Abstract
Background
The role of nursing home (NH) information technology (IT) in quality improvement has not been clearly established, and its impacts on communication between care givers and patient outcomes in these settings deserve further attention.
Objectives
In this research, we describe a mixed method approach to explore communication strategies used by healthcare providers for resident skin risk in NH with high IT Sophistication (ITS).
Methods
Sample included NH participating in the statewide survey of ITS. We incorporated rigorous observation of 8- and 12-hour shifts, and focus groups to identify how NH IT and a range of synchronous and asynchronous tools are used. Social network analysis tools and qualitative analysis were used to analyze data and identify relationships between ITS dimensions and communication interactions between care providers.
Results
Two of the nine ITS dimensions (resident care-technological and administrative activities-technological) and Total ITS were significantly negatively correlated with number of unique interactions. As more processes in resident care and administrative activities are supported by technology, the lower the number of observed unique interactions. Additionally, four thematic areas emerged from staff focus groups that demonstrate how important IT is to resident care in these facilities including providing resident-centered care, teamwork and collaboration, maintaining safety and quality, and using standardized information resources.
Conclusion
Our findings in this study confirm prior research that as technology support (resident care and administrative activities) and overall ITS increases, observed interactions between staff members decrease. Conversations during staff interviews focused on how technology facilitated resident centered care through enhanced information sharing, greater virtual collaboration between team members, and improved care delivery. These results provide evidence for improving the design and implementation of IT in long term care systems to support communication and associated resident outcomes.
Keywords: Communication, Social network analysis, Nursing home, Information technology, Workflow
1. Introduction
For over a decade the Institute of Medicine has been addressing quality of care in healthcare organizations, including nursing homes (NH)[1, 2]. However, during this time, the role information technology (IT) plays in NH quality improvement has still not been clearly established, and its impacts on communication and resident outcomes deserve further attention. In this research, we describe a mixed method approach used to explore communication strategies for skin risk used by healthcare providers in NH with high IT Sophistication (ITS). We incorporated rigorous observational methods and used networking analysis tools to understand when and where skin risk communication interactions between nurses and nurse assistants occur in NH with greater IT adoption. We also used qualitative focus groups to identify how health IT and a range of synchronous and asynchronous tools are used to support risk assessment communication. Ultimately, if our understanding of communication and workflow in NH with high IT use can be improved, we can develop guidelines for IT design, implementation to increase utilization of these tools, and benchmarks for success to support resident outcomes in NH considering IT adoption or expansion.
1.1 Parent Studies
The specific aim and research questions for this study were developed from findings of several previous NH studies conducted in the Midwestern United States. These previous studies have been described in past manuscripts; however, they will be briefly reviewed here again.
The first study developed a survey tool to measure NH ITS using nine dimensions related to the functional, technological, and integration of NH IT [3]. Development of the IT sophistication variables and survey items was based on Nolan's Stage Theory drawn from prior work in manufacturing and acute care settings [4, 5]. Dimensions were defined as the types of NH activities supported by IT; including, the extent of use of IT, and how well IT is integrated with internal and external systems, respectively. Each of these three dimensions was explored in the activities related to resident care, clinical support, and administration with input from NH IT experts.
In the second study, the ITS tool was used in a statewide survey of Missouri NH to explicate total ITS measures in each of the nine domains [6]. A total of 199 facilities (41% response rate) participated in the second study. Participating facilities were stratified by ownership, bed size, and regional location. Homes were stratified into metro-urban-rural regions, based on population, using Beale codes to identify three county continuum codes (Cook & Mizer, 1989). Metro included total facilities with 250,000 people or more in central, fringe, and metro counties; urban status designation was given in counties with between 2,500 to 250,000 people that were adjacent and not adjacent to metro areas; finally, rural status was assigned to facilities in rural counties with less than 2,500 people. These variables were considered as total ITS was assessed across the state [7]. Results indicate that the functional ITS domain was related to NH bed size and location, while IT integration domain was associated with type of ownership.
During the third study, NH facilities participating in the statewide ITS survey were recruited to participate in a study to determine correlations between seven nationally reported NH quality measures related to skin care, and total ITS scores [8]. In this final study, we found statistically significant positive correlations between the percentage of residents with decline in activities of daily living and every ITS domain. We also found significant negative correlations between the percentage of residents with incontinence and ITS in the clinical support domain. We believe, increasing IT sophistication improves communication between clinicians and nonclinicians, such as NA, and this is the reason for the significant correlations between IT sophistication and quality. Although this study does not address the relationship between quality and IT sophistication, we believe increasing IT sophistication influences how interactions take place in clinical settings. These findings lead us to the current specific aim and research questions.
Specific Aim
Explore skin risk assessment communication strategies used in high IT nursing homes
Research Questions
What technologies or environmental tools are used to communicate skin risk during staff interactions in nursing homes with high ITS?
Do staff interactions about skin risk assessment differ within nursing homes with varying levels of high ITS?
2. Methods
2.1 Sample
The sample used in this research was selected from the NH participating in the statewide survey of ITS described previously. Following the statewide survey, total ITS scores were tabulated for each NH and a clustering procedure was used to evaluate distances between clusters of NH based on their score [9]. The clustering procedure was used to identify facilities with the highest ITS scores (5), medium ITS scores (6), and lowest ITS scores (5) among those participating in the statewide survey. Data from facilities with the highest ITS scores are included in this study. For this study, facility identification numbers (4, 6, 7, 8, and 9) were designated relative to the entire sample of 16 homes and their sequence of recruitment during the study (Table 1). All five NH had not-for-profit status. Four NH had a bed size of 60-120, one NH had >120 beds. Three NH were located in urban areas, one NH was located in a metropolitan area, and one NH was located rurally. Total ITS for the five NH ranged from 642 to 661 out of a total possible 900 ITS score [9]. Resident care had the highest ITS followed by clinical support and administrative activities.
