prevalence of disabilities and associated health conditions among adults – United States, 1999. JAMA. 1999;285:1571–2. [PubMed] [Google Scholar]
- 5.Hsiao C-J, Cherry DK, Beatty PC, Rechtsteiner EA, Division of Health Care Statistics National Ambulatory Medical Care Survey: 2007 Summary. DHHS, CDC, National Center for Health Statistics. National Health Statistics Reports. 2010;27:1–32. [PubMed] [Google Scholar]
- 6.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003;290:2443–54. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 7.Hegmann K, editor. Occupational Medicine Practice Guidelines. Denver CO: Reed Group; 2014. Low back disorders. (American College of Occupational and Environmental Medicine). [Google Scholar]
- 8.The personal physician’s role in helping patients with medical conditions stay at work or return to work. American College of Occupational and Environmental Medicine. Position Statement. 2008 Dec 11; doi: 10.1097/JOM.0000000000001055. [DOI] [PubMed] [Google Scholar]
- 9.Williams CM, Henschke N, Maher CG, et al. Red flags to screen for vertebral fracture in patients presenting with low-back pain. Cochrane Database Syst Rev. 2013 Jan 31;1:CD008643. doi: 10.1002/14651858.CD008643.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Downie A, Williams C, Henschke N, et al. Red flags to screen for malignancy and fracture in patients with low back pain: systematic review. BMJ. 2013;347:f7095. doi: 10.1136/bmj.f7095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA, American Society of Interventional Pain Physicians Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. 2009;12:E35–70. [PubMed] [Google Scholar]
- 12.Downie A, Williams CM, Henschke N, et al. Red flags to screen for malignancy and fracture in patients with low back pain. Br J Sports Med. 2014;48:1518. doi: 10.1136/bjsports-2014-f7095rep. [DOI] [PubMed] [Google Scholar]
- 13.Talmage JB, Melhorn JM, Hyman M. When staying at work or returning to work is in the patients’ best interest. In: Talmage JB, Melhorn JM, Hyman M, editors. AMA Guides to the Evaluation of Work Ability and Return to Work. 2nd. Chicago, Ill: American Medical Association; 2011. pp. 1–7. [Google Scholar]
- 14.IAIABC Disability Management and Return to Work Committee. Return to Work: A Foundational Approach to Return to Function. Madison, Wis: International Association of Industrial Accident Boards and Commissions; Apr 19, 2016. [Google Scholar]
- 15.Hoffmann TC, Del Mar CB, Strong J, Mai J. Patients’ expectations of acute low back pain management: implications for evidence uptake. BMC Fam Pract. 2013;14:7. doi: 10.1186/1471-2296-14-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dictionary of Occupational Titles. Office of Administrative Law Judges Law Library. US Department of Labor; [Google Scholar]
- 17.Hazard RG, Haugh LD, Reid PT, Preble JB, MacDonald L. Early prediction of chronic disability after occupational low back injury. Spine. 1996;21:945–51. doi: 10.1097/00007632-199604150-00008. [DOI] [PubMed] [Google Scholar]
- 18.Savage RA, Whitehouse GH, Roberts N. The relationship between the magnetic resonance imaging appearance of the lumbar spine and low back pain, age and occupation in males. Eur Spine J. 1997;6:106–14. doi: 10.1007/BF01358742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Videman T, Battie MC, Gibbons LE, Maravilla K, Manninen H, Kaprio J. Associations between back pain history and lumbar MRI findings. Spine. 2003;28:582–8. doi: 10.1097/01.BRS.0000049905.44466.73. [DOI] [PubMed] [Google Scholar]
- 20.Borenstein DG, O’Mara JW, Jr, Boden SD, et al. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: a seven-year follow-up study. J Bone Joint Surg Am. 2001;83-A:1306–11. doi: 10.2106/00004623-200109000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Boos N, Rieder R, Schade V, Spratt KF, Semmer N, Aebi M. 1995 Volvo Award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine. 1995;20:2613–25. doi: 10.1097/00007632-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 22.Kleinstuck F, Dvorak J, Mannion AF. Are “structural abnormalities” on magnetic resonance imaging a contraindication to the successful conservative treatment of chronic nonspecific low back pain? Spine. 2006;31:2250–7. doi: 10.1097/01.brs.0000232802.95773.89. [DOI] [PubMed] [Google Scholar]
- 23.Modic MT, Obuchowski NA, Ross JS, et al. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology. 2005;237:597–604. doi: 10.1148/radiol.2372041509. [DOI] [PubMed] [Google Scholar]
- 24.Jarvik JJ, Hollingworth W, Heagerty P, Haynor DR, Deyo RA. The Longitudinal Assessment of Imaging and Disability of the Back (LAIDBack) Study: baseline data. Spine. 2001;26:1158–66. doi: 10.1097/00007632-200105150-00014. [DOI] [PubMed] [Google Scholar]
- 25.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- 26.Stadnik TW, Lee RR, Coen HL, Neirynck EC, Buisseret TS, Osteaux MJ. Annular tears and disk herniation: prevalence and contrast enhancement on MR images in the absence of low back pain or sciatica. Radiology. 1998;206:49–55. doi: 10.1148/radiology.206.1.9423651. [DOI] [PubMed] [Google Scholar]