Table I. Total Observation Times (NH × Shift).
| Facility 4 | Facility 6 | Facility 7 | Facility 8 | Facility 9 | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Ownership | Not for Profit | Not for Profit | Not for Profit | Not for Profit | Not for Profit | Total By Shift |
| Bedsize | 78 | 134 | 78 | 111 | 120 | |
| Location | Urban | Rural | Metro | Urban | Urban | |
|
| ||||||
| 8hr Day (min) | 598 | 286 | 320 | 509 | 64 | 1777 |
| 8hr Evening (min) | 264 | 494 | 686 | 333 | 144 | 1921 |
| 8hr Night (min) | 14 | 80 | 312 | 242 | 0 | 648 |
| 12hr Day (min) | 0 | 471 | 0 | 0 | 252 | 723 |
| 12hr Night (min) | 0 | 266 | 0 | 0 | 0 | 266 |
|
| ||||||
| Total Time (min) | 876 | 1597 | 1318 | 1084 | 460 | 5335 |
| Total Time (hrs) | 14.6 | 26.6 | 22.0 | 18.2 | 7.7 | 88.9 |
2.2 Observations and Coding
A structured observation field note guide was used to document communication strategies regarding pressure ulcer prevention practices that included four classifications: risk assessment, skin care, mechanical loading and support surfaces, and education. Using the field note guide we sought to complete a work design analysis that describes staff movements, actions, gestures, and phrases associated with direct care staff, as well as communication strategies that relay the preventive skin-care needs of residents. Field notes included: (1) contextual information about the time, place, and direct-care staff involved in the observation, (2) objective descriptions of observed events and conversations, (3) information about actions, dialogue, and context. Study staff were instructed to be sensitive to both verbal and nonverbal cues, which would indicate particular nursing home staff were not wanting to participate in answering questions or being observed as they work, to reduce intrusiveness. The use of this observation field note guide, procedures, and coding methods included measures of inter-observer agreement and inter-rater reliability. These methods are described in related case study research, including two facilities with extreme ranges (High and Low) of NH ITS [10]. We will provide a brief overview of methods used for the current research.
For the current study, we included only documented observations and coding from the five NHs clustered together and designated as high ITS. Only observations documented by research staff in the risk assessment classification are included. Observations at each facility began with introductions of research and administrative staff, facility tours, and an overview of the project conducted by the principal investigator. Two research team members conducted all observations in tandem, including a PhD prepared RN with expertise in gerontology and informatics, and a research assistant with a healthcare background. Observations were documented of RN/LPN and CNA personnel who were working together as a team on a nursing unit. The research team worked with administrators to select nursing units and staff responsible for areas where residents at high risk of skin breakdown were located. Total observation time for two observers was tallied based on 8- and 12- hour shifts and is provided for each NH in Table I. Observed interactions were made on three 8-hour shifts (8hr day, 8hr evening, and 8hr night) and two 12-hour shifts (12hr day and 12hr night). Not all nursing homes had all types of shifts, for example, Facility 4 only had 8 hour shifts and Facility 6 had a combination of 8 and 12 hour shifts. The shifts that existed are shown in Table II. Shifts that did not exist in NHs were not part of the scheduling design and are represented as “-” in Table II. During observations, inter-observer agreement was assessed periodically to prevent observer drift, maintaining a consistent 90% index of agreement between the two research staff conducting observations. The same two observers conducted all observations in all facilities to maintain consistency.
Table II. Total Interactions (Unique Interactions) per hour by shift.
| Facility 4 | Facility 6 | Facility 7 | Facility 8 | Facility 9 | |
|---|---|---|---|---|---|
| 8hr Day | 46 (11) | 42(14) | 54(13) | 68(13) | 79(18) |
| 8hr Evening | 43 (8) | 34(11) | 45(11) | 51(16) | 71(18) |
| 8hr Night | 176 (13) | 65(9) | 61(17) | 62(18) | - |
| 12hr Day | - | 43(7) | - | - | 73(18) |
| 12hr Night | - | 40(17) | - | - | - |
Following the observations, data were coded using recommended evidence-based pressure ulcer prevention treatment guidelines that were used to develop the field note guide [11]. Researchers drafted a set of coding rules used by coders to maintain consistent coding procedures. Inter-rater agreement between coders was established using a sample of coded observations (n=220). Two way McNemar's tests were evaluated to determine consistency of coding and disagreements were reviewed until a consensus was reached by coders.
2.3 Communication network analysis
Once the observations were coded, communication network analysis was used to quantitatively study and create visual representations of the interactions among providers. Communication network analysis was performed using a social networking software called ORA aka ORA-NetScenes (Carnegie Mellon University and Netanomics) [12, 13]. ORA has been used in the past to study organizational risk, terrorist networks, and business and economies. ORA has also been used to study communication and acute patient care hand-offs originating in emergency departments [14-17] and in the assessment of public health activity [18-20]. To our knowledge, software analytics like these have not been used in NH. In this study, we used ORA software to assess interactions between nursing staff (LPN/RN and CNA) regarding pressure ulcer risk communication and the locations where communication occurred. We further explored how interactions varied during different shifts.
Observational data was used to compute frequency of unique interactions between agents in locations by shift for each NH. This data was then imported into ORA for communication network visualization and for computation of the network measures. For computation purposes, information from the observations including initiator, recipient, and location of the interactions were represented as nodes and links. These interactions were used to connect nodes representing agents (initiator and recipient) involved in an interaction in a specific location. Individual network analysis measures were computed for the different shifts in each of the five NH. Measures pertaining to the overall network, initiator-recipient network and initiator-location network were calculated.
To answer research questions, we selected two node-level centrality measures that together provide a concise and sufficient perspective of the providers that are critical to communication [21]. Centrality measures the extent to which a node has a critical position in a network where all nodes are of the same type. There are various centrality measures such as degree, betweenness, closeness, etc. We used degree centrality and betweenness centrality since these measures will help us understand which nodes occupy a strategic position in a network [22, 23]. Degree centrality is the number of links to and from a node. Betweenness centrality is the frequency with which a node lies on the shortest path connecting all other pairs of nodes in the network. Nodes that are high in both betweenness and degree centrality are important because of their central location, ability to connect agents, and ability to act as conduits for information transfer. Nodes that are high in betweenness but low in degree centrality are important as they are connecting disconnected groups. Nodes that are low in betweenness but high in degree centrality are important as they are either sources or basins of information. To be able to compare across networks, degree centrality and betweenness centrality were scaled prior to comparison.
2.4 Focus Groups
Focus groups on each of three shifts (day, evening, night) were conducted at each of the five NH. All nursing staff available at the time researchers were present were recruited to participate. Researchers spent a minimum of 2 days at each site to recruit as many staff as possible to participate in the groups. Each focus group included 3-6 participants. To minimize reactivity between different disciplines (RN/LPN and CNA), the goal was to keep focus groups homogenous in relation to the type of staff participating in the specific group
To maintain consistency, focus groups were conducted by reading verbatim predetermined questions from a structured questionnaire for NH staff. The same researcher conducted all focus groups (GA). Pause and probe methods were utilized to clarify points as staff discussed communication strategies [24]. All focus groups were recorded with a handheld digital recorder. A research assistant documented field notes during the focus groups to capture other anecdotal evidence that would not be captured on digital recordings, such as posture and facial expressions.
Transcribed recordings of each focus group were downloaded into a qualitative software package, NVIVO 10.0 for analysis. Thematic areas emerging from the coded data were collected in a series of nodes in NVIVO created by coders. In NVIVO, qualitative references coded into nodes are tabulated and can be searched after coding for similarities and differences in underlying statements. Coding continues until data saturation is reached, that is the point when no new information emerges from the captured dialogue [25]. These qualitative references provide the detailed descriptions that help to describe current communication strategies used by staff to maximize pressure ulcer prevention measures. Qualitative references also provide details that help explain assumptions made from network observations.
3. Results
3.1 Observation time, interactions and centrality measures
The total observation times for each facility are illustrated in Table I. The amount of observation time is reported according to the types of shifts across all facilities. Researchers spent a total of 88.9 hours of observation time including all shifts in these five facilities. There were similar amounts of total time spent observing staff on the 8hr day and 8hr evening shifts, approximately 29∼32 hours each. There were nearly 11 hours of total time observing 8hr night shift staff in all five facilities. The longest observational time was 11.4 hours during the 8hr evening shift in Facility 7. There were no observations made on the 8hr night shift in Facility 9, 12hr day shifts were present and observed in Facility 6 and Facility 9 and 12hr night shifts in Facility 6 (Table I).
Both total number of interactions and unique interactions were studied. Unique interactions are those between a unique initiator and a unique recipient. Since the observation times varied across the facilities and the shifts, total and unique interactions were normalized using the observation time. The normalized number of interactions observed during each of the shifts in the five NH is illustrated in Table II. Facility 6 had the least number of total interactions during both 8hr day and 8hr evening shifts (42 per hour and 34 per hour, respectively). After normalization, Facility 4 had the highest frequency of total interactions (176 per hour) on the 8 hour night shift; however, these observations occurred during the shift report when many interactions were taking place during rounds. Facility 9 had the next highest frequency on the 8 hour day shift (79 per hour). When frequencies of unique interactions were studied, Facility 4 had the least amount for both 8hr day and evening shifts (11 per hour and 8 per hour). Facility 8 and 9 had equivalent amounts of unique interactions (18 per hour) on 8 hour night shift and 8 hour day, evening, and 12 hour day shift, respectively. The interactions observed were tabulated and used to construct networks using ORA software. Total degree centrality and betweenness centrality measures were computed for care providers (CNA, RN, LPN and Wound Nurse) for each shift in each nursing home, see Table III. The networks and the measures are discussed in detail after correlations were computed.
Table III. Total Degree and Betweenness Centrality (Agent × Agent) Measures by Shift.