- 27.Boos N, Semmer N, Elfering A, et al. Natural history of individuals with asymptomatic disc abnormalities in magnetic resonance imaging: predictors of low back pain-related medical consultation and work incapacity. Spine. 2000;25:1484–92. doi: 10.1097/00007632-200006150-00006. [DOI] [PubMed] [Google Scholar]
- 28.Haldeman S. Presidential address, North American Spine Society: failure of the pathology model to predict back pain. Spine. 1990;15:718–24. [PubMed] [Google Scholar]
- 29.Snook SH. Work-related low back pain: secondary intervention. J Electromyography Kinesiology. 2004;14:153–60. doi: 10.1016/j.jelekin.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 30.The Back Pain Revolution. 2nd. New York, NY: Churchill Livingston; 2004. Risk factors for back pain: environmental risk factors: physical; pp. 101–2. [Google Scholar]
- 31.van Tulder M, Koes B. Low back pain and sciatica. Clinical Evidence. 2000;4:614–31. [Google Scholar]
- 32.van Tulder M, Koes B. Low back pain (acute) Clinical Evidence Concise. 2006;16:474–7. [PubMed] [Google Scholar]
- 33.van Tulder M, Koes B. Clinical Evidence Handbook. London: BMJ Publishing Group; 2008. Low back pain (acute) pp. 386–8. [Google Scholar]
- 34.Hashemi L, Webster BS, Clancy EA. Trends in disability duration and cost of workers’ compensation low back pain claims (1988-1966) J Occup Environ Med. 1998;40:1110–9. doi: 10.1097/00043764-199812000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Shaw WS, Pransky G, Patterson W, Winters T. Early disability risk factors for low back pain assessed at outpatient occupational health clinics. Spine. 2005;30:572–80. doi: 10.1097/01.brs.0000154628.37515.ef. [DOI] [PubMed] [Google Scholar]
- 36.MDGuidelines. Denver CO: Reed Group; 2015. [Google Scholar]
- 37.Shiffman RN, Dixon J, Brandt C, et al. The GuideLine Implementability Appraisal (GLIA): development of an instrument to identify obstacles to guideline implementation. BMC Med Informatics Decision Making. 2005;5:23. doi: 10.1186/1472-6947-5-23. Available at: http://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-5-23. Accessed December 6, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pediatrics. Vol. 114. American Academy of Pediatrics Policy Statement: 2004. Classifying recommendations for clinical practice guidelines; pp. 874–7. Available at: http://pediatrics.aappublications.org/content/pediatrics/114/3/874.full.pdf. Accessed December 6, 2016. [DOI] [PubMed] [Google Scholar]
- 39.Ricci JA, Stewart WF, Chee E, Leotta C, Foley K, Hochberg MC. Back pain exacerbations and lost productive time costs in United States workers. Spine. 2006;31:3052–60. doi: 10.1097/01.brs.0000249521.61813.aa. [DOI] [PubMed] [Google Scholar]
- 40.Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(suppl 2):21–4. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 41.Waddell G, Burton AK. Is Work Good For Your Health and Well-Being? London, UK: Department of Work and Pensions, HM Government (The Stationery Office); 2006. [Google Scholar]
- 42.Roelfs DJ, Shor E, Davidson KW, Schwartz JE. Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med. 2011;72:840–54. doi: 10.1016/j.socscimed.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Australian and New Zealand Consensus Statement on Health Benefits of Work. Position Statement: Realising the Health Benefits of Work. 2014 [Google Scholar]
- 44.Merrill RN, Pransky G, Hathaway J, Scott D. Illness and the workplace: a study of physicians and employers. J Fam Pract. 1990;31(1):55–8. [PubMed] [Google Scholar]
- 45.Kapoor S, Shaw WS, Pransky G, Patterson W. Initial patient and clinician expectations of return to work after acute onset of work-related low back pain. J Occup Environ Med. 2006;48:1173–80. doi: 10.1097/01.jom.0000243401.22301.5e. [DOI] [PubMed] [Google Scholar]
- 46.Coste J, Lefrançois G, Guillemin F, Pouchot J, French Study Group for Quality of Life in Rheumatology Prognosis and quality of life in patients with acute low back pain: insights from a comprehensive inception cohort study. Arthritis Rheum. 2004;51:168–76. doi: 10.1002/art.20235. Available at: http://onlinelibrary.wiley.com/doi/10.1002/art.20235/pdf. Accessed December 6, 2016. [DOI] [PubMed] [Google Scholar]
- 47.Shaw W, Kristman VL, Vezina N. Workplace issues. In: Patrick Loisel JR, editor. Handbook of Work Disability. New York, NY: Springer Science+Business Media; 2013. pp. 163–82. [Google Scholar]
- 48.White M, Wagner S, Schultz IZ, Murray E, Bradley SM, Hsu V, et al. Modifiable workplace risk factors contributing to workplace absence across health conditions: a stakeholder-centered best-evidence synthesis of systematic reviews. Work (Reading, Mass) 2013;45:475–92. doi: 10.3233/WOR-131628. [DOI] [PubMed] [Google Scholar]
- 49.Feurestein M. Multidisciplinary approach to the prevention, evaluation and management of work-related disability. J Occup Rehabil. 1991;1:5–12. doi: 10.1007/BF01073276. [DOI] [PubMed] [Google Scholar]