| Total Degree Centrality | |||||
|---|---|---|---|---|---|
| Facility | Shift | C N A | RN | LPN | Wound Nurse |
| 4 | 8 hr morning | 0.045 | 0.004 | 0.011 | 0.009 |
| 8 hr evening | 0.023 | 0.019 | - | 0.084 | |
| 8 hr night | 0.012 | - | 0.200 | - | |
|
| |||||
| 6 | 8 hr morning | 0.085 | 0.002 | - | - |
| 8 hr evening | 0.080 | 0.011 | - | - | |
| 8 hr night | 0.170 | 0.006 | - | - | |
| 12 hr day | 0.023 | 0.049 | 0.009 | 0.106 | |
| 12 hr night | - | 0.017 | 0.076 | 0.044 | |
|
| |||||
| 7 | 8 hr morning | 0.059 | 0.004 | 0.015 | - |
| 8 hr evening | 0.035 | 0.006 | 0.018 | - | |
| 8 hr night | 0.164 | 0.061 | - | - | |
|
| |||||
| 8 | 8 hr morning | 0.023 | 0.015 | - | 0.007 |
| 8 hr evening | 0.078 | 0.029 | 0.041 | - | |
| 8 hr night | 0.092 | 0.002 | 0.097 | 0.005 | |
|
| |||||
| 9 | 8 hr morning | 0.181 | 0.025 | - | - |
| 8 hr evening | 0.090 | 0.005 | - | - | |
| 12 hr day | 0.162 | - | 0.150 | - | |
|
| |||||
| Betweeness Centrality | |||||
| Facility | Shift | C N A | RN | LPN | Wound Nurse |
|
| |||||
| 4 | 8 hr morning | 0.174 | 0.083 | 0.038 | 0.000 |
| 8 hr evening | 0.000 | 0.018 | - | 0.214 | |
| 8 hr night | 0.000 | - | 0.000 | - | |
|
| |||||
| 6 | 8 hr morning | 0.033 | 0.000 | - | - |
| 8 hr evening | 0.000 | 0.000 | - | - | |
| 8 hr night | 0.000 | 0.167 | - | - | |
| 12 hr day | 0.000 | 0.200 | 0.100 | 0.000 | |
| 12 hr night | - | 0.000 | 0.000 | 0.024 | |
|
| |||||
| 7 | 8 hr morning | 0.083 | 0.028 | 0.056 | - |
| 8 hr evening | 0.000 | 0.019 | 0.000 | - | |
| 8 hr night | 0.250 | 0.167 | - | - | |
|
| |||||
| 8 | 8 hr morning | 0.051 | 0.128 | - | 0.013 |
| 8 hr evening | 0.000 | 0.000 | 0.310 | - | |
| 8 hr night | 0.033 | 0.000 | 0.000 | 0.000 | |
|
| |||||
| 9 | 8 hr morning | 0.000 | 0.000 | - | - |
| 8 hr evening | 0.167 | 0.000 | - | - | |
| 12 hr day | 0.250 | - | 0.333 | - | |
3.2 Correlations between total (unique) interactions and centrality measures against ITS
Correlations were computed for both the number of interactions (total and unique) and the centrality measures against the nine dimensions of ITS measures for the five high IT NHs. Two of the nine ITS dimensions (resident care-technological, and administrative activities-technological) were significantly negatively correlated at the 95% confidence level with number of unique interactions (Table IV). Total ITS was significantly negatively correlated at the 99% confidence level with the number of unique interactions. The same ITS dimensions (resident care-technological, administrative activities-technological and total ITS) were significantly negatively correlated with CNA total degree and LPN betweenness centrality measures. In addition, administrative activities-integration was also correlated with CNA total degree centrality. These correlations indicate as more processes in resident care and administrative activities are supported by technology, the lower the number of observed unique interactions between staff in these NH. Similarly, among the high IT homes, the higher the total IT sophistication of a nursing home, the lower the number of unique staff interactions in these homes.
Table IV. Correlations for IT Sophistication by Observed Interactions.
| IT Sophistication Domain and Dimension | Total Interactions | Unique Interactions | C N A Total Degree Centrality | LPN Between Centrality | |
|---|---|---|---|---|---|
| Resident Care | Functional | -0.418 | -0.336 | 0.085 | -0.382 |
| Technological | -0.184 | *-0.573 | *-0.528 | *-0.673 | |
| Integration | - | - | - | - | |
|
| |||||
| Clinical Support | Functional | 0.121 | -0.158 | 0.103 | 0.011 |
| Technological | - | - | - | - | |
| Integration | - | - | - | - | |
|
| |||||
| Administrative Activities | Functional | - | - | - | - |
| Technological | 0.184 | *-0.573 | *-0.528 | *-0.673 | |
| Integration | 0.001 | *-0.397 | *-0.572 | -0.536 | |
|
| |||||
| Total IT Sophistication | -0.163 | **-0.656 | *-0.531 | *-0.739 | |
p<.05
p<.01
3.3 Network Analysis
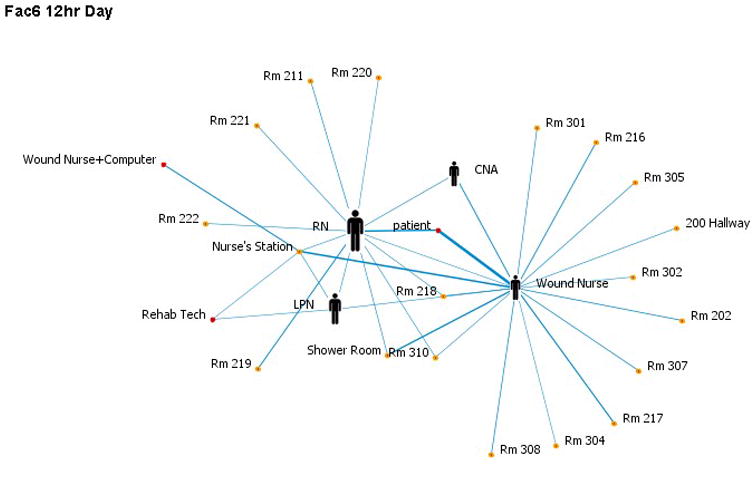
When studying the interactions visually (networks obtained from ORA), different patterns between nursing homes with varying levels of ITS and among various shifts were observed (Figure 1a-c). In the figures, a node represents a human involved in an interaction or a location where the interaction occurred. Patient is represented using a circle and are identified separately from patient rooms, because some patient interactions occur in other locations. A person icon was used to identify key care providers of interest (RN, CNA, LPN, Wound Nurse). A link represents an interaction between at least two humans (patient, key care provider of interest or others) in a given location. We have recreated the figures so that the width of the links (line thickness) is proportional to the frequency of the interactions. Additionally, the person icons were sized by betweenness to indicate the extent to which identified providers have power in controlling the flow of information. For instance, in one of the facilities with the highest ITS (Facility 4) during the 8 hour day shift (figure 1a), CNAs were primarily involved in interactions in or near resident rooms with residents, RNs and LPNs. They had no interactions with administrators or other care providers such as a wound nurse. The interaction patterns tend to show two almost separate networks, one centered around CNAs and the other around the wound nurse. CNAs' interactions outside direct-resident care took place only through LPNs. However, CNAs had the highest total degree centrality as well as betweenness centrality of 0.045 and 0.174 respectively. In comparison, RNs and LPNs had only total degree centrality of 0.004 and 0.011 respectively, and betweenness centrality of 0.083 and 0.038 respectively (Table III). Thus, the CNAs were highest in both total degree and betweenness, and hence are central to the network connecting otherwise disconnected providers and serving as good conduits for information transfer. In other words, CNAs are central to connecting networks and passing on information to clinical RN/LPNs, but not to specialist nurses, such as the wound care nurse.
Figure 1.
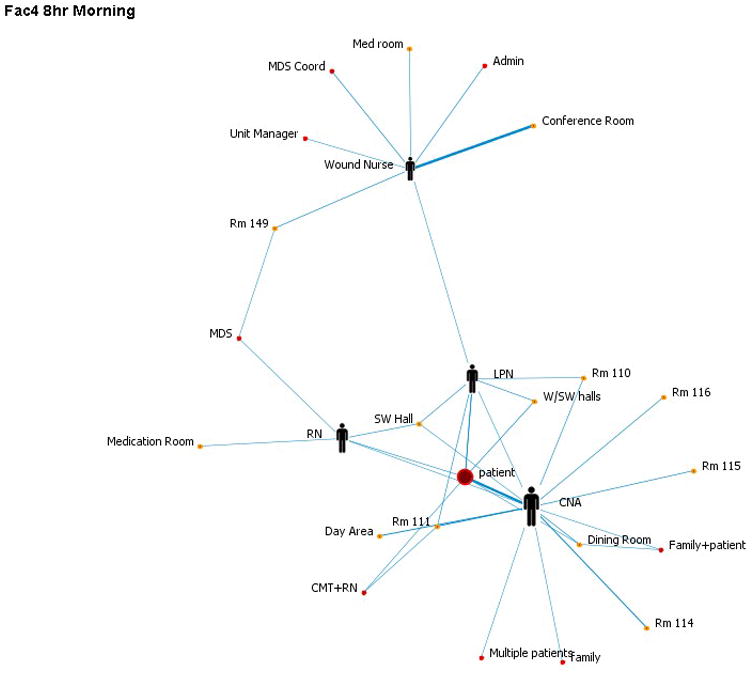
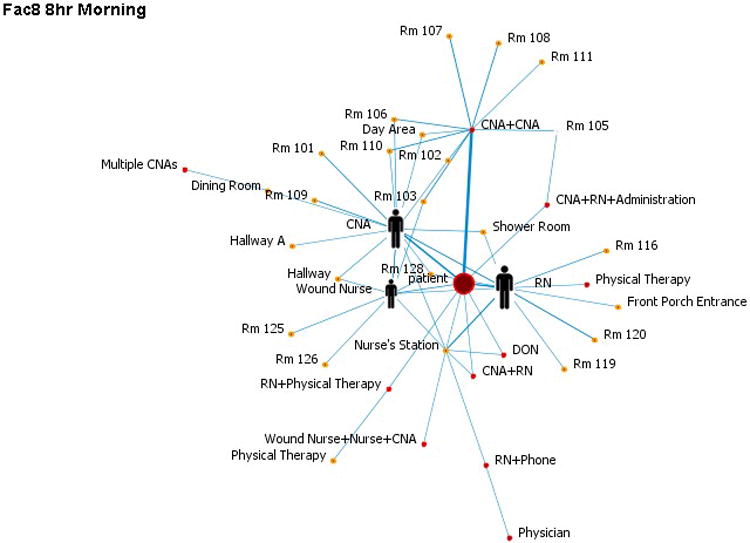
On the contrary, one of the facilities with the second lowest total ITS (Facility 8) when visually represented has only one large network inclusive of all providers (figure 1b). Here there were no LPNs in the 8hr day shift. Furthermore, CNAs were not central to the interactions. Specifically, the total degree centrality for CNAs was only 0.023, and betweenness centrality was only 0.051, and comparatively for RNs was 0.015 and 0.128 respectively. Thus, CNAs did not have a similar strategic position in the communication network.
While comparing 8-hour day shift interactions against those during 12-hour day shifts in one of the facilities with the highest total ITS (Facility 6, figure 1c), 12-hour day shifts had fewer CNA interactions and they were more peripheral. RNs, LPNs and wound nurses were central to interactions. Specifically, CNAs had a betweenness centrality of close to zero compared to RNs with 0.2 and LPNs with 0.1. This theme emerged across both day and night shifts (in fact, with no CNA interactions during the 12hr night shift). It was also noted that Facility 6 had the highest levels of resident care-technological, administrative activities-technological and second highest level of administrative activities-integration ITS.
On the other hand, CNA interactions during the 12hr day shift were quite the opposite in Facility 9 with the lowest levels of resident care-technological, administrative activities-technological, administrative activities-integration and total ITS. In this case, the 12hr day shift had a lot of CNA interactions. This is also further emphasized in that CNAs had higher total degree and betweenness centrality values of 0.162 and 0.250 respectively.
3.4 Focus Groups
A total of 35 focus groups with 137 staff were conducted in the five high IT nursing homes. Using NVIVO, four thematic areas emerged from the focus groups that demonstrate how important IT is in relation to communication strategies about skin risk in these facilities. Emerging themes included providing resident-centered care, teamwork and collaboration, maintaining safety and quality, and using standardized information resources. Direct quotes are used to demonstrate how staff described these important concepts.
3.4.1 Providing resident-centered care
In this sample of NH, high ITS facilitated workflows that promoted resident centered care. Technology-centered resident care is not resident-centered care [26], but technology can enhance resident centered care that empowers people with information to make decisions at the point of clinical encounters. Examples of this phenomenon were discussed in various comments made by staff members, (“All information is in the computer,” “The nurses have the computer right outside the door. They don't have to run back and look for a paper chart. Saves time.”), The result of having technology in close proximity influences resident centered care by improving care delivery through better access to documentation, timely communication, and reporting. Through their IT systems, personnel and providers are able to access the resident's record remotely, including the ability to access diagnostic study reports. Staff described how increased access improves decision making by all. For example, leadership (“The DON, Unit Managers, and Charge Nurse on call has access at home at all times”), providers/physicians (“All the physicians that have residents at this facility have access to their medical records”), and support positions such as rehab and dietary (“The level of access is specific to each user/department,” “If you go into the EMR, they can see everything that has been documented”).
Initial support of IT systems by nursing, including leadership, during implementation was lacking due to perceptions that “it took staff away from resident care” and leadership did not want to see “staff sitting behind the desk working on a computer and ignoring resident care.” These perceptions influenced IT implementation decisions to put people and IT nearer to resident care areas. As nursing and leadership have become more comfortable with technology perceptions have changed. Staff indicated that IT “helps the quality of care, because staff can still get out on the floor and take care of residents.”
These high ITS NH have a great deal of integration that supports resident centered care. In particular, all the NH in this study are interoperable with an acute care facility, including lab results with alerts/critical value notification, utilization of e-mail, and sending comments/requests to providers. This level of ITS integration provides more effective communication between staff, (“If you bring up a communication form, then you are just writing a note to the physician,” “They can choose to send a communication form to the physician, which includes a subject line, and who it is going to”). These systems provide a level of accountability that paper systems cannot provide.
3.4.2 Teamwork and collaboration
The use of NH IT has been reported to improve teamwork and collaboration between physicians, licensed staff, and certified staff [27]. For these NH facilities, the IT system was supported by their parent organization, a locally owned tertiary care facility, providing acute, home-based, and long-term care. Descriptions of the organizational structure illustrate how integrated direct care staff was in IT implementation, (“A former director of nursing moved into an IT specialist role and he and another employee (who used to be a staffing coordinator, Med Tech, and CNA) helped build the software to meet the functions…”). More evidence of how this level of integration improved teamwork and collaboration was discovered in statements about how email was used to facilitate communication about skin risk assessment, (“The e-mail is set-up in groups so e-mail can be sent to just RNs, or just CNAs, or housekeeping, or individuals,” “accessible on the home computers; this is seen as a benefit,” “The night nurses especially use e-mail to communicate with the DON.”).
Although, the high tech NH had a high level of IT integration, nursing staff still relied on the printing of reports or work/task lists and sometimes documented in the computer at the end of their shift. Descriptions of this workflow included: (“They have ‘cheat sheets’ with the information on their ‘to do that day’ and reconcile it with the computer,” “they have ‘cheat sheets’ which indicates who has wounds, who needs breathing treatments, Accu-Cheks, and other miscellaneous information to help them get organized with the work needed”). These workflows included documenting information that was verbally relayed to the nurse or through paper checklists utilized by the CNA to communicate to the nurse about care provided to residents during the shift. Direct documentation in the computer by CNAs, although available, was limited to electronic task lists and status boards that were monitored by nurses. Even though electronic sources were available, some CNAs still relied on paper checklists or notes, (“There is a mini-care plan (cheat sheet) in the resident closets,” “the CNAs have a form to fill out to report anything wrong with the resident and gives [the report] to the Charge Nurse or Treatment Nurse,” “the CNAs don’t really work very much with the information system.” “The Administrator feels strongly that CNAs are not to be sitting in front of a computer for long periods of time. She wants them free to take care of the residents.…the responsibility is on the nurses to document the ADLs and have the CNAs take care of the residents”).
In addition to the use of electronic e-mail or documentation in the IT system, staff frequently passed information to each other through floor conferences, huddles, all staff meetings, and shift reports. During these verbal exchanges of information, staff were provided information regarding resident satisfaction results, wound reports, quality/safety reports, and resident care issues. Descriptions of these communication strategies include, (“We do huddles of 5 min or less on every shift,” “Once a month they have an all staff meeting on the first payday of each month,” “the DON has monthly nursing staff meetings,” “families are included in staff meetings.”).
3.4.3 Maintaining safety and quality
In these high technology facilities, licensed nurses seemed to be the most frequent users of the IT system; however, all staff relied on different components for communication including clinical alerts, task lists, electronic Medication Administration Record (eMAR), standardized documentation fields, standardized protocols tied to the electronic record, standardized reports, and interdisciplinary communication to monitor and improve the safety and quality of resident care. Using these resources staff had the opportunity to monitor care delivery more closely. For example, (“If the staff does not do the intervention within the time frame allotted, the computer will show it as a ‘pink box (meaning it's not done)”; “Each facility has someone do a once a weekly vigil and documentation of any pressure ulcers. That report goes to the Director of Nursing, Administrator, Chief Executive Officer, Dietician, Medical Director, Quality Improvement Department, and several others to oversee it”; “We compare ourselves to the National and State averages as well as to the other facilities. If there is something that we are out of range on, it will be reviewed to see what we can do to improve the scores.”).
3.4.4 Using standardized information resources
One of the advantages of using an IT system is standardized wound care and treatment protocols that can enhance skin risk assessment. These facilities are working with physicians to implement best practice guidelines into the IT for instance a plastic surgeon who is a specialist in wounds. These standards include the (“weekly assessment and documentation of progress, monthly detailed assessment and photos scanned in” and the use of pressure ulcer preventions, including “repositioning every 2 hours, turning,”“ keeping clean and dry, applying barrier creams, nutrition, and cushions.” If an intervention or order deviates from the standard “they are asked by the computer if they deviate from standard – ‘are you sure you want to change it?’ This is a safety check system.”)
Staff receives alerts through the status board, task lists, care plans, and standardized documentation fields in the IT system. With standardized documentation fields, (“nurses use canned text, but will individualize the resident care plan; always tailored to the resident along with canned text.” This information is displayed “on the status board, (where) there is a function in the intervention list called ‘treatment status,’ and it can be customized in regards to wounds and treatment.”) This status board “is like a ‘home page’ providing access to other areas of the chart, alerts, tasks, and hot links to other areas of the chart for quick reference.
4. Discussion
We have conducted extensive pilot work looking at the relationship between ITS in our statewide sample and quality measures. The multiple findings supporting one another in these studies using different methodologies provides convergence of our results with greater validity of findings. In preliminary work, we found in NH with higher ITS and more robust communication through IT versus less robust low ITS NH, there were fewer interactions in locations where NH staff typically congregate. For example, in low ITS NH, interactions were primarily located around central nursing stations and the NH with higher ITS had interactions more proximal to the point of resident care, down hallways where resident rooms were located [10]. Our findings in this study are similar in that, as IT in resident care and administrative processes increases, unique interactions between staff members decrease. Staff who were interviewed discussed how technology use facilitated resident centered care through enhanced information sharing, greater virtual collaboration between team members, and improved care delivery.
We know from our previous research in Missouri NHs that diverse IT adoption measures are significantly correlated with change in quality measures [8]. We found that increasing NH IT adoption significantly correlated with quality measures for residents' with declining activities of daily living and residents experiencing increased incontinence [8]. For instance, IT adoption in Clinical Support processes that included computerized laboratory results reporting were associated with improved incontinence quality measures. This possibly shows that with higher ITS (clinical support-functional) RNs are able to take on a more central role in care delivery because of better access to information. This is intuitive since clinical support technologies include electronic laboratory reporting systems and radiology reporting systems that RNs would need to access in order to manage treatment regimens and to monitor for condition changes. We did not find similar results in this study as interactions and centrality measures did not appear to be significantly related to clinical support ITS dimensions. In other results, we also found as IT adoption increased in Resident Care, residents experiencing a decline in daily living activities increased. Our research findings illustrate that NHs with greater IT adoption have more robust communication technologies integrated into their environment; therefore, our assumption is that staff are able to communicate about episodes of decline earlier, more frequently, with less face to face interactions [10]. We have upheld this assumption through this work that fewer unique interactions are associated as total ITS in resident care and administrative activities increases.
There are mixed results about how technology impacts staff interactions and outcomes. For example, in a survey of communication in a South Carolina NH staff expressed a preference for synchronous (face to face) communication compared to asynchronous methods and rated synchronous communication as leading to better communication quality. Staff also reported utilizing asynchronous tools more frequently to receive information compared to giving or reporting information to another staff member, which again they preferred to do face to face. However, synchronous communication has been associated with increased interruptions, disruptions to workflow and thus, may have implications for performance and errors [28]. These staff perceptions about the “quality” of interactions or information exchange using face to face mechanisms compared to IT is important given the findings of the current study. Even if higher ITS leads to decreased direct interactions between staff, we need to ensure that the quality of information exchange still meets the needs of staff and residents. In some cases face to face communication is still preferred and optimal and this should be considered in the design and implementation of ITS in NH. Studies linking the effects of these types of proximal and distal clinical workflows in NH to IT adoption have not been conducted to our knowledge. In the future, we plan to extend this work to understand proximal (face to face interactions) and distal workflow (skin care performance) measures needed to describe more fully how health IT affects workflow and quality of care.
5. Conclusions
The role of IT in NH care deserves greater attention than it has received during the past few years. These settings are increasingly accountable to a diverse set of patient safety goals and outcomes, such as increased emphasis on the prevention of infections, falls, and pressure ulcers [29]. These outcomes, coupled with a changing resident population, are placing increased demands on nurses and other healthcare providers, including increasingly complex care, critical decisions, coordination, teamwork and increased utilization of IT [30]. Greater understanding about how IT influences workflow and reduces demands on nursing staff will lead to better quality of care for NH residents.
10. Summary points.
What is known before the study
Information technology can be a useful tool to manage the complex needs of chronically ill elderly residents in nursing homes.
The role of information technology in NH quality improvement has not been clearly established.
Impacts of information technology on communication between care givers and resident outcomes in NH settings deserve further attention.
What the study has added to the body of knowledge
Increasing IT sophistication influences multidisciplinary communication and numbers of interactions between healthcare providers.
Staff interactions are influenced mostly by increasing NH IT adoption in resident care and administrative activities.
Healthcare providers indicate increasing IT sophistication has a role in quality improvement, resident centered care, safety, teamwork/collaboration, and standardization.
Acknowledgments
This project was supported by grant number K08HS016862 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the author and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
6. Authors Contributions: GA conceptualized study design, conducted data collection, performed data analysis, and drafted manuscript; KP conceptualized design, performed data analysis, and drafted manuscript; LS conceptualized design, performed data analysis, and drafted manuscript; BS assisted with coding methodologies, conducted data analysis and drafted manuscript; KC assisted with study design by consulting on analytic methodologies using ORA software, data analysis interpretations, and manuscript drafts.
7. Conflicts of Interest: The authors declare that they have no conflicts of interest in the research
9. Protection of Human and Animal Subjects: The study was reviewed and approved by the University of Missouri's Institutional Review Board before the study began.
Contributor Information
Gregory L. Alexander, University of Missouri, Sinclair School of Nursing, Phone: 573-882-9346.
Kalyan S. Pasupathy, Patient-Centered Research, Aurora Research Institute, 960 N. 12th St., Suite 4120, Milwaukee, WI 53233, Phone (414) 219-5371.
Linsey M. Steege, School of Nursing, University of Wisconsin – Madison, 600 Highland Avenue, K6/362 CSC, Madison, WI 53792-2455, Phone: 608-263-5191.
E. Bradley Strecker, Sinclair School of Nursing, University of Missouri – Columbia, Cell: 816-392-2933.
Kathleen M. Carley, Institute for Software Research, Office: Wean Hall 5130, Pittsburgh, PA 15213, Tel: (412) 268-6016, Fax: (412) 268-1744.
Reference List
- 1.Kohn L, Corrigan J, Donaldson M. To Err is Human. Washington DC: National Academies Press; 1999. [PubMed] [Google Scholar]
- 2.Wunderlich GS, Kohler PO, editors. Institute of Medicine. Improving the Quality of Long Term Care. Washington DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 3.Alexander GL, Wakefield DS. IT sophistication in nursing homes. Journal of the American Medical Directors Association. 2009;10:398–407. doi: 10.1016/j.jamda.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nolan RL. Managing the computer resource: A stage hypothesis. Communications of the ACM. 1973;16:399–405. [Google Scholar]
- 5.Pare G, Sicotte C. Information technology sophistication in health care: An instrument validation study among Canadian hospitals. International Journal of Medical Informatics. 2001;63:205–223. doi: 10.1016/s1386-5056(01)00178-2. [DOI] [PubMed] [Google Scholar]
- 6.Alexander GL, Madsen R, Wakefield DS. A Regional Assessment of Information Technology Sophistication in Missouri Nursing Homes. Policy, Politics & Nursing Practice. 2010;11:214–225. doi: 10.1177/1527154410386616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alexander GL, Madsen D, Herrick S, Russell B. In: Measuring IT sophistication in nursing homes. Kerm Henriksen PJBBPMAKMMLGB, editor. Rockville Maryland: AHRQ; 2008. pp. 91–105. AHRQ Publication No. 08-0034-CD edition. [PubMed] [Google Scholar]
- 8.Alexander GL, Madsen R. IT sophistication and quality measures in nursing homes. Journal of Gerontological Nursing. 2009;35:22–27. doi: 10.3928/00989134-20090527-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Communication strategies used by nursing assistants in nursing homes with diverse IT sophistication. 2014 [Google Scholar]
- 10.Case studies of IT sophistication in nursing homes: A mixed method approach to examine communication strategies about pressure ulcer prevention practices. International Journal of Industrial Ergonomics. in press. [Google Scholar]
- 11.Agency for Healthcare Research and Quality ((AHRQ) formerly AHCPR) Treatment of Pressure Ulcers. Silver Springs, Maryland: AHCPR Publishing Clearinghouse; 1994. Report No.13: Publication No.: 95-0652 edition. [Google Scholar]
- 12.Carley KM, Reminga J, Storrick J, Pfeffer J, Columbus D. ORA User's guide 2013. CMU-ISR-13-108. Carnegie Mellon University, School of Computer Science: Institute for Software Research; 2013. [Google Scholar]
- 13.Carley KM, Pfeffer J. Dynamic Network Analysis (DNA) and ORA. In: Schmorrow DD, Nicholson DM, editors. Advances in Design for Cross-Cultural Activities Part I. CRC Press; 2012. pp. 265–274. [Google Scholar]
- 14.Effken JA, Carley KM, Gephart S, Verran JA, Bianchi D, Reminga J, Brewer BB. Using ORA to explore the relationship of nursing unit communication to patient safety and quality outcomes. International Journal of Medical Informatics. 2011;80:507–517. doi: 10.1016/j.ijmedinf.2011.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Effken JA, Carley KM, Lee J, Brewer BB, Verran JA. Simulating nursing unit performance with OrgAhead. Computers Informatics Nursing. 2012;30:620–626. doi: 10.1097/NXN.0b013e318261f1bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Benham-Hutchins MM, Effken JA. Multi-professional patterns and methods of communication during patient handoffs. International Journal of Medical Informatics. 2010;79:252–267. doi: 10.1016/j.ijmedinf.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Effken JA, Gephart SM, Brewer BB, Carley KM. Using ORA, a network analysis tool, to assess the relationship of handoffs to quality and safety outcomes. Computers Informatics Nursing. 2013;31:36–44. doi: 10.1097/NXN.0b013e3182701082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merrill JA, Carley KM, Orr MG, Jeon CY, Storrick J. Topology of local health officials' advice networks: Mind the gaps. Journal of Public Health Management Practice. 2012;18:602–608. doi: 10.1097/PHH.0b013e31825d20ac. [DOI] [PubMed] [Google Scholar]
- 19.Merrill JA, Carley KM, Orr MG, Jeon CY, Storrick J. Patterns of interaction among local public health officials and the adoption of recommended practices. Frontiers in Public Health Services and Systems Research. 2012;1 [Google Scholar]
- 20.Merrill JA, Keeling JW, Carley KM. A comparative study of 11 local health department organizational networks. Journal of Public Health Management Practice. 2010;16:564–576. doi: 10.1097/PHH.0b013e3181e31cee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Valente T. Social Networks and Health: Models, Methods, and Applications. New York: Oxford University Press; 2010. [Google Scholar]
- 22.Borgatti SP. Centrality and network flow. Social Networks. 2005;27:55–71. [Google Scholar]
- 23.Freeman LC. Centrality in social networks conceptual clarification. Social Networks. 1978;1:215–239. [Google Scholar]
- 24.Krueger RA. Focus Groups: A Practical Guide for Applied Research. 2nd edition. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 25.Barroso J. In Nursing Research 7th edition Edited by LoBiondo-Wood G, Haber J. St. Louis: Mosby; 2010. Qualitative Approaches to Research; pp. 101–125. [Google Scholar]
- 26.Stewart M. Towards a global definition of patient centred care. BMJ. 2001;322:444–445. doi: 10.1136/bmj.322.7284.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Institute of Medicine. Key capabilities of an electronic health record system. National Academies Press; Washington DC: 2003. [PubMed] [Google Scholar]
- 28.Huang Y, Garrett S. Defining characteristics of communication quality in culture-changed long term care facilities. Journal of Communication in Healthcare. 2012;5:227–238. [Google Scholar]
- 29.The Joint Commission. Long Term Care: 2013 National Patient Safety Goals. 2012 [Google Scholar]
- 30.Institute of Medicine. The Future of Nursing: Leading Change Advancing Health. Washington DC: National Academies Press; 2011. [PubMed] [Google Scholar]


